Abstract
Background/Objectives: Benign choledochojejunal anastomotic stricture (CJS) is a major late adverse event (AE) after choledochojejunostomy. An endoscopic method using balloon-assisted enteroscopy endoscopic retrograde cholangiopancreatography (BAE-ERCP) was recently developed for CJS. Methods: We retrospectively reviewed 45 patients (98 cases) who underwent BAE-ERCP for benign CJS. The primary endpoint was the success rate of ERCP. The secondary endpoints were AEs and the recurrence rate of benign CJS. Results: ERCP was successful in 36 patients (80%). Balloon dilation of the anastomosis was performed in all 36 patients in whom ERCP was successful, and temporary plastic stent (PS) placement was performed in 20 of these patients (55.6%). Three cases of PS migration and one case of portal vein thrombosis occurred as mild AEs. However, one case of intestinal perforation required emergency surgery for repair. In univariate analysis, proficiency in ERCP procedures (p = 0.019) and surgery at our hospital (p = 0.010) emerged as major factors affecting the procedural success. In univariate analysis, only the early onset of CJS within 400 days after choledochojejunostomy was extracted as a significant factor for the early recurrence of CJS after ERCP (p = 0.036). Conclusions: To ensure successful BAE-ERCP for CJS, it is essential to have proficiency in the ERCP and collect as much detailed information about prior surgery as possible before the procedure. Additionally, the risk of CJS recurrence might be high in patients in whom CJS develops early after surgery.
1. Introduction
Choledochojejunostomy is a widely performed surgical procedure for treating hepatobiliary pancreatic diseases such as pancreatic cancer and bile duct cancer, as well as biliary injuries. Benign choledochojejunal anastomotic stricture (CJS) is a major late adverse event (AE) after choledochojejunostomy with a reported incidence of approximately 10% [1,2,3]. As it is difficult to perform endoscopic retrograde cholangiopancreatography (ERCP) to treat CJS after gastrointestinal reconstruction, affected patients have traditionally been treated using percutaneous transhepatic biliary drainage (PTBD) or other surgical procedures [2]. However, endoscopic treatment using balloon-assisted enteroscopy ERCP (BAE-ERCP) has been developed in recent years for patients with pancreatobiliary diseases [4,5,6]. Several studies have described the usefulness of endoscopic balloon dilation and temporary stent placement for relieving CJS via BAE-ERCP [7,8]. However, difficult cases are still encountered, such as those in which the enteroscope cannot be inserted because of intestinal adhesion or the stricture cannot be penetrated because of severe stricture. In recent years, the usefulness of endoscopic ultrasound-guided biliary drainage (EUS-BD) in cases of CJS that are difficult to treat with BAE-ERCP has been described [9,10,11]. However, no large-scale prospective studies on EUS-BD for the treatment of CJS have been reported. Moreover, we encounter cases in which CJS recurrence occurs during long-term follow-up despite successful endoscopic treatment, necessitating frequent endoscopic treatment. However, few reports examined the factors related to the success rate of BAE-ERCP procedures for CJS or factors related to CJS recurrence [12,13,14].
Therefore, this study investigated the short- and long-term clinical outcomes of patients with benign CJS who received BAE-ERCP.
2. Materials and Methods
2.1. Study Design
Figure 1 presents the patient flow chart. The inclusion criteria were as follows: CJS-associated signs (detection of intrahepatic bile duct dilatation by imaging); signs of acute cholangitis, such as elevated serum liver and biliary enzymes (>1.5 × the upper limit of normal) or fever (body temperature of ≥38 °C); and CJS confirmed by cholangiography and endoscopy during ERCP. The exclusion criteria were as follows: reflux cholangitis, intrahepatic stones without CJS, malignant CJS, liver abscess without CJS, postoperative biliary fistula without CJS, cholangitis of unknown origin, and refusal to participate in the study. A total of 45 patients with CJS who underwent BAE-ERCP were enrolled, and 98 BAE-ERCP procedures were performed in these patients.
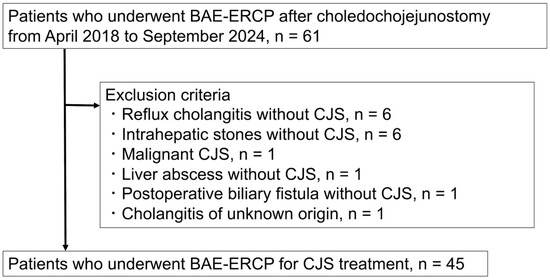
Figure 1.
