Thenar Muscle Atrophy: Clinical, Electrodiagnostic, and Ultrasound Features in 197 Patients
Abstract
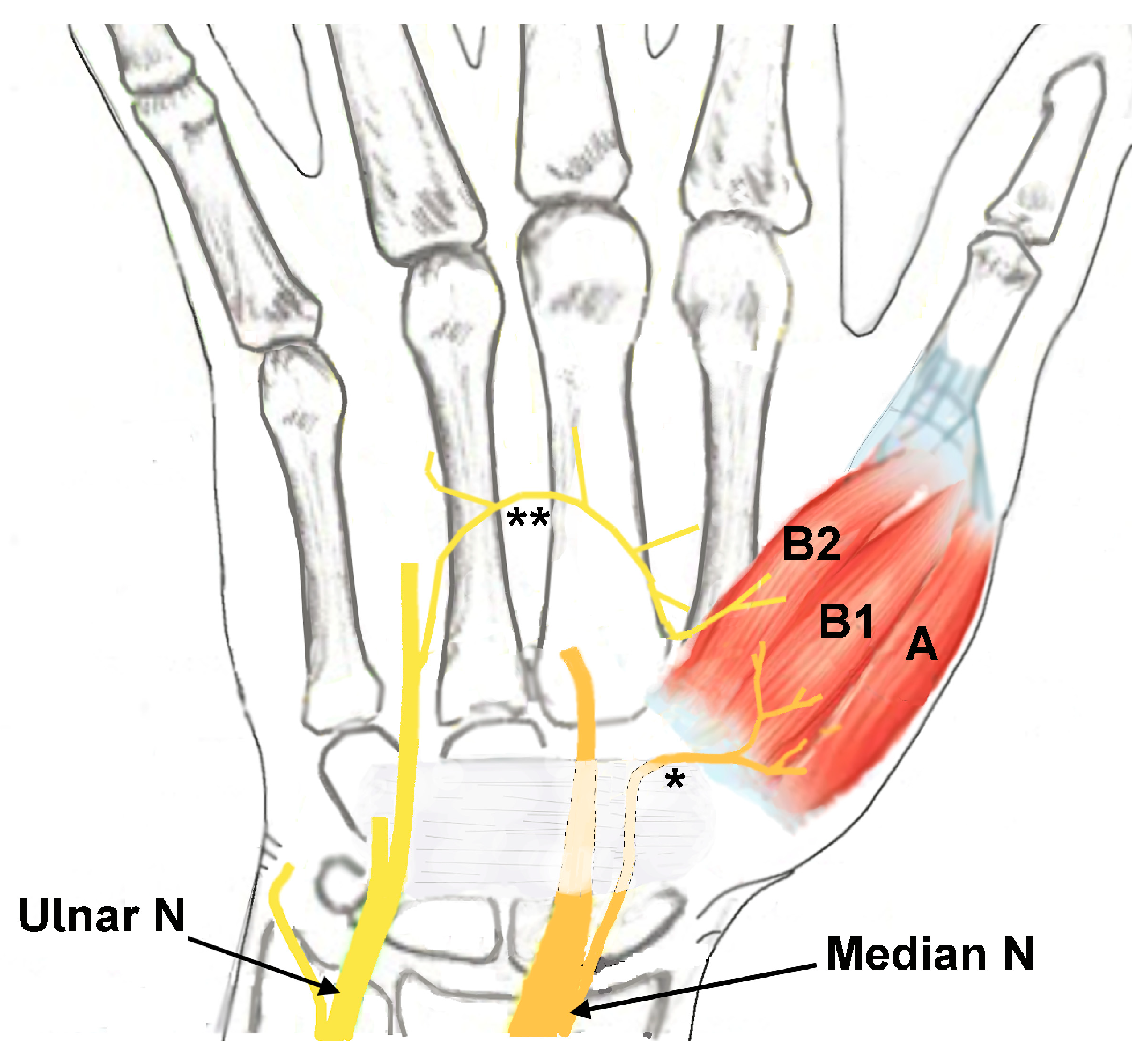
1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Metrics Collected
2.3. Statistical Analysis
2.4. Institutional Review Board Approval of Research
3. Results
3.1. Demographics
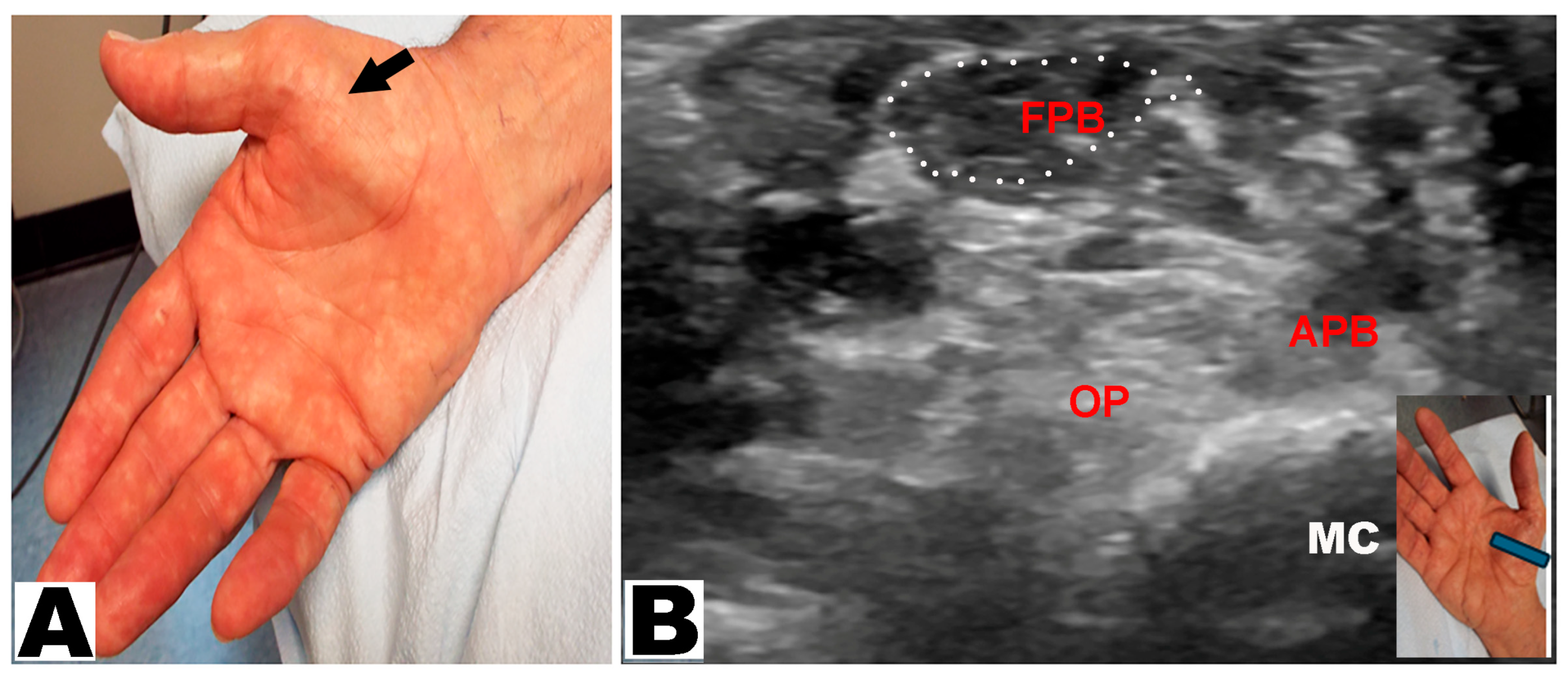
3.2. Neurological Examination
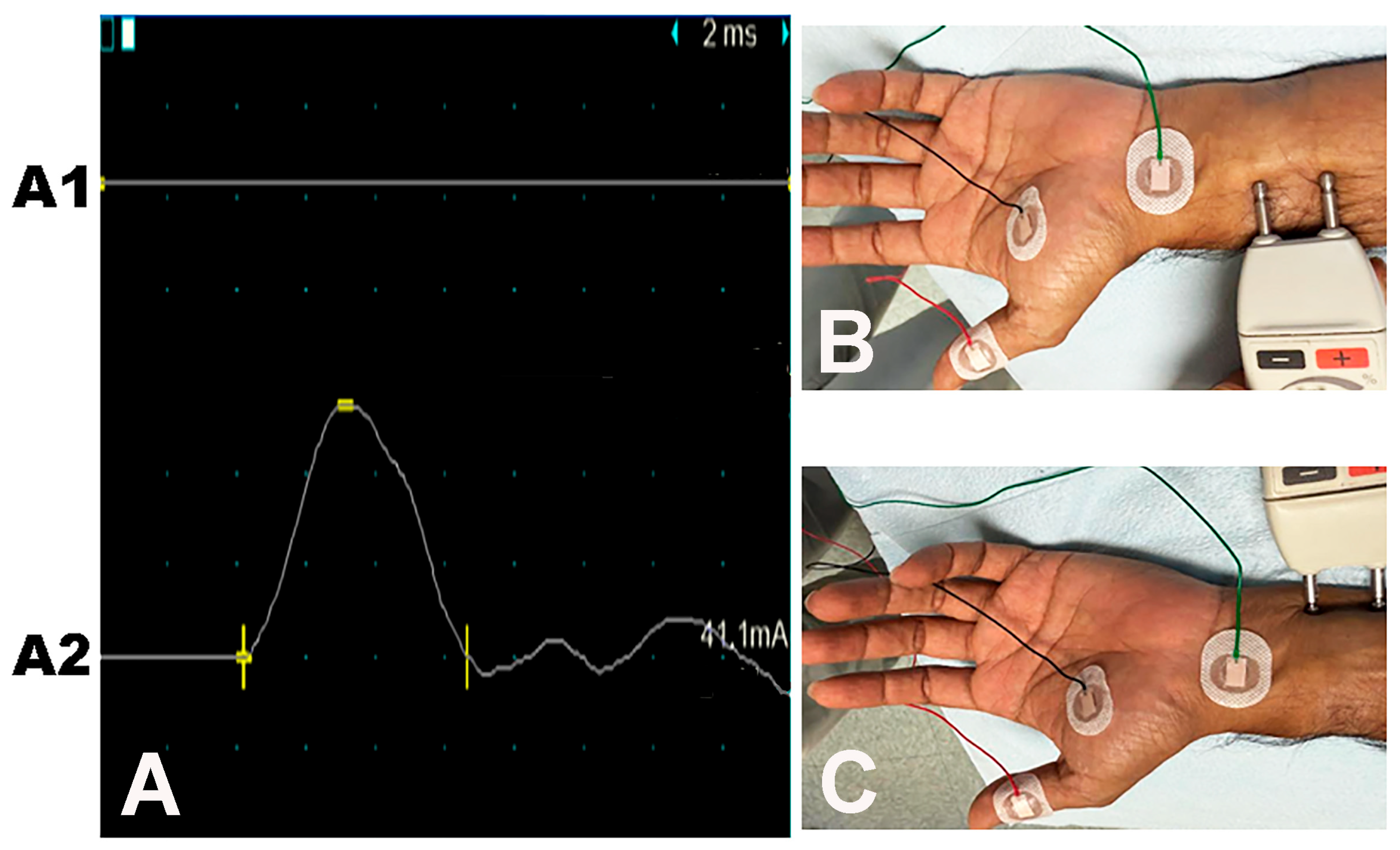
3.3. Electrodiagnostic Studies
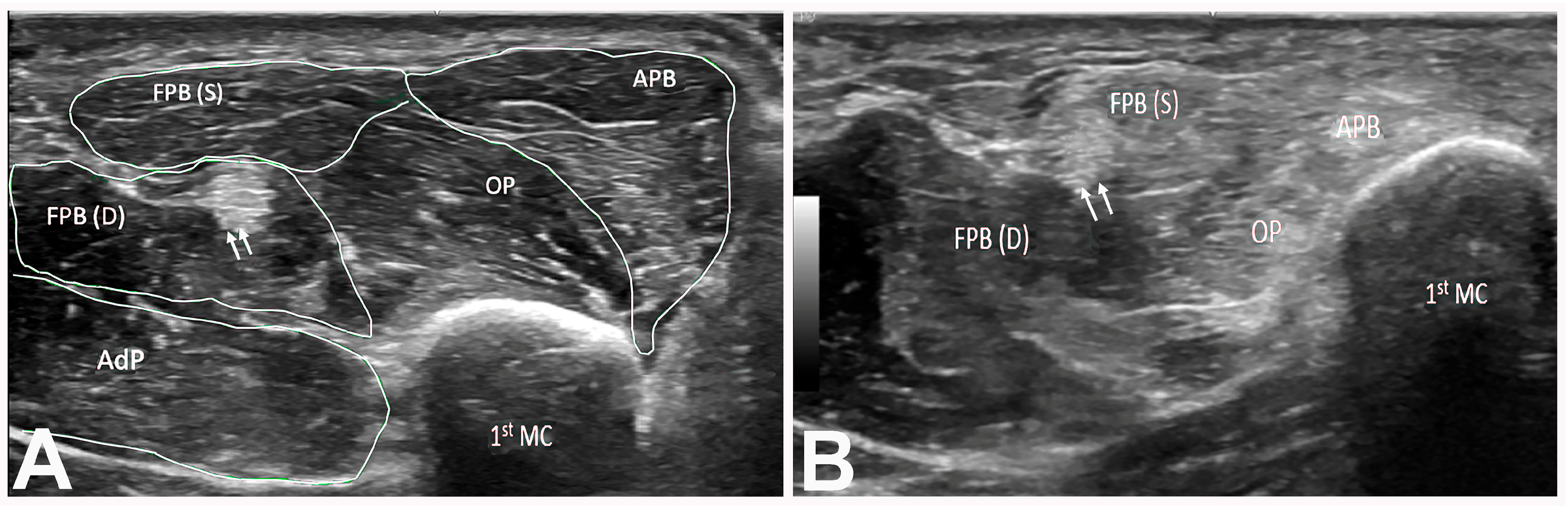
3.4. Ultrasound Studies
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Luxenburg, D.; Rizzo, M.G. Anatomy, Shoulder and Upper Limb, Hand Thenar Eminence; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Gupta, S.; Michelsen-Jost, H. Anatomy and function of the thenar muscles. Hand Clin. 2012, 28, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Caetano, E.B.; Nakamichi, Y.d.C.; de Andrade, R.A.; Sawada, M.M.; Nakasone, M.T.; Vieira, L.A.; Sabongi, R.G. Flexor pollicis brevis muscle. Anatomical study and clinical implications. Open Orthop. J. 2017, 11, 1321–1329. [Google Scholar] [CrossRef]
- Grechenig, W.; Peicha, G.; Weiglein, A.; Tesch, P.; Lawrence, K.; Mayr, J.; Preidler, K.W. Sonographic evaluation of the thenar compartment musculature. J. Ultrasound Med. 2000, 19, 733–741. [Google Scholar] [CrossRef][Green Version]
- Fernandes, C.H.; Meirelles, L.M.; Neto, J.R.; Nakachima, L.R.; dos Santos, J.B.G.; Faloppa, F. Carpal tunnel syndrome with thenar atrophy: Evaluation of the pinch and grip strength in patients undergoing surgical treatment. Hand 2013, 8, 60–63. [Google Scholar] [CrossRef] [PubMed]
- Hunt, J.R. Neuritis of the thenar branch of the median nerve: A well-defined type of atrophy of the hand. Trans. Am. Neurol. Assoc. 1909, 35, 184. [Google Scholar]
