Maternal and Neonatal Outcomes of Cervical Colonization in Adolescent Pregnancies: A Brief Report
Abstract
1. Introduction
2. Methodology
3. Statistical Analyses
4. Results
4.1. General Characteristics
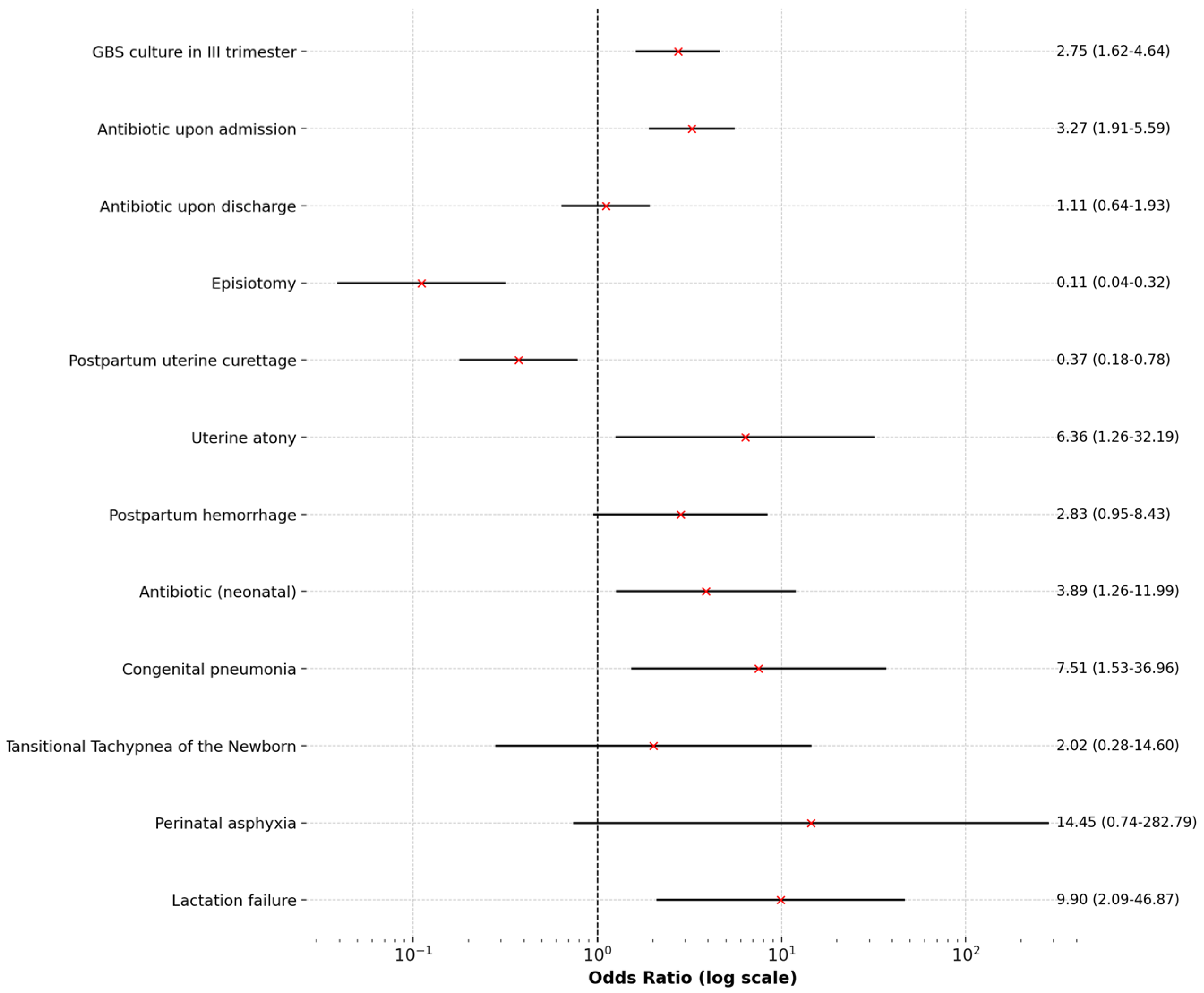
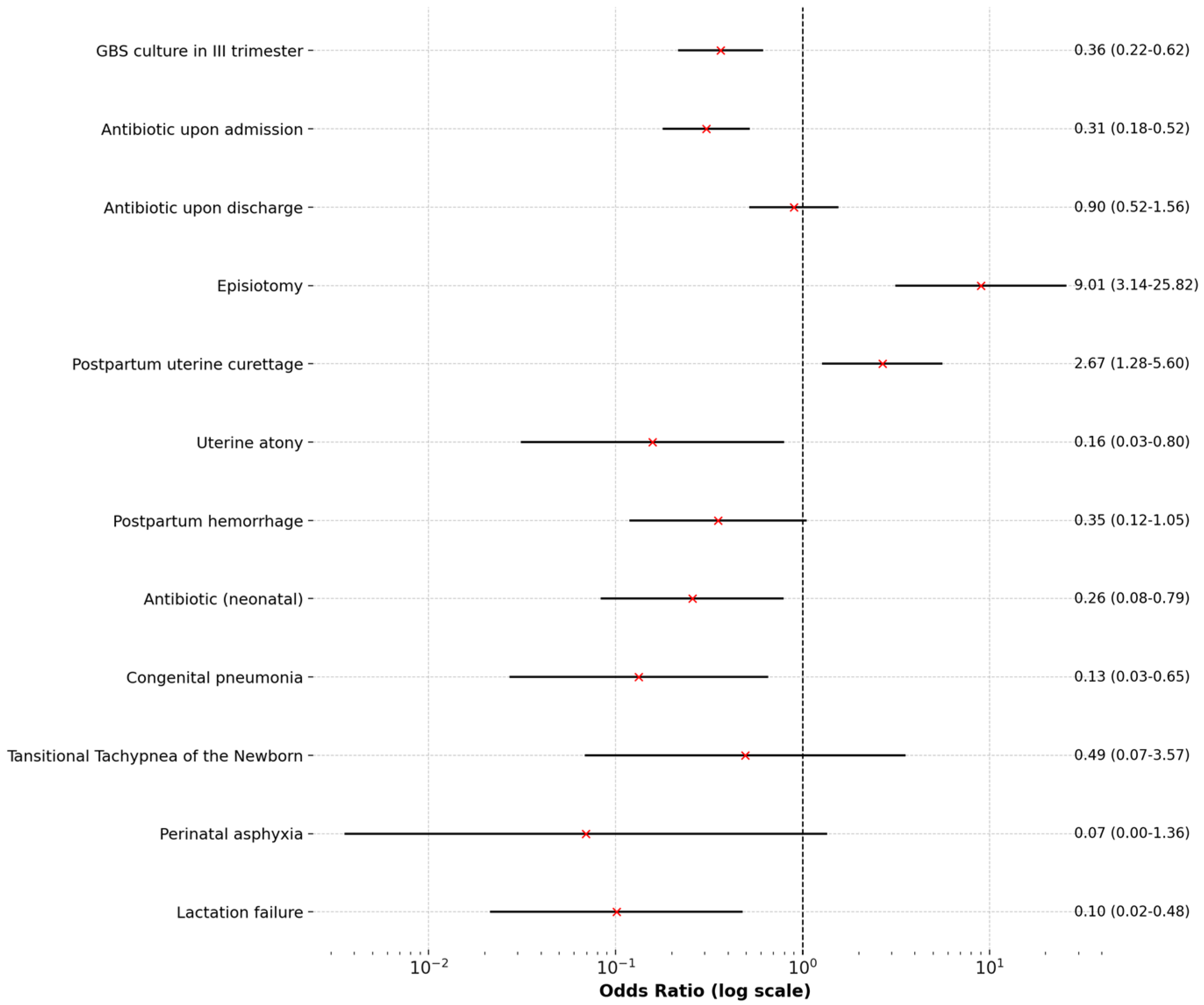
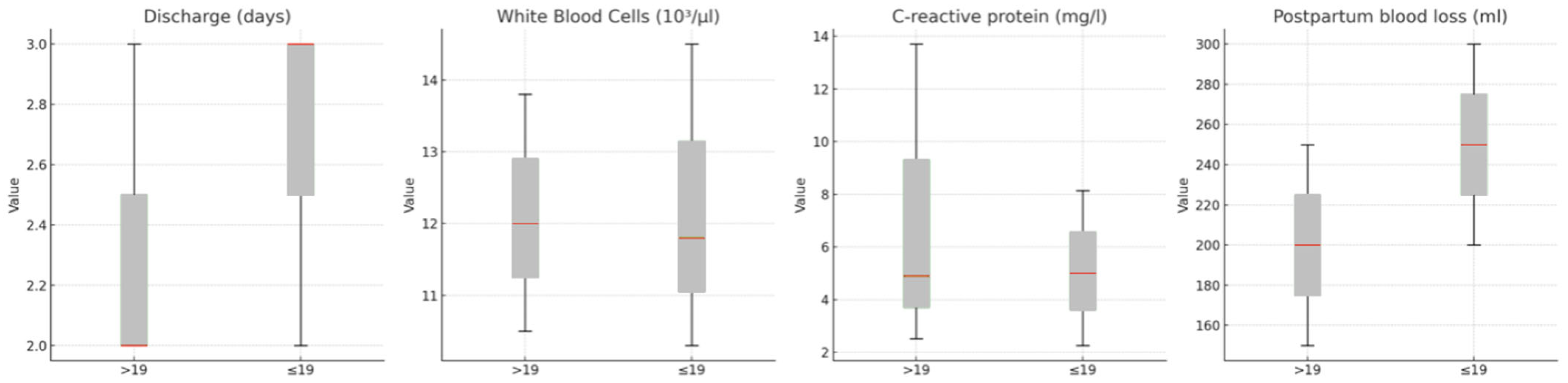
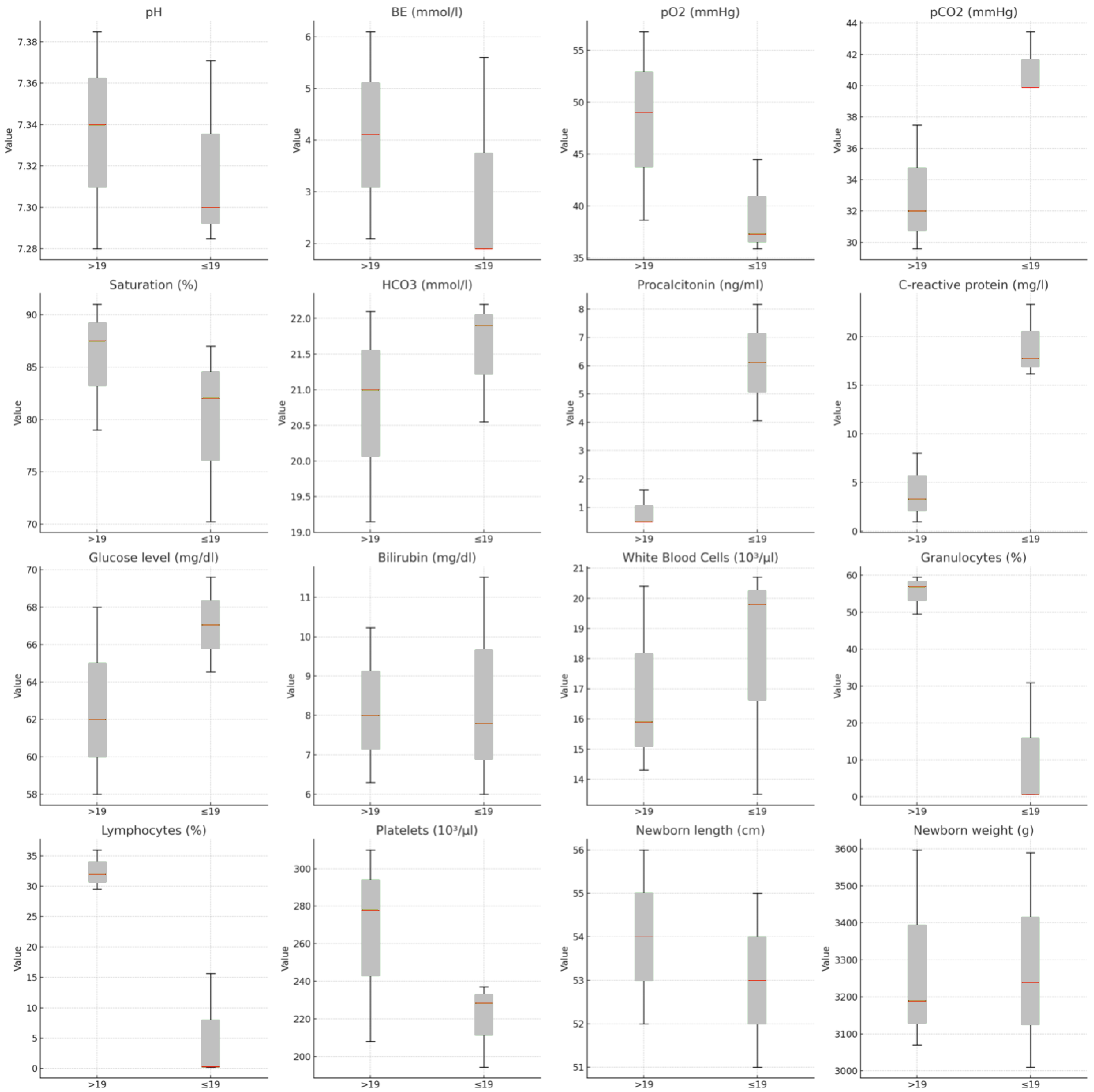
4.2. Comparison Between Groups
5. Discussion
6. Clinical Implications
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Staniczek, J.; Manasar-Dyrbuś, M.; Stojko, R.; Jendyk, C.; Sadłocha, M.; Winkowska, E.; Orszulak, D.; Niziński, K.; Skowronek, K.; Toczek, J.; et al. Adolescent Pregnancy: A Comparative Insight into the Prevalence and Risks of Obstetric Complications in a Polish Cohort. J. Clin. Med. 2024, 13, 5785. [Google Scholar] [CrossRef] [PubMed]
- Akoh, C.C.; Pressman, E.K.; Cooper, E.; Queenan, R.A.; Pillittere, J.; O’Brien, K.O. Prevalence and Risk Factors for Infections in a Pregnant Adolescent Population. J. Pediatr. Adolesc. Gynecol. 2016, 30, 71–75. [Google Scholar] [CrossRef] [PubMed]
- de Azevedo, W.F.; Diniz, M.B.; da Fonseca, E.S.V.B.; de Azevedo, L.M.R.; Evangelista, C.B. Complications in adolescent pregnancy: Systematic review of the literature. Einstein 2015, 13, 618–626. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Çift, T.; Korkmazer, E.; Temur, M.; Bulut, B.; Korkmaz, B.; Ozdenoğlu, O.; Akaltun, C.; Üstünyurt, E. Adolescent pregnancies: Complications, birth outcomes and the possible solutions. Ginekol. Pol. 2017, 88, 393–397. [Google Scholar] [CrossRef] [PubMed]
- Staniczek, J.; Manasar-Dyrbuś, M.; Rybak-Krzyszkowska, M.; Kondracka, A.; Orszulak, D.; Niziński, K.; Sadłocha, M.; Drosdzol-Cop, A.; Stojko, R.; Illa, M. Systematic review and meta-analysis of the association between young maternal age and fetal abnormalities. Sci. Rep. 2024, 14, 22562. [Google Scholar] [CrossRef]
- Drosdzol-Cop, A.; Staniczek, J.; Orszulak, D.; Kowalczyk, K.; Fuchs, A.; Sieroszewski, P.; Wielgos, M.; Kalinka, J.; Huras, H.; Wegrzyn, P.; et al. The Polish Society of Gynecologists and Obstetricians’ Expert Group Recommendations regarding adolescent pregnancy. Ginekol. Pol. 2023, 94, 258–267. [Google Scholar] [CrossRef] [PubMed]
- Diabelková, J.; Rimárová, K.; Dorko, E.; Urdzík, P.; Houžvičková, A.; Argalášová, Ľ. Adolescent Pregnancy Outcomes and Risk Factors. Int. J. Environ. Res. Public Health 2023, 20, 4113. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- La Rosa, V.L.; Geraci, A.; Iacono, A.; Commodari, E. Affective Touch in Preterm Infant Development: Neurobiological Mechanisms and Implications for Child–Caregiver Attachment and Neonatal Care. Children 2024, 11, 1407. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Leftwich, H.K.; Alves, M.V.O. Adolescent Pregnancy. Pediatr. Clin. N. Am. 2017, 64, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Amjad, S.; Chandra, S.; Osornio-Vargas, A.; Voaklander, D.; Ospina, M.B. Maternal Area of Residence, Socioeconomic Status, and Risk of Adverse Maternal and Birth Outcomes in Adolescent Mothers. J. Obstet. Gynaecol. Can. 2019, 41, 1752–1759. [Google Scholar] [CrossRef] [PubMed]
- Govender, T.; Reddy, P.; Ghuman, S. Obstetric outcomes and antenatal access among adolescent pregnancies in KwaZulu-Natal, South Africa. S. Afr. Fam. Pract. 2017, 60, 1–7. [Google Scholar] [CrossRef]
| Variable | >19 | ≤19 | p-Value | |
|---|---|---|---|---|
| n | 178 | 89 | ||
| GBS positive culture in III trimester | 68 (38.20%) | 56 (62.92%) | <0.001 | |
| Cultured pathogens | ||||
| Candida albicans | 112 (62.92%) | 65 (73.03%) | 0.131 | |
| Candida glabrata | 14 (7.87%) | 4 (4.49%) | 0.437 | |
| Candida tropicalis | 1 (0.56%) | 0 (0.00%) | 1 | |
| Candida crusei | 0 (0.00%) | 1 (1.12%) | 0.723 | |
| Streptococcus agalactiae | 62 (34.83%) | 32 (35.96%) | 0.964 | |
| Staphylococcus aureus | 20 (11.24%) | 8 (8.99%) | 0.724 | |