Patient flow chart. BAE-ERCP, balloon-assisted enteroscopy and endoscopic retrograde cholangiopancreatography; CJS, choledochojejunal anastomotic stricture (Source: Koh Kitagawa).
This study was approved by the Nara Medical University Ethics Committee (#2701) and was performed in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology Statement. The need for written informed consent for study participation was waived because of the retrospective study design. Hence, an opt-out approach was used.
2.2. ERCP
Before undergoing ERCP, all patients provided written informed consent. For ERCP, the patient was typically placed in the prone position. In cases in which insertion of the scope into the intestinal tract was difficult, the patient was placed in the supine or lateral position, and manual compression was applied to the abdomen. Anesthesia or sedation was achieved using midazolam and buprenorphine hydrochloride or haloperidol and dexmedetomidine hydrochloride as needed. Vital signs were monitored by electrocardiography, and oxygen saturation was continuously assessed during the procedure. Oxygen was administered via a nasal cannula as needed. A balloon-assisted enteroscope (EI-580BT; Fujifilm Medical, Tokyo, Japan) was used in the procedure (Figure 2). Once the scope reached the choledochojejunal anastomosis, anastomosis was observed to identify the presence of CJS. Using a standard ERCP catheter (MTW ERCP catheter; MTW Endoskopie, Wesel, Germany), selective bile duct cannulation was performed with wire-guided cannulation and contrast medium injection.
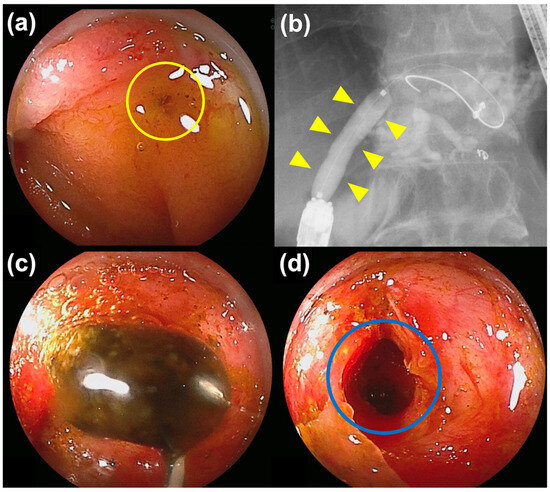
Figure 2.
Balloon-assisted enteroscopy and endoscopic retrograde cholangiopancreatography for choledochojejunal anastomotic stricture (CJS). (a) Endoscopic image of the anastomosis with a pinhole-like choledochojejunal anastomotic stricture (yellow circle). (b) Fluoroscopic image. Balloon dilation for CJS was performed (yellow arrowheads). (c) The patient had complicated intrahepatic stones, which were removed using a basket catheter. (d) All of the stones were removed, and the anastomosis was patent (blue circle), negating the need for stent placement (Source: Koh Kitagawa).
After biliary cannulation, CJS was first relieved using a balloon catheter (Hurricane™ RX, Boston Scientific, Natick, MA, USA; REN, Kaneka Medix Corp., Osaka, Japan). The diameter of the expansion balloon was selected according to the diameter of the bile duct. For patients with intrahepatic stones, the stones were removed using a basket catheter (Medi-Globe 8-Wire Nitinol Basket, Medi-Globe GmbH, Rohrdorf, Germany). In cases in which no stones were present and CJS was sufficiently relieved by balloon dilation, the procedure was completed without plastic stent (PS) placement. Conversely, if it were judged that CJS had not been sufficiently released because a narrowing “waist” remained by fluoroscopy at the anastomosis site after balloon dilation or a stone remained, PSs were placed. In patients who underwent PS placement, balloon dilation and PS replacement were performed every 3–4 months, and the stents were scheduled for removal after 6–12 months. The stent-demanding time (SDT) was defined as the period from initial PS placement until a PS was no longer required or the last follow-up.
2.3. Outcomes and Definition
Technical success was defined as successful advancement of the enteroscope to the choledochojejunal anastomosis, successful biliary cannulation, and successful CJS dilation using a balloon catheter. Clinical success was defined as an improvement in clinical symptoms or a reduction in serum transaminase levels of at least 50% within 14 days after ERCP. CJS recurrence was defined as the reappearance of clinical and diagnostic findings meeting the inclusion criteria after a previously successful CJS treatment by ERCP.
