Malignant Ependymoblastoma Mimicking a Benign Pilocytic Astrocytoma
Abstract
1. Introduction
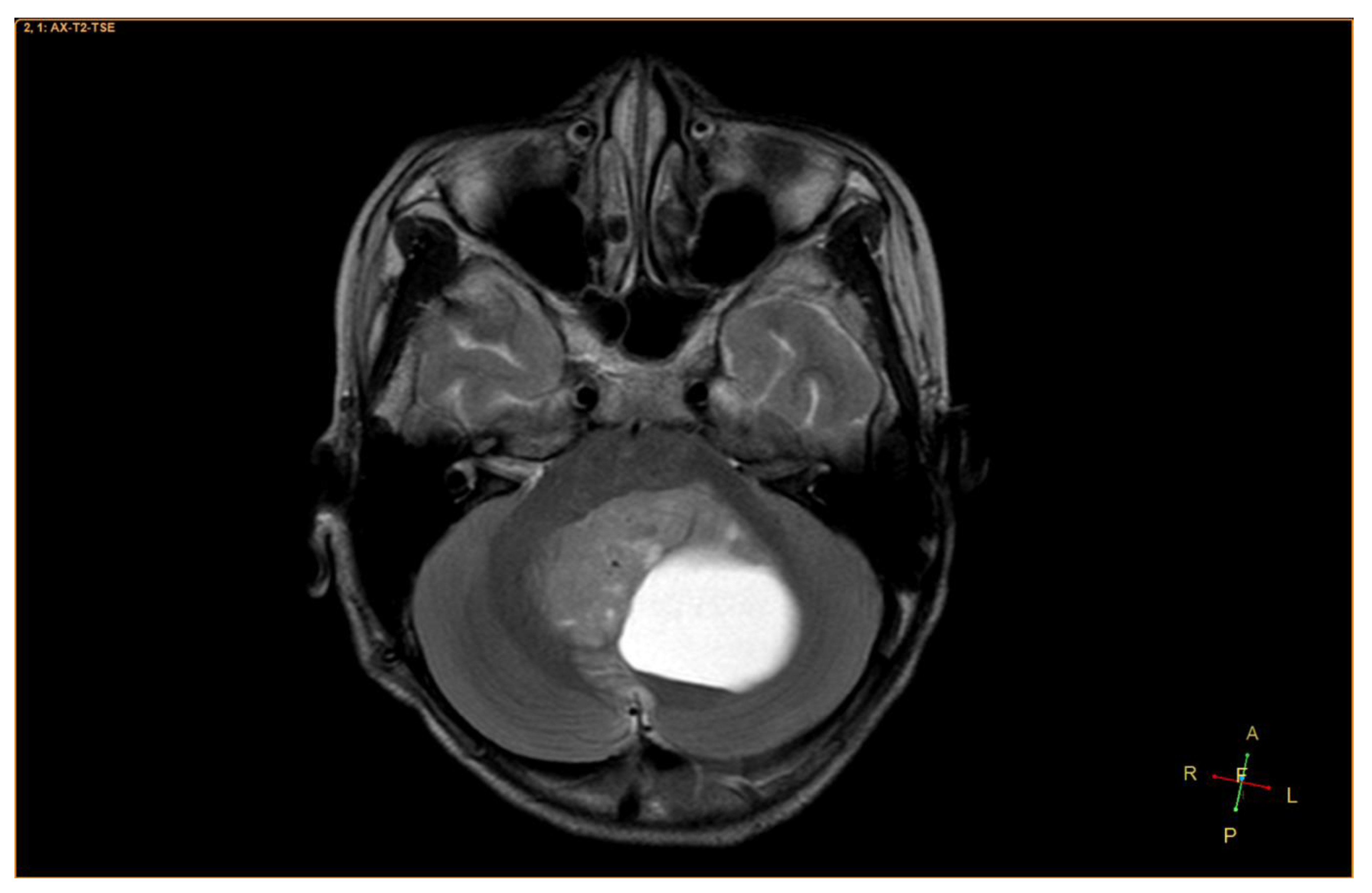
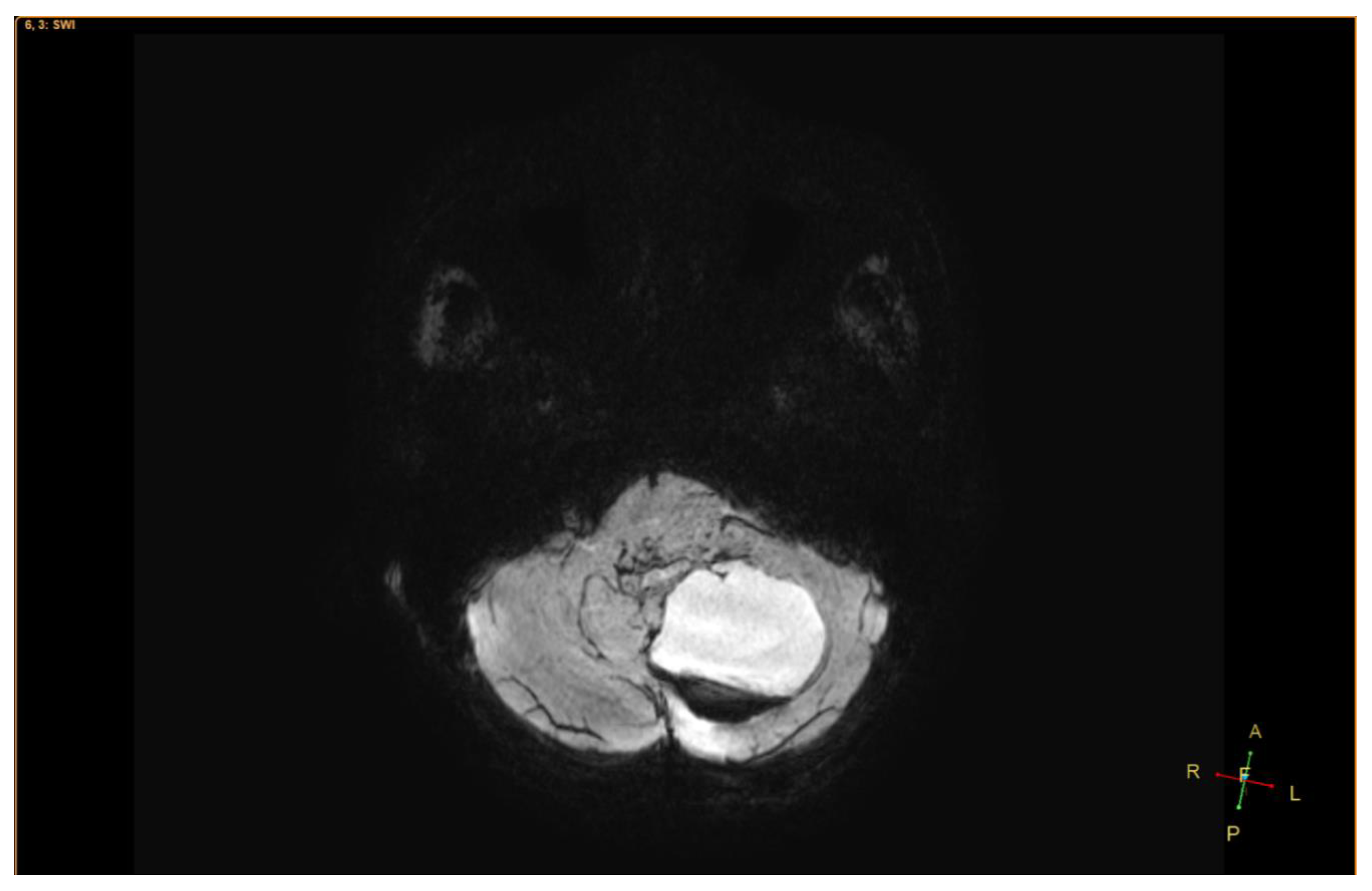
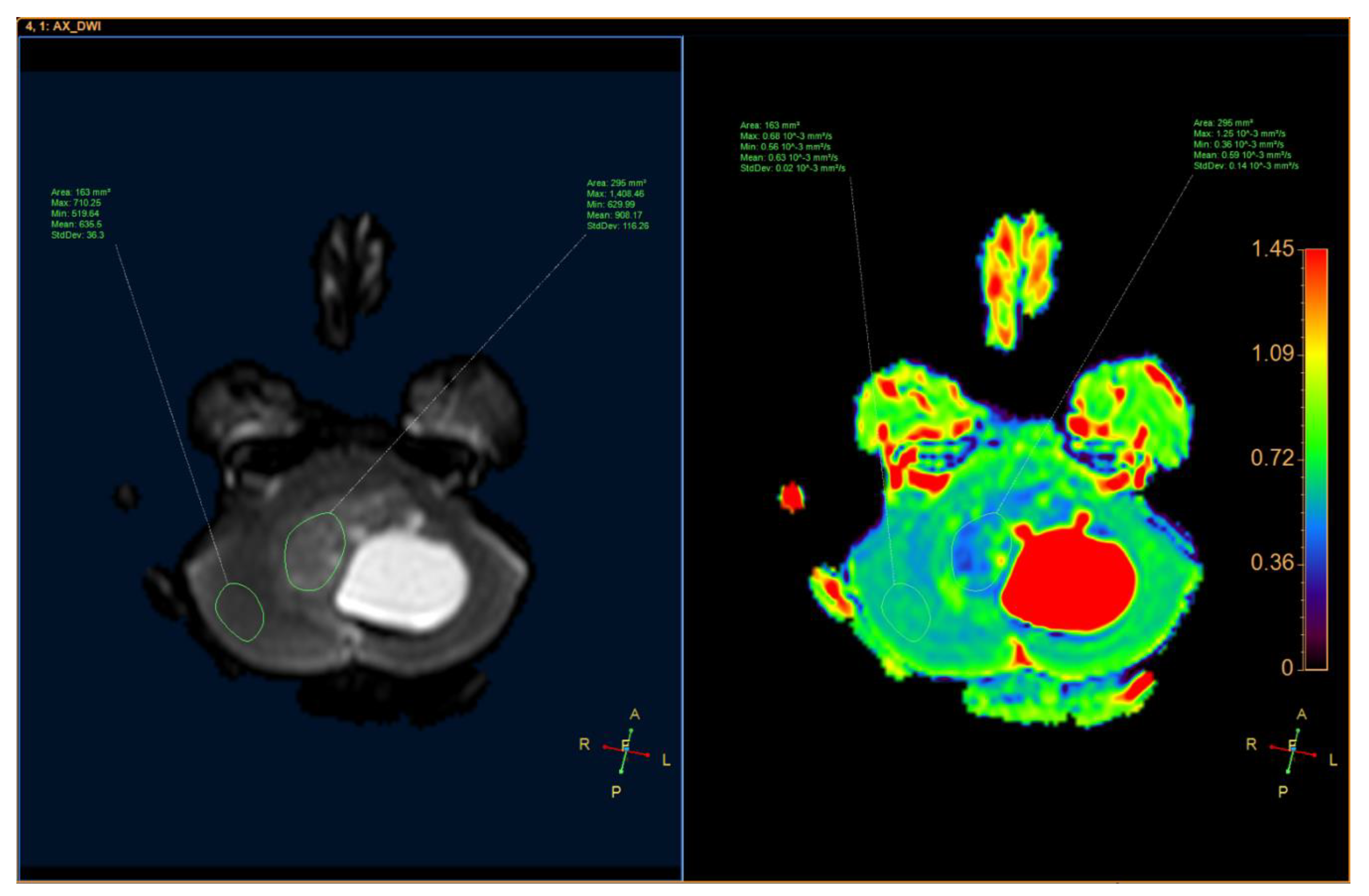
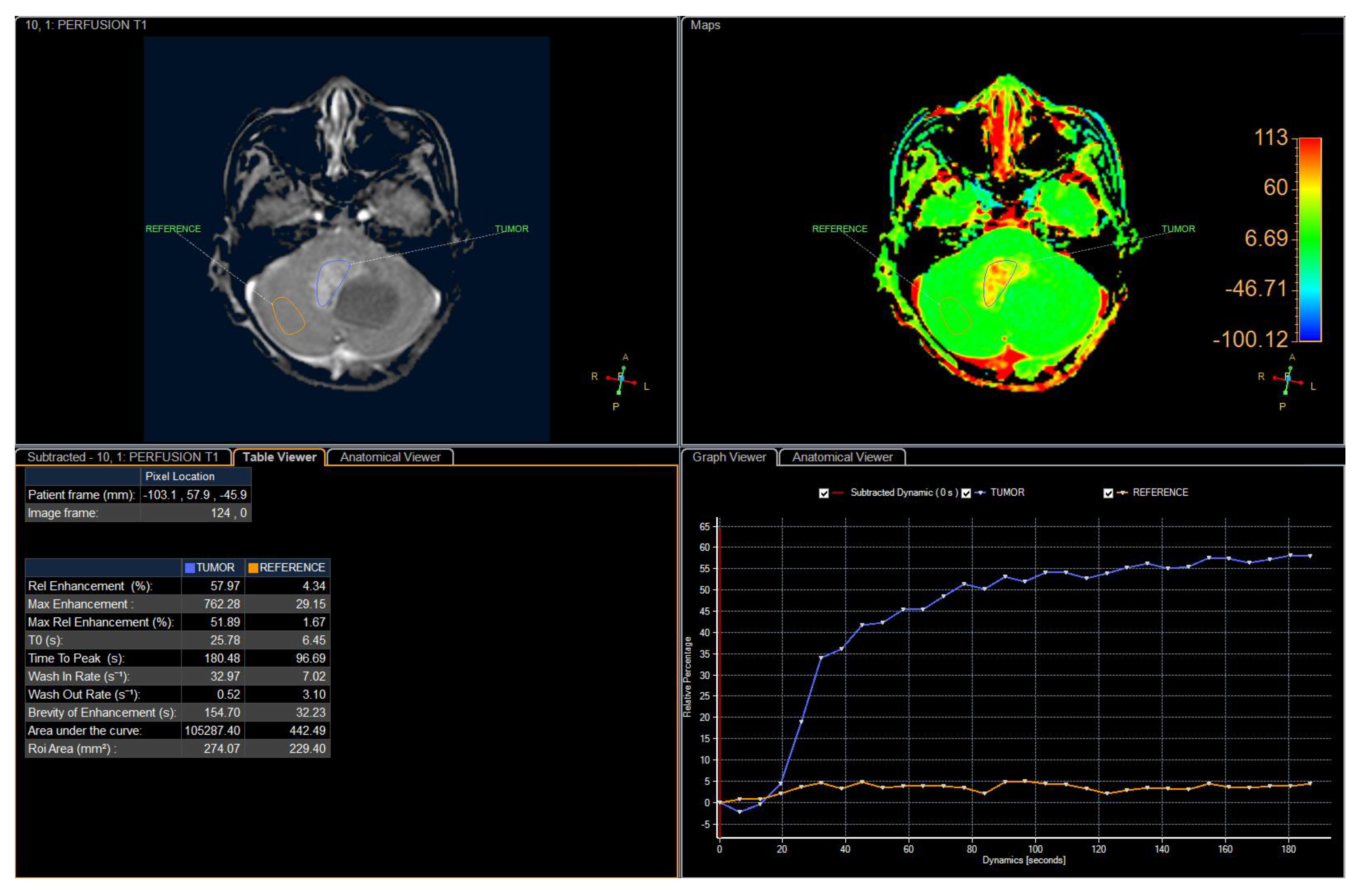
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bailey, P.; Cushing, H. A Classification of the Tumors of the Glioma Group on a Histogenetic Basis with a Correlated Study of Prognosis; J. B. Lippincott & Co.: Philadelphia, PA, USA, 1926. [Google Scholar]
- Rubinstein, L.J. The definition of the ependymoblastoma. Arch. Pathol. 1970, 90, 35–45. [Google Scholar] [PubMed]
- Louis, D.N.; Ohgaki, H.; Wiestler, O.D.; Cavenee, W.K.; Burger, P.C.; Jouvet, A.; Scheithauer, B.W.; Kleihues, P. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007, 114, 97–109. [Google Scholar] [CrossRef] [PubMed]
