Long-Term Health Consequences of SARS-CoV-2: Reaction Time and Brain Fog
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Reaction Time (RT)
2.3. Cognitive Impairment Questionnaire
2.4. Human Participants (Ethics and Consent)
2.5. Data Analysis
3. Results
3.1. Sample Description
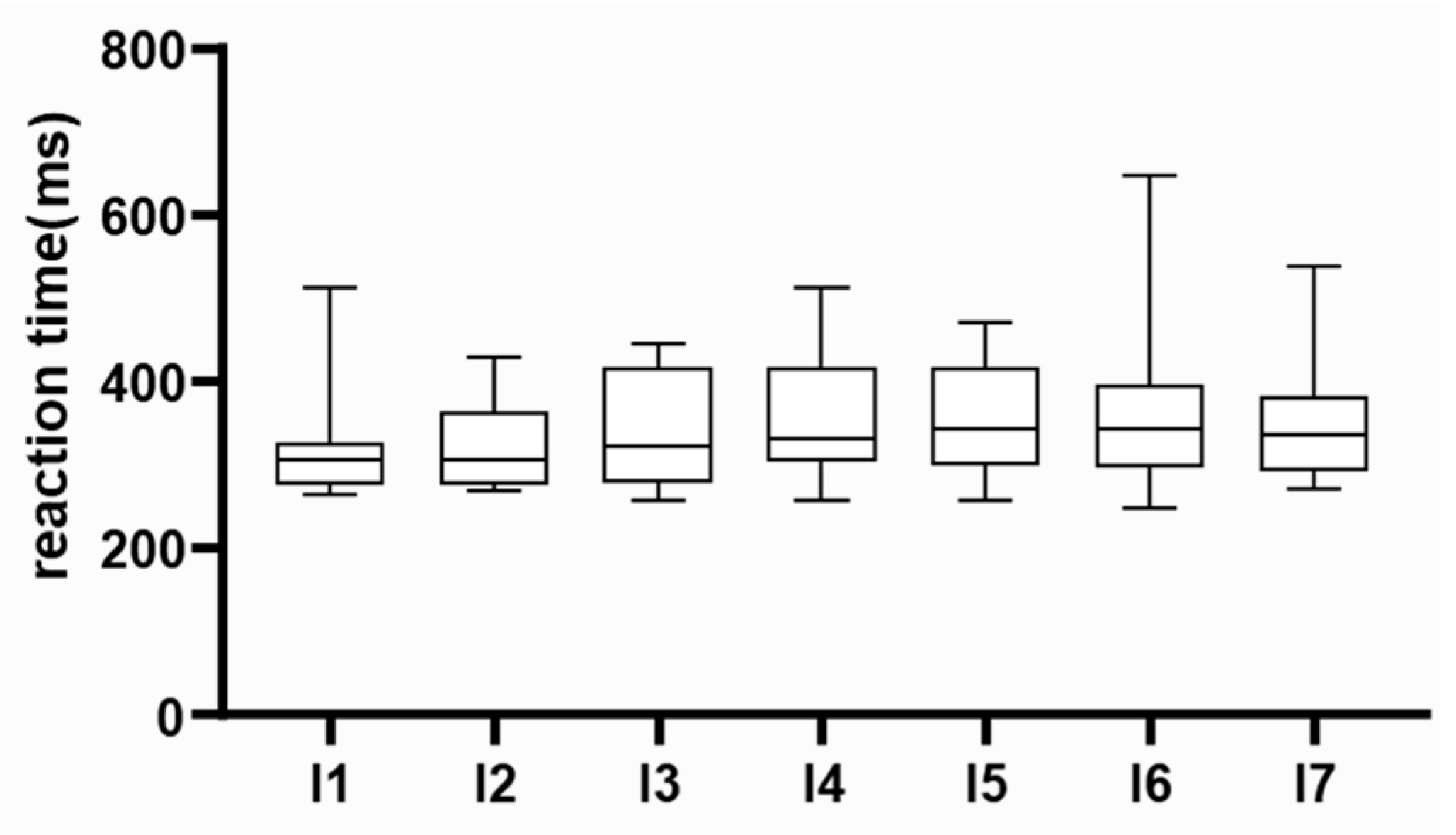
3.2. Data Quality Assessment
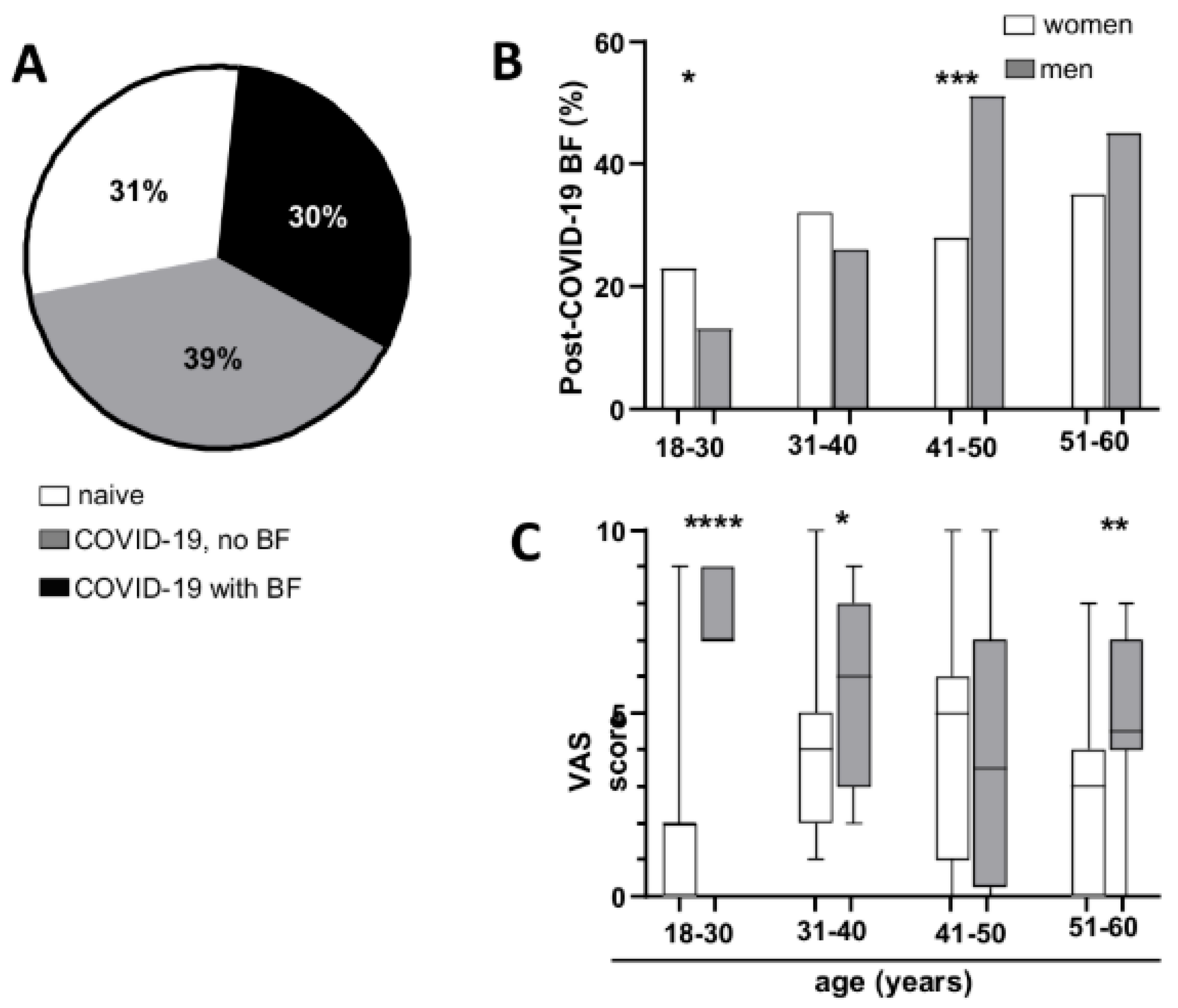
3.3. Prevalence of Brain Fog After COVID-19
3.4. Bothersome
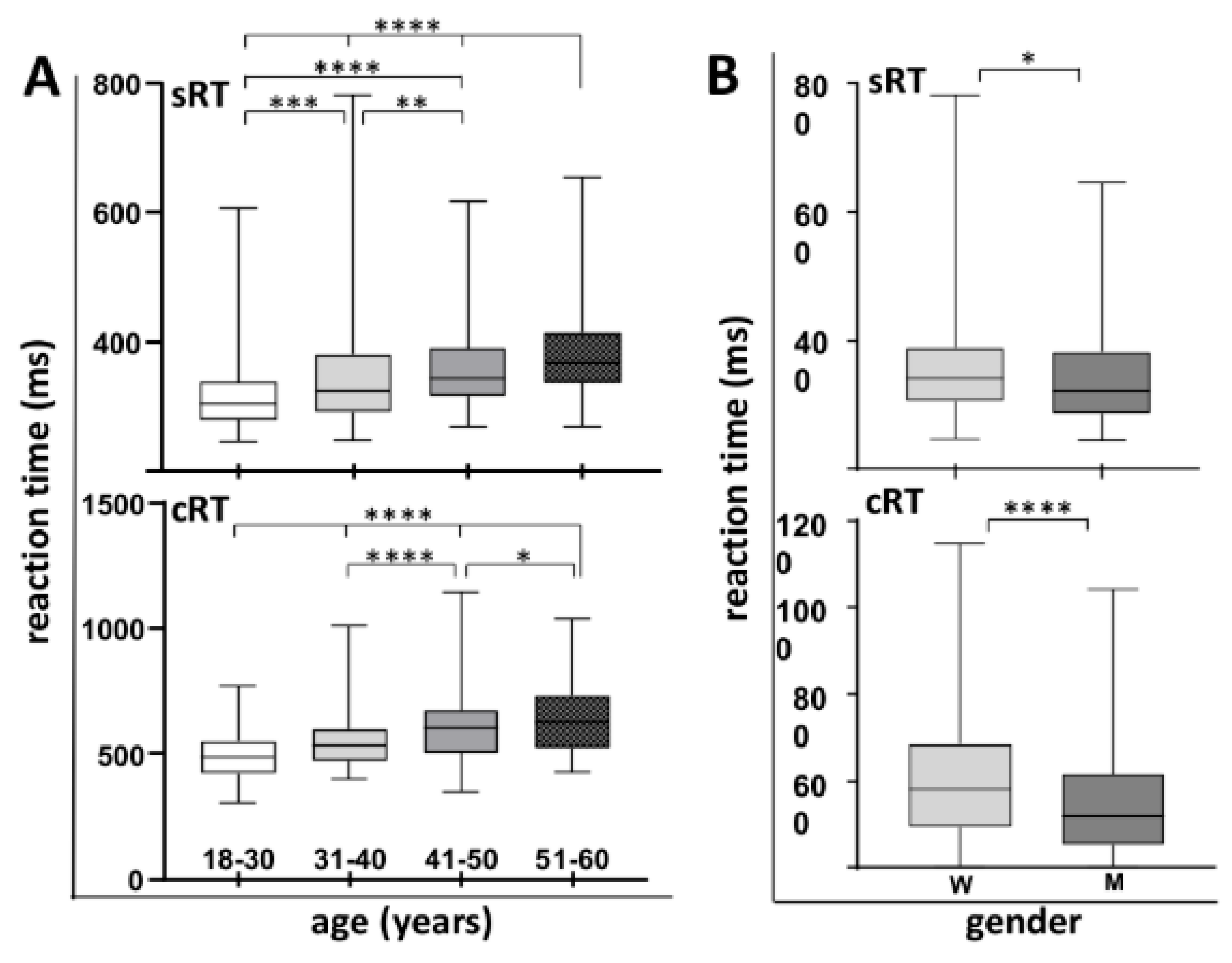
3.5. Differences in Simple and Complex Reaction Time Relative to Age and Gender
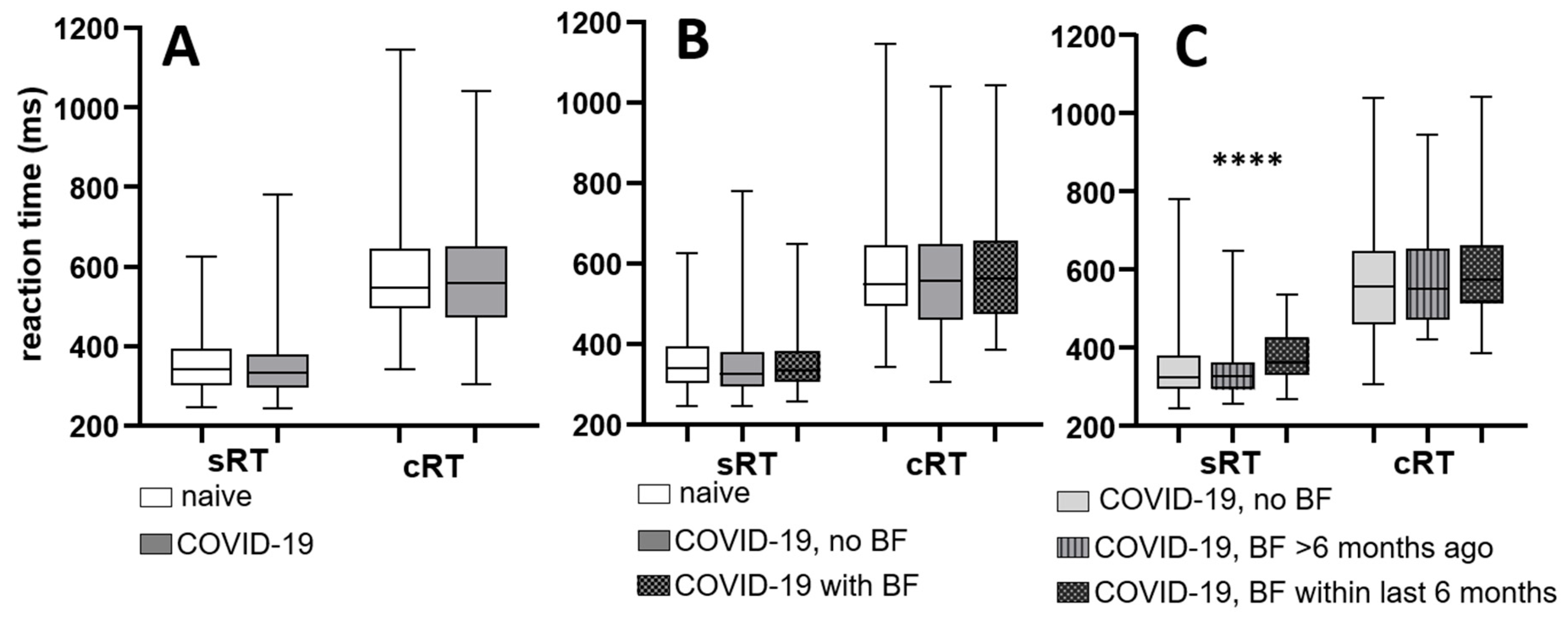
3.6. Reaction Times in Relation to COVID-19 Recovery and Reported Brain Fog
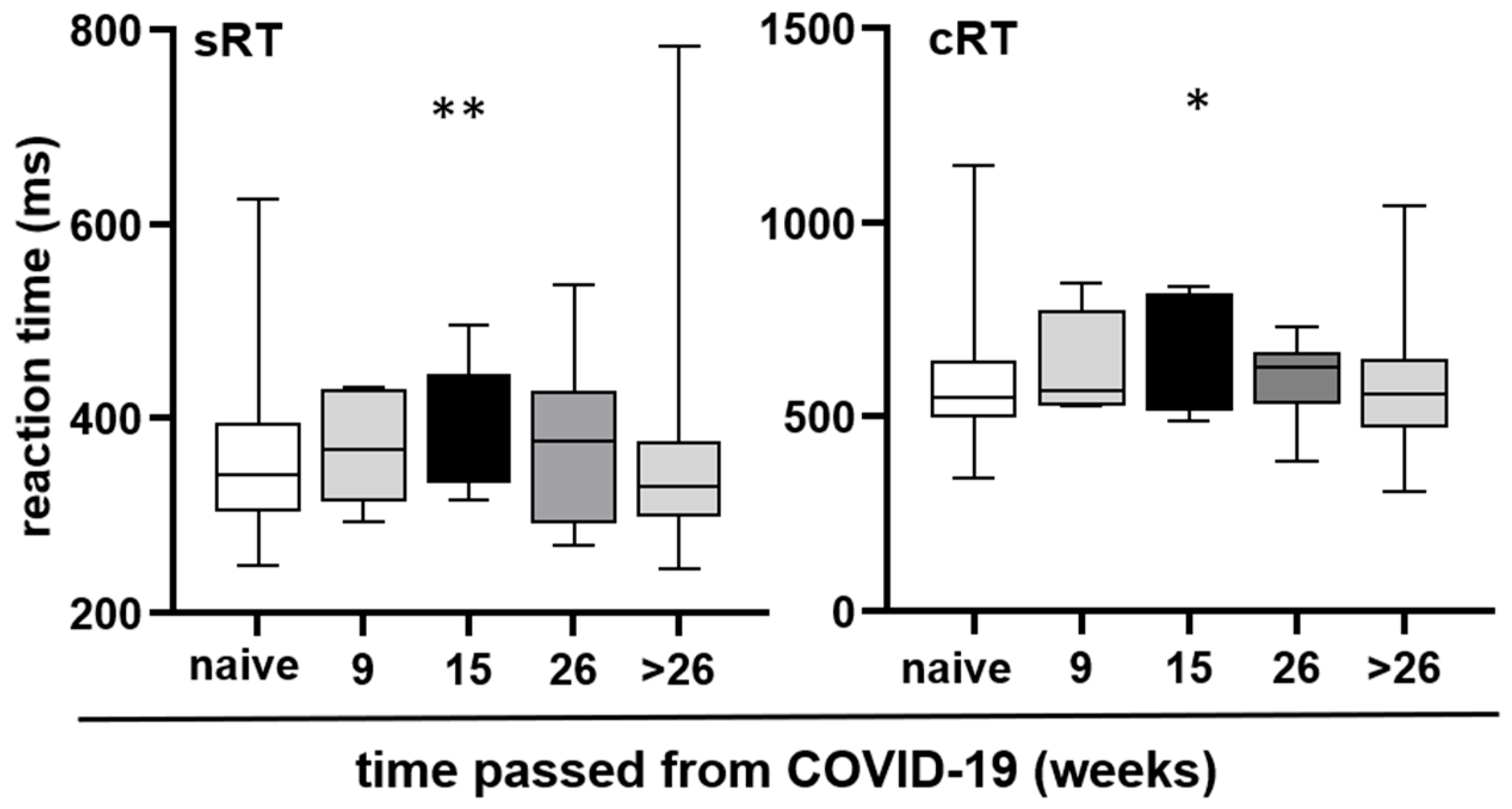
3.7. Changes in Reaction Time over Time Following COVID-19 Infection
3.8. Correlation Between Age, Brain Fog Severity, and Reaction Time
3.8.1. Age and Reaction Times
3.8.2. Age and Presence of Brain Fog
3.8.3. Age and “Bothersome” Brain Fog Parameters
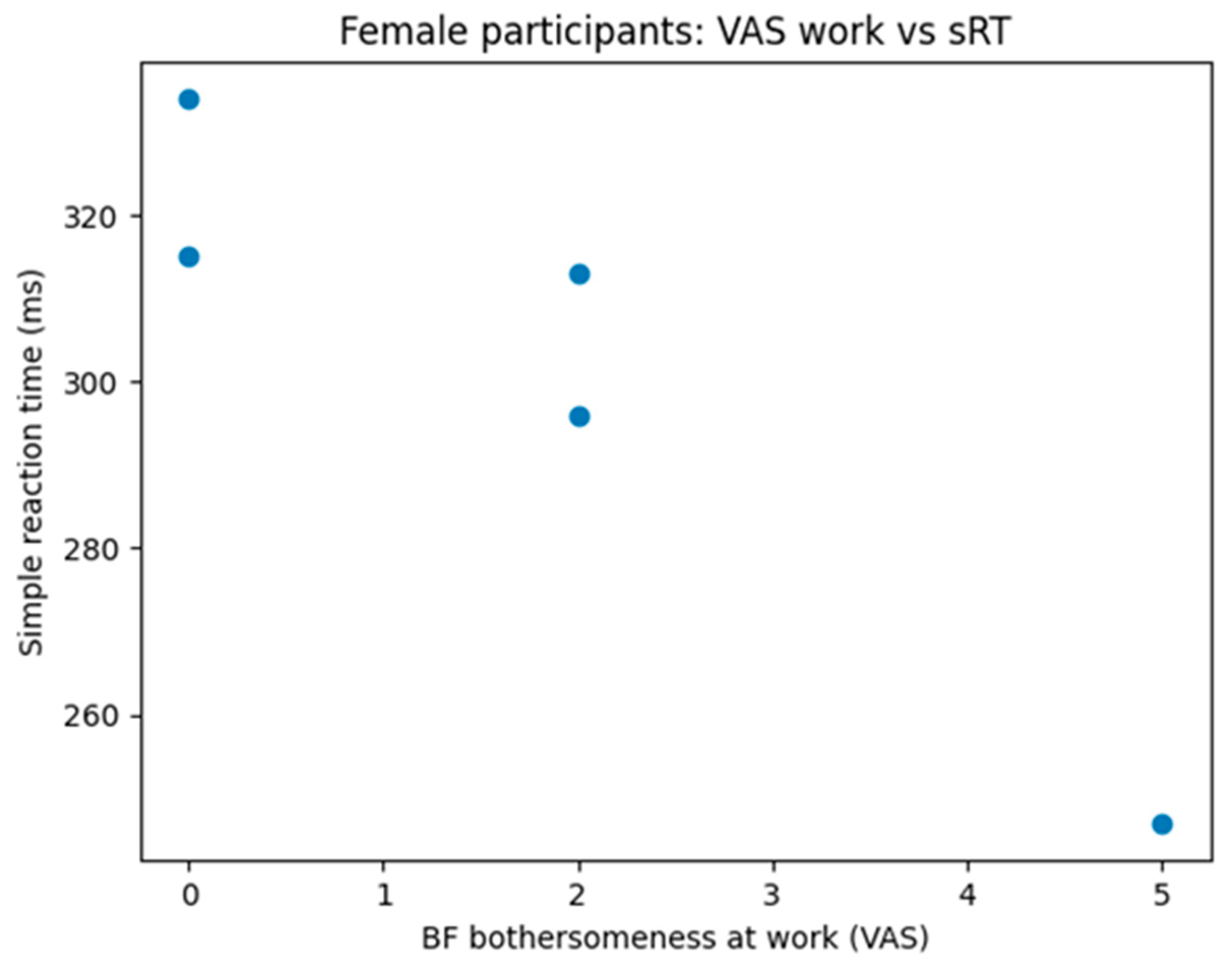
3.8.4. Subjective Brain Fog Severity and Objective Cognitive Performance (Exploratory)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACE2 | Angiotensin-converting enzyme 2 |
| BF | Brain fog |
| cRT | Complex reaction time |
| COVID-19 | Coronavirus disease 2019 |
| CRP | C-reactive protein |