The primary endpoint was the ERCP success rate. The secondary endpoints were AEs, the benign CJS recurrence rate, and long-term prognosis.
The diagnosis and severity of acute cholangitis were determined based on the Tokyo Guideline 2018 [15]. AEs were evaluated using the American Society for Gastrointestinal Endoscopy severity grading system [16]. Furthermore, the introduction phase was defined as the first 3 years of the study, and the proficiency phase was defined as the last 3 years of the study.
Iwasa et al. previously conducted a receiver operating characteristic analysis of recurrence after endoscopic balloon dilation for CJS [12], determining that the risk of recurrence is higher if CJS occurs earlier than 13.2 months after choledochojejunostomy. Therefore, we defined the development of CJS within 400 days after surgery as early-onset CJS. These outcomes were evaluated for each of the 45 patients, while AEs related to ERCP were evaluated for 98 ERCP procedures.
2.4. Statistical Analyses
EZR ver. 2.7 (Saitama Medical Center, Jichi Medical University, Saitama, Japan) [17], which is a graphical user interface for R ver. 4.2.2 (The R Foundation for Statistical Computing, Vienna, Austria), was used to perform statistical analyses. The chi-squared test or Fisher’s exact test was used to compare categorical variables. The t-test or the Mann–Whitney U test was used to analyze continuous data with skewed distributions. Univariate analysis was performed to assess the associations between possible risk factors for ERCP failure. The associations between the median time to CJS recurrence and 11 parameters were evaluated via Cox proportional hazard model analyses. Survival curves for time to CJS recurrence were estimated using the Kaplan–Meier method. p of <0.05 was considered statistically significant.
3. Results
3.1. Participant Characteristics
The median follow-up period was 943 days (range, 13–2324). Table 1 presents the clinical and demographic characteristics of the patients. The most common cause of biliary reconstruction surgery was pancreatic cancer. Moreover, the reconstruction types were pancreaticoduodenectomy (PD) and modified Child’s method in 45 cases, followed by the Roux-en-Y (R-Y) method in 13 cases. Intrahepatic stone complications were observed in 28 patients (62.2%). The median time from surgery to ERCP was 1057 days (range, 116–12,807).

Table 1.
Patient characteristics.
3.2. Procedural Details and AEs
Table 2 presents the ERCP procedural details and adverse events. ERCP was successful in 36 patients (80%). All unsuccessful procedures were attributable to failure of the scope to reach the choledochojejunal anastomosis. Balloon dilation of the anastomosis was performed in all 36 patients in whom ERCP was successful, and PS placement was performed in 20 of these patients (55.6%). In patients who underwent PS placement, the median SDT was 154 days. Regarding AEs, all three cases of PS migration and the case of portal vein thrombosis were mild. However, one case of intestinal perforation required emergency surgery to repair the perforation. This intestinal perforation occurred during ERCP for periodic PS replacement.

Table 2.
Endoscopic retrograde cholangiopancreatography procedures and adverse events.
3.3. Potential Factors Affecting Procedural Success
Univariate analysis identified proficiency concerning ERCP (p = 0.0193) and the facility at which the surgery was performed (p = 0.010) as significant factors affecting procedural success (Table 3).

Table 3.
Potential factors affecting procedural success (univariate analysis).
3.4. Recurrence of CJS
Among the 36 patients in whom endoscopic treatment was successful, eight (22.2%) experienced recurrence of CJS. Survival curve for time to CJS recurrence was shown in Figure 3. Univariate analysis identified early-onset CJS as a significant factor for the early recurrence of CJS after ERCP (hazard ratio = 4.651; 95% confidence interval = 1.102–19.63; p = 0.036; Table 4).
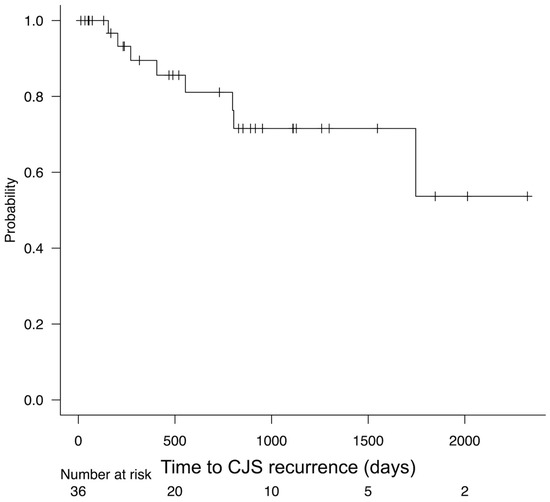
Figure 3.
