Sterile Cerebrospinal Fluid Culture at Cryptococcal Meningitis Diagnosis Is Associated with High Mortality
Abstract
:1. Introduction
2. Materials and Methods
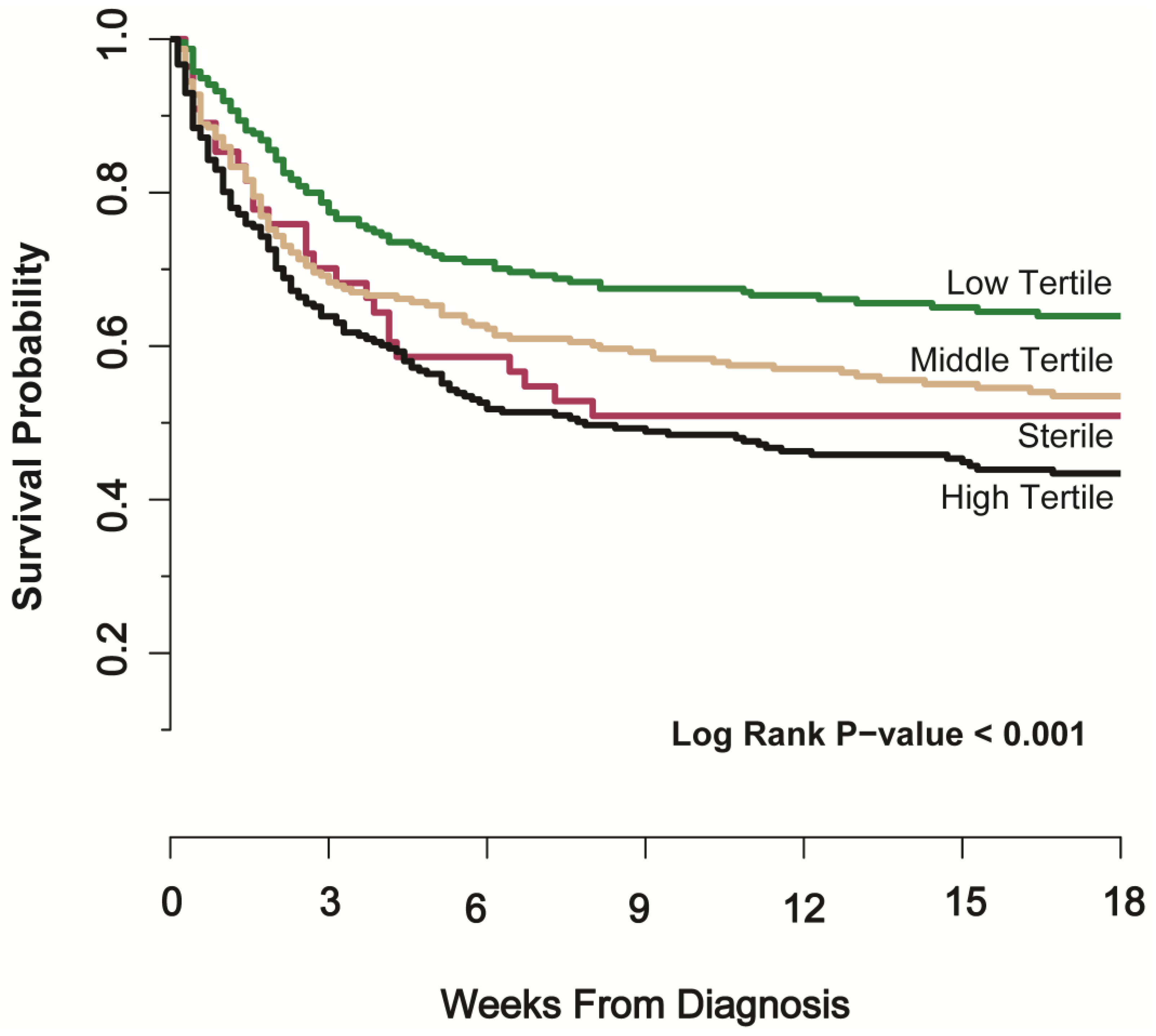
3. Results
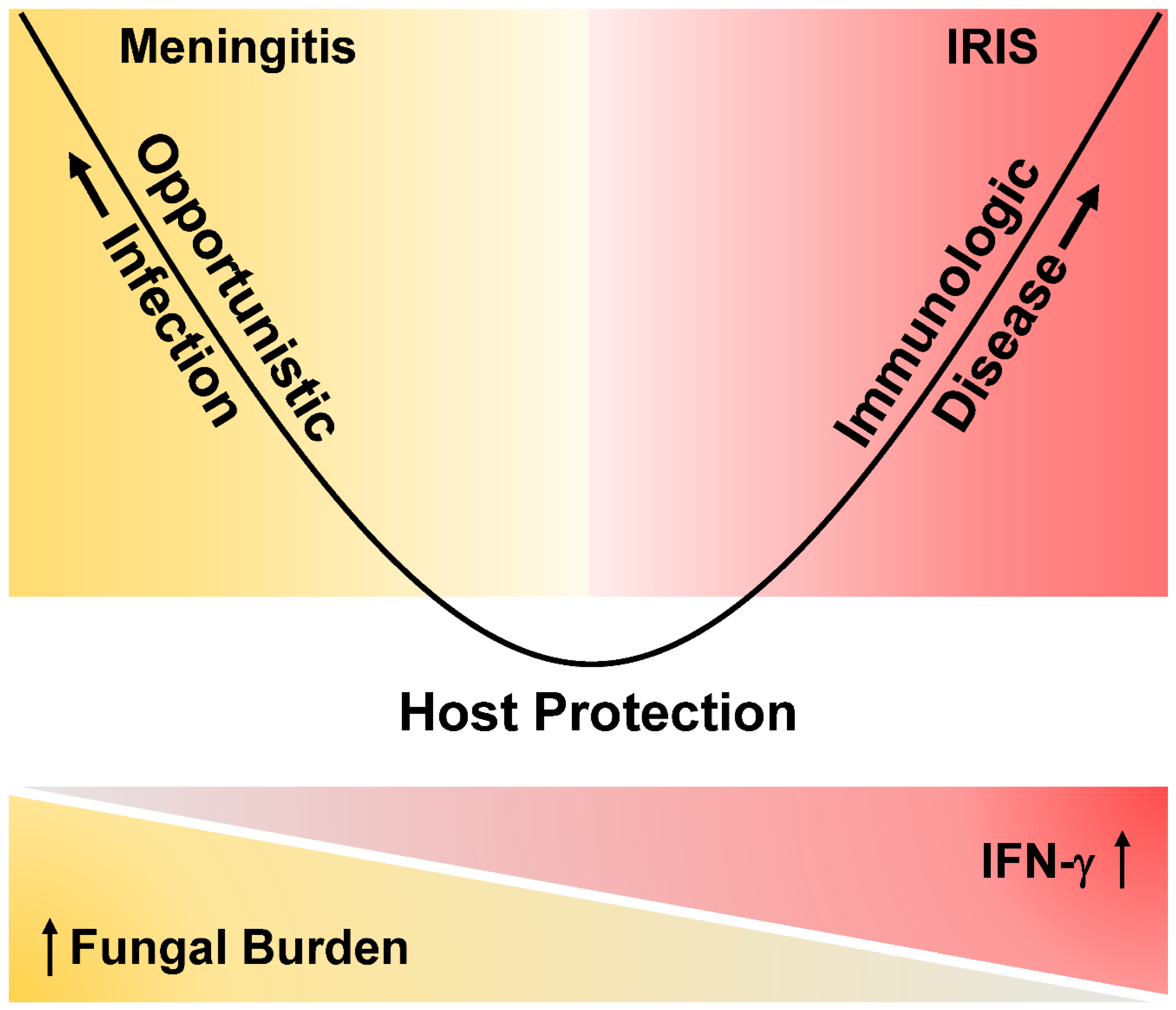
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Durski, K.N.; Kuntz, K.M.; Yasukawa, K.; Virnig, B.A.; Meya, D.B.; Boulware, D.R. Cost-effective diagnostic checklists for meningitis in resource-limited settings. J. Acquir. Immune Defic. Syndr. 2013, 63, e101–e108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ellis, J.; Bangdiwala, A.S.; Cresswell, F.V.; Rhein, J.; Nuwagira, E.; Ssebambulidde, K.; Tugume, L.; Rajasingham, R.; Bridge, S.C.; Muzoora, C.; et al. The Changing Epidemiology of HIV-Associated Adult Meningitis, Uganda 2015–2017. Open Forum Infect. Dis. 2019, 6, ofz419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajasingham, R.; Govender, N.P.; Jordan, A.; Loyse, A.; Shroufi, A.; Denning, D.W.; Meya, D.B.; Chiller, T.M.; Boulware, D.R. The global burden of HIV-associated cryptococcal infection in adults in 2020: A modelling analysis. Lancet Infect. Dis. 2022, 22, 1748–1755. [Google Scholar] [CrossRef]
- Boulware, D.R.; Rolfes, M.A.; Rajasingham, R.; von Hohenberg, M.; Qin, Z.; Taseera, K.; Schutz, C.; Kwizera, R.; Butler, E.K.; Meintjes, G.; et al. Multisite validation of cryptococcal antigen lateral flow assay and quantification by laser thermal contrast. Emerg. Infect. Dis. 2014, 20, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Jarvis, J.N.; Bicanic, T.; Loyse, A.; Namarika, D.; Jackson, A.; Nussbaum, J.C.; Longley, N.; Muzoora, C.; Phulusa, J.; Taseera, K.; et al. Determinants of mortality in a combined cohort of 501 patients with HIV-associated Cryptococcal meningitis: Implications for improving outcomes. Clin. Infect. Dis. 2014, 58, 736–745. [Google Scholar] [CrossRef]
- Carmona, S.; Bor, J.; Nattey, C.; Maughan-Brown, B.; Maskew, M.; Fox, M.P.; Glencross, D.K.; Ford, N.; MacLeod, W.B. Persistent High Burden of Advanced HIV Disease Among Patients Seeking Care in South Africa’s National HIV Program: Data From a Nationwide Laboratory Cohort. Clin. Infect. Dis. 2018, 66, S111–S117. [Google Scholar] [CrossRef] [Green Version]