| NIH | National Institutes of Health |
| PASC | Post-acute sequelae of SARS-CoV-2 |
| RT | Reaction time |
| sRT | Simple reaction time |
| SARS-CoV-2 | Severe acute respiratory syndrome coronavirus 2 |
| VAS | Visual analogue scale |
References
- Nagi, M.N.; Mansour, M.A. Protective effect of thymoquinone against doxorubicin-induced cardiotoxicity in rats: A possible mechanism of protection. Pharmacol. Res. 2000, 41, 283–289. [Google Scholar] [CrossRef]
- Pehlivan, D.Y.; Durdağı, G. Effects of thymoquinone on blood parameters in doxorubicin cardiotoxicity. Exp. Appl. Med. Sci. 2020, 1, 7–16. [Google Scholar]
- Corman, V.M.; Lienau, J.; Witzenrath, M. Coronaviruses as the cause of respiratory infections. Internist 2019, 60, 1136–1145. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Chen, P.; Wang, J.; Feng, J.; Zhou, H.; Li, X.; Zhong, W.; Hao, P. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci. China Life Sci. 2020, 63, 457–460. [Google Scholar] [CrossRef]
- Zhou, P.; Yang, X.L.; Wang, X.G.; Hu, B.; Zhang, L.; Zhang, W.; Si, H.-R.; Zhu, Y.; Li, B.; Huang, C.-L.; et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 2020, 579, 270–273. [Google Scholar] [CrossRef]
- Higgins, V.; Sohaei, D.; Diamandis, E.P.; Prassas, I. COVID-19: From an acute to chronic disease? Potential long-term health consequences. Crit. Rev. Clin. Lab. Sci. 2021, 58, 297–310. [Google Scholar] [CrossRef] [PubMed]
