Relationship Between Each of the Four Major Motor Symptoms and At-Home Physical Activity in Individuals with Parkinson’s Disease: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Demographic and Clinical Characteristics
2.3. At-Home PA Measurement
2.4. Motor Symptom Measurement
2.5. Statistical Analysis
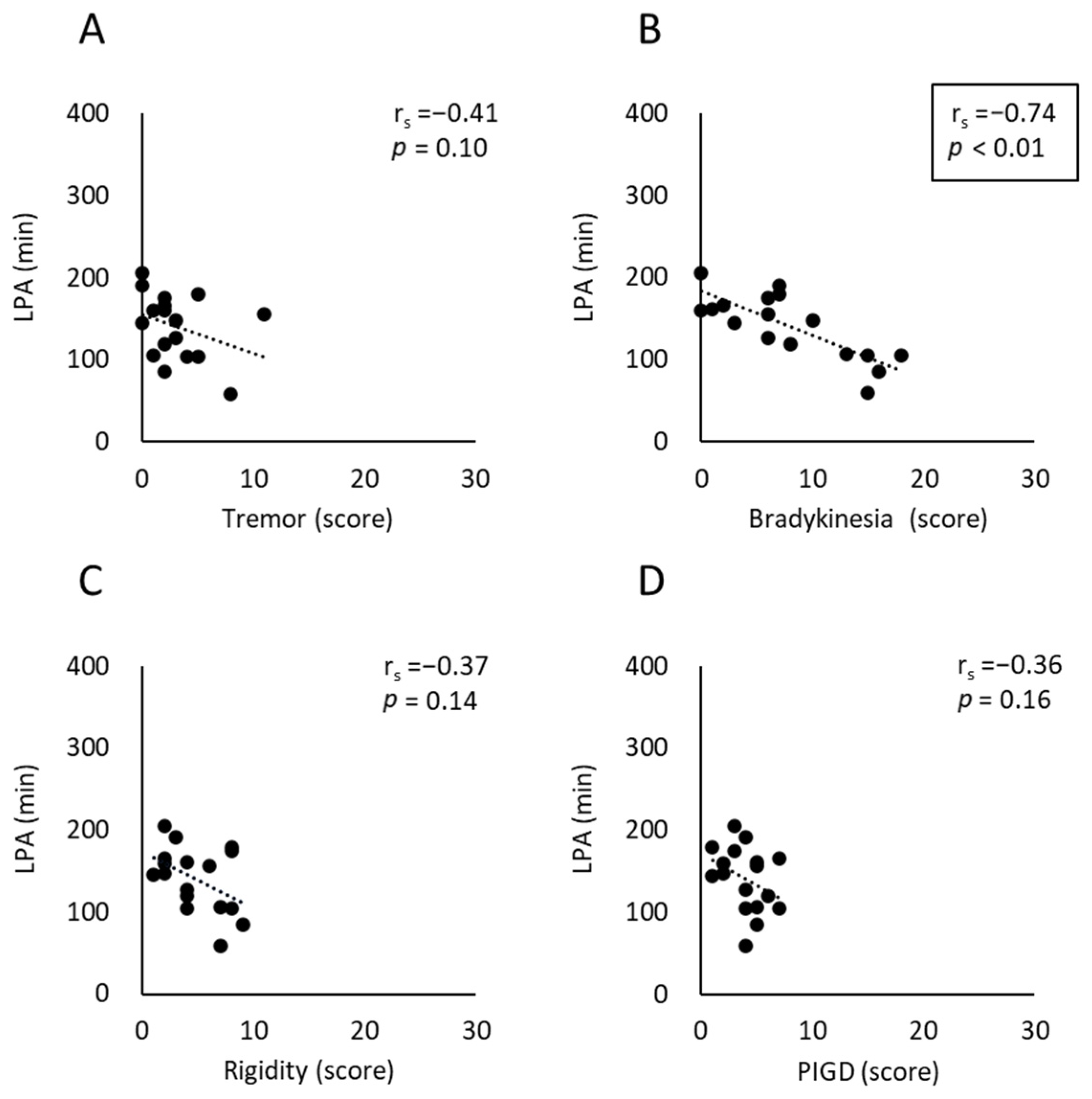
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADLs | Activities of daily living |
| CI | Confidence interval |
| HY | Hoehn and Yahr |
| LPA | Light physical activity |
| LEDD | Levodopa equivalent daily dose |
| LSVT BIG | Lee Silverman Voice Treatment BIG |
| MDS-UPDRS | Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale |
| MET | Metabolic equivalent |
| MVPA | Moderate-to-vigorous physical activity |
| PA | Physical activity |
| PD | Parkinson’s disease |
| PIGD | Postural instability/gait disorder |
| SB | sedentary behavior |
References
- GBD 2016 Neurology Collaborators. Global, regional, and national burden of neurological disorders, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 459–480. [Google Scholar] [CrossRef] [PubMed]
- Kalia, L.V.; Lang, A.E. Parkinson’s disease. Lancet 2015, 386, 896–912. [Google Scholar] [CrossRef]
- Bloem, B.R.; Okun, M.S.; Klein, C. Parkinson’s disease. Lancet 2021, 397, 2284–2303. [Google Scholar] [CrossRef] [PubMed]
- Pickrell, A.M.; Youle, R.J. The roles of PINK1, parkin, and mitochondrial fidelity in Parkinson’s disease. Neuron 2015, 85, 257–273. [Google Scholar] [CrossRef]
- Tolosa, E.; Garrido, A.; Scholz, S.W.; Poewe, W. Challenges in the diagnosis of Parkinson’s disease. Lancet Neurol. 2021, 20, 385–397. [Google Scholar] [CrossRef]
- Obeso, J.A.; Rodríguez-Oroz, M.C.; Rodríguez, M.; Lanciego, J.L.; Artieda, J.; Gonzalo, N.; Olanow, C.W. Pathophysiology of the basal ganglia in Parkinson’s disease. Trends Neurosci. 2000, 23 (Suppl. 10), S8–S19. [Google Scholar] [CrossRef]
- Simon, D.K.; Tanner, C.M.; Brundin, P. Parkinson disease epidemiology, pathology, genetics, and pathophysiology. Clin. Geriatr. Med. 2020, 36, 1–12. [Google Scholar] [CrossRef]
- Stoker, T.B.; Greenland, J.C. Parkinson’s Disease: Pathogenesis and Clinical Aspects; Codon Publications: Brisbane, AU, USA, 2018. [Google Scholar]
- Borrione, P.; Tranchita, E.; Sansone, P.; Parisi, A. Effects of physical activity in Parkinson’s disease: A new tool for rehabilitation. World J. Methodol. 2014, 4, 133–143. [Google Scholar] [CrossRef]
- Jankovic, J. Parkinson’s disease: Clinical features and diagnosis. J. Neurol. Neurosurg. Psychiatry 2008, 79, 368–376. [Google Scholar] [CrossRef] [PubMed]