- Wartenberg, R. Partial thenar atrophy. Arch. Neur Psych. 1939, 42, 373–394. [Google Scholar] [CrossRef]
- Ticku, H.; Katirji, B. Clinical reasoning: A 55-year-old woman with painless hand weakness and atrophy. Neurology 2024, 103, e209561. [Google Scholar] [CrossRef]
- Stoian, A.; Motataianu, A.; Bajko, Z.; Balasa, A. Guillain-Barre and acute transverse myelitis overlap syndrome following obstetric surgery. J. Crit. Care Med. 2020, 6, 74–79. [Google Scholar] [CrossRef]
- Voermans, N.C.; Schelhaas, H.J.; Munneke, M.; Zwarts, M.J. Dissociated small hand muscle atrophy in aging: The ‘senile hand’ is a split hand. Eur. J. Neurol. 2006, 13, 1381–1384. [Google Scholar] [CrossRef] [PubMed]
- Tuncali, D.; Barutcu, A.Y.; Terzioglu, A.; Uludag, K.; Aslan, G. The thenar index: An objective assessment and classification of thenar atrophy based on static hand imprints and clinical implications. Plast. Reconstr. Surg. 2006, 117, 1916–1926. [Google Scholar] [CrossRef] [PubMed]
- Cartwright, M.S.; Hobson-Webb, L.D.; Boon, A.J.; E Alter, K.; Hunt, C.H.; Flores, V.H.; A Werner, R.; Shook, S.J.; Thomas, T.D.; Primack, S.J.; et al. Evidence-based guideline: Neuromuscular ultrasound for the diagnosis of carpal tunnel syndrome. Muscle Nerve 2012, 46, 287–293. [Google Scholar] [CrossRef]
- Lee, H.; Jee, S.; Park, S.H.; Ahn, S.-C.; Im, J.; Sohn, M.K. Quantitative muscle ultrasonography in carpal tunnel syndrome. Ann. Rehabil. Med. 2016, 40, 1048–1056. [Google Scholar] [CrossRef]
- Simon, N.G.; Ralph, J.W.; Lomen-Hoerth, C.; Poncelet, A.N.; Vucic, S.; Kiernan, M.C.; Kliot, M. Quantitative ultrasound of denervated hand muscles. Muscle Nerve 2015, 52, 221–230. [Google Scholar] [CrossRef]