- Wadman, M.; Couzin-Frankel, J.; Kaiser, J.; Matacic, C. A rampage through the body. Science 2020, 368, 356–360. [Google Scholar] [CrossRef]
- Gupta, A.; Madhavan, M.V.; Sehgal, K.; Nair, N.; Mahajan, S.; Sehrawat, T.S.; Bikdeli, B.; Ahluwalia, N.; Ausiello, J.C.; Wan, E.Y.; et al. Extrapulmonary manifestations of COVID-19. Nat. Med. 2020, 26, 1017–1032. [Google Scholar] [CrossRef]
- Rus, C.P.; de Vries, B.E.K.; de Vries, I.E.J.; Nutma, I.; Kooij, J.J.S. Treatment of 95 post-COVID patients with SSRIs. Sci. Rep. 2023, 13, 18599. [Google Scholar] [CrossRef]
- Peter, R.S.; Nieters, A.; Kräusslich, H.G.; O Brockmann, S.; Göpel, S.; Kindle, G.; Merle, U.; Steinacker, J.M.; Rothenbacher, D.; Kern, W.V. Post-acute sequelae of COVID-19 six to twelve months after infection: Population-based study. Br. Med. J. 2022, 379, e071050. [Google Scholar] [CrossRef]
- Al-Aly, Z.; Xie, Y.; Bowe, B. High-dimensional characterization of post-acute sequelae of COVID-19. Nature 2021, 594, 259–264. [Google Scholar] [CrossRef]
- Kelly, K.M.; Anghinah, R.; Kullmann, A.; Ashmore, R.C.; Synowiec, A.S.; Gibson, L.C.; Manfrinati, L.; de Araújo, A.; Spera, R.R.; Brucki, S.M.D.; et al. Oculomotor, vestibular, reaction time, and cognitive tests as objective measures of neural deficits in patients post COVID-19 infection. Front. Neurol. 2022, 13, 919596. [Google Scholar] [CrossRef]
