Abstract
Background and Importance: Chronic subdural hematoma (cSDH) is a common and complex neurosurgical problem, particularly in elderly patients. Revision surgery for chronic subdural hematoma can be challenging, particularly in cases with inhomogeneous, firm consistency and extensive adhesions. Clinical Presentation: In this article, we present our endless-loop craniotomy technique, which offers a novel approach to address these challenges by performing the wide, curved exposure of the subdural space utilizing the already-present burr hole. This technique allows for a wide, unobstructed view of the subdural space, enabling the access and evacuation of this chronic and often adhesive subdural hematoma. Conclusion: We believe that endless-loop craniotomy is a valuable addition to the neurosurgeon’s armamentarium for managing complex cases of revision surgery in chronic subdural hematomas.
1. Introduction
Chronic subdural hematoma (cSDH) is a common and complex neurosurgical problem, particularly in elderly patients. Despite advances in surgical techniques and postoperative care, cSDH frequently recurs, posing significant challenges to neurosurgeons. The recurrence rate for cSDH is estimated to range from 15% to 30%, with some studies reporting rates as high as 50% in certain patient populations []. The consequences of recurrence can be devastating, leading to significant morbidity, mortality, and healthcare resource utilization.
The pathophysiology of cSDH recurrence is multifactorial, involving a complex interplay of factors, including patient demographics, underlying comorbidities, and technical aspects of surgical intervention. Patient factors such as older age, female sex, and pre-existing cognitive impairments have been identified as risk factors for recurrence [].
Recurrent cSDH often presents with subtle but significant clinical symptoms, including headache, confusion, and cognitive decline. Delayed diagnosis and treatment can lead to further neurological deterioration, increased morbidity, and poorer outcomes. As the global population ages, the incidence of cSDH is likely to increase, emphasizing the need for effective management strategies and evidence-based guidelines for the prevention and treatment of recurrent cSDH [,].
At the moment, there is no clearly developed treatment plan for recurrent chronic hematomas; interventions can include the repeated placement of drainage, craniotomy, embolization of the middle meningeal artery, or conservative therapy with tranexamic acid or atorvastatin.
2. Clinical Presentation
A 79-year-old man presented to our university hospital with a 2-month history of headache, confusion, and left-sided hemiparesis. A computed tomography (CT) scan revealed a large, bilateral chronic subdural hematoma with a significant mass effect from the right side. The patient was treated with right-sided burr-hole trepanation, hematoma evacuation, and subdural drain placement for 2 days. The symptoms improved postoperatively, and because of the asymptomatic clinical course, middle meningeal arterial (MMA) embolization was performed for the treatment of left-sided cSDH. The patient was discharged 7 days after surgical treatment.
Unfortunately, 18 days after discharge, the patient developed a seizure disorder and showed right-sided hemiparesis and incomplete aphasia, resulting in a hospital readmission. The CT scan revealed progression of the left-sided cSDH with the flattening of the gyration and, thus, was seen as symptomatic (Figure 1A). A reexamination of the head CT revealed that a 71.8 mL cSDH had returned. The patient was taken to the operating room and underwent burr-hole trepanation and hematoma evacuation. However, due to the firm hematoma, no subdural drain placement was achievable, and the post-op CT scan revealed a postoperative subarachnoid hemorrhage (Figure 1B).
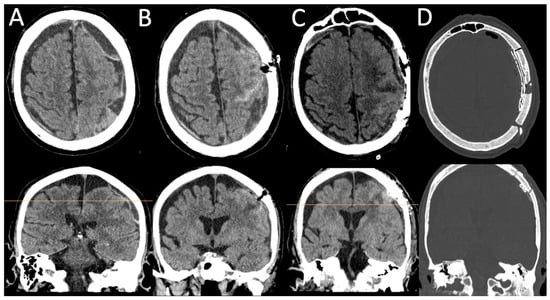
Figure 1.
