Virtual Reality and Simulation Videos as Effective Training Tools for Creating Safe and Inclusive Environments for Transgender People
Abstract
:1. Introduction
2. Materials and Methods
2.1. Objectives
- To create and validate the educational audiovisual resources to be used.
- To assess their impacts by:
- Measuring knowledge growth.
- Analyse the changes in content, attitudes, and procedures.
- Measure the degree of satisfaction with the methodology used.
2.2. Participants
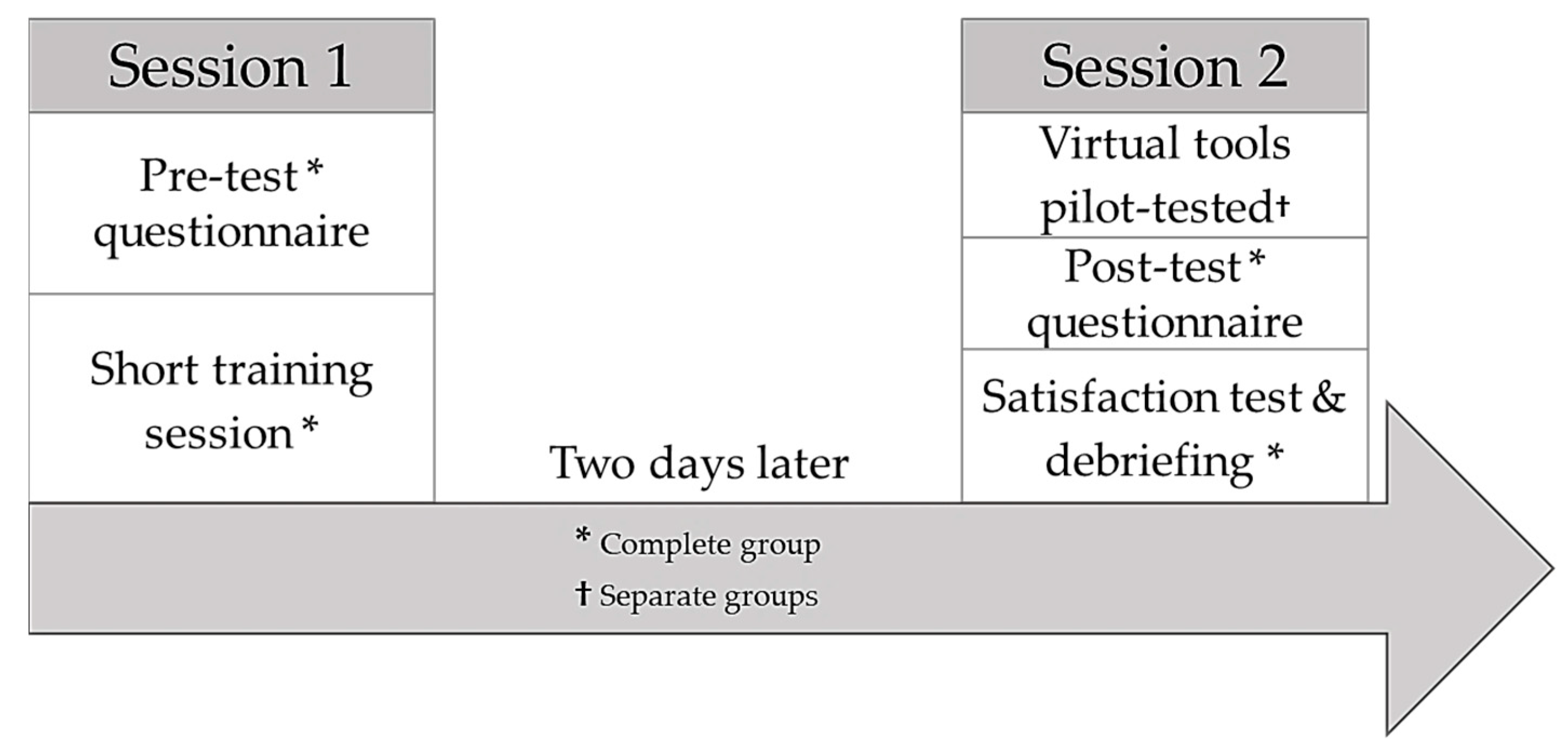
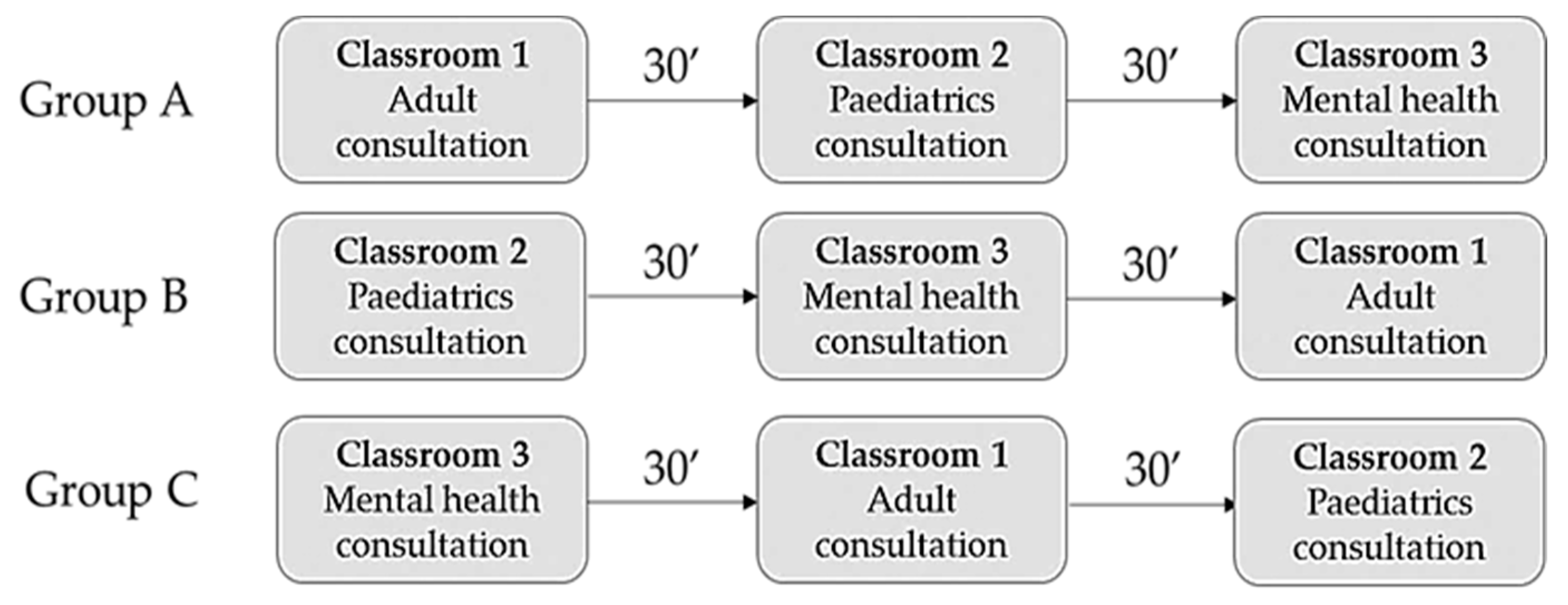
2.3. Design and Methodology
2.4. Instruments
2.5. Data Processing and Analysis
2.6. Ethics and Confidentiality
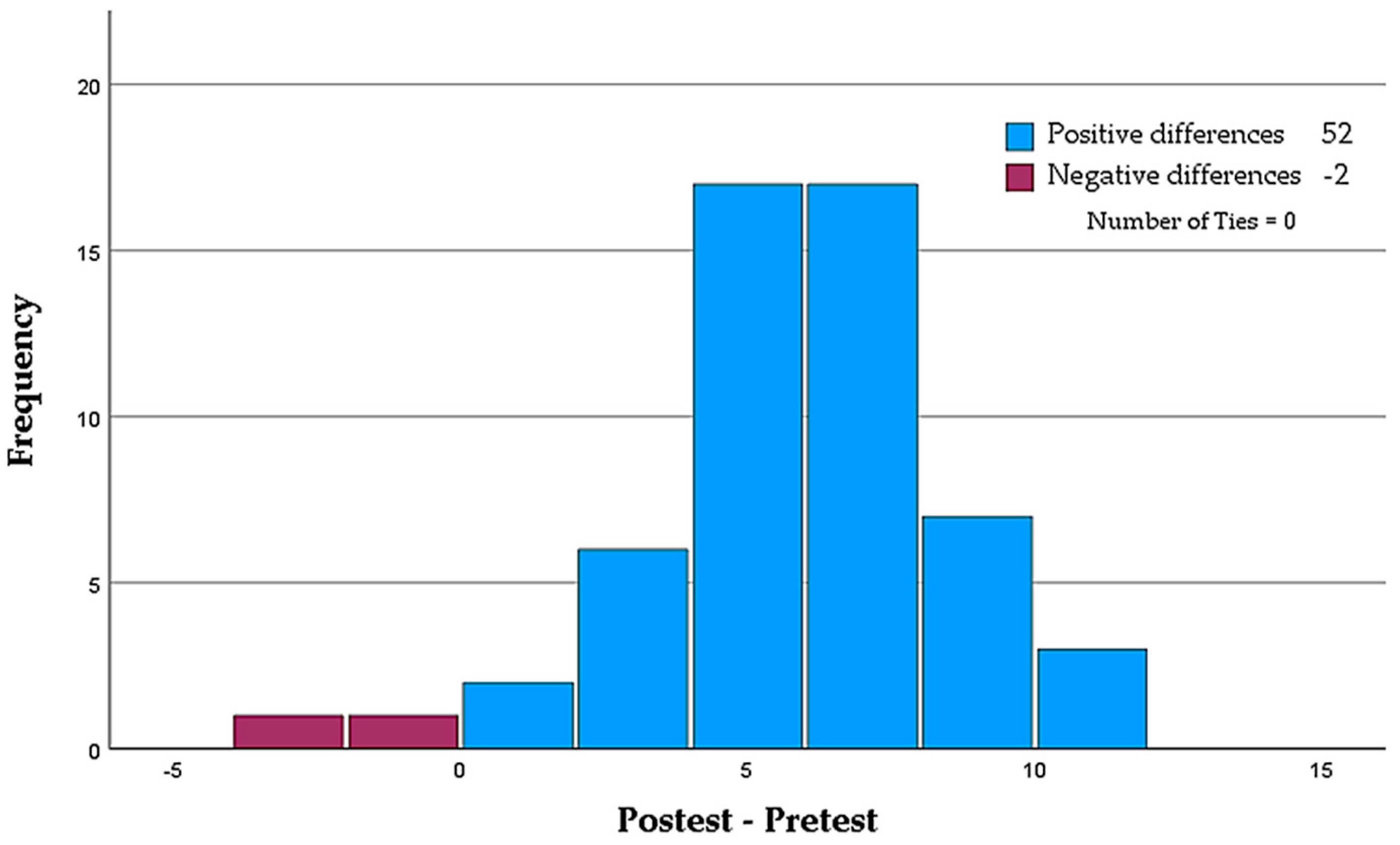
