1. Introduction
Bochdalek hernias (BHs) are congenital diaphragmatic defects resulting from an incomplete fusion of the posterolateral diaphragmatic foramina during embryonic development. These hernias typically manifest in the neonatal period with respiratory distress but can occasionally remain asymptomatic until adulthood. The incidence of BHs in adults is approximately 0.17% [
1,
2].
The predominant left-sided laterality of Bochdalek hernias (80–90%) results from the premature closure of the right pleuroperitoneal and the protective effect of the liver [
1,
3,
4]. Adult BHs may be associated with other congenital anomalies—such as intestinal malrotation—further complicating the clinical picture [
3,
5].
The clinical presentation of BHs in adults is often non-specific and variable. Patients may report intermittent abdominal pain, dyspnea, chest discomfort, or gastroesophageal reflux symptoms. These vague presentations frequently lead to misdiagnosis or delayed diagnosis, as symptoms may be attributed to more common conditions such as chronic obstructive pulmonary disease, gastroesophageal reflux disease, or hiatal hernias. This diagnostic challenge necessitates a high degree of clinical suspicion to prevent complications such as bowel obstruction, strangulation, or respiratory compromise [
6,
7].
Computed tomography (CT) is the gold standard for diagnosing adult Bochdalek hernias, providing detailed visualization of the diaphragmatic defect and herniated abdominal contents [
1,
7]. While magnetic resonance imaging (MRI) and chest radiography may be helpful, they generally offer less definitive information. Ramspott et al. conducted the largest systematic review of adult BH repairs, emphasizing the critical role of CT imaging in both diagnosis and surgical planning [
3].
Surgical repair remains the definitive treatment for symptomatic BHs. Historically, open surgical techniques have dominated management; however, since approximately 2012, there has been a significant transition toward minimally invasive approaches. Laparoscopic and thoracoscopic techniques offer several advantages, including reduced postoperative pain, shorter hospital stays, and faster recovery times. Despite these benefits, some studies suggest that minimally invasive approaches—particularly when using mesh reinforcements—may have higher recurrence rates compared to open surgery [
3,
4].
Surgical repair typically involves reducing the herniated contents, excising any hernia sac present, and closing the diaphragmatic defect. In many cases, reinforcement with a mesh is recommended to strengthen the repair and reduce recurrence risk. Dual-layer mesh configurations are often preferred to minimize adhesions or erosions of the adjacent viscera, thereby enhancing the durability of the repair [
3,
7,
8,
9].
2. Case Presentation
A 42-year-old Israeli male mathematics teacher with a smoking history presented to the emergency department with acute, diffuse abdominal pain lasting 3 h, most pronounced in the epigastrium. He reported a several-year history of episodic bloating, crampy abdominal pain, occasional chest pain, and shortness of breath, but denied nausea, vomiting, or fever. He had no significant medical history and was not on any regular medications.
Upon examination, the patient was diaphoretic and tachycardic (120 beats per minute) but normotensive (120/80 mmHg) with oxygen saturation of 95% on room air. Abdominal examination revealed tenderness in the left upper quadrant without peritoneal signs. Lung auscultation demonstrated slightly decreased breath sounds on the left side. The electrocardiogram showed normal sinus rhythm with low-voltage QRS complexes, and a chest radiograph revealed an air–fluid level above the diaphragm without free air beneath it.