- Zhang, Y.; Dong, C. Unveiling the dynamic mechanisms of generative AI in English language learning: A hybrid study based on fsQCA and system dynamics. Behav. Sci. 2024, 14, 1015. [Google Scholar] [CrossRef] [PubMed]
- Stoet, G. PsyToolkit: A software package for programming psychological experiments using Linux. Behav. Res. Methods 2010, 42, 1096–1104. [Google Scholar] [CrossRef] [PubMed]
- Stoet, G. PsyToolkit: A novel web-based method for running online questionnaires and reaction-time experiments. Teach. Psychol. 2017, 44, 24–31. [Google Scholar] [CrossRef]
- Chen, K.C.; Weng, C.Y.; Hsiao, S.; Tsao, W.L.; Koo, M. Cognitive decline and slower reaction time in elderly individuals with mild cognitive impairment. Psychogeriatrics 2017, 17, 364–370. [Google Scholar] [CrossRef]
- Graveson, J.; Bauermeister, S.; McKeown, D.; Bunce, D. Intraindividual reaction time variability, falls, and gait in old age: A systematic review. J. Gerontol. B Psychol. Sci. Soc. Sci. 2016, 71, 857–864. [Google Scholar] [CrossRef] [PubMed]
- Lewis, R.D.; Brown, J.M. Influence of muscle activation dynamics on reaction time in the elderly. Eur. J. Appl. Physiol. Occup. Physiol. 1994, 69, 344–349. [Google Scholar] [CrossRef]