- Rhein, J.; Hullsiek, K.H.; Evans, E.E.; Tugume, L.; Nuwagira, E.; Ssebambulidde, K.; Kiggundu, R.; Mpoza, E.; Musubire, A.K.; Bangdiwala, A.S.; et al. Detrimental Outcomes of Unmasking Cryptococcal Meningitis With Recent ART Initiation. Open Forum Infect. Dis. 2018, 5, ofy122. [Google Scholar] [CrossRef] [Green Version]
- Rhein, J.; Hullsiek, K.H.; Tugume, L.; Nuwagira, E.; Mpoza, E.; E Evans, E.; Kiggundu, R.; A Pastick, K.; Ssebambulidde, K.; Akampurira, A.; et al. Adjunctive sertraline for HIV-associated cryptococcal meningitis: A randomised, placebo-controlled, double-blind phase 3 trial. Lancet Infect. Dis. 2019, 19, 843–851. [Google Scholar] [CrossRef]
- Williams, D.A.; Kiiza, T.; Kwizera, R.; Kiggundu, R.; Velamakanni, S.; Meya, D.B.; Rhein, J.; Boulware, D.R. Evaluation of fingerstick cryptococcal antigen lateral flow assay in HIV-infected persons: A diagnostic accuracy study. Clin. Infect. Dis. 2015, 61, 464–467. [Google Scholar] [CrossRef] [Green Version]
- Boulware, D.R.; Meya, D.B.; Muzoora, C.; Rolfes, M.A.; Hullsiek, K.H.; Musubire, A.; Taseera, K.; Nabeta, H.W.; Schutz, C.; Williams, D.A.; et al. Timing of antiretroviral therapy after diagnosis of cryptococcal meningitis. N. Engl. J. Med. 2014, 370, 2487–2498. [Google Scholar] [CrossRef]
- Rhein, J.; Morawski, B.M.; Hullsiek, K.H.; Nabeta, H.W.; Kiggundu, R.; Tugume, L.; Musubire, A.; Akampurira, A.; Smith, K.D.; Alhadab, A.; et al. Efficacy of adjunctive sertraline for the treatment of HIV-associated cryptococcal meningitis: An open-label dose-ranging study. Lancet Infect. Dis. 2016, 16, 809–818. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dyal, J.; Akampurira, A.; Rhein, J.; Morawski, B.M.; Kiggundu, R.; Nabeta, H.W.; Musubire, A.K.; Bahr, N.C.; A Williams, D.; Bicanic, T.; et al. Reproducibility of CSF quantitative culture methods for estimating rate of clearance in cryptococcal meningitis. Med. Mycol. 