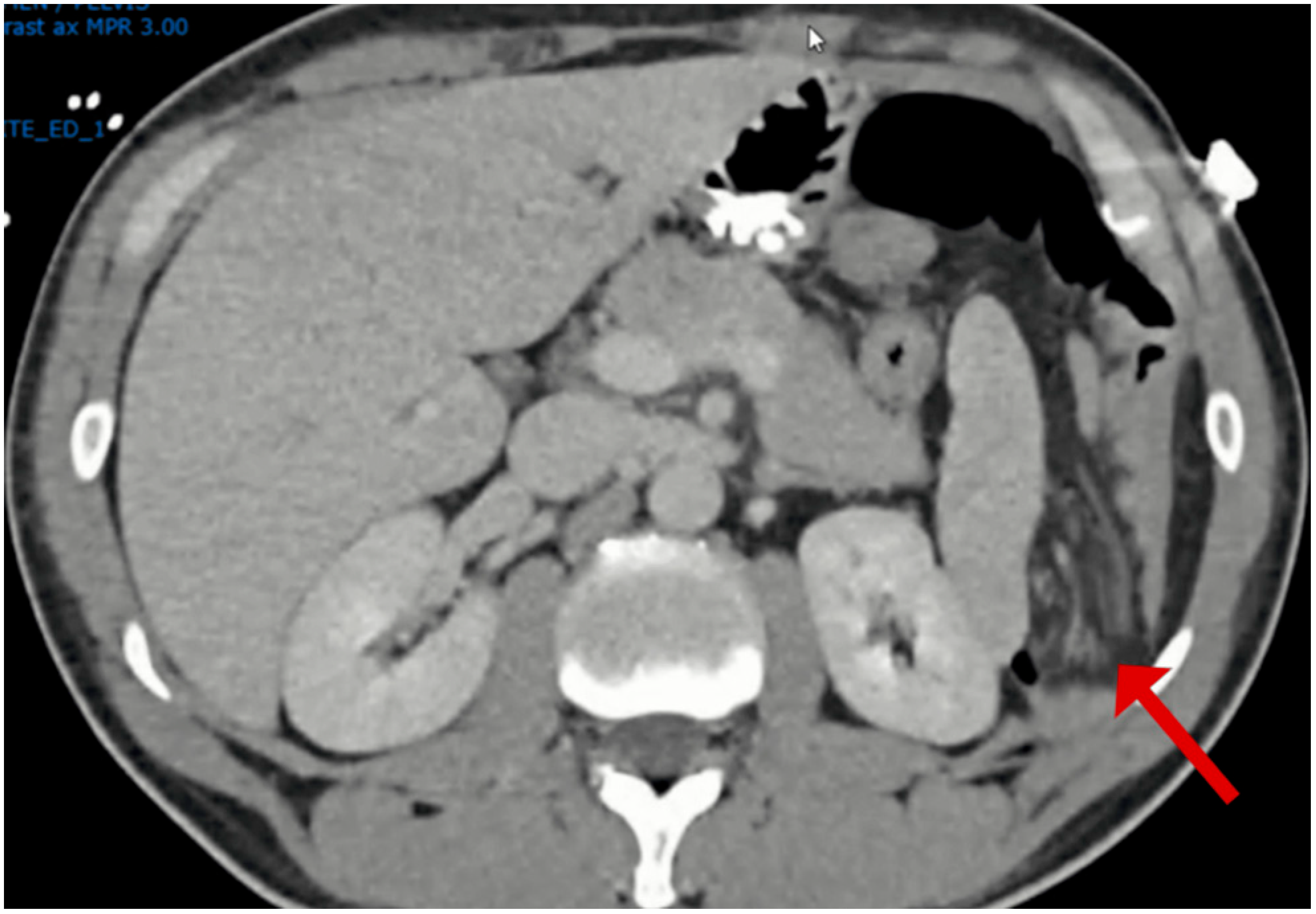
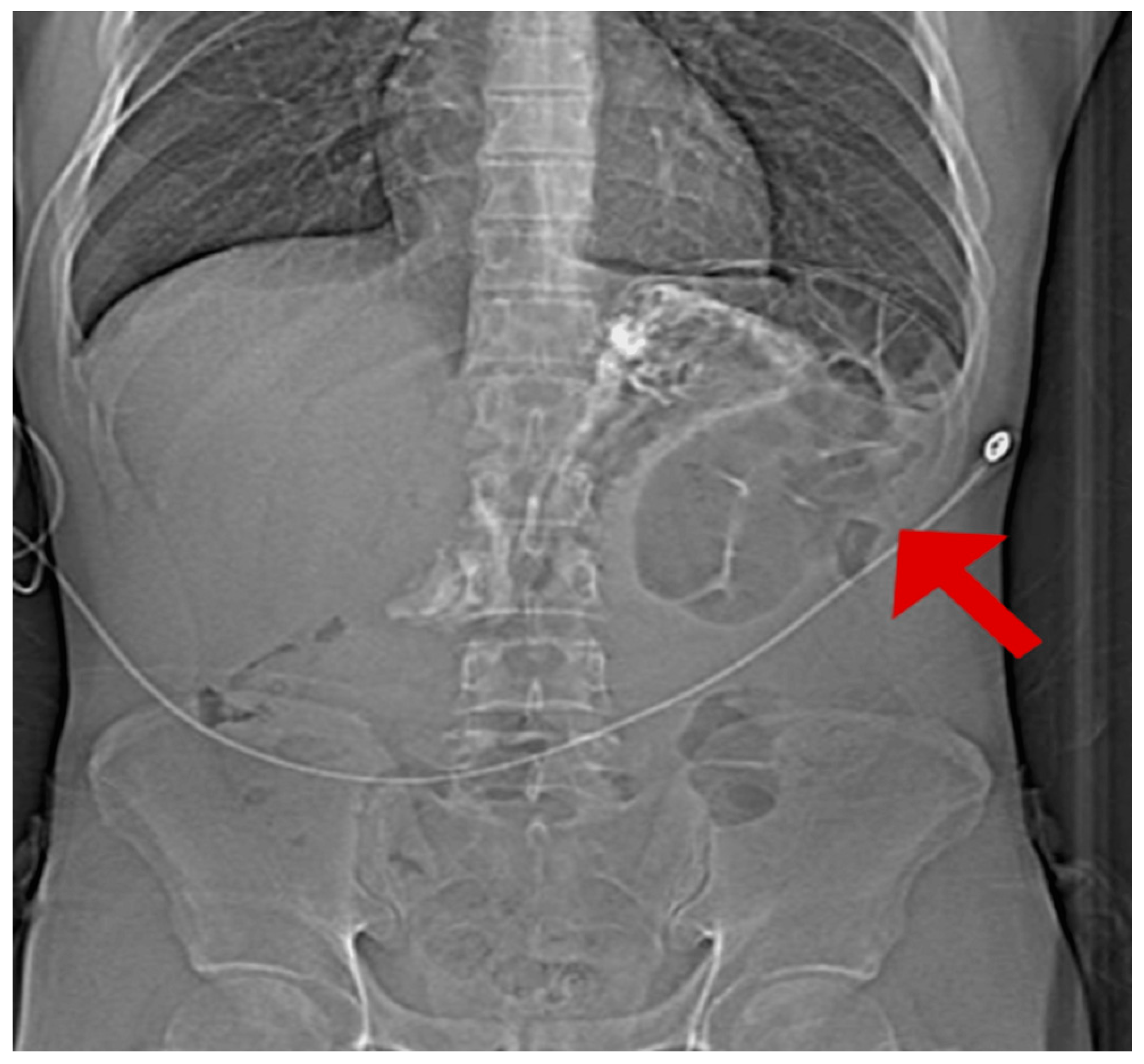
Given the initial suspicion of a perforated peptic ulcer, a non-contrast computed tomography (CT) scan was performed. This revealed a left-sided Bochdalek hernia with small bowel protrusion and signs of strangulation (
Figure 1,
Figure 2,
Figure 3 and
Figure 4).
The patient underwent emergency laparoscopic surgery. He was positioned in the right lateral decubitus position with a 10 mm trocar inserted in the left periumbilical region, supplemented by three additional 5 mm ports. Upon exploration, approximately 1.5 m of strangulated small bowel was found herniated through a posterior diaphragmatic defect. The bowel was gently reduced using a ‘hand-over-hand’ technique, with two atraumatic graspers coordinating traction with expiration to minimize diaphragmatic interference. The right lateral decubitus positioning allowed gravity to assist reduction once the bowel was freed from the hernia ring. Following complete reduction, the bowel showed no signs of ischemia or necrosis after reperfusion (
Figure 5).