(A,B): Pre- and post-burr-hole CT scans after left-sided cSDH evacuation in axial and coronal views. (C,D): Different window settings after revision surgery with endless-loop craniotomy and the placement of a Jackson-Pratt drain. The yellow horizontal line on the coronal slices shows the axial level.
After the patient showed no clinical improvement, we identified an indication for revision surgery by means of craniotomy and hematoma evacuation, which was performed using the herein-introduced endless-loop craniotomy technique. Details of the surgical steps are displayed in the next section. Because of the vulnerable cortex and an already-present postoperative hemorrhage, we chose a non-watertight dura closure, and an epidural Jackson-Pratt drain was left for 2 days (Figure 1C,D). Figure 2 shows an illustration of the two different surgical techniques in a sagittal CT scout: burr-hole (A) and endless-loop craniotomy (B). The detailed operative steps for craniotomy, dura opening, and drain management are shown in Figure 3 and Figure 4. The operation was performed as planned without intraoperative complications.
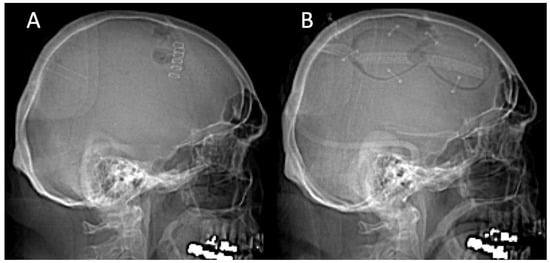
Figure 2.
(A): Sagittal X-ray after burr-hole evacuation of bilateral chronic subdural hematomas. (B): X-ray after revision surgery with endless-loop craniotomy. Note the in situ Jackson-Pratt drain directed posteriorly.
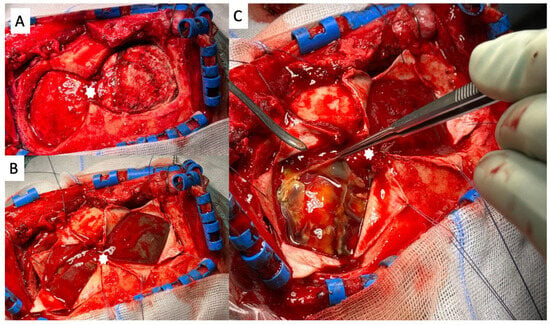
Figure 3.
An intraoperative view of the endless-loop craniotomy procedure for revision surgery. White asterisks mark the former burr hole. (A): Endless-loop craniotomy was performed, involving the wide, curved exposure of the dura mater with the T-incision flap retracted anteriorly. (B): The dura mater was incised in a visualized manner, allowing for the wider exposure of the subdural space. White asterisks mark the pre-existing position of the dura opening. (C): The subdural hematoma was visualized, with its “cranificated” appearance and its inhomogeneous, firm consistency.
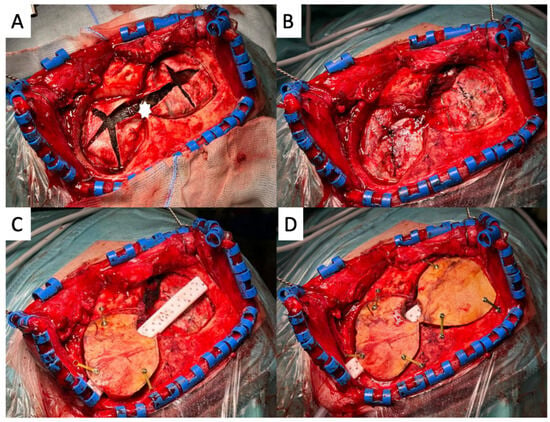
Figure 4.
An intraoperative view of the final steps of the endless-loop craniotomy procedure. (A): The dural lips were swiveled back to their original position. White asterisks mark the pre-existing position of the dura opening. (B): The dura mater was sutured using a continuous suture technique in a non-watertight fashion. (C): An epidural Jackson-Pratt drain was inserted to drain any residual hematoma, and the partial reinsertion of the bone flap was visualized. (D): The bone flap was partially reinserted, allowing for the closure of the craniotomy site.