- Pedrianes-Martin, P.B.; Hernanz-Rodriguez, G.M.; Gonzalez-Martin, J.M.; Perez-Valera, M.; De Pablos-Velasco, P.L. Ultrasonographic size of the thenar muscles of the nondominant hand correlates with total body lean mass in healthy subjects. Acad. Radiol. 2021, 28, 517–523. [Google Scholar] [CrossRef] [PubMed]
- Nagura, I.; Kanatani, T.; Harada, Y.; Takase, F.; Inui, A.; Mifune, Y.; Kuroda, R. Preoperative evaluation of thenar muscles in carpal tunnel syndrome by ultrasonography. Hand Clin. 2022, 38, 55–58. [Google Scholar] [CrossRef] [PubMed]
- Misirlioglu, T.O.; Ozyemisci, T.O. Reliability of sonographic muscle thickness measurements of the thenar and hypothenar muscles. Muscle Nerve 2018, 57, E14–E17. [Google Scholar] [CrossRef] [PubMed]
- Iyer, V.G. Ultrasonography in patients with congenital thenar hypoplasia (Cavanagh syndrome) and co-morbid carpal tunnel syndrome. Clin. Neurophysiol. Pract. 2021, 6, 256–259. [Google Scholar] [CrossRef]
- Iyer, V.G. Clinical reasoning: A septuagenarian with painless ulceration on the fingertip. Neurology 2023, 101, e1473–e1477. [Google Scholar] [CrossRef]
- Dilokhuttakarn, T.; Naito, K.; Kinoshita, M.; Sugiyama, Y.; Goto, K.; Iwase, Y.; Kaneko, K. Evaluation of thenar muscles by MRI in carpal tunnel syndrome. Exp. Ther. Med. 2017, 14, 2025–2030. [Google Scholar] [CrossRef]
- Shields, L.B.E.; Iyer, V.G.; Kluthe, T.; Zhang, Y.P.; Shields, C.B. Carpal tunnel syndrome in the very elderly: Clinical, electrodiagnostic, and ultrasound features in a cohort of 187 patients. Neurol. Int. 2025, 17, 137. [Google Scholar] [CrossRef]
- Iyer, V.G. Understanding nerve conduction and electromyographic studies. Hand Clin. 1993, 9, 273–287. [Google Scholar] [CrossRef]