Kaplan–Meier curve for time to choledochojejunal anastomotic stricture (CJS) recurrence (Source: Koh Kitagawa).

Table 4.
Cox proportional hazards regression for the duration of anastomosis patency.
3.5. Prognosis
Table 5 presents the prognosis of the patients with CJS. Five patients (11.1%) died during the follow-up period, including four who succumbed to pancreatic cancer recurrence and one to severe liver abscess.

Table 5.
Prognosis.
4. Discussion
In this study, the short-term clinical outcomes after BAE-ERCP for benign CJS improved with increased procedural proficiency. Although the long-term prognosis was generally good, the development of CJS in the early postoperative period after choledochojejunostomy was a substantial risk factor for early CJS recurrence. Given the single death attributable to severe liver abscess, patients who undergo choledochojejunostomy require careful follow-up using imaging and blood tests, even if CJS was successfully resolved using ERCP.
Owing to the development of BAE-ERCP techniques, many cases of CJS that previously could only be treated using PTBD or repeat surgery can now be treated endoscopically [7,8,12,14,18]. However, BAE-ERCP carries substantial technical difficulty [19,20]. Few studies have examined the factors related to the failure of BAE-ERCP for various biliary–pancreatic diseases [4,21,22]. However, factors that affect the failure of BAE-ERCP procedures have been described, including R-Y reconstruction methods, naive duodenal papilla, malignant tumors [4], and the first ERCP attempt [21]. Interestingly, the success rate of the procedure in this study was significantly lower in patients who underwent choledochojejunostomy at another hospital, and the cause was failure of the enteroscope to reach the anastomosis. In such cases, it was often impossible to check the operation records before performing ERCP, and the details of the surgical procedure and postoperative course were unknown. Therefore, the possibility that difficulty in inserting the scope decreased the success of the procedure cannot be dismissed. Furthermore, the success rate of the procedure was significantly higher during the last 3 years of the study than during the first 3 years. Moreover, few reports have described the learning curve for BAE-ERCP [23,24,25]. According to past reports, at least 30 procedures must be completed to gain proficiency in BAE-ERCP. The existence of a learning curve for BAE-ERCP in CJS treatment is also apparent.
In recent years, improvements in surgical outcomes and advances in preoperative and postoperative adjuvant therapies have improved the prognosis of patients with pancreatobiliary malignant neoplasms, and the number of patients with relatively long survival has increased [26,27,28,29]. In 2022, hepatobiliary and pancreatic surgeons at our institution identified a narrow preoperative common bile duct (≤9 mm) as a significant risk factor for the development of CJS after PD [30]. Thus, CJS is more likely to occur in patients with relatively early-stage malignancies who do not have biliary obstruction or obstructive jaundice. In recent years, the development of diagnostic imaging and endoscopic techniques has increased the likelihood of detecting early-stage pancreatic and biliary malignancies [27,31,32,33,34,35]. As such, CJS is a more important issue for long-term survivors after choledochojejunostomy. Particularly, repeated CJS recurrence can substantially diminish quality of life. Several reports previously identified possible risk factors for CJS relapse [12,13,14]. Iwasa et al. reported that CJS occurring within 13.2 months after bile duct jejunostomy is a significant risk factor for the early recurrence of CJS [12]. Based on this report, our study investigated the effect of the timing of postoperative CJS onset on recurrence using a cutoff of 400 days. Our results aligned with those of Iwasa et al., as we identified the development of CJS early after choledochojejunostomy as the only risk factor for early recurrence after endoscopic treatment. Meanwhile, previous studies described a relationship between the disappearance of the waist on fluoroscopic images when the stricture is dilated with a balloon catheter and a lower risk of CJS recurrence [12,13]. However, disappearance of the waist did not affect the time to CJS recurrence in our study. The possible reasons for the incongruent findings include difficulty in judging the disappearance of the waist on fluoroscopic images and high variability in the diameter of the bile duct and that of the balloon used in each patient. Additionally, the effect of PS placement after balloon dilation cannot be neglected. Iwasa et al. treated CJS using balloon dilation during ERCP without stent placement [12]. Contrarily, if we judged that CJS dilation with a balloon catheter was insufficient, we placed a PS and performed periodical stent replacement until sufficient dilation was achieved. Therefore, further investigation is needed to determine the impact of the disappearance of the waist during balloon dilation on CJS.