The patient made a significant recovery after surgery, with an improvement in cognitive function, motor strength, and seizure control. He was discharged from the hospital 2 weeks after repeat surgery and was able to return to his normal activities. Four weeks after the operation, the patient had a routine consultation with us, and a follow-up CT scan was performed, which showed positive dynamics (Figure 5). In addition, the patient felt well; the neurological deficit had fully regressed, and the patient is undergoing planned rehabilitation.
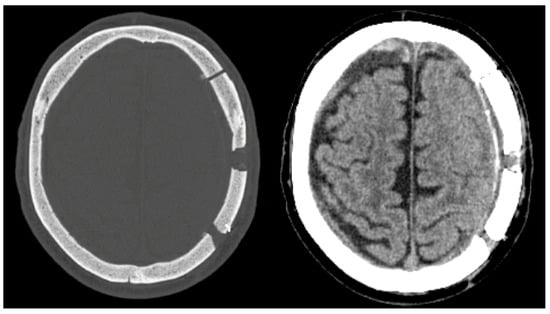
Figure 5.
Postoperative conditions in the long-term course (4 weeks postoperatively). The CT scan of the bone and soft tissue window showed the regular position of bone fragments and the clearly regressed width of the subdural hematoma on the left side without any space-occupying effect or clinical significance.
3. Key Steps in Performing Endless-Loop Craniotomy
- Extend the present burr-hole incision in a T-shaped manner;
- Use the present burr hole for craniotomy in an endless-loop “∞” fashion;
- Close the dura in a non-watertight fashion;
- Place an epidural Jackson-Pratt drain.
4. Discussion
This case highlights the challenges of operating on firm, chronic SDH showing complexity that requires careful planning and execution. These hematomas can be adherent to the surrounding brain tissue, making it difficult to separate them from the brain, and they can be difficult to evacuate through a sole burr hole. Additionally, the risk of bleeding and damage to the surrounding brain tissue is usually increased in these cases [,,].
There are various studies by our colleagues on the recurrence of chronic hematomas and the different approaches to addressing this issue, both pharmacologically and surgically []. Additionally, various intravascular interventions, such as embolization, are becoming more and more common. However, the question arises, as in our case, regarding the best course of action to take when further recurrence occurs even after the embolization of the middle meningeal artery []. The literature increasingly discusses the issue of craniotomy following minimally invasive interventions. For example, Wei Zhu et al. propose the removal of hematomas by drilling multiple holes in the lateral skull. The author reports that this technique draws inspiration from the treatment of moyamoya disease, where the scalp, through these bone holes, forms multiple “meat column” structures with a strong absorption capability. This allows the scalp to penetrate into the hematoma, potentially leading to the resolution of the cSDH [].
To overcome these challenges, neurosurgeons may use the herein-proposed technique of endless-loop craniotomy, which offers several benefits for revision surgery in these cases. The procedure involves the wide, curved exposure of the subdural space, allowing for the facilitated evacuation of the hematoma and minimizing the risk of bleeding. The wide exposure also reduces the risk of damage to the surrounding brain tissue and improves visualization of the surgical site.
One of the significant advantages of this technique is its ability to utilize the pre-existing incision, transforming it into a T-shaped configuration. This approach addresses the difficulty of extending a craniotomy from a previously performed incision while ensuring that the resulting cosmetic defect is minimal. Furthermore, the creation of two separate craniotomies, with almost no shared bony edge, may have potential advantages, including a reduced risk of postoperative complications such as epidural hematomas, infections, and other post-craniotomy issues.
Although we acknowledge the absence of comparative studies, we hypothesize that this design may offer benefits in terms of postoperative outcomes due to the lack of a large continuous bone edge, which could otherwise increase the risk of complications.
We would like to emphasize that this article primarily serves as a form of technical report describing the methodology of a single patient. However, we plan to conduct a prospective analysis in the future to compare this technique with conventional methods and evaluate its effectiveness more comprehensively.
