Comparison of Prototype Transparent Mask, Opaque Mask, and No Mask on Speech Understanding in Noise
Abstract
1. Introduction
2. Materials and Methods
2.1. Positionality Statement
2.2. Participants
2.3. Masks
2.4. Stimuli and Recording Instrumentation
2.5. Study Procedures
- Condition 1—NMA (No Mask Audio-only; Lists 19–20, 37–38).
- Condition 2—NMAV (No Mask Audiovisual; Lists 13–14, 47–48).
- Condition 3—OMA (Opaque Mask Audio-only; Lists 1–2, 21–22).
- Condition 4—OMAV (Opaque Mask Audiovisual; Lists 3–4, 17–18).
- Condition 5—TMA (Transparent Mask Audio-only; Lists 9–10, 11–12).
- Condition 6—TMAV (Transparent Mask Auditovisual; Lists 7–8, 29–30).
2.6. Data Analysis
3. Results
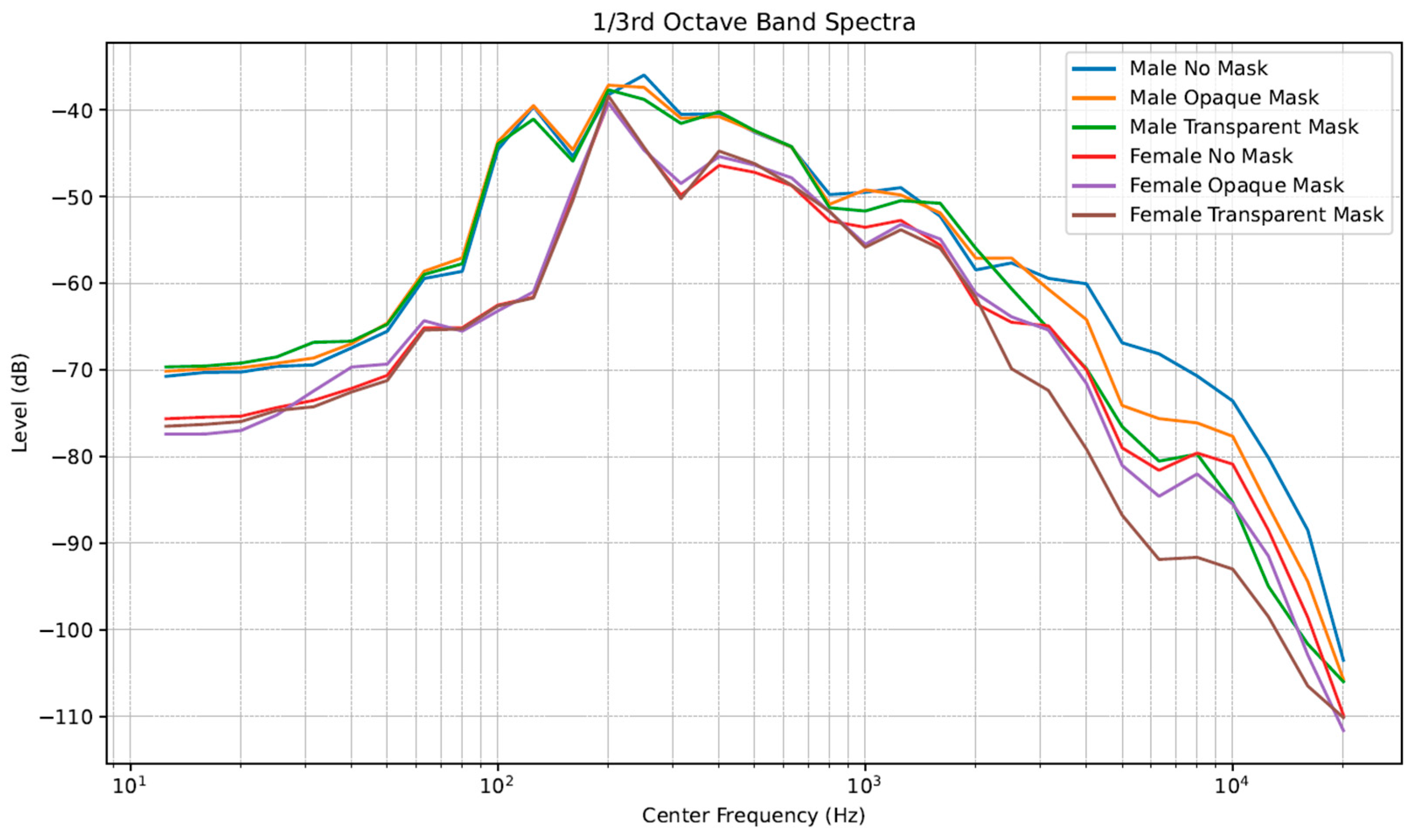
3.1. Spectral Analysis of Stimuli
3.2. Speech Perception in Noise Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ANOVA | Analysis of Variance |
| ASL | American Sign Language |
| CI | Cochlear Implant |
| CST | Connected Speech Test |
| FFT | Fast Fourier Transformation |
| HA | Hearing Aid |
| NH | Normal Hearing Group |
| NMA | No Mask Audio-Only Condition |
| NMAV | No Mask Audiovisual Condition |
| OMA | Opaque Mask Audio-Only Condition |
| OMAV | Opaque Mask Audiovisual Condition |
| MOD | Moderate Hearing Loss Group |
| RAU | Rationalized Arcsine Units |
| RMS | Root Mean Square |
| SEV | Severe-to-Profound Hearing Loss Group |
| SNR | Signal-to-Noise Ratio |
| TMA | Transparent Mask Audio-Only Condition |
| TMAV | Transparent Mask Audiovisual Condition |
References
- Mendel, L.L.; Gardino, J.A.; Atcherson, S.R. Speech understanding using surgical masks: A problem in health care? J. Am. Acad. Audiol. 2008, 19, 686–695. [Google Scholar] [CrossRef]
- Atcherson, S.R.; Mendel, L.L.; Baltimore, W.J.; Patro, C.; Lee, S.; Pousson, M.; Spann, M.J. The Effect of Conventional and Transparent Surgical Masks on Speech Understanding in Individuals with and without Hearing Loss. J. Am. Acad. Audiol. 2017, 28, 58–67. [Google Scholar] [CrossRef]
- Carroll, S.M.; Atcherson, S.R. Living in a Limited World: Experience of Lipreaders When Society Is Masked. J. Psychosoc. Nurs. Ment. Health Serv. 2023, 61, 18–26. [Google Scholar] [CrossRef]
- Badh, G.; Knowles, T. Acoustic and perceptual impact of face masks on speech: A scoping review. PLoS ONE 2023, 18, e0285009. [Google Scholar] [CrossRef]