| Enterococcus faecalis | 0 (0.00%) | 3 (3.37%) | 0.065 | |
| Escherichia coli | 0 (0.00%) | 3 (3.37%) | 0.065 | |
| Antibiotic therapy | ||||
| Antibiotic | 69 (38.76%) | 60 (67.42%) | <0.001 | |
| Type of antibiotic | Amoxicillin | 3 (4.29%) | 7 (11.11%) | 0.003 |
| Ampicillin | 57 (81.43%) | 33 (52.38%) | ||
| Clindamycin | 10 (14.29%) | 20 (31.75%) | ||
| None | 0 (0.00%) | 3 (4.76%) | ||
| Antibiotic upon discharge | 52 (29.21%) | 28 (31.46%) | 0.813 | |
| Antibiotic upon discharge | Amoxicillin | 51 (92.73%) | 24 (85.00%) | 0.023 |
| Clindamycin | 4 (7.27%) | 4 (25.00%) | ||
| Labor complications | ||||
| Episiotomy | 53 (29.78%) | 4 (4.49%) | <0.001 | |
| Postpartum uterine curettage | 45 (25.28%) | 10 (11.24%) | 0.012 | |
| Uterine atony | 2 (1.12%) | 6 (6.74%) | 0.031 | |
| Postpartum hemorrhage | 6 (3.37%) | 8 (8.99%) | 0.099 | |
| Neonatal outcomes | ||||
| nCPAP | 4 (100.00%) | 3 (33.33%) | 0.105 | |
| Antibiotic | 5 (2.81%) | 9 (10.11%) | 0.026 | |
| Congenital pneumonia | 2 (1.12%) | 7 (7.87%) | 0.012 | |
| Tansitional Tachypnea of the Newborn | 2 (1.12%) | 2 (2.25%) | 0.859 | |
| Perinatal asphyxia | 0 (0.00%) | 3 (3.37%) | 0.065 | |