This study did not control for potential confounding variables, such as age, sex, and underlying medical conditions, which might have affected the outcomes. Despite these limitations, this technical note provides valuable insights into the use of endless-loop craniotomy for revision surgery in firm, chronic subdural hematomas and highlights the need for further research in this area.
5. Conclusions
Overall, endless-loop craniotomy is a valuable technique to consider when managing firm, chronic subdural hematomas that were initially treated with burr-hole trepanation, as it offers a wide range of benefits such as enhanced exposure, surgical flexibility, and the potential to reduce the risk of recurrence, improving patient outcomes and minimizing the risk of complications.
Author Contributions
Conceptualization, A.R. and D.D.; methodology, D.D.; writing—original draft preparation, A.R.; writing—review and editing, D.D. and S.-Y.W.; project administration, F.G. and T.M.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Institutional Review Board approval was not required.
Informed Consent Statement
The patient consented to the anonymous publication of his case.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to ethical restrictions imposed by the institutional review board.
Acknowledgments
The authors would like to thank all the nurses and physicians involved in this case.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Dubinski, D.; Won, S.-Y.; Behmanesh, B.; Cantré, D.; Mattes, I.; Trnovec, S.; Baumgarten, P.; Schuss, P.; Freiman, T.M.; Gessler, F. Significance of Temporal Muscle Thickness in Chronic Subdural Hematoma. J. Clin. Med. 2022, 11, 6456. [Google Scholar] [CrossRef] [PubMed]
- Kan, P.; Fiorella, D.; Dabus, G.; Samaniego, E.A.; Lanzino, G.; Siddiqui, A.H.; Chen, H.; Khalessi, A.A.; Pereira, V.M.; Fifi, J.T.; et al. ARISE I Consensus Statement on the Management of Chronic Subdural Hematoma. Stroke 2024, 55, 1438–1448. [Google Scholar] [CrossRef] [PubMed]
- Maroufi, S.F.; Farahbakhsh, F.; Macdonald, R.L.; Khoshnevisan, A. Risk factors for recurrence of chronic subdural hematoma after surgical evacuation: A systematic review and meta-analysis. Neurosurg. Rev. 2023, 46, 270. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Yan, R.; Xie, F.; Richard, S.A. Hematoma cavity separation and neomembrane thickness are potential triggers of recurrence of chronic subdural hematoma. BMC Surg. 2022, 22, 236. [Google Scholar] [CrossRef] [PubMed]
- Thomas, J. Scruton, Updates on the diagnosis and management of subdural hematoma. JAAPA 2024, 37, 9–15. [Google Scholar] [CrossRef]
- Matsumoto, H.; Hanayama, H.; Okada, T.; Sakurai, Y.; Minami, H.; Masuda, A.; Tominaga, S.; Miyaji, K.; Yamaura, I.; Yoshida, Y. Which surgical procedure is effective for refractory chronic subdural hematoma? Analysis of our surgical procedures and literature review. J. Clin. Neurosci. 2018, 49, 40–47. [Google Scholar] [CrossRef] [PubMed]
- de Almeida Monteiro, G.; de Queiroz, T.S.; Gonçalves, O.R.; Cavalcante-Neto, J.F.; Batista, S.; Rabelo, N.N.; Welling, L.C.; Figueiredo, E.G.; Leal, P.R.L.; Solla, D.J.F. Efficacy and Safety of Atorvastatin for Chronic Subdural Hematoma: An Updated Systematic Review and Meta-Analysis. World Neurosurg. 2024, 188, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Link, T.W.; Schwarz, J.T.; Paine, S.M.; Kamel, H.; Knopman, J. Middle Meningeal Artery Embolization for Recurrent Chronic Subdural Hematoma: A Case Series. World Neurosurg. 2018, 118, e570–e574. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Ma, L.; Li, T.; Chen, H. Craniotomy hematoma was removed from the bone flap and multiple holes were drilled on the bone flap A case report. Medicine 2023, 102, e33781. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).