The indication for PS placement in BAE-ERCP for CJS treatment remains controversial. Tomoda et al. and Weng et al. reported that CJS treatment with balloon dilation without PS placement is a significant risk factor for CJS recurrence after treatment [14,18]. However, in cases involving PS placement, multiple ERCP procedures are required for periodic PS replacement or removal. This is not a problem in cases in which ERCP is technically easy, but when intestinal adhesions complicate scope insertion, the risk of AEs might be elevated. Iwasa et al. reported the effectiveness of single-balloon dilation via ERCP for CJS, considering the disadvantages of PS placement [12]. They proposed a treatment strategy in which CJS is initially treated with balloon dilation alone, and metallic stents are temporarily placed in cases of relapse. We experienced several AEs in cases of PS placement, such as PS migration and intestinal perforation during periodic PS replacement. Given the lack of evidence regarding stent placement for CJS, further evaluation is needed regarding the optimal stent selection and placement period, as well as its efficacy and safety.
Conversely, in our study, treatment via EUS-BD was performed in one case in which BAE-ERCP was unsuccessful. The usefulness of CJS treatment via EUS-BD has also been reported in recent years [9,10,11]. However, most previous studies on EUS-BD for CJS treatment were retrospective studies with small numbers of patients. In BAE-ERCP, it is possible to observe the choledochojejunal anastomosis site on the endoscopic screen, enabling assessment of the benign or malignant nature of CJS. Meanwhile, the inability to determine the benign or malignant nature of CJS is a drawback of EUS-BD. Therefore, further research is necessary to determine whether BAE-ERCP or EUS-BD is superior for CJS treatment.
However, this study had multiple limitations. First, this was a single-center retrospective study with a small number of patients. Consequently, it was not possible to perform multivariate analysis. In addition, the possibility of bias regarding patient selection or treatment decision making cannot be dismissed.
5. Conclusions
Technical proficiency and the availability of detailed information about past operations before the procedure are critical factors for the success of BAE-ERCP for CJS. Furthermore, the risk of CJS recurrence can be increased when CJS develops early after surgery.
Author Contributions
Conceptualization, K.K. (Koh Kitagawa) and S.A.; Data curation, S.A., J.-i.H., K.K. (Kosuke Kaji), A.M., Y.M., Y.O., and T.I.; Formal analysis, K.K. (Koh Kitagawa) and S.A.; Investigation, K.K. (Koh Kitagawa) and S.A.; Methodology, K.K. (Koh Kitagawa) and S.A.; Project administration, K.K. (Koh Kitagawa) and S.A.; Resources, K.K. (Koh Kitagawa) and S.A.; Supervision, H.Y.; Validation, K.K. (Koh Kitagawa) and S.A.; Visualization, K.K. (Koh Kitagawa) and S.A.; Writing the original draft, S.A. and K.K. (Koh Kitagawa); Writing review and editing, H.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Nara Medical University (protocol code 2701 and date of approval 4 August 2024).
Informed Consent Statement
Written informed consent was not required for this retrospective study using anonymized data. An opt-out method approved by the Ethics Committee was employed, whereby study information was disclosed on the hospital website and patients were given the opportunity to decline participation.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflicts of interest for this article.