A 5 cm posterior diaphragmatic defect was identified with no hernia sac present. The defect was closed primarily with non-absorbable sutures and reinforced with a dual-layer Symbotex mesh.
2.1. Investigations
The diagnosis was established through imaging and laboratory studies. The initial chest radiograph showed an air–fluid level above the left hemidiaphragm, followed by a non-contrast CT (
Figure 6).
Laboratory investigations showed values consistent with an inflammatory response to bowel strangulation (
Table 1).
Laboratory investigations performed at presentation show mild leukocytosis and respiratory alkalosis, consistent with an inflammatory response to bowel strangulation. Abbreviations used are as follows: μL = microliter; g/dL = grams per deciliter; mEq/L = milliequivalents per liter; mg/dL = milligrams per deciliter; pH = potential of hydrogen (measure of acidity/alkalinity); pO2 = partial pressure of oxygen; pCO2 = partial pressure of carbon dioxide; mmHg = millimeters of mercury. The increased white blood cell count indicates an acute inflammatory response, while the slightly elevated pH with decreased pCO2 suggests respiratory alkalosis, likely due to tachypnea secondary to pain and respiratory compromise from the diaphragmatic hernia.
2.2. Differential Diagnosis
A perforated peptic ulcer initially seemed plausible due to the acute abdominal pain and referred shoulder pain; however, the absence of free air beneath the diaphragm on radiography made this diagnosis less likely.
Acute mesenteric ischemia, though consistent with acute abdominal pain, was less probable considering the patient’s young age and lack of relevant cardiovascular risk factors. The clinical presentation helped prioritize our differential diagnosis. The severe epigastric pain radiating to the left shoulder, isolated epigastric tenderness, and retching without productive vomiting suggested diaphragmatic irritation rather than mesenteric ischemia. The absence of atrial fibrillation on ECG, normal lactate levels, and, most importantly, the chest radiograph and non-contrast CT demonstrating a herniated bowel with mechanical closed-loop obstruction made mesenteric thrombosis less likely. While the strangulated, incarcerated bowel could produce ischemic-type pain, the imaging findings of mechanical obstruction without pneumatosis intestinalis, portal venous gas, or bowel wall thickening effectively excluded primary mesenteric vascular occlusion.
Cardiac ischemia entered the differential due to the chest discomfort and tachycardia but was effectively ruled out by the normal ECG findings and predominantly abdominal nature of the pain. Aortic dissection or aneurysm rupture and pneumothorax were also considered given the severity of presentation but were excluded based on clinical and imaging findings. Necrotizing pancreatitis was ruled out based on the absence of typical CT findings and normal serum markers.
A complicated hiatal hernia represented a more challenging diagnostic consideration, as it could potentially present with similar symptoms and radiographic findings. However, the CT scan definitively identified the posterior diaphragmatic defect characteristic of a Bochdalek hernia, with a herniated small bowel demonstrating signs of strangulation, which was ultimately confirmed during surgical intervention.
The elevated white blood cell count and respiratory alkalosis evident in the laboratory studies further supported the diagnosis of Bochdalek hernia with bowel strangulation, representing an inflammatory response to compromised bowel perfusion and tachypnea secondary to both pain and mechanical respiratory compromise from thoracic displacement of abdominal contents.
Given the acute presentation with severe, unrelenting pain and clear evidence of a complicated diaphragmatic hernia, immediate intervention was indicated. The diagnostic and therapeutic approaches focused on ruling out these life-threatening emergencies before proceeding with urgent surgical exploration.