- Hirani, S. An update to the present carpal tunnel syndrome (CTS) nerve conduction grading tool. Int. Arch. Clin. Physiol. 2020, 2, 006. [Google Scholar]
- Bland, J.D. A neurophysiological grading scale for carpal tunnel syndrome. Muscle Nerve 2000, 23, 1280–1283. [Google Scholar] [CrossRef]
- Wijntjes, J.; Saris, C.; Doorduin, J.; van Alfen, N.; van Engelen, B.; Mul, K. Improving Heckmatt muscle ultrasound grading scale through Rasch analysis. Neuromuscul. Disord. 2024, 42, 14–21. [Google Scholar] [CrossRef]
- Moreta, M.C.; Fleet, A.; Reebye, R.; McKernan, G.; Berger, M.; Farag, J.; Munin, M.C. Reliability and validity of the modified Heckmatt scale in evaluating muscle changes with ultrasound in spasticity. Arch. Rehabil. Res. Clin. Transl. 2020, 2, 100071. [Google Scholar] [CrossRef] [PubMed]
- Seok, J.I. A beginner’s guide to peripheral nerve ultrasound. J. Clin. Neurophysiol. 2022, 24, 46–52. [Google Scholar] [CrossRef]
- Hollander, M.; Wolfe, D.A. Nonparametric Statistical Methods; John Wiley & Sons: New York, NY, USA, 1973. [Google Scholar]
- Shields, L.B.E.; Iyer, V.G.; Zhang, Y.P.; Shields, C.B. Proximal median nerve neuropathy: Electrodiagnostic and ultrasound findings in 62 patients. Front. Neurol. 2024, 15, 1468813. [Google Scholar] [CrossRef] [PubMed]
- Gronfors, H.; Makela, K.; Himanen, S.L. Shear wave velocity of the thenar muscle Is associated with the neurophysiologic severity of carpal tunnel syndrome. J. Clin. Neurophysiol. 2025; Online ahead of print. [Google Scholar] [CrossRef]
- Iida, N.; El Hor, H.; Larson, D.R.; Luetmer, M.T.; Laughlin, R.S.; Amadio, P.C. Elasticity characteristics of thenar muscles in carpal tunnel syndrome. Ultrasound Med. Biol. 2025, 51, 592–597. [Google Scholar] [CrossRef] [PubMed]