2016, 54, 361–369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Butler, E.K.; Boulware, D.R.; Bohjanen, P.R.; Meya, D.B. Long term 5-year survival of persons with cryptococcal meningitis or asymptomatic subclinical antigenemia in Uganda. PLoS ONE 2012, 7, e51291. [Google Scholar] [CrossRef] [Green Version]
- Graybill, J.R.; Sobel, J.; Saag, M.; Van Der Horst, C.; Powderly, W.; Cloud, G.; Riser, L.; Hamill, R.; Dismukes, R.; NIAID Mycoses Study Group; et al. Diagnosis and management of increased intracranial pressure in patients with AIDS and cryptococcal meningitis. The NIAID Mycoses Study Group and AIDS Cooperative Treatment Groups. Clin. Infect. Dis. 2000, 30, 47–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van der Horst, C.M.; Saag, M.S.; Cloud, G.A.; Hamill, R.J.; Graybill, J.R.; Sobel, J.D.; Johnson, P.C.; Tuazon, C.U.; Kerkering, T.; Moskovitz, B.L.; et al. Treatment of cryptococcal meningitis associated with the acquired immunodeficiency syndrome. National Institute of Allergy and Infectious Diseases Mycoses Study Group and AIDS Clinical Trials Group. N. Engl. J. Med. 1997, 337, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Rolfes, M.A.; Hullsiek, K.H.; Rhein, J.; Nabeta, H.W.; Taseera, K.; Schutz, C.; Musubire, A.; Rajasingham, R.; Williams, D.A.; Thienemann, F.; et al. The effect of therapeutic lumbar punctures on acute mortality from cryptococcal meningitis. Clin. Infect. Dis. 2014, 59, 1607–1614. [Google Scholar] [CrossRef] [Green Version]
- Jarvis, J.N.; Meintjes, G.; Bicanic, T.; Buffa, V.; Hogan, L.; Mo, S.; Tomlinson, G.; Kropf, P.; Noursadeghi, M.; Harrison, T.S. Cerebrospinal fluid cytokine profiles predict risk of early mortality and immune reconstitution inflammatory syndrome in HIV-associated cryptococcal meningitis. PLoS Pathog. 2015, 11, e1004754. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boulware, D.R.; Bonham, S.C.; Meya, D.; Wiesner, D.L.; Park, G.S.; Kambugu, A.; Janoff, E.N.; Bohjanen, P. Paucity of initial cerebrospinal fluid inflammation in cryptococcal meningitis is associated with subsequent immune reconstitution inflammatory syndrome. J. Infect. Dis. 2010, 202, 962–970. [Google Scholar] [CrossRef] [Green Version]