2.3. Treatment
Following diagnosis, the patient underwent emergency laparoscopic repair. The patient’s hemodynamic stability and definitive preoperative diagnosis permitted this minimally invasive approach, which some authors have recommended even in acute settings once the relevant conditions are met. The right lateral decubitus positioning was specifically chosen over standard supine laparoscopy based on anatomical considerations, as gravity would displace the abdominal viscera medially and inferiorly in this position, creating a clear operative corridor to the left posterolateral diaphragm. This approach provided superior exposure to the Bochdalek defect location while improving ergonomics for the surgical team, allowing instruments to approach the defect at optimal angles without fighting against gravity, and facilitated safer bowel reduction by allowing the herniated contents to fall naturally into the abdominal cavity once released. The laparoscopic approach provided excellent visualization of the defect and thorough inspection of the reduced bowel, which showed no signs requiring resection. The 5 cm defect was closed with non-absorbable sutures and reinforced with a dual-layer Symbotex mesh, with a 5 cm overlap beyond the defect margins. The use of non-absorbable mesh reinforcement was considered essential given the chronic nature of this congenital defect and its large size, as the benefits of mesh reinforcement in preventing recurrence substantially outweigh the potential risks of adhesions. The dual-layer Symbotex composite mesh features an anti-adhesive ePTFE layer on the visceral side to minimize bowel adhesions, while the parietal side consists of polypropylene, which promotes tissue integration with the diaphragm. The mesh was secured using a combination of intracorporeal non-absorbable sutures placed circumferentially at 2 cm intervals and supplemented with absorbable tacks placed only on the lateral aspect to avoid potential pericardial injury, ensuring complete apposition to the diaphragmatic surface while preventing mesh migration or herniation.
2.4. Outcome and Follow-Up
The patient’s postoperative course was uncomplicated, with a four-day hospital stay. The nasogastric tube was removed on the first postoperative day once oral intake was tolerated.
At the one-month follow-up, the patient reported the complete resolution of his episodic abdominal pain. Subsequent evaluations at six months, one year, and annually thereafter demonstrated continued symptom-free status with no evidence of recurrence at the four-year follow-up. Follow-up assessments were based on clinical evaluation and symptom review without routine imaging surveillance. While some centers advocate for periodic imaging to detect subclinical recurrence, our patient remained completely asymptomatic throughout the follow-up period. We acknowledge that the absence of routine imaging represents a limitation, as small asymptomatic recurrences could potentially be missed without cross-sectional imaging.
3. Discussion
Despite significant advancements in diagnostic imaging and minimally invasive surgical techniques, adult Bochdalek hernias remain a diagnostic challenge due to their subtle and often vague clinical presentations. Patients may present with intermittent, crampy abdominal pain accompanied by respiratory symptoms that can easily be misattributed to more common conditions such as hiatal hernias, chronic obstructive pulmonary disease, or cardiac ischemia.
The predominant left-sided laterality of Bochdalek hernias (80–90%), as observed in our patient, results from earlier right pleuroperitoneal canal closure and the liver’s protective effect [
1,
2]. Ramspott et al.’s systematic review identified only 44 adult right-sided cases between 2004 and 2021, emphasizing their rarity [
3]. While right-sided hernias show a female predominance in middle-aged patients [
3], left-sided hernias demonstrate more equal gender distribution. Most adult Bochdalek hernias present with chronic, non-specific symptoms that can persist for years before diagnosis [
3,
4,
5], contrasting with our patient’s acute presentation requiring emergency intervention.
The clinical presentation of Bochdalek hernias varies considerably. While many adult cases are asymptomatic and discovered incidentally, symptomatic patients often present with abdominal pain, dyspnea, or chest discomfort [
4,
5]. Goh et al. highlighted that the presentation of right-sided hernias may be particularly subtle due to the protective effect of the liver, leading to delayed diagnosis [
5]. In contrast, our patient with a left-sided hernia presented with acute symptoms, which facilitated prompt diagnosis and treatment. This acute presentation with signs of bowel obstruction necessitated emergency intervention, consistent with findings reported by Ramspott et al. in their case of a complicated right-sided Bochdalek hernia [
3,
6].