- Rayegani, S.M.; Malekmahmoodi, R.; Aalipour, K.; Nouri, F. The relationship between ultrasound and electrodiagnostic findings in relation of the severity of carpal tunnel syndrome. BMC Musculoskelet. Disord. 2024, 25, 864. [Google Scholar] [CrossRef]
- Heckmatt, J.Z.; Leeman, S.; Dubowitz, V. Ultrasound imaging in the diagnosis of muscle disease. J. Pediatr. 1982, 101, 656–660. [Google Scholar] [CrossRef] [PubMed]
- Vincenten, S.; Teeselink, S.; Voermans, N.; van Engelen, B.; Mul, K.; van Alfen, N. Establishing the role of muscle ultrasound as an imaging biomarker in facioscapulohumeral muscular dystrophy. Neuromuscul. Disord. 2023, 33, 936–944. [Google Scholar] [CrossRef] [PubMed]
- Wijntjes, J.; van Alfren, N. Muscle ultrasound: Present state and future opportunities. Muscle Nerve 2021, 63, 455–466. [Google Scholar] [CrossRef] [PubMed]



| Type of Thenar Atrophy | Description | Mechanism |
|---|---|---|
| Total | APB, OP, and FPB muscles are atrophic, leading to a “flat” thenar eminence | 1. Severe CTS: median nerve innervates all thenar muscles, including both heads of the FPB muscle |
| 2. Severe CTS and ulnar neuropathy causing atrophy of all thenar muscles, including both heads of the FPB muscle | ||
| 3. T1 radiculopathy causing atrophy of all thenar muscles, including both heads of the FPB muscle | ||
| Partial | APB and OP muscles are atrophic with an intact FPB muscle visible in the distal/medial part of the thenar eminence | 1. Severe CTS with intact deep head of the FPB (innervated by the ulnar nerve) |
| 2. Severe CTS with an intact FPB muscle due to ulnar innervation of both heads | ||