- Bicanic, T.; Muzoora, C.; Brouwer, A.E.; Meintjes, G.; Longley, N.; Taseera, K.; Rebe, K.; Loyse, A.; Jarvis, J.; Bekker, L.-G.; et al. Independent association between rate of clearance of infection and clinical outcome of HIV associated cryptococcal meningitis: Analysis of a combined cohort of 262 patients. Clin. Infect. Dis. 2009, 49, 702–709. [Google Scholar] [CrossRef]
- Scriven, J.E.; Rhein, J.; Hullsiek, K.H.; Von Hohenberg, M.; Linder, G.; Rolfes, M.A.; Williams, D.A.; Taseera, K.; Meya, D.B.; Meintjes, G.; et al. Early ART after cryptococcal meningitis is associated with cerebrospinal fluid pleocytosis and macrophage activation in a multisite randomized trial. J. Infect. Dis. 2015, 212, 769–778. [Google Scholar] [CrossRef]
- Rajasingham, R.; Meya, D.B.; Boulware, D.R. Integrating cryptococcal antigen screening and pre-emptive treatment into routine HIV care. J. Acquir. Immune Defic. Syndr. 2012, 59, e85–e91. [Google Scholar] [CrossRef] [Green Version]
- Haddow, L.; Colebunders, R.; Meintjes, G.; Lawn, S.D.; Elliott, J.H.; Manabe, Y.C.; Bohjanen, P.; Sungkanuparph, S.; Easterbrook, P.J.; French, M.; et al. Cryptococcal immune reconstitution inflammatory syndrome in HIV-1-infected individuals: Proposed clinical case definitions. Lancet Infect. Dis. 2010, 10, 791–802. [Google Scholar] [CrossRef] [Green Version]
- Pirofski, L.A.; Casadevall, A. Immune-Mediated Damage Completes the Parabola: Cryptococcus neoformans Pathogenesis Can Reflect the Outcome of a Weak or Strong Immune Response. mBio 2017, 8, e02063-17. [Google Scholar] [CrossRef] [Green Version]
- Pirofski, L.A.; Casadevall, A. The damage-response framework of microbial pathogenesis and infectious diseases. Adv. Exp. Med. Biol. 2008, 635, 135–146. [Google Scholar]
- Wiesner, D.L.; Boulware, D.R. Cryptococcus-Related Immune Reconstitution Inflammatory Syndrome(IRIS): Pathogenesis and Its Clinical Implications. Curr. Fungal Infect. Rep. 2011, 5, 252–261. [Google Scholar] [CrossRef] [Green Version]