- Giovannoni, G.; van Schalkwyk, J.; Fritz, V.U.; Lees, A.J. Bradykinesia akinesia inco-ordination test (BRAIN TEST): An objective computerised assessment of upper limb motor function. J. Neurol. Neurosurg. Psychiatry 1999, 67, 624–629. [Google Scholar] [CrossRef]
- Berardelli, A.; Rothwell, J.C.; Thompson, P.D.; Hallett, M. Pathophysiology of bradykinesia in Parkinson’s disease. Brain 2001, 124, 2131–2146. [Google Scholar] [CrossRef]
- Kim, S.D.; Allen, N.E.; Canning, C.G.; Fung, V.S.C. Postural instability in patients with Parkinson’s disease. Epidemiology, pathophysiology and management. CNS Drugs 2013, 27, 97–112. [Google Scholar] [CrossRef]
- Grabli, D.; Karachi, C.; Welter, M.L.; Lau, B.; Hirsch, E.C.; Vidailhet, M.; François, C. Normal and pathological gait: What we learn from Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 2012, 83, 979–985. [Google Scholar] [CrossRef]
- Bloem, B.R.; Hausdorff, J.M.; Visser, J.E.; Giladi, N. Falls and freezing of gait in Parkinson’s disease: A review of two interconnected, episodic phenomena. Mov. Disord. 2004, 19, 871–884. [Google Scholar] [CrossRef] [PubMed]
- Hariz, G.M.; Forsgren, L. Activities of daily living and quality of life in persons with newly diagnosed Parkinson’s disease according to subtype of disease, and in comparison to healthy controls. Acta Neurol. Scand. 2011, 123, 20–27. [Google Scholar] [CrossRef]
- Rahman, S.; Griffin, H.J.; Quinn, N.P.; Jahanshahi, M. Quality of life in Parkinson’s disease: The relative importance of the symptoms. Mov. Disord. 2008, 23, 1428–1434. [Google Scholar] [CrossRef] [PubMed]
- Yano, S.; Koohsari, M.J.; Shibata, A.; Ishii, K.; Mavoa, S.; Oka, K. Assessing physical activity and sedentary behavior under free-living conditions: Comparison of Active Style Pro HJA-350IT and ActiGraphTM GT3X. Int. J. Environ. Res. Public Health 2019, 16, 3065. [Google Scholar] [CrossRef]
- Tanaka, C.; Reilly, J.J.; Tanaka, S. Correlations between the Japanese version of the Global Physical Activity Questionnaire and accelerometer-measured physical activity and sedentary time in adult women and men. J. Act. Sedentary Sleep Behav. 2024, 3, 29. [Google Scholar] [CrossRef]
- van Nimwegen, M.; Speelman, A.D.; Overeem, S.; van de Warrenburg, B.P.; Smulders, K.; Dontje, M.L.; Borm, G.F.; Backx, F.J.; Bloem, B.R.; Munneke, M.; et al. Promotion of physical activity and fitness in sedentary patients with Parkinson’s disease: Randomised controlled trial. BMJ 2013, 346, f576. [Google Scholar] [CrossRef]
- Colón-Semenza, C.; Latham, N.K.; Quintiliani, L.M.; Ellis, T.D. Peer coaching through mHealth targeting physical activity in people with Parkinson disease: Feasibility study. JMIR mHealth uHealth 2018, 6, e42. [Google Scholar] [CrossRef]