- van der Feltz-Cornelis, C.; Turk, F.; Sweetman, J.; Khunti, K.; Gabbay, M.; Shepherd, J.; Montgomery, H.; Strain, W.D.; Lip, G.Y.; Wootton, D.; et al. Prevalence of mental health conditions and brain fog in people with long COVID: A systematic review and meta-analysis. Gen. Hosp. Psychiatr. 2024, 88, 10–22. [Google Scholar] [CrossRef]
- Lippi, G.; Sanchis-Gomar, F.; Henry, B.M. COVID-19 and its long-term sequelae: What do we know in 2023? Pol. Arch. Intern. Med. 2023, 133, 16402. [Google Scholar] [CrossRef]
- Garrigues, E.; Janvier, P.; Kherabi, Y.; Le Bot, A.; Hamon, A.; Gouze, H.; Doucet, L.; Berkani, S.; Oliosi, E.; Mallart, E.; et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J. Infect. 2020, 81, e4–e6. [Google Scholar] [CrossRef]
- The Writing Committee for the COMEBAC Study Group; Morin, L.; Savale, L.; Pham, T.; Colle, R.; Figueiredo, S.; Harrois, A.; Gasnier, M.; Lecoq, A.-L.; Meyrignac, O.; et al. Four-month clinical status of a cohort of patients after hospitalization for COVID-19. J. Am. Med. Assoc. 2021, 325, 1525–1534. [Google Scholar] [CrossRef]
- Chen, C.; Haupert, S.R.; Zimmermann, L.; Shi, X.; Fritsche, L.G.; Mukherjee, B. Global prevalence of post-coronavirus disease 2019 (COVID-19) condition or long COVID: A meta-analysis and systematic review. J. Infect. Dis. 2022, 226, 1593–1607. [Google Scholar] [CrossRef]
