1. Introduction
External dacryocystorhinostomy (DCR) is a well-known procedure that was first described by Toti in 1904 [
1]. It is performed worldwide with only a few modifications. The basic idea is to marsupialize the sac into the nasal cavity to eliminate epiphora and recurrent dacryocystitis. Among experienced surgeons, external DCR procedures exhibit success rates ranging from 90% to 95% [
2]. In the 1980s and 1990s, with the advent of the endoscope, endoscopic DCR techniques were developed [
3,
4,
5]. The endoscopic approach eliminates the need for a skin incision and provides the surgeon with exceptional visualization of the lacrimal sac during dissection and marsupialization [
6]. Endoscopic DCR is now a well-established technique for treating nasolacrimal duct obstruction, demonstrating success rates that are comparable to those achieved with the external approach [
7,
8,
9,
10]. Traditionally, the removal of the frontal and lacrimal bone above the lacrimal sac has been performed using osteotomes or standard drills. However, these methods can damage surrounding soft tissues. Advances in technology have led to the development of new instruments aimed at minimizing this harm. One such method is piezosurgery, a relatively recent bone-cutting technique that uses ultrasound vibrations. This approach, which is widely utilized in oral and maxillofacial surgery, is increasingly being applied to various new clinical applications. Its main advantages are the preservation of soft tissues, precise bone cutting, and the possibility of use in narrow spaces. Over the past 5 years, several authors have presented their experience with the use of this tool in ENT, including antromastoidectomy, stapedectomy, the osteoplastic flap procedure, removal of osteomas of the frontal bone, and revision endoscopic sinus surgery [
11,
12,
13,
14]. There are reports on other functional procedures for the nose, including septoplasty and rhinoplasty, as surgery moves toward less invasive techniques [
15,
16]. This technology is also utilized in dentistry, demonstrating that even in local anesthesia procedures, patients experience more comfort during the procedures and improved postoperative outcomes such as reduced swelling or bleeding [
17].
The equipment utilizes the piezoelectric effect. This effect results from the passage of an electric current through ceramic material, making it contract and expand. The vibrations created are amplified and transferred to the blade of the piezoelectric tool. In this way, a mechanical cutting effect exclusively on mineralized tissues is achieved. Piezoelectric devices offer an innovative ultrasonic technique for performing osteotomies that is considered safer and more effective than traditional methods that use rotating instruments. Various inserts have been developed to maximize the benefits based on the surgeon’s specific needs [
18]. Our aim is to describe our technique using this instrument to standardize the procedure. Further studies are underway to determine whether the piezoelectric system should become the gold standard for exposing the lacrimal sac.
2. Materials and Methods
2.1. Patient Evaluation
Nasolacrimal duct obstruction (NLDO) frequently leads to persistent and bothersome epiphora (excessive tearing). In cases of longstanding NLDO, mucus can build up, potentially resulting in a mucocele in the nasolacrimal sac or even acute or chronic dacryocystitis (inflammation of the tear sac). Patients with nasolacrimal system obstruction typically present with epiphora. Dacryocystitis can cause noticeable erythema (redness) at the medial canthus (corner of the eye) and a mucopurulent discharge from the puncta (tear duct openings). It is crucial to inquire about any history of pain, redness, or discharge from the medial canthal area, since these symptoms may indicate dacryocystitis. Additionally, it is crucial to ask about nasal obstruction, which could be indicative of sinusitis or nasal polyps; epistaxis (nosebleeds), possibly signaling a tumor; and previous sinus surgeries that might have caused iatrogenic injury. Finally, septal deviation and the surgical accessibility of the lacrimal fossa should be documented. A thorough physical examination should include a detailed assessment of the eyelids for swelling, redness, or lesions and the sclera for signs of active infection. It is important to carefully evaluate punctal patency (whether the tear duct openings are functioning properly) and their positioning. Conditions such as punctal strictures and eyelid malpositioning (like entropion, where the eyelid turns inward, or ectropion, where it turns outward) can lead to poor tear drainage. Nasal endoscopy is essential for examining the intranasal anatomy in detail. This procedure allows for the inspection of the inferior and middle meatus (passages within the nasal cavity) for any indications of sinusitis, including mucopurulent drainage, inflammation, or the presence of polyps obstructing normal airflow and drainage pathways. A diagnostic syringing of the nasolacrimal system is essential for identifying any obstructions. The procedure begins by anesthetizing the conjunctiva with a local anesthetic. A lacrimal cannula is attached to a 2 mL or 3 mL saline-filled syringe. The cannula is inserted through the lower punctum into the mid-canalicular area. If the punctum is narrowed, gentle dilation with a punctal dilator may be needed. Syringing helps determine the following:
- -
Saline percentage passing into the nose;
- -
Reflux through the lower punctum;
- -
Reflux through the upper punctum;
- -
Quality of reflux (mucoid or clear);
- -
Ease of syringing.