- Gibbs, B.B.; Hergenroeder, A.L.; Katzmarzyk, P.T.; Lee, I.M.; Jakicic, J.M. Definition, measurement, and health risks associated with sedentary behavior. Med. Sci. Sports Exerc. 2015, 47, 1295–1300. [Google Scholar] [CrossRef]
- Lord, S.; Godfrey, A.; Galna, B.; Mhiripiri, D.; Burn, D.; Rochester, L. Ambulatory activity in incident Parkinson’s: More than meets the eye? J. Neurol. 2013, 260, 2964–2972. [Google Scholar] [CrossRef]
- von Rosen, P.; Hagströmer, M.; Franzén, E.; Leavy, B. Physical activity profiles in Parkinson’s disease. BMC Neurol. 2021, 21, 71. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, S.; Kelly, V.E. Quantifying physical activity in early Parkinson disease using a commercial activity monitor. Park. Relat. Disord. 2019, 66, 171–175. [Google Scholar] [CrossRef] [PubMed]
- Benka Wallén, M.; Franzén, E.; Nero, H.; Hagströmer, M. Levels and patterns of physical activity and sedentary behavior in elderly people with mild to moderate Parkinson disease. Phys. Ther. 2015, 95, 1135–1141. [Google Scholar] [CrossRef]
- Skidmore, F.M.; Mackman, C.A.; Pav, B.; Shulman, L.M.; Garvan, C.; Macko, R.F.; Heilman, K.M. Daily ambulatory activity levels in idiopathic Parkinson disease. J. Rehabil. Res. Dev. 2008, 45, 1343–1348. [Google Scholar] [CrossRef]
- Galperin, I.; Hillel, I.; Del Din, S.; Bekkers, E.M.J.; Nieuwboer, A.; Abbruzzese, G.; Avanzino, L.; Nieuwhof, F.; Bloem, B.R.; Rochester, L.; et al. Associations between daily-living physical activity and laboratory-based assessments of motor severity in patients with falls and Parkinson’s disease. Park. Relat. Disord. 2019, 62, 85–90. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef]
- Tomlinson, C.L.; Stowe, R.; Patel, S.; Rick, C.; Gray, R.; Clarke, C.E. Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov. Disord. 2010, 25, 2649–2653. [Google Scholar] [CrossRef]
- Hoehn, M.M.; Yahr, M.D. Parkinsonism: Onset, progression and mortality. Neurology 1967, 17, 427–442. [Google Scholar] [CrossRef]
- Hirakawa, Y.; Sakurai, H.; Takeda, K.; Koyama, S.; Iwai, M.; Motoya, I.; Kanada, Y.; Kawamura, N.; Kawamura, M.; Tanabe, S. Measurement of physical activity divided into inside and outside the home in people with Parkinson’s disease: A feasibility study. J. Eval. Clin. Pract. 2025, 31, e14251. [Google Scholar] [CrossRef]
- Nagayoshi, S.; Oshima, Y.; Ando, T.; Aoyama, T.; Nakae, S.; Usui, C.; Kumagai, S.; Tanaka, S. Validity of estimating physical activity intensity using a triaxial accelerometer in healthy adults and older adults. BMJ Open Sport Exerc. Med. 2019, 5, e000592. [Google Scholar] [CrossRef] [PubMed]