Diagnostically, contrast-enhanced CT remains the gold standard for identifying adult Bochdalek hernias, with excellent sensitivity and specificity for delineating the diaphragmatic defect and herniated contents [
3,
7]. Sandstrom and Stern reported that CT can achieve sensitivity of 98% and specificity of 99% in detecting diaphragmatic hernias, making it the preferred initial cross-sectional imaging modality [
10]. In our case, CT imaging clearly demonstrated the left-sided diaphragmatic hernia with signs of bowel strangulation, guiding our subsequent surgical approach.
While chest radiography provided initial clues with an air–fluid level above the diaphragm, its sensitivity is limited for diaphragmatic hernias. Iochum et al. found that conventional radiography detects only 30–40% of diaphragmatic hernias, with high rates of misdiagnosis or delayed diagnosis [
11]. Niwa et al. further emphasized this diagnostic challenge, reporting a case where multiple imaging modalities were required to establish a definitive diagnosis of a Bochdalek hernia in an adult [
12]. Their findings align with our experience, where the initial chest radiograph was suggestive but not definitive, emphasizing the critical role of cross-sectional imaging in achieving an accurate diagnosis.
Regarding surgical management, various approaches have been described for the repair of Bochdalek hernias, including open (thoracotomy or laparotomy) and minimally invasive (thoracoscopic or laparoscopic) techniques. Moro et al. emphasized that the surgical approach should be tailored to the individual case, considering factors such as hernia content, the presence of strangulation, and surgeon expertise [
7]. Increasingly, minimally invasive approaches are preferred due to reduced surgical trauma and faster recovery [
8,
9].
Our case featured the following two distinctive aspects of surgical management that warrant discussion in light of the existing literature:
Laparoscopic Approach for Acute Presentation with Strangulation: The decision to proceed with a laparoscopic approach despite the acute presentation with bowel strangulation represents an evolution in the surgical management of complicated Bochdalek hernias. Traditionally, open approaches were favored in acute settings, particularly with suspected bowel compromise. However, our successful laparoscopic management demonstrates the feasibility and efficacy of minimally invasive techniques even in emergency scenarios. Patle et al. similarly reported successful laparoscopic repair of a right-sided Bochdalek hernia, emphasizing the advantages of minimal surgical trauma and quicker recovery [
8]. However, their case did not involve bowel strangulation, making our approach more novel for this particular presentation.
Right Lateral Decubitus Positioning for Left-Sided Defect: The use of right lateral decubitus positioning for the repair of a left-sided Bochdalek hernia represents an innovative technical modification that has not been extensively described in the literature. This positioning strategy allowed gravity to aid in the visualization of and access to the posterolateral diaphragmatic defect, facilitating a more ergonomic approach to the repair. Most reported cases use standard positioning for either thoracoscopic or laparoscopic approaches. Ver et al. described the successful minimally invasive repair of a right-sided diaphragmatic hernia but did not specifically address positioning considerations [
9]. Our experience suggests that this positioning strategy may offer significant advantages for left-sided defects, particularly when bowel reduction and thorough inspection are necessary.
The surgical technique of primary closure with mesh reinforcement employed in our case aligns with contemporary approaches described in the literature. Rosen et al. advocated for the use of mesh in their report of laparoscopic repair of a right-sided Bochdalek hernia, noting the importance of adequate reinforcements to prevent recurrence [
13]. Similarly, Enomoto et al. described the successful repair of a right-sided defect using mesh, though their approach was open rather than laparoscopic [
14]. Palanivelu et al. provided more substantial evidence supporting this approach in their retrospective study of nine adult patients with diaphragmatic hernias repaired laparoscopically with mesh reinforcement, reporting no recurrences at a mean follow-up of 58 months [
15]. Their findings suggest that primary closure with prosthetic reinforcement offers superior long-term outcomes compared to primary suture repair alone, particularly for defects larger than 3 cm, as in our case.