- Francis, R.; Leavitt, M.; McLelland, C.; Hamilton, D.F. The influence of facemasks on communication in healthcare settings: A systematic review. Disabil. Rehabil. 2024, 46, 637–649. [Google Scholar] [CrossRef]
- Giovanelli, E.; Gianfreda, G.; Gessa, E.; Valzolgher, C.; Lamano, L.; Lucioli, T.; Tomasuolo, E.; Rinaldi, P.; Pavani, F. The effect of face masks on sign language comprehension: Performance and metacognitive dimensions. Conscious. Cogn. 2023, 109, 103490. [Google Scholar] [CrossRef]
- Grassi, J.; Oliveira, I.B.; Chiriboga, L.F.; Maia, A.A.; Attianezi, M.; Almeida, A.N.P. Effects on communication due to face mask use: An integrative review. Rev. Bras. Enferm. 2023, 76, e20220674. [Google Scholar] [CrossRef] [PubMed]
- Jackson, I.R.; Perugia, E.; Stone, M.A.; Saunders, G.H. The impact of face coverings on audio-visual contributions to communication with conversational speech. Cogn. Res. Princ. Implic. 2024, 9, 25. [Google Scholar] [CrossRef] [PubMed]
- McCrackin, S.D.; Ristic, J. Improving masked communication: The case for transparent masks. Front. Commun. 2024, 9, 1371142. Available online: https://www.frontiersin.org/journals/communication/articles/10.3389/fcomm.2024.1371142 (accessed on 19 June 2025). [CrossRef]
- Rahne, T.; Fröhlich, L.; Plontke, S.; Wagner, L. Influence of surgical and N95 face masks on speech perception and listening effort in noise. PLoS ONE 2021, 16, e0253874. [Google Scholar] [CrossRef]
- Saunders, G.H.; Jackson, I.R.; Visram, A.S. Impacts of face coverings on communication: An indirect impact of COVID-19. Int. J. Audiol. 2021, 60, 495–506. [Google Scholar] [CrossRef] [PubMed]
- Atcherson, S.R.; McDowell, B.R.; Howard, M.P. Acoustic effects of non-transparent and transparent face coverings. J. Acoust. Soc. Am. 2021, 149, 2249. [Google Scholar] [CrossRef] [PubMed]
- Corey, R.M.; Jones, U.; Singer, A.C. Acoustic effects of medical, cloth, and transparent face masks on speech signals. J. Acoust. Soc. Am. 2020, 148, 2371. [Google Scholar] [CrossRef]
- Goldin, A.; Weinstein, B.E.; Shiman, N. How do medical masks degrade speech perception? Hear. Rev. 2020, 27, 8–9. Available online: https://hearingreview.com/hearing-loss/health-wellness/how-do-medical-masks-degrade-speech-reception (accessed on 6 April 2020).