- Murakami, H.; Kawakami, R.; Nakae, S.; Yamada, Y.; Nakata, Y.; Ohkawara, K.; Sasai, H.; Ishikawa-Takata, K.; Tanaka, S.; Miyachi, M. Accuracy of 12 wearable devices for estimating physical activity energy expenditure using a metabolic chamber and the doubly labeled water method: Validation study. JMIR mHealth uHealth 2019, 7, e13938. [Google Scholar] [CrossRef]
- Park, J.; Ishikawa-Takata, K.; Tanaka, S.; Mekata, Y.; Tabata, I. Effects of walking speed and step frequency on estimation of physical activity using accelerometers. J. Physiol. Anthropol. 2011, 30, 119–127. [Google Scholar] [CrossRef][Green Version]
- Buckley, C.; Cavadino, A.; Del Din, S.; Lord, S.; Taylor, L.; Rochester, L.; Kerse, N. Quantifying reliable walking activity with a wearable device in aged residential care: How many days are enough? Sensors 2020, 20, 6314. [Google Scholar] [CrossRef]
- Sasaki, J.E.; Júnior, J.H.; Meneguci, J.; Tribess, S.; Marocolo Júnior, M.; Stabelini Neto, A.; Virtuoso Júnior, J.S. Number of days required for reliably estimating physical activity and sedentary behaviour from accelerometer data in older adults. J. Sports Sci. 2018, 36, 1572–1577. [Google Scholar] [CrossRef]
- Hart, T.L.; Swartz, A.M.; Cashin, S.E.; Strath, S.J. How many days of monitoring predict physical activity and sedentary behaviour in older adults? Int. J. Behav. Nutr. Phys. Act. 2011, 8, 62. [Google Scholar] [CrossRef] [PubMed]
- Goetz, C.G.; Tilley, B.C.; Shaftman, S.R.; Stebbins, G.T.; Fahn, S.; Martinez-Martin, P.; Poewe, W.; Sampaio, C.; Stern, M.B.; Dodel, R.; et al. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): Scale presentation and clinimetric testing results. Mov. Disord. 2008, 23, 2129–2170. [Google Scholar] [CrossRef] [PubMed]
- Duncan, R.P.; Earhart, G.M. Randomized controlled trial of community-based dancing to modify disease progression in Parkinson disease. Neurorehabil. Neural. Repair 2012, 26, 132–143. [Google Scholar] [CrossRef]
- Portney, L.G.; Watkins, M.P. Foundations of Clinical Research: Applications to Practice, 3rd ed.; Pearson Prentice Hall: Upper Saddle River, NJ, USA, 2009. [Google Scholar]
- Osborne, J.W.; Overbay, A. The power of outliers (and why researchers should ALWAYS check for them). Pract. Assess. Res. Eval. 2004, 9, 6. [Google Scholar] [CrossRef]
- Tukey, J.W. Exploratory Data Analysis; Addison-Wesley Publishing Company: Philippines, PA, USA, 1977. [Google Scholar]
- Blair, C.K.; Morey, M.C.; Desmond, R.A.; Cohen, H.J.; Sloane, R.; Snyder, D.C.; Demark-Wahnefried, W. Light-intensity activity attenuates functional decline in older cancer survivors. Med. Sci. Sports Exerc. 2014, 46, 1375–1383. [Google Scholar] [CrossRef]