The pressure required for irrigation is often referred to as the “educated finger,” a technique developed by the examiner through practice. The cannula should then be carefully advanced into the lacrimal sac. It is essential to verify the positioning of the cannula within the sac by detecting a firm stop; a soft stop may indicate either a distal canalicular obstruction or, more frequently, a normal kinking of the distal common canaliculus, which impedes the entry of the cannula into the sac. This procedure should be performed on both eyes in an identical manner.
Nasal endoscopy should be a standard part of the preoperative workup for all patients. It is essential when considering an endonasal Dacryocystorhinostomy (DCR) technique. During the procedure, a flexible endoscope is inserted into the nasal cavity to examine the anterior nasal area for polyps or other abnormalities. The endoscope is then advanced to assess the septum for any deviations, the health of the mucosa, and the shape and position of the middle turbinate. It is vital to identify sufficient space for performing an endoscopic DCR, as the presence of other abnormalities may complicate the procedure. The most common issue occurs when there is a deviation toward the operative side, which can obstruct access and may necessitate a septoplasty.
Before conducting endoscopic surgery, a CT scan is performed to thoroughly understand the nasal anatomy and its relationship with the lacrimal sac and duct. In rare instances, a dacryocystogram (or dacryo-CT scan) may be necessary, especially when fistulas, iatrogenic trauma, or tumors in the lacrimal sac are suspected.
2.2. Operative Technique
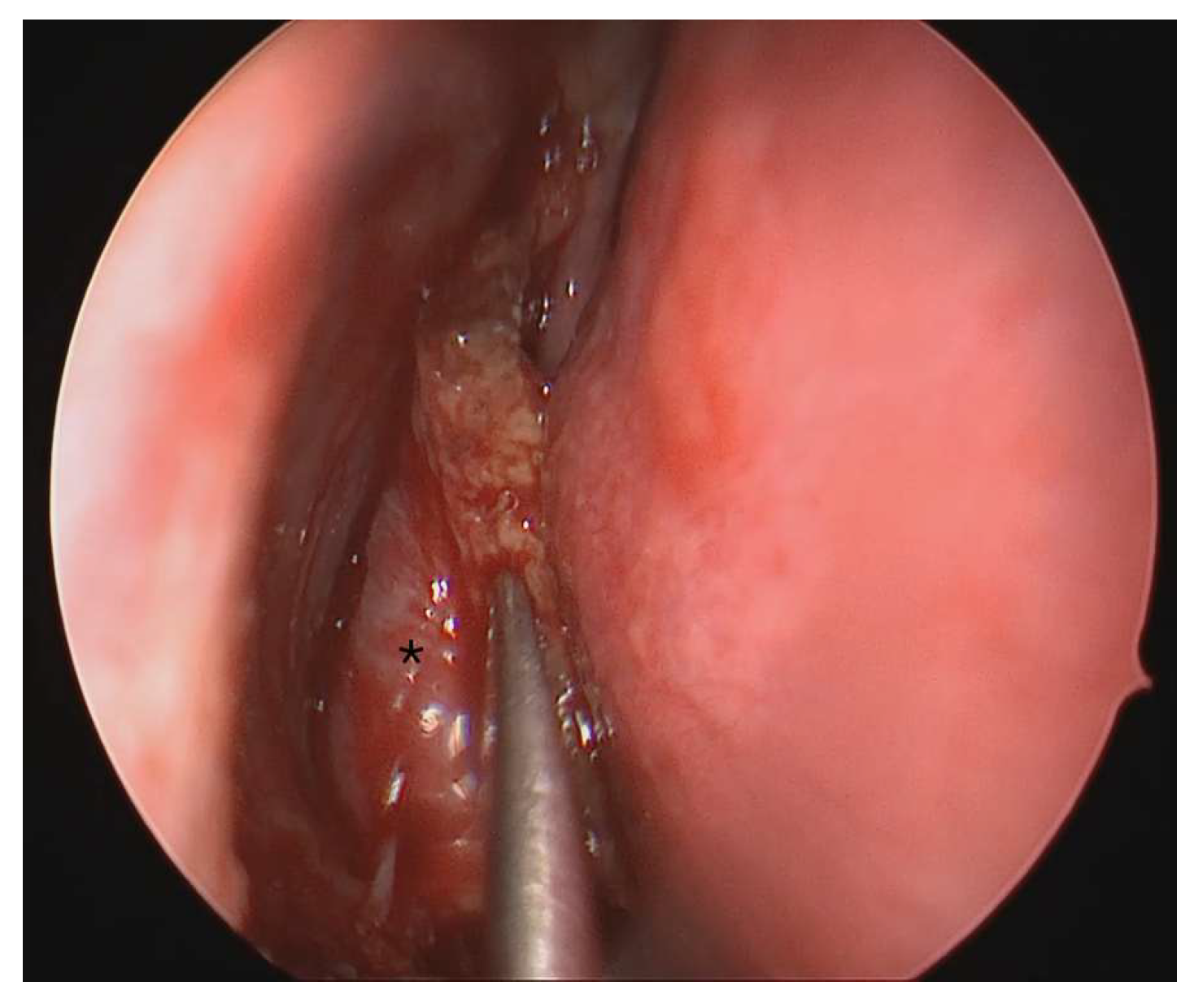
Endoscopic dacryocystorhinostomy (DCR) is performed under general anesthesia. The patient is positioned supine with the head elevated at an inclination of 15–30 degrees in the anti-Trendelenburg position. The lacrimal system is examined and, if necessary, dilated to permit the insertion of lacrimal splints. Lacrimal dilation involves gently pulling the side of the eyelid with a finger, aligning the lacrimal dilator perpendicularly to the eyelid margin, and inserting it 1 to 2 mm through the punctum. The dilator is rotated 90 degrees (parallel to the eyelid margin), and gentle pressure is applied to dilate the punctum using the conical shape of the punctum dilator. A lacrimal probe can then be inserted using a similar technique. A “hard stop” indicates that the probe has entered the lacrimal fossa and the bone is palpated. A rigid 0-degree endoscope is used. Nasal pledgets soaked in 1:1000 epinephrine are inserted into the middle