Rare Pediatric Posterior Stroke Case Report with Discussion of Brainstem Lesions
Abstract
1. Background
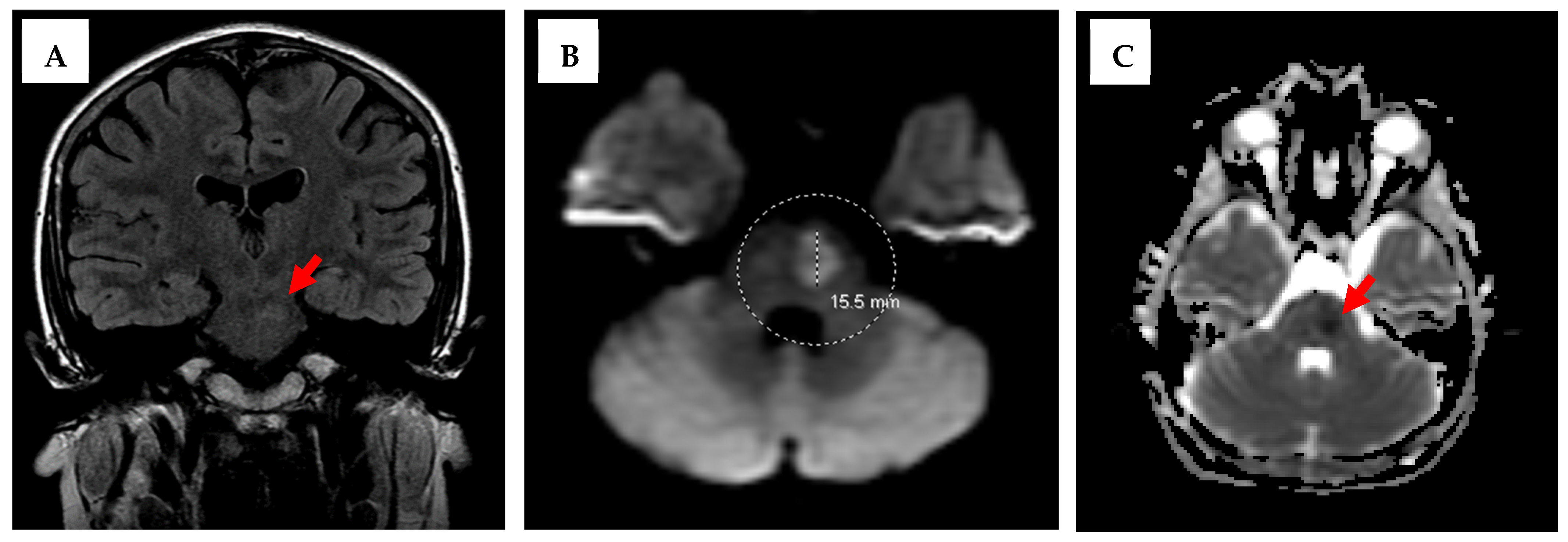
2. Case
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Broderick, J.; Talbot, G.T.; Prenger, E.; Leach, A.; Brott, T. Stroke in children within a major metropolitan area: The surprising importance of intracerebral hemorrhage. J. Child. Neurol. 1993, 8, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Schoenberg, B.S.; Mellinger, J.F.; Schoenberg, D.G. Cerebrovascular disease in infants and children: A study of incidence, clinical features, and survival. Neurology 1978, 28, 763–768. [Google Scholar] [CrossRef] [PubMed]
- Earley, C.J.; Kittner, S.J.; Feeser, B.R.; Gardner, J.; Epstein, A.; Wozniak, M.A.; Wityk, R.; Stern, B.J.; Price, T.R.; Macko, R.F.; et al. Stroke in children and sickle-cell disease: Baltimore-Washington Cooperative Young Stroke Study. Neurology 1998, 51, 169–176. [Google Scholar] [CrossRef]
- Fullerton, H.J.; Wu, Y.W.; Zhao, S.; Johnston, S.C. Risk of stroke in children: Ethnic and gender disparities. Neurology 2003, 61, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Zahuranec, D.B.; Brown, D.L.; Lisabeth, L.D.; Morgenstern, L.B. Is it time for a large, collaborative study of pediatric stroke? Stroke 2005, 36, 1825–1829. [Google Scholar] [CrossRef] [PubMed]
- Khalaf, A.; Iv, M.; Fullerton, H.; Wintermark, M. Pediatric Stroke Imaging. Pediatr Neurol. 2018, 86, 5–18. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fink, M.; Slavova, N.; Grunt, S.; Perret, E.; Regényi, M.; Steinlin, M.; Bigi, S. Posterior Arterial Ischemic Stroke in Childhood: Clinical Features and Neuroimaging Characteristics. AHA J Stroke. 2019, 50, 2329–2335. [Google Scholar] [CrossRef] [PubMed]
- Carey, S.; Wrogemann, J.; Booth, F.A.; Rafay, M.F. Epidemiology, Clinical Presentation, and Prognosis of Posterior Circulation Ischemic Stroke in Children. Pediatr. Neurol. 2017, 74, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Carey, S.; Rafay, M. Pediatric Posterior Arterial Ischemic Stroke: A Summary of Current Knowledge. Pediatr. Stroke. 2021, 2, 1–38. Available online: https://pediatricstrokejournal.com/pediatric-posterior-arterial-ischemic-stroke-a-summary-of-current-knowledge/ (accessed on 2 June 2025).