- Chatys-Bogacka, Ż.; Mazurkiewicz, I.; Słowik, J.; Nowak, K.; Sydor, W.; Wizner, B.; Słowik, A.; Wnuk, M.; Drabik, L. Sex-related patient-reported brain fog symptoms in non-hospitalised COVID-19 patients. Neurol. Neurochir. Pol. 2023, 57, 111–120. [Google Scholar] [CrossRef]
- Der, G.; Deary, I.J. Age and sex differences in reaction time in adulthood: Results from the United Kingdom Health and Lifestyle Survey. Psychol. Aging 2006, 21, 62–73. [Google Scholar] [CrossRef]
- Salthouse, T.A. Aging and measures of processing speed. Biol. Psychol. 2000, 54, 35–54. [Google Scholar] [CrossRef]
- Hardwick, R.M.; Forrence, A.D.; Costello, M.G.; Zackowski, K.; Haith, A.M. Age-related increases in reaction time result from slower preparation, not delayed initiation. J. Neurophysiol. 2022, 128, 582–592. [Google Scholar] [CrossRef]
- Jain, A.; Bansal, R.; Kumar, A.; Singh, K.D. A comparative study of visual and auditory reaction times on the basis of gender and physical activity levels of medical first-year students. Int. J. Appl. Basic Med. Res. 2015, 5, 124–127. [Google Scholar] [CrossRef] [PubMed]
- Lipps, D.B.; Galecki, A.T.; Ashton-Miller, J.A. On the implications of a sex difference in the reaction times of sprinters at the Beijing Olympics. PLoS ONE 2011, 6, e26141. [Google Scholar] [CrossRef] [PubMed]