- Isaacs, H. Fetal brain tumors: A review of 154 cases. Am. J. Perinatol. 2009, 26, 453–466. [Google Scholar] [CrossRef]
- Mørk, S.J.; Rubinstein, L.J. Ependymoblastoma. A reappraisal of a rare embryonal tumor. Cancer 1985, 55, 1536–1542. [Google Scholar] [CrossRef]
- Amit, S.; Chand, P.; Pantola, C.; Agarwal, A. Ependymoblastoma in an adult: A diagnostic challenge on cytology. BMJ Case Rep. 2011, 2011, bcr0920114746. [Google Scholar] [CrossRef] [PubMed]
- Ding, D.; Zhao, A.; Qiu, B.; Xing, D.; Guan, G.; Guo, Z. Ependymoblastoma with cystic change in a child. J. Neurosurg. Pediatr. 2014, 13, 658–665. [Google Scholar] [CrossRef] [PubMed]
- Nowak, J.; Seidel, C.; Berg, F.; Pietsch, T.; Friedrich, C.; von Hoff, K.; Rutkowski, S.; Warmuth-Metz, M. MRI characteristics of ependymoblastoma: Results from 22 centrally reviewed cases. AJNR Am. J. Neuroradiol. 2014, 35, 1996–2001. [Google Scholar] [CrossRef] [PubMed]
- Nowak, J.; Seidel, C.; Pietsch, T.; Alkonyi, B.; Fuss, T.L.; Friedrich, C.; von Hoff, K.; Rutkowski, S.; Warmuth-Metz, M. Systematic comparison of MRI findings in pediatric ependymoblastoma with ependymoma and CNS primitive neuroectodermal tumor not otherwise specified. Neuro Oncol. 2015, 17, 1157–1165. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gard, A.P.; Perry, D.A.; Abdessalam, S.; Bowdino, B.S. Sacrococcygeal ependymoblastoma. Childs Nerv. Syst. 2015, 31, 2215–2216. [Google Scholar] [CrossRef] [PubMed]