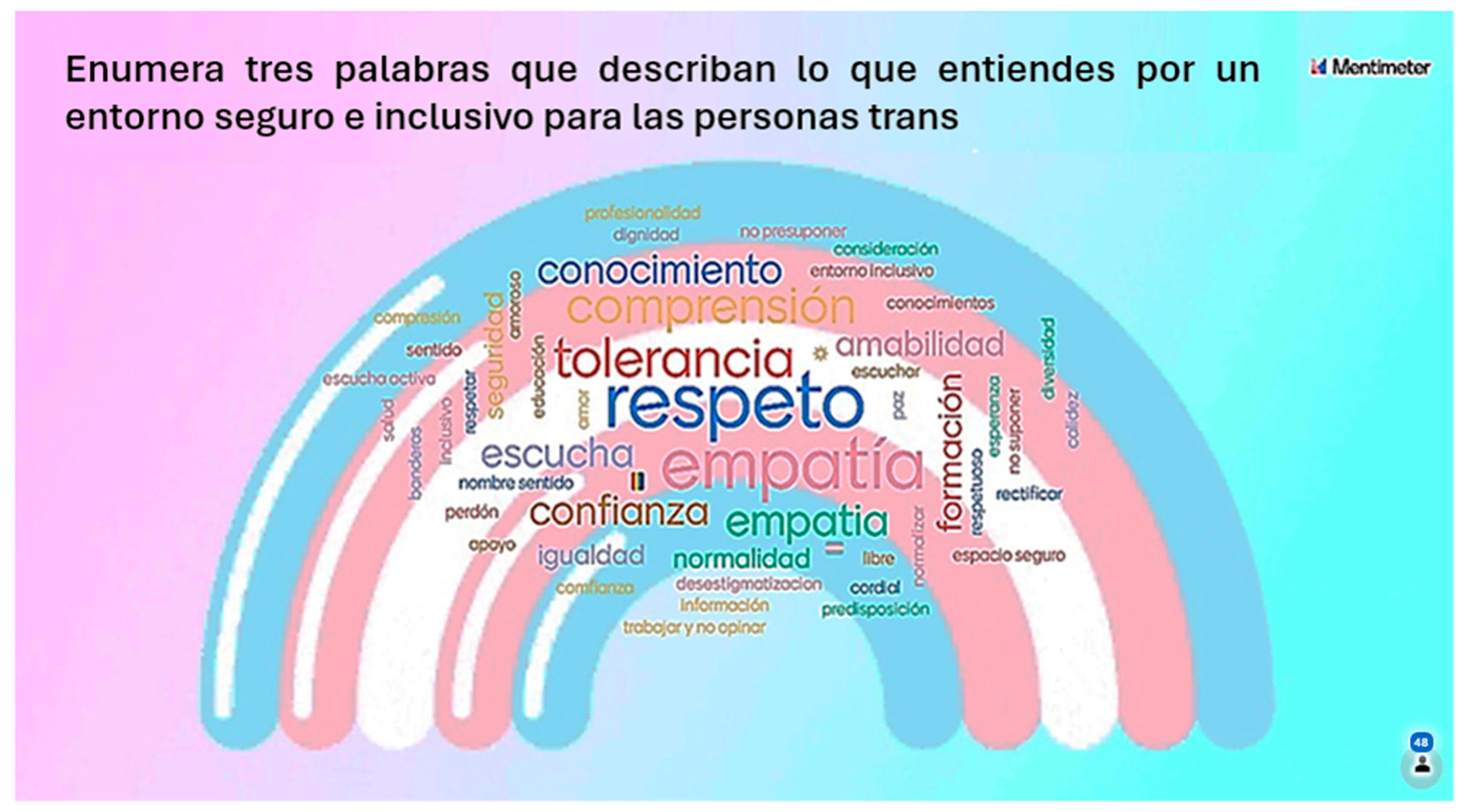
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Public Involvement Statement
Guidelines and Standards Statement
Acknowledgments
Conflicts of Interest
Appendix A
- Please select the correct statement regarding the pathologisation of transgenderism:
- Transgenderism is no longer considered a psychiatric condition.