| Lactation failure | 2 (1.12%) | 9 (10.11%) | 0.002 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manasar-Dyrbuś, M.; Staniczek, J.; Stojko, R.; Gibała, P.; Jendyk, C.; Winkowska, E.; Niziński, K.; Sieroszewska, D.; Sieroszewski, A.; Drosdzol-Cop, A. Maternal and Neonatal Outcomes of Cervical Colonization in Adolescent Pregnancies: A Brief Report. Pediatr. Rep. 2025, 17, 36. https://doi.org/10.3390/pediatric17020036
Manasar-Dyrbuś M, Staniczek J, Stojko R, Gibała P, Jendyk C, Winkowska E, Niziński K, Sieroszewska D, Sieroszewski A, Drosdzol-Cop A. Maternal and Neonatal Outcomes of Cervical Colonization in Adolescent Pregnancies: A Brief Report. Pediatric Reports. 2025; 17(2):36. https://doi.org/10.3390/pediatric17020036
Chicago/Turabian StyleManasar-Dyrbuś, Maisa, Jakub Staniczek, Rafał Stojko, Piotr Gibała, Cecylia Jendyk, Ewa Winkowska, Kacper Niziński, Diana Sieroszewska, Aleksander Sieroszewski, and Agnieszka Drosdzol-Cop. 2025. "Maternal and Neonatal Outcomes of Cervical Colonization in Adolescent Pregnancies: A Brief Report" Pediatric Reports 17, no. 2: 36. https://doi.org/10.3390/pediatric17020036
APA StyleManasar-Dyrbuś, M., Staniczek, J., Stojko, R., Gibała, P., Jendyk, C., Winkowska, E., Niziński, K., Sieroszewska, D., Sieroszewski, A., & Drosdzol-Cop, A. (2025). Maternal and Neonatal Outcomes of Cervical Colonization in Adolescent Pregnancies: A Brief Report. Pediatric Reports, 17(2), 36. https://doi.org/10.3390/pediatric17020036