- Smolle, E.; Smolle, M.; Ronaghi, F.; Rogatsch, H.; Moinfar, F.; Haybaeck, J. A case report of an ependymoblastoma in the rectovaginal space and a review of the literature. Anticancer Res. 2014, 34, 819–827. [Google Scholar] [PubMed]
- Morovic, A.; Damjanov, I. Neuroectodermal ovarian tumors: A brief overview. Histol. Histopathol. 2008, 23, 765–771. [Google Scholar] [PubMed]
- Gupta, A.; Dwivedi, T. A Simplified Overview of World Health Organization Classification Update of Central Nervous System Tumors 2016. J. Neurosci. Rural Pract. 2017, 8, 629–641. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.H.; Ko, S.F.; Chen, Y.L.; Wong, H.F.; Wai, Y.Y. Ependymoblastoma: CT and MRI demonstration. Clin. J. Radiol. 2002, 27, 21–25. [Google Scholar]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thong, P.M.; Minh Duc, N. Malignant Ependymoblastoma Mimicking a Benign Pilocytic Astrocytoma. Neurol. Int. 2020, 12, 41-47. https://doi.org/10.3390/neurolint12030010
Thong PM, Minh Duc N. Malignant Ependymoblastoma Mimicking a Benign Pilocytic Astrocytoma. Neurology International. 2020; 12(3):41-47. https://doi.org/10.3390/neurolint12030010
Chicago/Turabian StyleThong, Pham Minh, and Nguyen Minh Duc. 2020. "Malignant Ependymoblastoma Mimicking a Benign Pilocytic Astrocytoma" Neurology International 12, no. 3: 41-47. https://doi.org/10.3390/neurolint12030010
APA StyleThong, P. M., & Minh Duc, N. (2020). Malignant Ependymoblastoma Mimicking a Benign Pilocytic Astrocytoma. Neurology International, 12(3), 41-47. https://doi.org/10.3390/neurolint12030010