- Roup, C.M.; Wiley, T.L.; Safady, S.H.; Stoppenbach, D.T. Tympanometric Screening Norms for Adults. Am. J. Audiol. 1998, 7, 55–60. [Google Scholar] [CrossRef]
- Cox, R.M.; Alexander, G.C.; Gilmore, C. Development of the Connected Speech Test (CST). Ear Hear. 1987, 8 (Suppl. S5), 119S–126S. [Google Scholar] [CrossRef]
- Cox, R.M.; Alexander, G.C.; Gilmore, C.; Pusakulich, K.M. Use of the Connected Speech Test (CST) with hearing-impaired listeners. Ear Hear. 1988, 9, 198–207. [Google Scholar] [CrossRef]
- Bench, J.; Kowal, A.; Bamford, J. The BKB (Bamford-Kowal-Bench) sentence lists for partially-hearing children. Br. J. Audiol. 1979, 13, 108–112. [Google Scholar] [CrossRef]
- Niquette, P.; Arcaroli, J.; Revit, L.; Parkinson, A.; Staller, S.; Skinner, M.; Killion, M. Development of the BKB-SIN Test. In Proceedings of the Annual Meeting of the American Auditory Society, Scottsdale, AZ, USA, 13–15 March 2003. [Google Scholar]
- Studebaker, G.A. A “rationalized” arcsine transform. J. Speech Hear. Res. 1985, 28, 455–462. [Google Scholar] [CrossRef]
- Benjamini, Y.; Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. Roy. Stat. Soc. Ser. B 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Noble, W.S. How does multiple testing correction work? Nat. Biotechnol. 2009, 27, 1135–1137. [Google Scholar] [CrossRef]
- Gelfer, M.P.; Young, S.R. Comparisons of intensity measures and their stability in male and female speakers. J. Voice 1997, 11, 178–186. [Google Scholar] [CrossRef]
- Zhang, Z. Contribution of laryngeal size to differences between male and female voice production. J. Acoust. Soc. Am. 2021, 150, 4511. [Google Scholar] [CrossRef]
- Mendel, L.L.; Pousson, M.A.; Shukla, B.; Sander, K.; Larson, B. Listening Effort and Speech Perception Performance Using Different Facemasks. J. Speech Lang. Hear. Res. 2022, 65, 4354–4368. [Google Scholar] [CrossRef]
- Thibodeau, L.M.; Thibodeau-Nielsen, R.B.; Tran, C.M.Q.; Jacob, R.T.S. Communicating During COVID-19: The Effect of Transparent Masks for Speech Recognition in Noise. Ear Hear. 2021, 42, 772–781. [Google Scholar] [CrossRef]
- Rahne, T.; Wagner, T.M.; Kopsch, A.C.; Plontke, S.K.; Wagner, L. Influence of Age on Speech Recognition in Noise and Hearing Effort in Listeners with Age-Related Hearing Loss. J. Clin. Med. 2023, 12, 6133. [Google Scholar] [CrossRef] [PubMed]
- McCrackin, S.D.; Provencher, S.; Mendell, E.; Ristic, J. Transparent masks reduce the negative impact of opaque masks on understanding emotional states but not on sharing them. Cogn. Res. Princ. Implic. 2022, 7, 59, Erratum in Cogn. Res. Princ. Implic. 2022, 7, 75. [Google Scholar] [CrossRef] [PubMed]
- Pavlova, M.A.; Sokolov, A.A. Reading Covered Faces. Cereb. Cortex. 2022, 32, 249–265. [Google Scholar] [CrossRef] [PubMed]