- Lana Rde, C.; de Araujo, L.N.; Cardoso, F.; Rodrigues-de-Paula, F. Main determinants of physical activity levels in individuals with Parkinson’s disease. Arq. Neuro-Psiquiatr. 2016, 74, 112–116. [Google Scholar] [CrossRef] [PubMed]
- Bouça-Machado, R.; Rosário, A.; Caldeira, D.; Caldas, A.C.; Guerreiro, D.; Venturelli, M.; Tinazzi, M.; Schena, F.; Ferreira, J.J. Physical activity, exercise, and physiotherapy in Parkinson’s disease: Defining the concepts. Mov. Disord. Clin. Pract. 2020, 7, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Iwai, M.; Koyama, S.; Takeda, K.; Hirakawa, Y.; Motoya, I.; Sakurai, H.; Kanada, Y.; Okada, Y.; Kawamura, N.; Kawamura, M.; et al. Effect of Lee Silverman Voice Treatment® BIG on the major motor symptoms in patients with moderate Parkinson’s disease: An observational study. J. Gerontol. Geriatrics 2024, 72, 76–82. [Google Scholar] [CrossRef]
- Lee, D.H.; Woo, B.S.; Park, Y.H.; Lee, J.H. General treatments promoting independent living in Parkinson’s patients and physical therapy approaches for improving gait—A comprehensive review. Medicina 2024, 60, 711. [Google Scholar] [CrossRef] [PubMed]
- Dibble, L.E.; Hale, T.F.; Marcus, R.L.; Gerber, J.P.; LaStayo, P.C. High intensity eccentric resistance training decreases bradykinesia and improves quality of life in persons with Parkinson’s disease: A preliminary study. Park. Relat. Disord. 2009, 15, 752–757. [Google Scholar] [CrossRef]
- Memar, S.; Delrobaei, M.; Pieterman, M.; McIsaac, K.; Jog, M. Quantification of whole-body bradykinesia in Parkinson’s disease participants using multiple inertial sensors. J. Neurol. Sci. 2018, 387, 157–165. [Google Scholar] [CrossRef]


| Sex [M/F] | No. | Age [Years] | MMSE [Points] | Time Since Diagnosis [Years] | LEDD [mg/Day] | HY Stage | SB [min] | LPA [min] | MVPA [min] | MDS-UPDRS Part 3 [Scores] | Tremor | Rigidity | Bradykinesia | PIGD |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F | 1 | 78 | 30 | 11 | 650 | 2 | 470.1 | 147.8 | 5.1 | 17 | 3 | 2 | 10 | 2 |
| 2 | 63 | 30 | 5 | 150 | 2 | 515.7 | 175.0 | 10.6 | 16 | 2 | 8 | 6 | 3 | |
| 3 | 86 | 29 | 7 | 900 | 4 | 542.6 | 119.3 | 6.4 | 20 | 2 | 4 | 8 | 6 | |
| 4 | 64 | 30 | 8 | 100 | 2 | 488.6 | 160.0 | 2.1 | 5 | 1 | 2 | 0 | 2 | |
| 5 | 53 | 30 | 2 | 600 | 2 | 468.6 | 180.0 | 10.6 | 21 | 5 | 8 | 7 | 1 | |
| 6 | 57 | 29 | 4 | 350 | 2 | 522.9 | 160.6 | 4.0 | 12 | 2 | 4 | 1 | 5 | |
| 7 | 71 | 25 | 8 | 400 | 3 | 544.6 | 165.6 | 3.6 | 13 | 2 | 2 | 2 | 7 | |
| 8 | 63 | 30 | 10 | 500 | 4 | 538.7 | 58.7 | 24.3 | 39 | 8 | 7 | 15 | 4 | |
| 9 | 70 | 27 | 0 | 0 | 2 | 463.6 | 155.7 | 10.7 | 31 | 11 | 6 | 6 | 5 | |
| 10 | 66 | 29 | 0 | 0 | 2 | 363.6 | 190.9 | 8.4 | 14 | 0 | 3 | 7 | 4 | |