- Both the WHO in its ICD and the APA in its DSM have removed transgenderism from their lists of psychiatric conditions.
- Only the APA in its current DSM recognises transgenderism as a psychiatric condition.
- None of the above is true.
- The difference between a transsexual person and a transgender person is that:
- The former undergoes treatments and/or surgeries that adjust their physical characteristics to the gender they identify with, while the latter does not necessarily accept their corporeality.
- The former does not undergo treatments and/or surgeries that adjust their physical characteristics to the gender they identify with, while the latter does, as they do not accept their corporeality.
- Both terms are used interchangeably.
- Neither is correct.
- Please select the correct statement:
- Gender expression is an indication of a person’s sexual orientation.
- Biological sex is the sex we are born with and is binary.
- Gender identity is one’s sense of belonging to one gender or another and may or may not be in accordance with biological sex.
- All of the above are correct.
- Please select the main barrier to accessing healthcare for transgender people:
- Prejudice.
- Transphobia.
- Ignorance.
- All of the above.
- Please select the correct statement:
- There is no protocol for action in the Canary Islands, but efforts are being made to address the needs of the population.
- The Canary Islands already have a protocol for the care of trans people that does not include intersex people.
- The Canary Islands have an approved protocol for trans and intersex people.
- None of the above is correct.
- Please select the most appropriate option if you worked at a primary care facility and had a trans woman among your users:
- I would always use the name appearing in her medical record.
- If we do not know the person, we can use their surname and then ask for their first name and pronouns.
- Until such time as this person’s registry office documents are amended, we must adhere to the patient record for legal reasons.
- If possible, I would rather not have any transgender person in my quota.
- When you meet a trans person for the first time, you:
- Ask for their meaningful name and preferred pronouns.
- Flatter them by telling them that they do not show it or that they hide it very well, as this empowers them and helps to create a therapeutic environment.
- Ask for their deadname.
- All of the above are correct.
- Meeting the specific needs of the LGBTIQ+ population is included in:
- The code of ethics for the nursing profession.
- The Canary Islands protocol for the care of trans* people.
- The Spanish Trans Law.
- The 2030 Agenda.
- Which law states that trans people have the right to be cared for by trained health professionals who are knowledgeable about the specific trans health reality?
- Canarian Law 2/2021 of 7 June, on social equality and non-discrimination on grounds of gender identity, gender expression, and sexual characteristics.
- Spanish Law 4/2023 of 28 February, for the real and effective equality of trans people and for the guarantee of the rights of LGTBI people.
- Spanish Law 3/2007 of 15 March, regulating the registry rectification of the mention regarding the sex of persons.
- None of the above. It is a duty of the health professional, not a right of the user.
- Regarding the gynaecological/urological care of a trans man, we should NOT:
- Include him in breast cancer screenings.
- Include him in cervical cancer screenings.
- Include him in prostate cancer screenings.
- Provide him with pregnancy support and perinatal care.
- What makes an environment safe for a transgender person?
- Above all, the use of neutral and inclusive language.
- A respectful approach.
- The use of brochures, banners, and infographics in the facility.
- All of the above are correct.
- In your practice, you see a 4–5-year-old child whose parents are concerned about his or her behaviour and statements, which suggest that he or she is a transgender child. You:
- Tell their parents that this is just another stage of sexual development, cases like this are very common, and not to make a big deal out of it, but to follow it up.
- Tell their parents not to encourage this behaviour so that it is not perpetuated over time, they should be patient, and that their child will be normal in the future.
- Actively listen to the child’s story, without conditioning him/her.
- Refer the child to the paediatric endocrinologist to begin hormone treatment and avoid the development of secondary sexual characteristics that may generate dysphoria in the future.
- Please select the most appropriate steps for trans children:
- From the ages of 4 to 10 years: social transition; from the ages of 11 to 14 years: hormone treatment; ≥14 years old: puberty blockers.
- From the ages of 4 to 10 years: puberty blockers; from the ages of 11 to 14 years: social transition; ≥14 years old: hormone treatment.
- From the ages of 4 to 10 years: social transition; from the ages of 11 to 14 years: puberty blockers; ≥14 years old: hormone treatment.
- None of them is correct. Trans children cannot receive any type of hormone treatment until they come of age (at 18 years old in the Spanish context).
- What would be the most appropriate way to address the sexual health of transgender people?
- By asking them openly if and how they have sexual relations.
- By asking them ‘Do you have any questions about your sexual health?’
- By asking them ‘Do you mind if I ask you a few questions about your sexuality?’
- The sexual sphere of transgender people should not be assessed by nurses, as they may feel intimidated.
- You work at a hospital. A trans man is being admitted to your unit for a mastectomy and you are told: ‘His name is Anthony, but his medical records and ID card say his name is Patricia... I need you to give me a bed for his admission.’ Please select the correct option:
- If his name does not match his legal documents and medical records, he cannot be admitted.
- He will be admitted to a ward with other females in accordance with his sex at birth.
- If possible, he/she will be given a bed in a private room and admitted alone.
- He should be admitted to a ward with other males in accordance with his gender.