- Luvizutto, G.J.; Sisconetto, A.T.; Appelt, P.A.; Sucupira, K.S.M.B.; Neto, E.d.M.; de Souza, L.A.P.S. Can the choice reaction time be modified after COVID-19 diagnosis? A prospective cohort study. Dement. Neuropsychol. 2022, 16, 354–360. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Lu, S.; Chen, J.; Wei, N.; Wang, D.; Lyu, H.; Shi, C.; Hu, S. The landscape of cognitive function in recovered COVID-19 patients. J. Psychiatr. Res. 2020, 129, 98–102. [Google Scholar] [CrossRef] [PubMed]
- do Carmo Filho, A.; van Duinkerken, E.; Tolentino, J.C.; Schmidt, S.L. Attention profile of physically recovered COVID-19 inpatients on the day of discharge. J. Psychiatr. Res. 2022, 150, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Manukyan, P.; Deviaterikova, A.; Velichkovsky, B.B.; Kasatkin, V. The impact of mild COVID-19 on executive functioning and mental health outcomes in young adults. Healthcare 2022, 10, 1891. [Google Scholar] [CrossRef] [PubMed]
| Age | Total | Men | Women |
|---|---|---|---|
| 18–30 | 150 | 55 | 95 |
| 31–40 | 159 | 57 | 102 |
| 41–50 | 149 | 53 | 96 |
| 51–60 | 141 | 49 | 92 |
| By Age | 18–30 | 31–40 | 41–50 | 51–60 |
|---|---|---|---|---|
| 18–30 | – | 0.0027 | <0.0001 | <0.0001 |
| 31–40 | <0.0001 | – | 0.0055 | <0.0001 |
| 41–50 | <0.0001 | <0.0001 | – | 0.0017 |