References
- Dimou, F.M.; Adhikari, D.; Mehta, H.B.; Olino, K.; Riall, T.S.; Brown, K.M. Incidence of hepaticojejunostomy stricture after hepaticojejunostomy. Surgery 2016, 160, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Booij, K.A.C.; Coelen, R.J.; de Reuver, P.R.; Besselink, M.G.; van Delden, O.M.; Rauws, E.A.; Busch, O.R.; van Gulik, T.M.; Gouma, D.J. Long-term follow-up and risk factors for strictures after hepaticojejunostomy for bile duct injury: An analysis of surgical and percutaneous treatment in a tertiary center. Surgery 2018, 163, 1121–1127. [Google Scholar] [CrossRef] [PubMed]
- House, M.G.; Cameron, J.L.; Schulick, R.D.; Campbell, K.A.; Sauter, P.K.; Coleman, J.; Lillemoe, K.D.; Yeo, C.J. Incidence and outcome of biliary strictures after pancreaticoduodenectomy. Ann. Surg. 2006, 243, 571–576. [Google Scholar] [CrossRef] [PubMed]
- Tanisaka, Y.; Ryozawa, S.; Itoi, T.; Yamauchi, H.; Katanuma, A.; Okabe, Y.; Irisawa, A.; Nakahara, K.; Iwasaki, E.; Ishii, K.; et al. Efficacy and factors affecting procedure results of short-type single-balloon enteroscopy–assisted ERCP for altered anatomy: A multicenter cohort in Japan. Gastrointest. Endosc. 2022, 95, 310–318.e1. [Google Scholar] [CrossRef] [PubMed]
- Shimatani, M.; Matsushita, M.; Takaoka, M.; Koyabu, M.; Ikeura, T.; Kato, K.; Fukui, T.; Uchida, K.; Okazaki, K. Effective short double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy: A large case series. Endoscopy 2009, 41, 849–854. [Google Scholar] [CrossRef] [PubMed]
- Yamada, A.; Kogure, H.; Nakai, Y.; Takahara, N.; Mizuno, S.; Tada, M.; Koike, K. Performance of a new short-type double-balloon endoscope with advanced force transmission and adaptive bending for pancreaticobiliary intervention in patients with surgically altered anatomy: A propensity-matched analysis. Dig. Endosc. 2019, 31, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Tomoda, T.; Kato, H.; Ueki, T.; Ogawa, T.; Hirao, K.; Akimoto, Y.; Matsumoto, K.; Horiguchi, S.; Tsutsumi, K.; Okada, H. Efficacy of double-balloon enteroscopy-assisted endoscopic balloon dilatation combined with stent deployment for hepaticojejunostomy anastomotic stricture. Dig. Endosc. 2022, 34, 604–611. [Google Scholar] [CrossRef] [PubMed]
- Iwasa, Y.; Iwashita, T.; Iwata, K.; Okuno, M.; Shimojo, K.; Uemura, S.; Tezuka, R.; Senju, A.; Iwata, S.; Shimizu, M. Safety and efficacy of covered self-expandable metallic stent for choledochojejunal anastomotic stricture: A multi-center retrospective cohort study. Dig. Dis. Sci. 2024, 69, 3481–3487. [Google Scholar] [CrossRef] [PubMed]
- Dell’Anna, G.; Nunziata, R.; Delogu, C.; Porta, P.; Grassini, M.V.; Dhar, J.; Barà, R.; Bencardino, S.; Fanizza, J.; Mandarino, F.V.; et al. The role of therapeutic endoscopic ultrasound in management of malignant double obstruction (biliary and gastric outlet): A comprehensive review with clinical scenarios. J. Clin. Med. 2024, 13, 7731. [Google Scholar] [CrossRef] [PubMed]
- Iwashita, T.; Uemura, S.; Tezuka, R.; Senju, A.; Yasuda, I.; Shimizu, M. Current status of endoscopic ultrasound-guided antegrade intervention for biliary diseases in patients with surgically altered anatomy. Dig. Endosc. 2023, 35, 264–274. [Google Scholar] [CrossRef] [PubMed]
- Nagai, K.; Mukai, S.; Abe, M.; Sofuni, A.; Tsuchiya, T.; Tanaka, R.; Tonozuka, R.; Yamamoto, K.; Matsunami, Y.; Kojima, H.; et al. Long-term outcomes after EUS-guided antegrade intervention for benign bilioenteric anastomotic stricture. Gastrointest. Endosc. 2024, 99, 50–60. [Google Scholar] [CrossRef] [PubMed]