References
- Coleman, E.; Bockting, W.; Botzer, M.; Cohen-Kettenis, P.; DeCuypere, G.; Feldman, J.; Fraser, L.; Green, J.; Knudson, G.; Meyer, W.J.; et al. Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, Version 7. Int. J. Transgenderism 2012, 13, 165–232. [Google Scholar] [CrossRef]
- Coleman, E.; Radix, A.E.; Bouman, W.P.; Brown, G.R.; de Vries, A.L.C.; Deutsch, M.B.; Ettner, R.; Fraser, L.; Goodman, M.; Green, J.; et al. Standards of Care for the Health of Transgender and Gender Diverse People, Version 8. Int. J. Transgender Health 2022, 23 (Suppl. S1), S1–S259. [Google Scholar] [CrossRef] [PubMed]
- Carabez, R.M.; Eliason, M.J.; Martinson, M. Nurses’ Knowledge About Transgender Patient Care: A Qualitative Study. Adv. Nurs. Sci. 2016, 39, 257–271. [Google Scholar] [CrossRef] [PubMed]
- Yingling, C.T.; Cotler, K.; Hughes, T.L. Building nurses’ capacity to address health inequities: Incorporating lesbian, gay, bisexual and transgender health content in a family nurse practitioner programme. J. Clin. Nurs. 2017, 26, 2807–2817. [Google Scholar] [CrossRef] [PubMed]
- Carabez, R.; Scott, M. ‘Nurses don’t deal with these issues’: Nurses’ role in advance care planning for lesbian, gay, bisexual and transgender patients. J. Clin. Nurs. 2016, 25, 3707–3715. [Google Scholar] [CrossRef] [PubMed]
- McCann, E.; Brown, M. Discrimination and resilience and the needs of people who identify as Transgender: A narrative review of quantitative research studies. J. Clin. Nurs. 2017, 26, 4080–4093. [Google Scholar] [CrossRef] [PubMed]
- Consejo Internacional de Enfermeras. Código Deontológico del CIE para la Profesión de Enfermería. 2006. 12p. Available online: http://www.enfermeriacanaria.com/wptfe/wp-content/uploads/Código-deontologico_CIE.pdf (accessed on 22 May 2023).
- Agencia Nacional de Evaluación de la Calidad y Acreditación (ANECA). Libro Blanco. Título de Grado en Enfermería. 2004. 336p. Available online: https://fcsalud.ua.es/es/portal-de-investigacion/documentos/enlaces-de-interes/libro-blanco-de-la-enfermeria.pdf (accessed on 13 May 2023).
- Lim, F.A.; Brown, D.V.; Jones, H. Lesbian, Gay, Bisexual, and Transgender Health: Fundamentals for Nursing Education. J. Nurs. Educ. 2013, 52, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Comunidad Autónoma de Canarias. Ley 2/2021, de 7 de Junio, de Igualdad Social y no Discriminación por Razón de Identidad de Género, Expresión de Género y Características Sexuales. BOE Núm 163, de 9 de Julio de 2021. 2021, p. 50. Available online: https://www.boe.es/eli/es-cn/l/2021/06/07/2 (accessed on 13 May 2023).
- Liu, J.; Yin, Y.; Kor, P.; Cheung, D.; Zhao, I.; Wang, S.; Su, J.J.; Christensen, M.; Tyrovolas, S.; Leung, A.Y.M. The Effects of Immersive Virtual Reality Applications on Enhancing the Learning Outcomes of Undergraduate Health Care Students: Systematic Review with Meta-synthesis. J. Med. Internet Res. 2023, 25, e39989. [Google Scholar] [CrossRef]
- Jans, C.; Bogossian, F.; Andersen, P.; Levett-Jones, T. Examining the impact of virtual reality on clinical decision making—An integrative review. Nurse Educ. Today 2023, 125, 105767. [Google Scholar] [CrossRef]
- Ruiz Hontangas, A.; Ferrer Ferrándiz, E.; Montejano Lozoya, R.; Mármol López, M.; Guirao-Goris, S.; Gea-Caballero, V. Evaluación de la vídeo-simulación como metodología docente para la entrevista motivacional en estudiantes de enfermería. Cult. Los. Cuid. Rev. Enfermería Humanidades 2019, 239–252. Available online: http://hdl.handle.net/20.500.12466/2373 (accessed on 17 August 2023). [CrossRef]
- Coll, C.; Mauri, T.; Rochera, M. La práctica de evaluación como contexto para aprender a ser aprendiz competente. Rev. Curric. Form. Profr. 2012, 16, 49–59. [Google Scholar]
- Petersen Cogo, A.; Dal Pai, D.; Badin Aliti, G.; Karnas Hoefel, H.; de Oliveira Azzolin, K.; BusinL; Unicovsky, M.A.R.; Kruse, M.H.L. Case studies and role play: Learning strategies in nursing. Rev. Bras. Enferm. 2016, 69, 1231–1235. [Google Scholar] [CrossRef]