meatus and the lateral nasal wall. The middle turbinate is carefully medialized to improve the view of the lateral nasal wall. Using the electrocautery scalpel and sharp dissection, a posteriorly based mucosal flap on the lateral nasal wall is lifted (
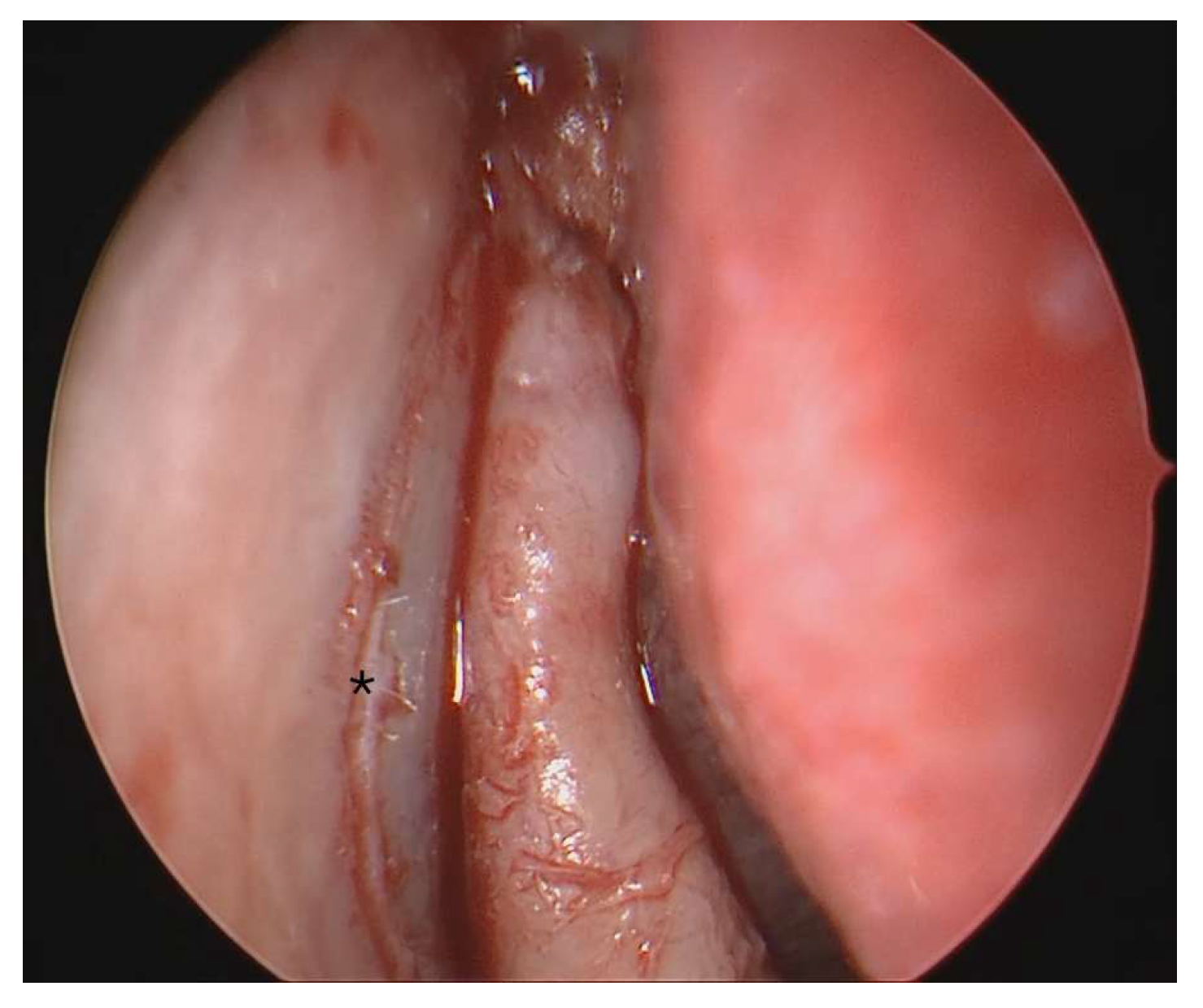
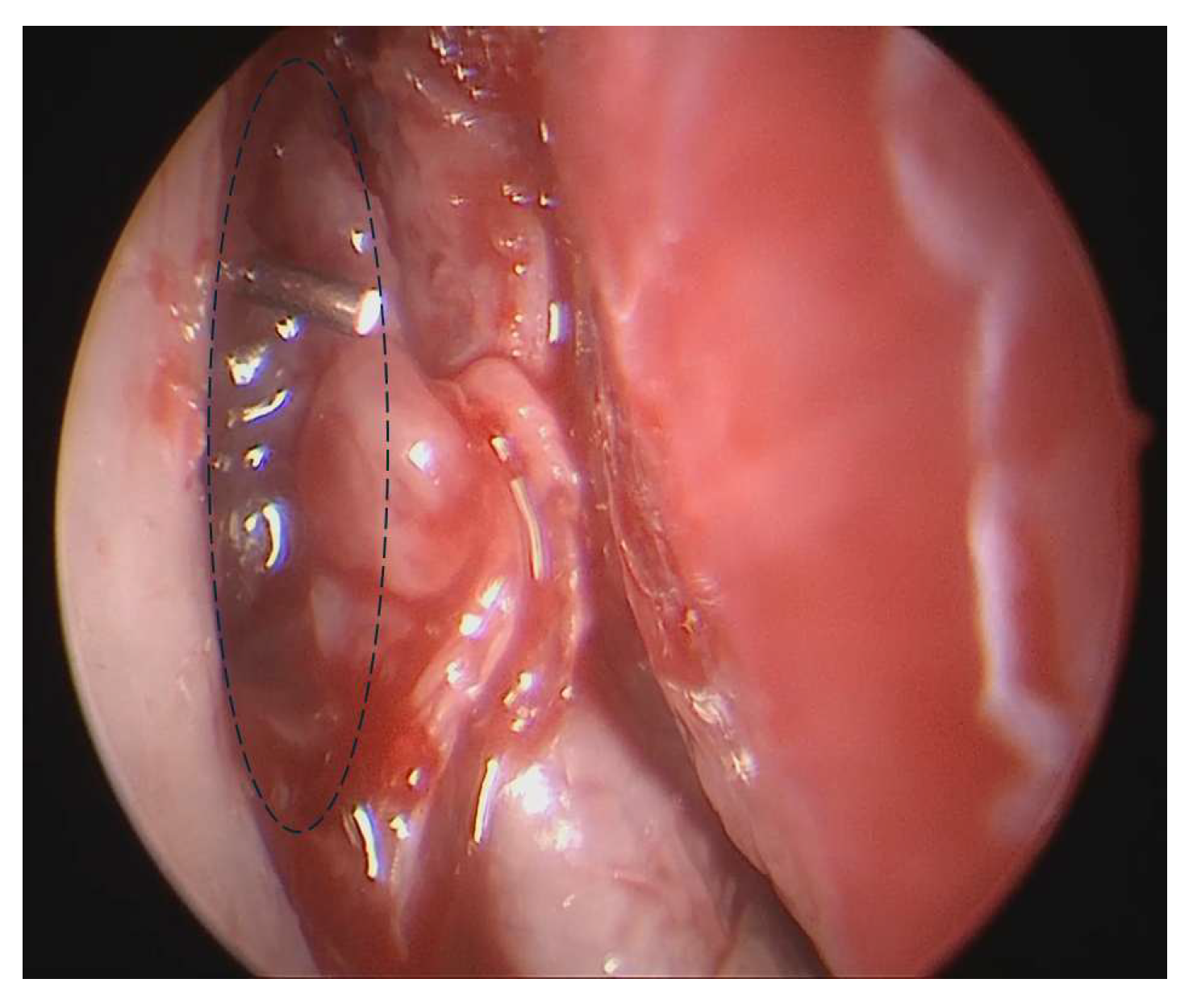
Figure 1). The incision is placed slightly above the insertion of the middle turbinate and extended 6 to 8 mm anterior to the turbinate onto the frontal process of the maxilla. The lower incision is placed approximately at the level of the free edge of the middle turbinate and merges into the upper incision. The position of the lacrimal sac is visualized from the inside with the help of an illuminated lacrimal stent, which is inserted through a punctum and placed in the lacrimal sac against the frontal process of the maxilla. While using a lacrimal stent is not necessary, it can assist surgeons, especially those with less experience or in cases of challenging anatomy, such as a high and deep-based lacrimal sac, to more accurately identify the lacrimal sac. The endoscope’s light source is turned off, dimming the illumination intranasally and enabling transillumination of the lacrimal sac. The thin lacrimal bone, situated behind the frontal process of the maxilla, is identified (
Figure 2) and removed using a piezoelectric scalpel with an OP3 insert (Piezosurgery, Mectron, Genova, Italy) (
Figure 3). Following the removal of the lacrimal bone and partially the lower part of the frontal process of the maxilla over the lacrimal sac, gentle cutaneous pressure on the lacrimal system reveals internal movement of the exposed sac. Once the lacrimal sac is fully exposed, a probe is inserted through the punctum into the sac. The probe is maneuvered both upwards and downwards to visualize the extent of the dissection from within. The upper third of the lacrimal sac is tented into the nasal cavity with the probe, after which a sickle knife is employed to make a vertical incision from the top to the bottom (
Figure 4). Care must be taken to avoid inserting the knife too deeply to prevent injury to the common canaliculus or the lateral aspect of the sac. Silastic lacrimal stents (BIKA) are then inserted through the superior and inferior puncta into the nose (
Figure 5). These stents are guided out through the nostrils and then knotted together, ensuring that the knot remains within the nasal fossa without exerting excessive tension on the lacrimal sac. Finally, the flap is repositioned to avoid obstructing the new stoma, and resorbable material is placed in the nose to stabilize the flap.