- Iwasa, Y.; Iwashita, T.; Iwata, K.; Uemura, S.; Okuno, M.; Tezuka, R.; Senju, A.; Mukai, T.; Shimizu, M. Long- and short-term outcomes of balloon dilation for benign choledochojejunal anastomotic stricture using balloon endoscopy-assisted ERCP: A multi-center retrospective cohort study. BMC Gastroenterol. 2023, 23, 191. [Google Scholar] [CrossRef] [PubMed]
- Sano, I.; Katanuma, A.; Kuwatani, M.; Kawakami, H.; Kato, H.; Itoi, T.; Ono, M.; Irisawa, A.; Okabe, Y.; Iwashita, T.; et al. Long-term outcomes after therapeutic endoscopic retrograde cholangiopancreatography using balloon-assisted enteroscopy for anastomotic stenosis of choledochojejunostomy/pancreaticojejunostomy. J. Gastroenterol. Hepatol. 2019, 34, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Weng, H.; Fan, Q.Q.; Gu, J.; Weng, M.Z.; Zhang, W.J.; Xu, L.M.; Zhang, Y.; Shu, Y.J.; Wang, X.F. Efficacy and long-term outcomes of single-balloon enteroscopy-assisted treatment for biliary obstruction after choledochojejunostomy. Surg. Endosc. 2024, 38, 6282–6293. [Google Scholar] [CrossRef] [PubMed]
- Kiriyama, S.; Kozaka, K.; Takada, T.; Strasberg, S.M.; Pitt, H.A.; Gabata, T.; Hata, J.; Liau, K.H.; Miura, F.; Horiguchi, A.; et al. Tokyo Guidelines 2018: Diagnostic criteria and severity grading of acute cholangitis (with videos). J. Hepato-Bil. Pancreat. Sci. 2018, 25, 17–30. [Google Scholar] [CrossRef] [PubMed]
- Cotton, P.B.; Eisen, G.M.; Aabakken, L.; Baron, T.H.; Hutter, M.M.; Jacobson, B.C.; Mergener, K.; Nemcek, A.; Petersen, B.T.; Petrini, J.L.; et al. A lexicon for endoscopic adverse events: Report of an ASGE workshop. Gastrointest. Endosc. 2010, 71, 446–454. [Google Scholar] [CrossRef] [PubMed]
- Kanda, Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Tomoda, T.; Kato, H.; Miyamoto, K.; Saragai, Y.; Mizukawa, S.; Yabe, S.; Takata, S.; Muro, S.; Uchida, D.; Matsumoto, K.; et al. Comparison between endoscopic biliary stenting combined with balloon dilation and balloon dilation alone for the treatment of benign hepaticojejunostomy anastomotic stricture. J. Gastrointest. Surg. 2020, 24, 1352–1358. [Google Scholar] [CrossRef] [PubMed]
- Shimatani, M.; Mitsuyama, T.; Tokuhara, M.; Masuda, M.; Miyamoto, S.; Ito, T.; Nakamaru, K.; Ikeura, T.; Takaoka, M.; Naganuma, M.; et al. Recent advances of endoscopic retrograde cholangiopancreatography using balloon assisted endoscopy for pancreaticobiliary diseases in patients with surgically altered anatomy: Therapeutic strategy and management of difficult cases. Dig. Endosc. 2021, 33, 912–923. [Google Scholar] [CrossRef] [PubMed]
- Shimatani, M.; Mitsuyama, T.; Yamashina, T.; Takeo, M.; Horitani, S.; Saito, N.; Matsumoto, H.; Orino, M.; Kano, M.; Yuba, T.; et al. Advanced technical tips and recent insights in ERCP using balloon-assisted endoscopy. DEN Open 2024, 4, e301. [Google Scholar] [CrossRef] [PubMed]
- Yane, K.; Katanuma, A.; Maguchi, H.; Takahashi, K.; Kin, T.; Ikarashi, S.; Sano, I.; Yamazaki, H.; Kitagawa, K.; Yokoyama, K.; et al. Short-type single-balloon enteroscope-assisted ERCP in postsurgical altered anatomy: Potential factors affecting procedural failure. Endoscopy 2017, 49, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Kogure, H.; Nakai, Y.; Ishigaki, K.; Hakuta, R.; Saito, K.; Saito, T.; Takahara, N.; Hamada, T.; Mizuno, S.; et al. Double-balloon endoscopy-assisted treatment of hepaticojejunostomy anastomotic strictures and predictive factors for treatment success. Surg. Endosc. 2020, 34, 1612–1620. [Google Scholar] [CrossRef] [PubMed]
- Hosono, K.; Sato, T.; Hasegawa, S.; Kurita, Y.; Yagi, S.; Iwasaki, A.; Fujita, Y.; Sekino, Y.; Tanida, E.; Kessoku, T.; et al. Learning curve of endoscopic retrograde cholangiopancreatography using single-balloon enteroscopy. Dig. Dis. Sci. 2022, 67, 2882–2890. [Google Scholar] [CrossRef] [PubMed]