The use of lateral positioning for diaphragmatic hernia repair has been reported in limited cases in the literature. Julien et al. described the successful use of right lateral positioning for laparoscopic repair of a left-sided Bochdalek hernia in a pregnant patient, demonstrating that this positioning strategy facilitates the procedure by improving surgical access and visualization [
16]. They noted that this positioning strategy significantly improved surgical ergonomics and facilitated better exposure of the diaphragmatic defect—observations that parallel our experience with the opposite laterality. The authors emphasized that lateral positioning allowed gravity to assist in visualization by causing the abdominal viscera to fall away from the surgical field, a principle we successfully applied in our left-sided case.
We think that, briefly, our case demonstrates several unique decision-making aspects that differentiate it from the previously reported cases. First, the combination of acute presentation with bowel strangulation and the choice of a minimally invasive approach represents a departure from traditional management algorithms that often favor open surgery in emergency settings. Second, our use of right lateral decubitus positioning for a left-sided Bochdalek hernia in the specific context of acute bowel strangulation—while lateral positioning has been described for traumatic diaphragmatic hernias—represents a novel application of this technique for congenital defects with acute complications [
9]. Third, our decision to proceed with primary repair despite the acute inflammatory changes, rather than staging the procedure, was based on the viable appearance of the reduced bowel and absence of contamination. These decisions collectively demonstrate how individualized surgical planning based on real-time assessment can optimize outcomes, even in challenging acute presentations.
Our patient’s excellent outcome, with the complete resolution of symptoms and no recurrence at the 4-year follow-up adds to the growing body of evidence supporting minimally invasive approaches for Bochdalek hernia repair. Machado conducted a comprehensive review of laparoscopic repair techniques for Bochdalek hernias in adults, demonstrating shorter hospital stays and fewer complications compared to open surgery [
17]. Our case provides further support for these findings, even in the context of a complicated presentation with bowel strangulation.
The successful management of our patient without the need for bowel resection highlights the importance of timely diagnosis and intervention. Despite the presence of strangulation, the herniated bowel showed no signs of ischemia or necrosis after reduction, enabling the preservation of the entire small bowel. This contrasts with the case reported by Ramspott et al., where intrathoracic bowel perforation necessitated right-sided hemicolectomy and anastomosis [
6]. This difference may be attributed to earlier diagnosis and intervention in our case, or possibly to differences in the pattern of vascular compromise between the left- and right-sided hernias.
In summary, despite modern imaging and surgical advancements, the diagnosis of adult Bochdalek hernias remains challenging due to their subtle symptomatology and anatomical nuances. Our case—featuring a left-sided Bochdalek hernia with bowel strangulation successfully managed via laparoscopy with right lateral decubitus positioning—contributes valuable insights to the existing literature. It reinforces the imperative to maintain a high index of suspicion in patients with combined gastro-respiratory complaints and to adopt an aggressive diagnostic and minimally invasive surgical approach when indicated. The innovative positioning strategy employed may represent a technical refinement worth considering in similar cases. Furthermore, our long-term follow-up confirms the durability of minimally invasive repair with mesh reinforcement, with no evidence of recurrence at 4 years postoperatively.
Based on our experience and review of the literature, several factors should guide surgeons in assessing the feasibility of minimally invasive repair in acute Bochdalek hernia presentations. Key considerations include the following: (1) hemodynamic stability of the patient; (2) clear-cut preoperative diagnosis that eliminates the need for diagnostic laparoscopy of other abdominal quadrants; (3) absence of bowel perforation or contamination on imaging; (4) duration of symptoms suggesting viability of herniated contents; and (5) surgeon experience with advanced laparoscopic techniques. Technical expertise requirements include proficiency in laparoscopic suturing, experience with mesh placement in the diaphragmatic position, and the ability to convert to open surgery if needed. We recommend that surgeons attempting this approach have substantial experience with advanced laparoscopic procedures and specific familiarity with diaphragmatic repairs. The learning curve can be mitigated by appropriate patient selection, with stable patients and smaller defects being ideal initial cases.