2.3. Postoperative Care
During the immediate postoperative period, the patient should be closely monitored for any occurrence of nosebleeds, also known as epistaxis. Mild nosebleeds are fairly common and usually subside within 12 to 24 h. However, if a significant nosebleed occurs, several interventions should be promptly undertaken. Initially, firm digital pressure should be applied to the front part of the nose (the anterior part) for at least 10 min, ensuring that the bleeding is controlled. If this proves insufficient, the nasal passages may need to be tightly packed with gauze or a specialized epistaxis pack designed to stem the flow of blood.
In rare cases where the bleeding continues despite these measures, it might be necessary to return the patient to the operating room for further intervention, although such occurrences are infrequent. During the first 48 h post-surgery, patients should avoid hot beverages, as the heat can dilate blood vessels and exacerbate nosebleeds. Additionally, to minimize the risk of provoking another bleed, patients should refrain from blowing their nose during the first week and should sneeze with their mouth open to reduce internal pressure on the nasal passages.
Once any nosebleeds have ceased, typically by the end of the first day, patients can begin using a steroid-based nasal spray, such as fluticasone, twice daily for a duration of four weeks to help reduce inflammation and promote healing. Alongside this, antibiotic drops and nasal rinses will be prescribed to prevent infection and keep the nasal passages clean for the initial two-week period following surgery. After four weeks, the stents placed during surgery will be carefully removed. This is performed by cutting them between the upper and lower puncta and delicately extracting them through the nose with the aid of an endoscope, ensuring precision and minimizing discomfort for the patient.
3. Discussion
Piezosurgery is an innovative system meticulously developed for cutting bone using micro-vibrations. This advanced equipment includes two ergonomic handpieces, two precise inserts, and two efficient peristaltic pumps, all connected to a sophisticated control unit. A key feature is its high-flow saline irrigation system, which atomizes the solution, creating a “bloodless” effect at the surgical site. This unique aspect significantly reduces thermal damage to both the bone surfaces and adjacent structures. The device operates on low-frequency ultrasonic waves ranging from 24 to 29 kHz, tailored to the specific density of the bone being cut. This carefully calibrated vibration frequency ensures optimal performance on mineralized tissue while safeguarding adjacent soft tissues. The cutting head immediately becomes inactive once it loses contact with mineralized tissue, thus preventing any accidental damage to sensitive areas such as tumors, blood vessels, or facial nerves.
This technique allows for the complete and meticulous exposure of the lacrimal sac. By employing the piezoelectric device to delicately remove the maxillary bone surrounding the sac, surgeons can create a large marsupialized lacrimal sac that is precisely covered with preserved nasal mucosal flaps. In every case, piezosurgery promotes rapid and efficient intraoperative management, resulting in precise, safe cuts. The surgical fields remain virtually blood-free, granting excellent visibility throughout the procedure without any signs of damage to the lacrimal sac. Piezosurgery has been linked to a reduced number of postoperative complications, particularly in terms of intraoperative bleeding [
19]. Effective bleeding control is especially crucial in endoscopic nasal surgeries, such as dacryocystorhinostomy (DCR), where even a small amount of blood can significantly impair the surgeon’s visibility.