- Baldovsky, M.D.; Okada, P.J. Pediatric stroke in the emergency department. J. Am. Coll. Emerg. Physicians Open. 2020, 1, 1578–1586. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dia, A.R.; Cifu, A.S.; Shah, A.P. Management of Patients with a Patent Foramen Ovale with History of Stroke or TIA. JAMA 2021, 325, 81–82. [Google Scholar] [CrossRef] [PubMed]
- Mojadidi, M.K.; Zaman, M.O.; Elgendy, I.Y.; Mahmoud, A.N.; Patel, N.K.; Agarwal, N.; Tobis, J.M.; Meier, B. Cryptogenic Stroke and Patent Foramen Ovale. J. Am. Coll. Cardiol. 2018, 71, 1035–1043. [Google Scholar] [CrossRef] [PubMed]
- Sposato, L.A.; Albin, C.S.W.; Elkind, M.S.V.; Kamel, H.; Saver, J.L. Patent Foramen Ovale Management for Secondary Stroke Prevention: State-of-the-Art Appraisal of Current Evidence. Stroke 2024, 55, 236–247. [Google Scholar] [CrossRef] [PubMed]
- Saharan, S.; Vettukattil, J.; Bhat, A.; Amula, V.; Bansal, M.; Chowdhury, D.; Dyamenahalli, U.; Gupta, S.K.; Das, B.; Susheel Kumar, T.K.; et al. Patent foramen ovale in children: Unique pediatric challenges and lessons learned from adult literature. Ann. Pediatr. Cardiol. 2022, 15, 44–52. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Karumuri, R. The continued need for pediatric management guidelines for cryptogenic stroke and patent foramen ovale. Neurology 2025, 104, 1024–1026. [Google Scholar] [CrossRef]
- Kent, D.M.; Saver, J.L.; Ruthazer, R.; Furlan, A.J.; Reisman, M.; Carroll, J.D.; Smalling, R.W.; Jüni, P.; Mattle, H.P.; Meier, B.; et al. Risk of Paradoxical Embolism (RoPE)-Estimated Attributable Fraction Correlates with the Benefit of Patent Foramen Ovale Closure: An Analysis of 3 Trials. Stroke 2020, 51, 3119–3123. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gates, P. The rule of 4 of the brainstem: A simplified method for understanding brainstem anatomy and brainstem vascular syndromes for the non-neurologist. Intern Med. J. 2005, 35, 263–266. [Google Scholar] [CrossRef] [PubMed]


| Types | Examples |
|---|---|
| Arteriopathies |
|
| Cardiac Problems |
|
| Hematologic/Hypercoagulable states/Thrombophilia |
|
| Genetic/Metabolic Disorders |
|
| Infection |
|
| Neonates (Perinatal stroke, 0–28 days) | Note: Neonates can present with seizure or seizure-like symptoms, and 10% of term neonatal seizures are secondary to perinatal strokes. |
| Other |
|
| Brainstem | Localization | Blood Supply | Cranial Nerves (CN) | Symptomology from CN Lesion | Structures & Symptomology from Structure Lesion (Applies to Entire Brainstem, Not Specific to One Area) |
|---|---|---|---|---|---|
| Midbrain | Medial | Posterior cerebral artery (PCA) | CN 3 (oculomotor) CN 4 (trochlear) |
| Medial Structures (primarily motor):
|
| Side (Lateral) | PCA | None | - | ||
| Pons | Medial | Anterior inferior cerebellar artery (AICA) | CN 6 (abducens) |
| |
| Side (Lateral) | Basilar artery | CN 5 (trigeminal) CN 7 (facial) CN 8 (vestibulocochlear) |
| Side (Lateral) Structures (primarily sensory):
| |
| Medulla | Medial | Posterior inferior cerebellar artery (PICA) | CN 12 (hypoglossal) |
| |
| Side (Lateral) | Anterior spinal artery (ASA) | CN 9 (glossopharyngeal) CN 10 (vagus) CN 11 (accessory) |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gould, L.A.; Carman, M.; Rossi, G.; Dhillon, J. Rare Pediatric Posterior Stroke Case Report with Discussion of Brainstem Lesions. Neurol. Int. 2025, 17, 178. https://doi.org/10.3390/neurolint17110178
Gould LA, Carman M, Rossi G, Dhillon J. Rare Pediatric Posterior Stroke Case Report with Discussion of Brainstem Lesions. Neurology International. 2025; 17(11):178. https://doi.org/10.3390/neurolint17110178
Chicago/Turabian StyleGould, Lauren A., Matthew Carman, Gian Rossi, and Jasvinder Dhillon. 2025. "Rare Pediatric Posterior Stroke Case Report with Discussion of Brainstem Lesions" Neurology International 17, no. 11: 178. https://doi.org/10.3390/neurolint17110178
APA StyleGould, L. A., Carman, M., Rossi, G., & Dhillon, J. (2025). Rare Pediatric Posterior Stroke Case Report with Discussion of Brainstem Lesions. Neurology International, 17(11), 178. https://doi.org/10.3390/neurolint17110178