- Uchida, D.; Tsutsumi, K.; Kato, H.; Matsumi, A.; Saragai, Y.; Tomoda, T.; Matsumoto, K.; Horiguchi, S.; Okada, H. Potential factors affecting results of short-type double-balloon endoscope-assisted endoscopic retrograde cholangiopancreatography. Dig. Dis. Sci. 2020, 65, 1460–1470. [Google Scholar] [CrossRef] [PubMed]
- Tanisaka, Y.; Mizuide, M.; Fujita, A.; Jinushi, R.; Ogawa, T.; Katsuda, H.; Saito, Y.; Miyaguchi, K.; Mashimo, Y.; Ryozawa, S. Competence development of trainees performing short-type single-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy. J. Hepato-Bil. Pancreat. Sci. 2022, 29, 1316–1326. [Google Scholar] [CrossRef] [PubMed]
- Grobmyer, S.R.; Pieracci, F.M.; Allen, P.J.; Brennan, M.F.; Jaques, D.P. Defining morbidity after pancreaticoduodenectomy: Use of a prospective complication grading system. J. Am. Coll. Surg. 2007, 204, 356–364. [Google Scholar] [CrossRef] [PubMed]
- Kanno, A.; Masamune, A.; Hanada, K.; Maguchi, H.; Shimizu, Y.; Ueki, T.; Hasebe, O.; Ohtsuka, T.; Nakamura, M.; Takenaka, M.; et al. Multicenter study of early pancreatic cancer in Japan. Pancreatology 2018, 18, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Nakachi, K.; Ikeda, M.; Konishi, M.; Nomura, S.; Katayama, H.; Kataoka, T.; Todaka, A.; Yanagimoto, H.; Morinaga, S.; Kobayashi, S.; et al. Adjuvant S-1 compared with observation in resected biliary tract cancer (JCOG1202, Ascot): A multicentre, open-label, randomised, controlled, phase 3 trial. Lancet 2023, 401, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Uesaka, K.; Boku, N.; Fukutomi, A.; Okamura, Y.; Konishi, M.; Matsumoto, I.; Kaneoka, Y.; Shimizu, Y.; Nakamori, S.; Sakamoto, H.; et al. Adjuvant chemotherapy of S-1 versus gemcitabine for resected pancreatic cancer: A phase 3, open-label, randomised, non-inferiority trial (JASPAC 01). Lancet 2016, 388, 248–257. [Google Scholar] [CrossRef] [PubMed]
- Nagai, M.; Nakagawa, K.; Nishiwada, S.; Terai, T.; Hokuto, D.; Yasuda, S.; Matsuo, Y.; Doi, S.; Akahori, T.; Sho, M. Clinically relevant late-onset biliary complications after pancreatoduodenectomy. World J. Surg. 2022, 46, 1465–1473. [Google Scholar] [CrossRef] [PubMed]
- Kitagawa, K.; Mitoro, A.; Suzuki, H.; Tomooka, F.; Asada, S.; Hanatani, J.I.; Motokawa, Y.; Iwata, T.; Osaki, Y.; Takeda, M.; et al. Role of liquid-based cytology in the endoscopic diagnosis of pancreatic ductal adenocarcinoma. J. Clin. Med. 2024, 13, 6148. [Google Scholar] [CrossRef] [PubMed]
- Kitagawa, K.; Mitoro, A.; Tomooka, F.; Asada, S.; Fujinaga, Y.; Nishimura, N.; Kaji, K.; Kawaratani, H.; Akahane, T.; Ozutsumi, T.; et al. Diagnostic yield of liquid-based cytology in serial pancreatic juice aspiration cytological examination. DEN Open 2023, 3, e177. [Google Scholar] [CrossRef] [PubMed]
- Sagami, R.; Nakahodo, J.; Minami, R.; Yamao, K.; Yoshida, A.; Nishikiori, H.; Takenaka, M.; Mizukami, K.; Murakami, K. True diagnostic ability of EUS-guided fine-needle aspiration/biopsy sampling for small pancreatic lesions ≤10 mm and salvage diagnosis by pancreatic juice cytology: A multicenter study. Gastrointest. Endosc. 2024, 99, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Hanada, K.; Shimizu, A.; Kurihara, K.; Ikeda, M.; Yamamoto, T.; Okuda, Y.; Tazuma, S. Endoscopic approach in the diagnosis of high-grade pancreatic intraepithelial neoplasia. Dig. Endosc. 2022, 34, 927–937. [Google Scholar] [CrossRef] [PubMed]
- Iiboshi, T.; Hanada, K.; Fukuda, T.; Yonehara, S.; Sasaki, T.; Chayama, K. Value of cytodiagnosis using endoscopic nasopancreatic drainage for early diagnosis of pancreatic cancer: Establishing a new method for the early detection of pancreatic carcinoma in situ. Pancreas 2012, 41, 523–529. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).