- Boulware, D.R.; Meya, D.B.; Bergemann, T.L.; Wiesner, D.L.; Rhein, J.; Musubire, A.; Lee, S.J.; Kambugu, A.; Janoff, E.N.; Bohjanen, P.R. Clinical features and serum biomarkers in HIV immune reconstitution inflammatory syndrome after cryptococcal meningitis: A prospective cohort study. PLoS Med. 2010, 7, e1000384. [Google Scholar] [CrossRef] [Green Version]
- Longley, N.; Harrison, T.S.; Jarvis, J.N. Cryptococcal immune reconstitution inflammatory syndrome. Curr. Opin. Infect. Dis. 2013, 26, 26–34. [Google Scholar] [CrossRef]
- Katchanov, J.; Blechschmidt, C.; Nielsen, K.; Branding, G.; Arastéh, K.; Tintelnot, K.; Meintjes, G.; Boulware, D.R.; Stocker, H. Cryptococcal meningoencephalitis relapse after an eight-year delay: An interplay of infection and immune reconstitution. Int. J. STD AIDS 2015, 26, 912–914. [Google Scholar] [CrossRef] [Green Version]
- Skipper, C.; Abassi, M.; Boulware, D.R. Diagnosis and Management of Central Nervous System Cryptococcal Infections in HIV-Infected Adults. J. Fungi 2019, 5, 65. [Google Scholar] [CrossRef] [Green Version]
- Kalata, N.; Ellis, J.; Kanyama, C.; Kuoanfank, C.; Temfack, E.; Mfinanga, S.; Lesikari, S.; Chanda, D.; Lakhi, S.; Nyazika, T.; et al. Short-term Mortality Outcomes of HIV-Associated Cryptococcal Meningitis in Antiretroviral Therapy-Naïve and -Experienced Patients in Sub-Saharan Africa. Open Forum Infect. Dis. 2021, 8, ofab397. [Google Scholar] [CrossRef]
- Altamirano, S.; Jackson, K.M.; Nielsen, K. The interplay of phenotype and genotype in Cryptococcus neoformans disease. Biosci. Rep. 2020, 40, BSR20190337. [Google Scholar] [CrossRef] [PubMed]
- Gerstein, A.C.; Jackson, K.M.; McDonald, T.R.; Wang, Y.; Lueck, B.D.; Bohjanen, S.; Smith, K.D.; Akampurira, A.; Meya, D.B.; Xue, C.; et al. Identification of Pathogen Genomic Differences That Impact Human Immune Response and Disease during Cryptococcus neoformans Infection. mBio 2019, 10, e01440-19. [Google Scholar] [CrossRef] [PubMed]