- Schneider, J.; Sandoz, V.; Equey, L.; Williams-Smith, J.; Horsch, A.; Bickle Graz, M. The Role of Face Masks in the Recognition of Emotions by Preschool Children. JAMA Pediatr. 2022, 176, 96–98. [Google Scholar] [CrossRef]



| Participant | Group | Age | Gender | Amplification | Modality |
|---|---|---|---|---|---|
| 1 | NH | 22 | F | N/A | Oral (English) |
| 2 | NH | 24 | M | N/A | Oral (English) |
| 3 | NH | 36 | F | N/A | Oral (English) |
| 4 | NH | 23 | F | N/A | Oral (English) |
| 5 | NH | 29 | F | N/A | Oral (English) |
| 6 | NH | 52 | M | N/A | Oral (English) |
| 7 | NH | 44 | F | N/A | Oral (English) |
| 8 | NH | 29 | F | N/A | Oral (English) |
| 9 | NH | 59 | F | N/A | Oral (English) |
| 10 | NH | 69 | M | N/A | Oral (English) |
| 11 | MOD | 35 | F | 1 CI; 1 HA | Oral (English) |
| 12 | MOD | 24 | M | 2 HA | Oral (English) |
| 13 | MOD | 70 | F | 2 HA | Oral (English) |
| 14 | MOD | 77 | M | 2 HA | Oral (English) |
| 15 | MOD | 46 | M | 2 HA | Oral (English) |
| 16 | MOD | 67 | F | 2 HA | Oral (English) |
| 17 | MOD | 68 | M | 2 HA | Oral (English) |
| 18 | MOD | 46 | F | N/A | Oral (English) |
| 19 | MOD | 71 | M | 2 HA | Oral (English) |
| 20 | MOD | 69 | M | 2 HA | Oral (English) |
| 21 | SEV | 43 | M | 2 CI | Oral (English) |
| 22 | SEV | 52 | F | 2 HA | SimCom |
| 23 | SEV | 73 | M | N/A | ASL |
| 24 | SEV | 39 | M | 2 CI | Oral (English) |
| 25 | SEV | 48 | F | 2 HA | SimCom |
| 26 | SEV | 46 | F | 1 HA | Oral (English) |
| 27 | SEV | 68 | F | 1 HA | SimCom |
| 28 | SEV | 50 | F | 1 CI; 1 HA | Oral (English) |
| 29 | SEV | 19 | F | N/A | ASL |
| 30 | SEV | 18 | F | 1 HA | ASL |
| Experimental Conditions | Male Talker | Female Talker | Difference |
|---|---|---|---|
| No Mask | −18.52 | −23.85 | 5.33 |
| Opaque Mask | −18.75 | −23.48 | 4.72 |
| Transparent Mask | −19.33 | −23.45 | 4.12 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Atcherson, S.R.; Finley, E.T.; Hahne, J. Comparison of Prototype Transparent Mask, Opaque Mask, and No Mask on Speech Understanding in Noise. Audiol. Res. 2025, 15, 103. https://doi.org/10.3390/audiolres15040103
Atcherson SR, Finley ET, Hahne J. Comparison of Prototype Transparent Mask, Opaque Mask, and No Mask on Speech Understanding in Noise. Audiology Research. 2025; 15(4):103. https://doi.org/10.3390/audiolres15040103
Chicago/Turabian StyleAtcherson, Samuel R., Evan T. Finley, and Jeanne Hahne. 2025. "Comparison of Prototype Transparent Mask, Opaque Mask, and No Mask on Speech Understanding in Noise" Audiology Research 15, no. 4: 103. https://doi.org/10.3390/audiolres15040103
APA StyleAtcherson, S. R., Finley, E. T., & Hahne, J. (2025). Comparison of Prototype Transparent Mask, Opaque Mask, and No Mask on Speech Understanding in Noise. Audiology Research, 15(4), 103. https://doi.org/10.3390/audiolres15040103