| Subtotal | 67.1 (9.2) | 29.5 [28.5, 30.0] | 5.5 (3.7) | 365.0 (287.3) | 2.0 [2.0, 4.0] | 491.9 (52.3) | 151.3 (36.0) | 8.6 (6.0) | 16.5 [12.8, 23.5] | 2.0 [1.8, 5.8] | 4.0 [2.0, 7.3] | 6.5 [1.8, 8.5] | 4.0 [2.0, 5.3] | |
| M | 11 | 75 | 25 | 2 | 350 | 2 | 604.3 | 104.3 | 3.0 | 28 | 4 | 4 | 15 | 4 |
| 12 | 80 | 27 | 3 | 600 | 3 | 594.3 | 104.3 | 10.0 | 38 | 5 | 8 | 18 | 7 | |
| 13 | 76 | 20 | 5 | 400 | 4 | 615.7 | 85.0 | 7.6 | 33 | 2 | 9 | 16 | 5 | |
| 14 | 47 | 30 | 17 | 450 | 1 | 541.0 | 205.7 | 16.0 | 5 | 0 | 2 | 0 | 3 | |
| 15 | 74 | 23 | 3 | 300 | 3 | 538.8 | 105.8 | 1.4 | 28 | 1 | 7 | 13 | 5 | |
| 16 | 72 | 30 | 3 | 400 | 4 | 550.0 | 126.8 | 1.8 | 20 | 3 | 4 | 6 | 4 | |
| 17 | 73 | 25 | 3 | 380 | 4 | 497.0 | 145.0 | 2.2 | 10 | 0 | 1 | 3 | 1 | |
| Subtotal | 71.0 (10.1) | 25.0 [23.0, 30.0] | 5.1 (4.9) | 411.4 (88.2) | 3.0 [2.0, 4.0] | 563 (39.7) | 125 (37.3) | 6.0 (5.1) | 28.0 [10.0, 33.0] | 2.0 [0, 4.0] | 4.0 [2.0, 8.0] | 13.0 [3.0, 16.0] | 4.0 [3.0, 5.0] | |
| Grand total | 68.7 (9.8) | 29.0 [25.0, 30.0] | 5.4 (4.3) | 384.1 (228.6) | 2.0 [2.0, 4.0] | 521.2 (59.0) | 140.6 (38.7) | 7.5 (5.8) | 20.0 [12.5, 29.5] | 2.0 [1.0, 4.5] | 4.0 [2.0, 7.5] | 7.0 [2.5, 14.0] | 4.0 [2.5, 5.0] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hirakawa, Y.; Sakurai, H.; Takeda, K.; Koyama, S.; Iwai, M.; Motoya, I.; Kanada, Y.; Kawamura, N.; Kawamura, M.; Tanabe, S. Relationship Between Each of the Four Major Motor Symptoms and At-Home Physical Activity in Individuals with Parkinson’s Disease: A Cross-Sectional Study. Neurol. Int. 2025, 17, 139. https://doi.org/10.3390/neurolint17090139
Hirakawa Y, Sakurai H, Takeda K, Koyama S, Iwai M, Motoya I, Kanada Y, Kawamura N, Kawamura M, Tanabe S. Relationship Between Each of the Four Major Motor Symptoms and At-Home Physical Activity in Individuals with Parkinson’s Disease: A Cross-Sectional Study. Neurology International. 2025; 17(9):139. https://doi.org/10.3390/neurolint17090139
Chicago/Turabian StyleHirakawa, Yuichi, Hiroaki Sakurai, Kazuya Takeda, Soichiro Koyama, Masanobu Iwai, Ikuo Motoya, Yoshikiyo Kanada, Nobutoshi Kawamura, Mami Kawamura, and Shigeo Tanabe. 2025. "Relationship Between Each of the Four Major Motor Symptoms and At-Home Physical Activity in Individuals with Parkinson’s Disease: A Cross-Sectional Study" Neurology International 17, no. 9: 139. https://doi.org/10.3390/neurolint17090139
APA StyleHirakawa, Y., Sakurai, H., Takeda, K., Koyama, S., Iwai, M., Motoya, I., Kanada, Y., Kawamura, N., Kawamura, M., & Tanabe, S. (2025). Relationship Between Each of the Four Major Motor Symptoms and At-Home Physical Activity in Individuals with Parkinson’s Disease: A Cross-Sectional Study. Neurology International, 17(9), 139. https://doi.org/10.3390/neurolint17090139