| CSF Fungal Burden | Sterile | Low CFU Tertile * | Middle CFU Tertile * | High CFU Tertile * | p-Value |
|---|---|---|---|---|---|
| (N = 55) | (N = 235) | (N = 234) | (N = 241) | ||
| Demographics | |||||
| Age, years | 37 [30, 42] | 34 [29, 40] | 36 [30, 40] | 35 [29, 40] | 0.09 |
| Women | 27 (49.1%) | 99 (42.1%) | 84 (35.9%) | 100 (41.5%) | 0.25 |
| Weight, kg | 55 [50, 60] | 53 [47, 60] | 52 [47, 60] | 52 [48, 59] | 0.52 |
| Glasgow Coma Score < 15 | 25 (45.5%) | 98 (41.9%) | 81 (34.8%) | 110 (45.6%) | 0.09 |
| CD4 Count, cells/μL | 70 [25, 96] | 25 [9, 62] | 15 [6, 39] | 10 [6, 28] | <0.001 |
| Receiving HIV Therapy | 39 (70.9%) | 108 (46.2%) | 75 (32.1%) | 63 (26.1%) | <0.001 |
| Months of HIV Therapy † | 2.3 [1.1, 12.8] | 4.1 [0.8, 19.7] | 3.0 [0.7, 24.4] | 15.0 [1.1, 38.8] | 0.10 |
| Baseline CSF Parameters | |||||
| Opening Pressure > 250 mm H2O | 10 (20.8%) | 89 (45.2%) | 125 (60.7%) | 145 (67.1%) | <0.001 |
| Opening Pressure, mm H2O | 168 [113, 240] | 230 [160, 340] | 288 [200, 401] | 348 [220, 473] | <0.001 |
| CSF > 5 White Cells/μL | 23 (46.0%) | 124 (54.1%) | 72 (32.3%) | 61 (26.2%) | <0.001 |
| CSF Protein, mg/dL | 55 [20, 124] | 76 [28, 140] | 57 [23, 97] | 56 [24, 117] | 0.13 |
| Variable | Hazard Ratio | Lower Bound 95%CI | Upper Bound 95%CI |
|---|---|---|---|
| Univariate Unadjusted [N = 765] | |||
| Sterile Group | 1.57 | 1.01 | 2.44 |
| Middle Tertile, 14,701–206,000 CFU/mL | 1.42 | 1.07 | 1.89 |
| High Tertile, >206,000 CFU/mL | 1.88 | 1.43 | 2.48 |
| Multivariate Adjusted Model #1 [N = 765] | |||
| Sterile Group | 1.63 | 1.04 | 2.56 |
| Middle Tertile, 14,701–206,000 CFU/mL | 1.40 | 1.05 | 1.87 |
| High Tertile, >206,000 CFU/mL | 1.84 | 1.40 | 2.45 |
| CD4+ T cell count, per 10 cells/μL | 1.00 | 0.99 | 1.01 |
| Multivariate Adjusted Model #2 [N = 765] | |||
| Sterile Group | 1.55 | 0.99 | 2.45 |
| Middle Tertile, 14,701–206,000 CFU/mL | 1.43 | 1.07 | 1.91 |
| High Tertile, >206,000 CFU/mL | 1.90 | 1.44 | 2.52 |
| CD4+ T cell count, per 10 cells/μL | 1.00 | 0.99 | 1.01 |
| Receiving ART at baseline | 1.17 | 0.94 | 1.47 |