| 51–60 | <0.0001 | <0.0001 | 0.0546 | – |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Lesac Brizić, A.; Popović, B.; Zavidić, T.; Todorović, N.; Petrović, V.; Pilipović-Broćeta, N.; Miljković, A.R.; Ljubotina, A.; Dejhalla, E. Long-Term Health Consequences of SARS-CoV-2: Reaction Time and Brain Fog. Neurol. Int. 2026, 18, 6. https://doi.org/10.3390/neurolint18010006
Lesac Brizić A, Popović B, Zavidić T, Todorović N, Petrović V, Pilipović-Broćeta N, Miljković AR, Ljubotina A, Dejhalla E. Long-Term Health Consequences of SARS-CoV-2: Reaction Time and Brain Fog. Neurology International. 2026; 18(1):6. https://doi.org/10.3390/neurolint18010006
Chicago/Turabian StyleLesac Brizić, Ana, Branislava Popović, Tina Zavidić, Nevena Todorović, Verica Petrović, Nataša Pilipović-Broćeta, Ana R. Miljković, Aleksandar Ljubotina, and Ema Dejhalla. 2026. "Long-Term Health Consequences of SARS-CoV-2: Reaction Time and Brain Fog" Neurology International 18, no. 1: 6. https://doi.org/10.3390/neurolint18010006
APA StyleLesac Brizić, A., Popović, B., Zavidić, T., Todorović, N., Petrović, V., Pilipović-Broćeta, N., Miljković, A. R., Ljubotina, A., & Dejhalla, E. (2026). Long-Term Health Consequences of SARS-CoV-2: Reaction Time and Brain Fog. Neurology International, 18(1), 6. https://doi.org/10.3390/neurolint18010006