| Partial with hypertrophy of the FPB | APB and OP muscles are atrophic, causing the lateral part of thenar eminence to be flat with a prominent “bulge” on the medial aspect from a large FPB muscle | Severe CTS with an intact FPB muscle compensating for the loss of the OP muscle; more likely when the FPB muscle is entirely supplied by the ulnar nerve |
| Characteristics | Number of Patients (n = 197) |
|---|---|
| Age (mean) | 68.8 years (Range: 15–92 years) |
| Sex (%) | |
| Male | 97 (49.2) |
| Female | 100 (50.8) |
| Side (%) | |
| Right | 109 (55.3) |
| Left | 59 (30.0) |
| Both | 29 (14.7) |
| Dominant hand (%) | |
| Right | 172 (87.3) |
| Left | 22 (11.2) |
| Ambidextrous | 3 (1.5) |
| Hand dominance corresponds with side of symptoms (%) | |
| Yes | 135 (68.5) |
| No | 62 (31.5) |
| Diabetes mellitus (%) | |
| Yes | 33 (16.8) |
| No | 164 (83.2) |
| History of carpal tunnel release = Yes (%) | 14 (6.2) |
| Number of Hands (n = 226) | |
|---|---|
| Thenar atrophy (%) | |
| Total | 52 (23.0) |
| Partial | 174 (77.0) |
| Prominent FPB = yes (%) | 44 (19.5) |
| Total atrophy | 0 (0%) |
| Partial atrophy | 44 (100%) |
| Weakness (%) | |
| APB | 226 (100.0) |
| OP | 226 (100.0) |
| FDI | 15 (6.6) |
| ADM | 6 (2.6) |
| FDP | 3 (1.3) |
| EDC | 2 (0.88) |
| FPL | 1 (0.44) |
| EPL | 1 (0.44) |
| Sensation loss = yes (%) * | 217 (96.0) |
| Severity * | Criteria | Total Number of Hands (n = 226) |
|---|---|---|
| Mild | Only sensory fascicles affected | 3 (1.3%) |
| Moderate | Sensory and motor fascicles affected | 0 (0%) |
| Moderately severe | Sensory and motor fascicles affected with motor unit changes (increase in polyphasic units) in APB | 1 (0.44%) |
| Severe | Loss of SNAP and loss of or decrease in amplitude CMAP of APB < 1 mV, along with needle EMG showing denervation of APB | 220 (97.3%) |