- Pereira Costa, B.; Velludo Veiga, E.; Alves dos Santos, C.; Cardoso Costa, J.; Leite Fava, S.; Rodrigues Resck, Z. Technology in health and its influence on nursing education. Rev. Pesqui. Cuid. Fundam. Online 2021, 13, 288–294. [Google Scholar]
- Lucena-Anton, D.; Fernandez-Lopez, J.C.; Pacheco-Serrano, A.I.; Garcia-Munoz, C.; Moral-Munoz, J.A. Virtual and Augmented Reality versus Traditional Methods for Teaching Physiotherapy: A Systematic Review. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 1780–1792. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, A.; Ivimey-Cook, E. Technology-enhanced simulation for healthcare professionals: A meta-analysis. Front. Med. 2023, 10, 1149048. [Google Scholar] [CrossRef]
- Lie, S.; Helle, N.; Sletteland, N.; Vikman, M.; Bonsaksen, T. Implementation of Virtual Reality in Health Professional Higher Education: Protocol for a Scoping Review. JMIR Res. Protoc. 2022, 11, e37222. [Google Scholar] [CrossRef]
- de Oliveira Salvador, P.; dos Santos Bezerril, M.; Santos Mariz, C.; Domingues Fernandes, M.; Amado Martins, J.; Pereira Santos, V. Virtual learning object and environment: A concept analysis. Rev. Bras. Enferm. 2017, 70, 572–579. [Google Scholar] [CrossRef]
- Slater, M. Immersion and the illusion of presence in virtual reality. Br. J. Psychol. 2018, 109, 431–433. [Google Scholar] [CrossRef]
- Rose, T.; Nam, C.; Chen, K. Immersion of virtual reality for rehabilitation—Review. Appl. Ergon. 2018, 69, 153–161. [Google Scholar] [CrossRef]
- Dhar, E.; Upadhyay, U.; Huang, Y.; Uddin, M.; Manias, G.; Kyriazis, D.; Wajid, U.; AlShawaf, H.; Abdul, S.S. A scoping review to assess the effects of virtual reality in medical education and clinical care. Digit. Health 2023, 9, 18. [Google Scholar] [CrossRef]
- Slater, P.; Hasson, F.; Gillen, P.; Gallen, A.; Parlour, R. Virtual simulation training: Imaged experience of dementia. Int. J. Older People Nurs. 2019, 14, e12243. [Google Scholar] [CrossRef] [PubMed]
- Piña-Jiménez, I.; Amador-Aguilar, R. La enseñanza de la enfermería con simuladores, consideraciones teórico-pedagógicas para perfilar un modelo didáctico. Enfermería Univ. 2015, 12, 152–159. [Google Scholar] [CrossRef]
- Baptista, R.; Martins, J.; Pereira, M.; Mazzo, A. Satisfação dos estudantes com as experiências clínicas simuladas: Validação de escala de avaliação. Rev. Lat. Am. Enferm. 2014, 22, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Lewis, R.; Strachan, A.; Smith, M. Is high fidelity simulation the most effective method for the development of non-technical skills in nursing? A review of the current evidence. Open Nurs. J. 2012, 6, 82. [Google Scholar] [CrossRef] [PubMed]
- Sweigart, L.; Burden, M.; Carlton, K.; Fillwalk, J. Virtual simulations across curriculum prepare nursing students for patient interviews. Clin. Simul. Nurs. 2014, 10, e139–e145. [Google Scholar] [CrossRef]
- Jeffries, R.; Rodgers, B.; Adamson, K. NLN Jeffries Simulation Theory: Brief Narrative description. Int. J. Nurs. Educ. Sch. 2020, 9, 292–293. [Google Scholar]
- Gil-Mateu, E.; Reverté-Villarroya, S.; Albacar-Riobóo, N.; Barceló-Prats, J. A Hybrid Methodology for the Evaluation of Clinical Practice in Final-Year Nursing Students. Nurs. Rep. 2023, 13, 1004–1015. [Google Scholar] [CrossRef] [PubMed]
- Jefatura del Estado. Ley Orgánica 3/2018, de 5 de Diciembre, de Protección de Datos Personales y Garantía de los Derechos Digitales. BOE-A-2018-16673. 2018, p. 67. Available online: https://www.boe.es/eli/es/lo/2018/12/05/3/con (accessed on 9 July 2023).
- Parlamento Europeo REGLAMENTO (UE) 2016/679 DELPARLAMENTOEUROPEOY DELCONSEJO de 27 de abril de 2016 Relativo a la Protección de las Personas Físicas en lo que Respecta al Tratamiento de Datos Personales y a la Libre Circulación de Estos Datos y por el que se Deroga la, D. D. Of. Unión Eur. 2016, 88. Available online: https://eur-lex.europa.eu/legal-content/ES/TXT/HTML/?uri=CELEX:32016R0679&from=ES (accessed on 9 July 2023).