Comparative histological analyses between piezosurgery, saws, and bur techniques reveal that the piezoelectric device fosters superior bony healing. The new bone formation is more robust and occurs more rapidly, primarily consisting of high-quality bone. Studies have shown that osteotomies performed using a bur or saw often result in less advanced stages of healing, with central areas filled with non-mineralized fibrovascular tissue. Therefore, piezosurgery seems more effective than traditional methods in enhancing the progression of skeletal repair [
20]. On the other hand, although studies demonstrate the superiority of the piezoelectric system, there are several drawbacks that may limit the widespread adoption of this technique. The primary considerations include an increased length of surgery as the piezoelectric system operates more slowly than the conventional burr, thereby prolonging operative time. While primary research primarily centers on odontoiatric and orthognathic procedures like tooth extractions or mandibular osteotomies, it is consistently observed that operative time with the piezoelectric system is notably longer [
17,
21]. This extended duration may represent a significant disadvantage. Even in our clinical practice, we observed a significant but unquantifiable lengthening of procedures. Ongoing studies aim to determine this data. Based on our experience, the piezoelectric device is less effective on dense and compact bone, resulting in extended operative time. In a limited number of cases, we had to convert osteotomies to conventional burrs or Kerrison punches. Ongoing studies are aimed at determining the cost–benefit ratios of this procedure. Additionally, the higher costs associated with the piezoelectric system can be a significant issue in underdeveloped countries or regions where the healthcare system lacks financial resources. Cost–benefit studies are required to assess if the longer operative time and higher costs are justified by the reduced invasiveness and comorbidity of the procedure.
Endoscopic DCR (dacryocystorhinostomy) is a relatively swift and straightforward procedure with a commendable success rate. One of its significant advantages is that it does not leave a facial scar, which can be aesthetically displeasing and, in some cases, disfiguring. Despite its simplicity, the procedure demands technical proficiency in endoscopic surgery and a comprehensive understanding of the anatomy. It is crucial to preserve the integrity of the lacrimal sac before making a precise incision in its medial wall with a wide opening to avoid scars and synechiae that could diminish the procedure’s effectiveness and necessitate revision surgery. Damaging the sac prior to the incision can lead to unwanted and problematic bleeding, causing the sac to deflate, which complicates recognition and may result in errors or incisions in the periorbita or surrounding tissues without effectively opening the lacrimal sac. Piezosurgery can help prevent undesired rupture of the lacrimal sac during the procedure. Since the initial report on the use of a piezoelectric system in DCR, known as powered DCR, which illustrated the safety of this tool and its comparable outcomes, there have been no studies aimed at standardizing and describing the technique [
22]. High-quality comparative studies are needed to validate or challenge this hypothesis. Considering the safety, low complication rate, and high efficacy of the procedure using conventional burrs or Kerrison punches, which have a success rate of approximately 90–95% [
7,
8,
9,
10], prospective studies are needed to evaluate whether the increased operative time and costs associated with the piezoelectric system are justified by improved outcomes. There is a lack of high-quality studies demonstrating the superiority of the piezoelectric system in performing osteotomies in endoscopic DCR techniques. Currently, it is not possible to confirm the superiority of the piezoelectric system for this procedure, and any potential benefits remain theoretical. This is a limitation of the present study. Case–control prospective studies are planned at our center to investigate these potential benefits and limitations.
Future research should focus on evaluating factors such as bone density, anatomical considerations (including the position and depth of the lacrimal sac), and the history of previous surgeries (such as revision DCR). This evaluation will aid surgeons in making an informed choice between the piezoelectric system and traditional burrs.
4. Conclusions
The primary advantage of piezosurgery is its selective cutting ability, which distinguishes between different tissue hardness levels and specifically targets mineralized structures. This capability helps avoid damage to surrounding soft tissues. In dacryocystorhinostomy (DCR), the piezoelectric system can be particularly beneficial because it preserves soft tissue integrity. Osteotomes, or standard drills, risk damaging the lacrimal sac during osteotomies. In contrast, a piezoelectric system may enable better access to the lacrimal sac while protecting soft tissues. However, further research, including case–control studies, is needed to determine whether this system provides better outcomes than traditional osteotomy procedures.