| Metrics | Number of Hands (n = 226) |
|---|---|
| CMAP of APB (%) | |
| Absent | 186 (82.3) |
| 0.1–2.0 mV | 36 (15.9) |
| 2.01–4.0 mV | 4 (1.8) |
| >4.0 mV | 0 (0) |
| CMAP of second lumbrical (%) (n = 188) | |
| Absent | 106 (56.4) |
| 0.1–2.0 mV | 82 (43.6) |
| 2.01–4.0 mV | 0 (0) |
| >4.0 mV | 0 (0) |
| Distal motor latency of APB (%) | |
| Absent | 186 (82.3) |
| 0.1–6.0 ms | 10 (4.4) |
| >6.1 ms | 30 (13.3) |
| Distal motor latency of second lumbrical (%) (n = 188) | |
| Absent | 106 (56.4) |
| 0.1–6.0 ms | 17 (9.0) |
| >6.1 ms | 65 (34.6) |
| Motor unit recruitment of APB (%) * | |
| Normal | 2 (0.88) |
| Decreased | 104 (46.2) |
| Absent | 119 (52.9) |
| Fibrillations/positive waves of APB (%) * | |
| No | 53 (23.6) |
| Yes | 172 (76.4) |
| Ulnar nerve neuropathy on side of thenar atrophy (%) (n = 94 [41.6]) | |
| Total atrophy | 35 (37.2) |
| Partial atrophy | 59 (62.8) |
| Ulnar nerve neuropathy on side of thenar atrophy with partial atrophy (%) (n = 59) | |
| Without FPB muscle hypertrophy | 44 (74.6) |
| With FPB muscle hypertrophy | 15 (25.4) |
| Number of Hands (n = 226) | |
|---|---|
| SNAP amplitude median nerve (%) | |
| Absent | 212 (93.8) |
| 1–10.0 μV | 5 (2.2) |
| 10.01–20.0 μV | 3 (1.3) |
| >20.0 μV | 6 (2.6) |
| SNAP latency median nerve (%) | |
| Absent | 212 (93.8) |
| 3.5–6.0 ms | 14 (6.2) |
| >6.0 ms | 0 (0) |
| Number of Hands (n = 226) | |
|---|---|
| APB hyperechoic | |
| Yes | 225 (99.6) |
| No | 1 (0.44) |
| OP hyperechoic | |
| Yes | 225 (99.6) |
| No | 1 (0.44) |
| FPB hyperechoic | |
| Yes | 29 (12.8) |
| No | 197 (87.2) |
| Wrist CSA | |
| <10 mm2 | 3 (1.3) |
| 10–20 mm2 | 104 (46.0) |
| >20 mm2 | 119 (52.7) |
| Forearm CSA | |
| 3–6 mm2 | 102 (45.1) |
| 7–10 mm2 | 104 (46.0) |