- López-Baamonde, M.; Martín-Calabuig, A.; Coca, M.; Fargas-Alpuente, M.; Gómez, L.; Bergé, R.; Tena, B. Simulación para formar en la competencia de valoración preanestésica: Diseño común para residentes de primer año de anestesiología y enfermeras de anestesia. Rev. Fund. Educ. Médica 2018, 21, 47. [Google Scholar] [CrossRef]
- Fealy, S.; Jones, D.; Hutton, A.; Graham, K.; McNeill, L.; Sweet, L.; Hazelton, M. The integration of immersive virtual reality in tertiary nursing and midwifery education: A scoping review. Nurse Educ. Today 2019, 79, 14–19. [Google Scholar] [CrossRef]
- Yánez, A.; Ortiz, L.; Espinosa, V. Information and communications technology (ICT) in health: A model to be applied in nursing training. Rev. Iberoam. Educ. Investig Enfermería 2016, 6, 29–36. [Google Scholar]
- Leite, K.; Santos, S.; Andrade, S.; Zaccara, A.; Brito, K.; Silva, S. The use of information technology and communication among teachers in the light of grounded theory. J. Nurs. UFPE Line 2016, 10, 515–523. [Google Scholar]
- Dieckmann, P.; Sharara-Chami, R.; Ersdal, H. Debriefing Practices in Simulation-Based Education. In Clinical Education for the Health Professions; Nestel, D., Reedy, G., McKenna, L., Gough, S., Eds.; Springer: Berlin/Heidelberg, Germany, 2020; pp. 1–17. [Google Scholar]
- Lillejord, S.; Børte, K.; Nesje, K.; Ruud, E. Learning and teaching with technology in higher education—A systematic review. Oslo Knowl. Cent. Educ. 2018, 2, 40–64. [Google Scholar]
- Khoirurakhmawati, Y.; Widyaningrum, K. The workshop increased knowledge, motivation and nursing attitude about five right drug administration. Enferm. Clin. 2020, 30, 221–224. [Google Scholar] [CrossRef]
- Ferreira, F.C.; Baffa Lourenço, A.; Alves da Cruz, A.; Henrique Paza, A.; Rodrigo Botero, E.; Matos Rocha, E. Argumentação em ambiente de realidade virtual: Uma aproximação com futuros professores de Física. RIED Rev. Iberoam. Educ. Distancia 2021, 24, 17. [Google Scholar] [CrossRef]
- González Vidal, I.; Cebreiro López, B.; Casal Otero, L. Nuevas competencias digitales en estudiantes potenciadas con el uso de Realidad Aumentada. Estudio Piloto. RIED Rev. Iberoam. Educ. Distancia 2021, 24, 21. [Google Scholar]
- Shorey, S.; Ng, E. The use of virtual reality simulation among nursing students and registered nurses: A systematic review. Nurse Educ. Today 2021, 98, 104662. [Google Scholar] [CrossRef] [PubMed]
- Kurul, R.; Ögün, M.; Neriman Narin, A.; Avci, S.; Yazgan, B. An Alternative Method for Anatomy Training: Immersive Virtual Reality. ASE Anat. Sci. Educ. 2020, 13, 648–656. [Google Scholar] [CrossRef] [PubMed]
- Hartstein, A.; Zimney, K.; Verkuyl, M.; Yockey, J.; Berg-Poppe, P. Virtual Reality Instructional Design in Orthopedic Physical Therapy Education: A Randomized Controlled Trial. J. Phys. Ther. Educ. 2022, 36, 176–184. [Google Scholar] [CrossRef]
- Ulrich, F.; Helms, N.; Frandsen, U.; Rafn, A. Learning effectiveness of 360 video: Experiences from a controlled experiment in healthcare education. Interact Learn Env. 2021, 29, 98–111. [Google Scholar] [CrossRef]
- Huhn, K.; McGinnis, P.; Wainwright, S.; Deutsch, J. A Comparison of 2 Case Delivery Methods: Virtual and Live. J. Phys. Ther. Educ. 2013, 27, 41–48. [Google Scholar] [CrossRef]
- Dyer, E.; Swartzlander, B.; Gugliucci, M. Using virtual reality in medical education to teach empathy. J. Med. Libr. Assoc. JMLA 2018, 106, 498. [Google Scholar] [CrossRef] [PubMed]
- Kyaw, B.; Saxena, N.; Posadzki, P.; Vseteckova, J.; Nikolaou, C.; George, P.; Divakar, U.; Masiello, I.; Kononowicz, A.A.; Zary, N.; et al. Virtual reality for health professions education: Systematic review and meta-analysis by the digital health education collaboration. J. Med. Internet Res. 2019, 21, e12959. [Google Scholar] [CrossRef] [PubMed]
- Cook, D. How much evidence does it take? A cumulative meta-analysis of outcomes of simulation-based education. Med. Educ. 2014, 48, 750–760. [Google Scholar] [CrossRef] [PubMed]
- Amini, H.; Gregory, M.; Abrams, M.; Luna, J.; Roland, M.; Sova, L.; Bean, C.; Huang, Y.; Pfeil, S.A.; Townsend, J.; et al. Feasibility and usability study of a pilot immersive virtual reality-based empathy training for dental providers. J. Dent. Educ. 2021, 85, 856–865. [Google Scholar] [CrossRef] [PubMed]
- Parejo-Aguilera, M.C.; Sacristán-Martín, M.C.; Velasco-Gil, M.C.; Álvarez-Collado, M.A.; Cortés-Ortega, M.I. QUIROforma: E-learning y flipped learning en la formación del personal de enfermería del área quirúrgica. Enfermería Docente 2020, 112, 66–69. Available online: https://www.huvv.es/sites/default/files/revistas/QUIROforma.pdf (accessed on 22 September 2023).