| Sterile CSF (N = 24) | Low CFU Tertile (N = 98) | Middle CFU Tertile (N = 99) | High CFU Tertile (N = 113) | p-Value | |
|---|---|---|---|---|---|
| LABS | Median [IQR] | ||||
| CD4 cells/μL | 64 [26, 121] | 20 [7, 49] | 15 [6, 32] | 10 [6, 30] | <0.001 |
| CSF white cells/μL | 25 [4, 155] | 20 [<5, 95] | <5 [<5, <5] | <5 [<5, <5] | <0.001 |
| CYTOKINES | Mean (95% CI) on log2 pg/mL scale | ||||
| IL-6 | 9.2 (7.8, 10.6) | 8.3 (7.6, 8.9) | 7.4 (6.7, 8.1) | 7.4 (6.9, 8.0) | 0.02 |
| IL-17 | 2.0 (0.8, 3.1) | 0.6 (0.0, 1.2) | −0.2 (−0.7, 0.4) | −0.3 (−0.8, 0.2) | <0.001 |
| IFN-γ | 3.0 (2.0, 3.9) | 1.7 (1.2, 2.2) | 1.4 (0.9, 1.8) | 1.3 (0.9, 1.7) | 0.02 |
| G-CSF | 7.0 (5.9, 8.1) | 5.1 (4.6, 5.6) | 4.7 (4.3, 5.0) | 5.0 (4.6, 5.3) | <0.001 |
| GM-CSF | 6.2 (5.4, 7.0) | 5.2 (4.9, 5.5) | 4.9 (4.6, 5.2) | 5.0 (4.7, 5.2) | <0.001 |
| CXCL2 (GRO-b) | 4.8 (3.9, 5.6) | 3.5 (3.0, 3.9) | 3.3 (2.8, 3.7) | 3.7 (3.3, 4.0) | 0.02 |
| IFN-α | 3.1 (2.2, 3.9) | 1.6 (1.0, 2.2) | 1.7 (1.3, 2.1) | 2.1 (1.7, 2.4) | 0.02 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Skipper, C.P.; Hullsiek, K.H.; Stadelman, A.; Williams, D.A.; Ssebambulidde, K.; Okafor, E.; Tugume, L.; Nuwagira, E.; Akampurira, A.; Musubire, A.K.; et al. Sterile Cerebrospinal Fluid Culture at Cryptococcal Meningitis Diagnosis Is Associated with High Mortality. J. Fungi 2023, 9, 46. https://doi.org/10.3390/jof9010046
Skipper CP, Hullsiek KH, Stadelman A, Williams DA, Ssebambulidde K, Okafor E, Tugume L, Nuwagira E, Akampurira A, Musubire AK, et al. Sterile Cerebrospinal Fluid Culture at Cryptococcal Meningitis Diagnosis Is Associated with High Mortality. Journal of Fungi. 2023; 9(1):46. https://doi.org/10.3390/jof9010046
Chicago/Turabian StyleSkipper, Caleb P, Katherine Huppler Hullsiek, Anna Stadelman, Darlisha A Williams, Kenneth Ssebambulidde, Elizabeth Okafor, Lillian Tugume, Edwin Nuwagira, Andrew Akampurira, Abdu K Musubire, and et al. 2023. "Sterile Cerebrospinal Fluid Culture at Cryptococcal Meningitis Diagnosis Is Associated with High Mortality" Journal of Fungi 9, no. 1: 46. https://doi.org/10.3390/jof9010046