| >10 mm2 | 20 (8.9) |
| Grade | Description | Total Number of Hands (n = 226) | Total Thenar Atrophy (n = 174) | Partial Thenar Atrophy (n = 52) |
|---|---|---|---|---|
| 1 | Normal | 1 (0.44%) | 1 (100%) | 0 (0%) |
| 2 | Increased muscle echogenicity (with normal architecture) with normal bone reflection | 21 (9.3%) | 2 (9.5%) | 19 (90.5%) |
| 3 | Further increased muscle echogenicity (with some loss of architecture) with reduced bone reflection | 152 (67.3%) | 23 (15.1%) | 129 (84.9%) |
| 4 | Markedly increased muscle echogenicity (with total loss of architecture) with absent bone reflection | 52 (23.0%) | 26 (50.0%) | 26 (50.0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shields, L.B.E.; Iyer, V.G.; Furmanek, S.; Zhang, Y.P.; Shields, C.B. Thenar Muscle Atrophy: Clinical, Electrodiagnostic, and Ultrasound Features in 197 Patients. Neurol. Int. 2025, 17, 201. https://doi.org/10.3390/neurolint17120201
Shields LBE, Iyer VG, Furmanek S, Zhang YP, Shields CB. Thenar Muscle Atrophy: Clinical, Electrodiagnostic, and Ultrasound Features in 197 Patients. Neurology International. 2025; 17(12):201. https://doi.org/10.3390/neurolint17120201
Chicago/Turabian StyleShields, Lisa B. E., Vasudeva G. Iyer, Stephen Furmanek, Yi Ping Zhang, and Christopher B. Shields. 2025. "Thenar Muscle Atrophy: Clinical, Electrodiagnostic, and Ultrasound Features in 197 Patients" Neurology International 17, no. 12: 201. https://doi.org/10.3390/neurolint17120201
APA StyleShields, L. B. E., Iyer, V. G., Furmanek, S., Zhang, Y. P., & Shields, C. B. (2025). Thenar Muscle Atrophy: Clinical, Electrodiagnostic, and Ultrasound Features in 197 Patients. Neurology International, 17(12), 201. https://doi.org/10.3390/neurolint17120201