- Kang, S.; Hong, C.; Lee, H. The impact of virtual simulation on critical thinking and self-directed learning ability of nursing students. Clin. Simul Nurs. 2020, 49, 66–72. [Google Scholar] [CrossRef]
- Chang, C.; Kao, C.; Hwang, G.; Lin, F. From experiencing to critical thinking: A contextual game-based learning approach to improving nursing students’ performance in electrocardiogram training. Educ. Technol. Res. Dev. 2020, 68, 1225–1245. [Google Scholar] [CrossRef]
- Noordman, J.; van der Weijden, T.; van Dulmen, S. Effects of video-feedback on the communication, clinical competence and motivational interviewing skills of practice nurses: A pre-test posttest control group study. J. Adv. Nurs. 2014, 70, 2272–2283. [Google Scholar] [CrossRef]
- Yoshioka-maeda, K.; Honda, C.; Sumikawa, Y.; Okamoto, Y.; Shimada, M.; Fujii, H.; Iwasaki-Motegi, R.; Miura, T.; Otsuki, M. Developing a Virtual Reality Simulation Program for Improving Nursing Students’ Clinical Reasoning Skills in Home Settings: A Protocol Paper. Nurs. Rep. 2022, 12, 968–979. [Google Scholar] [CrossRef]
- Laker, C.; Knight-Davidson, P.; Hawkes, D.; Driver, P.; Nightingale, M.; Winter, A.; McVicar, A. The Use of 360-Degree Video in Developing Emotional Coping Skills (Reduced Anxiety and Increased Confidence) in Mental Health Nursing Students: A Protocol Paper. Nurs. Rep. 2022, 12, 536–544. [Google Scholar] [CrossRef]
- Des Jarlais, D.; Lyles, C.; Crepaz, N.; Trend Group. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: The TREND statement. Am. J. Public Health 2004, 94, 361–366. [Google Scholar] [CrossRef] [PubMed]
| N | Range | Mean | Std. Deviation | Variance | |
|---|---|---|---|---|---|
| Pre-test | 56 | 9 | 7.98 | 1.949 | 3.800 |
| Post-test | 54 | 10 | 13.22 | 2.034 | 4.138 |
| Valid N (listwise) | 54 |
| Question Pre- and Post-Tests | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | 54 | 54 | 54 | 54 | 54 | 54 | 54 | 54 | 54 | 54 | 54 | 54 | 54 | 54 | 53 | |
| Chi-squared test b | 36.02 | 15.750 | 28.195 | 31.030 | 25.714 | 24.038 | ||||||||||
| Asymp. Sig. | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||||
| Exact Sig. (two-tailed) | <0.001 c | 0.049 c | 0.063 c | 1.000 c | 0.839 c | <0.001 c | <0.001 c | <0.001 c | <0.001 c | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Acosta, J.M.; Castro-Molina, F.J.; Delgado, N.; Díez-Fernández, O.; Rodríguez-Novo, N.; de Castro-Peraza, M.E.; Lorenzo-Rocha, N.D.; Torres-Jorge, J.M.; Fernández-Martínez, A.D.; Castellano-Fuenmayor, M.A. Virtual Reality and Simulation Videos as Effective Training Tools for Creating Safe and Inclusive Environments for Transgender People. Nurs. Rep. 2024, 14, 42-55. https://doi.org/10.3390/nursrep14010004
García-Acosta JM, Castro-Molina FJ, Delgado N, Díez-Fernández O, Rodríguez-Novo N, de Castro-Peraza ME, Lorenzo-Rocha ND, Torres-Jorge JM, Fernández-Martínez AD, Castellano-Fuenmayor MA. Virtual Reality and Simulation Videos as Effective Training Tools for Creating Safe and Inclusive Environments for Transgender People. Nursing Reports. 2024; 14(1):42-55. https://doi.org/10.3390/nursrep14010004
Chicago/Turabian StyleGarcía-Acosta, Jesús Manuel, Francisco Javier Castro-Molina, Naira Delgado, Olga Díez-Fernández, Natalia Rodríguez-Novo, María Elisa de Castro-Peraza, Nieves Doria Lorenzo-Rocha, Jesús Miguel Torres-Jorge, Alfredo David Fernández-Martínez, and María Andreína Castellano-Fuenmayor. 2024. "Virtual Reality and Simulation Videos as Effective Training Tools for Creating Safe and Inclusive Environments for Transgender People" Nursing Reports 14, no. 1: 42-55. https://doi.org/10.3390/nursrep14010004
APA StyleGarcía-Acosta, J. M., Castro-Molina, F. J., Delgado, N., Díez-Fernández, O., Rodríguez-Novo, N., de Castro-Peraza, M. E., Lorenzo-Rocha, N. D., Torres-Jorge, J. M., Fernández-Martínez, A. D., & Castellano-Fuenmayor, M. A. (2024). Virtual Reality and Simulation Videos as Effective Training Tools for Creating Safe and Inclusive Environments for Transgender People. Nursing Reports, 14(1), 42-55. https://doi.org/10.3390/nursrep14010004







