How 5G Wireless (and Concomitant Technologies) Will Revolutionize Healthcare?
Abstract
:1. Introduction
If banking were like health care, automated teller machine (ATM) transactions would take not seconds but perhaps days or longer as a result of unavailable or misplaced records. If home building were like health care, carpenters, electricians, and plumbers each would work with different blueprints, with very little coordination. If shopping were like health care, product prices would not be posted, and the price charged would vary widely within the same store, depending on the source of payment. If automobile manufacturing were like health care, warranties for cars that require manufacturers to pay for defects would not exist. As a result, few factories would seek to monitor and improve production line performance and product quality. If airline travel were like health care, each pilot would be free to design his or her own preflight safety check, or not to perform one at all [2].
2. Challenges Posed by the Current Healthcare System
2.1. Challenges with EHRs
2.2. Lack of Universal Access
2.3. The Long-Term Chronic Care Burden
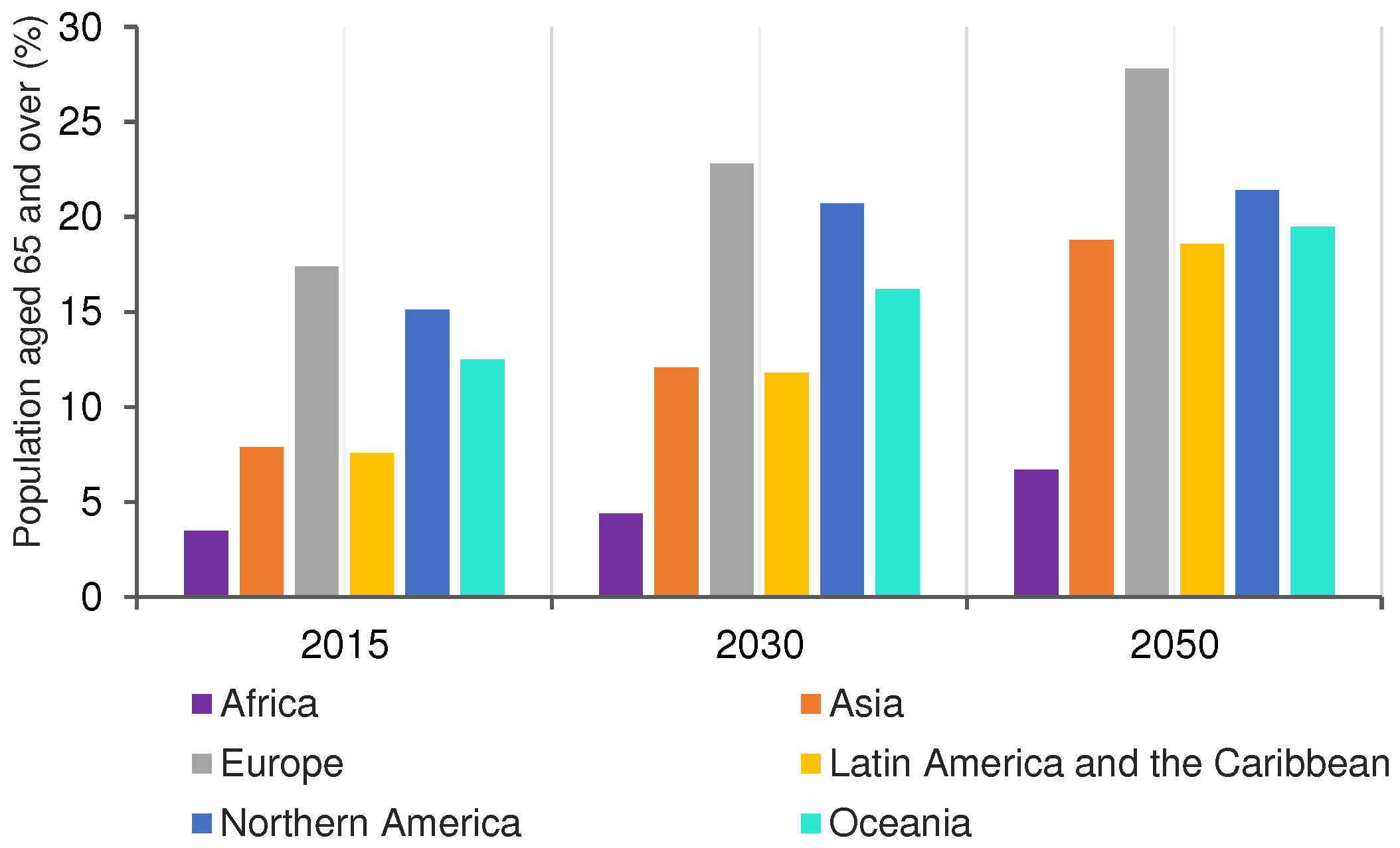
2.4. Challenges for Ageing Populations
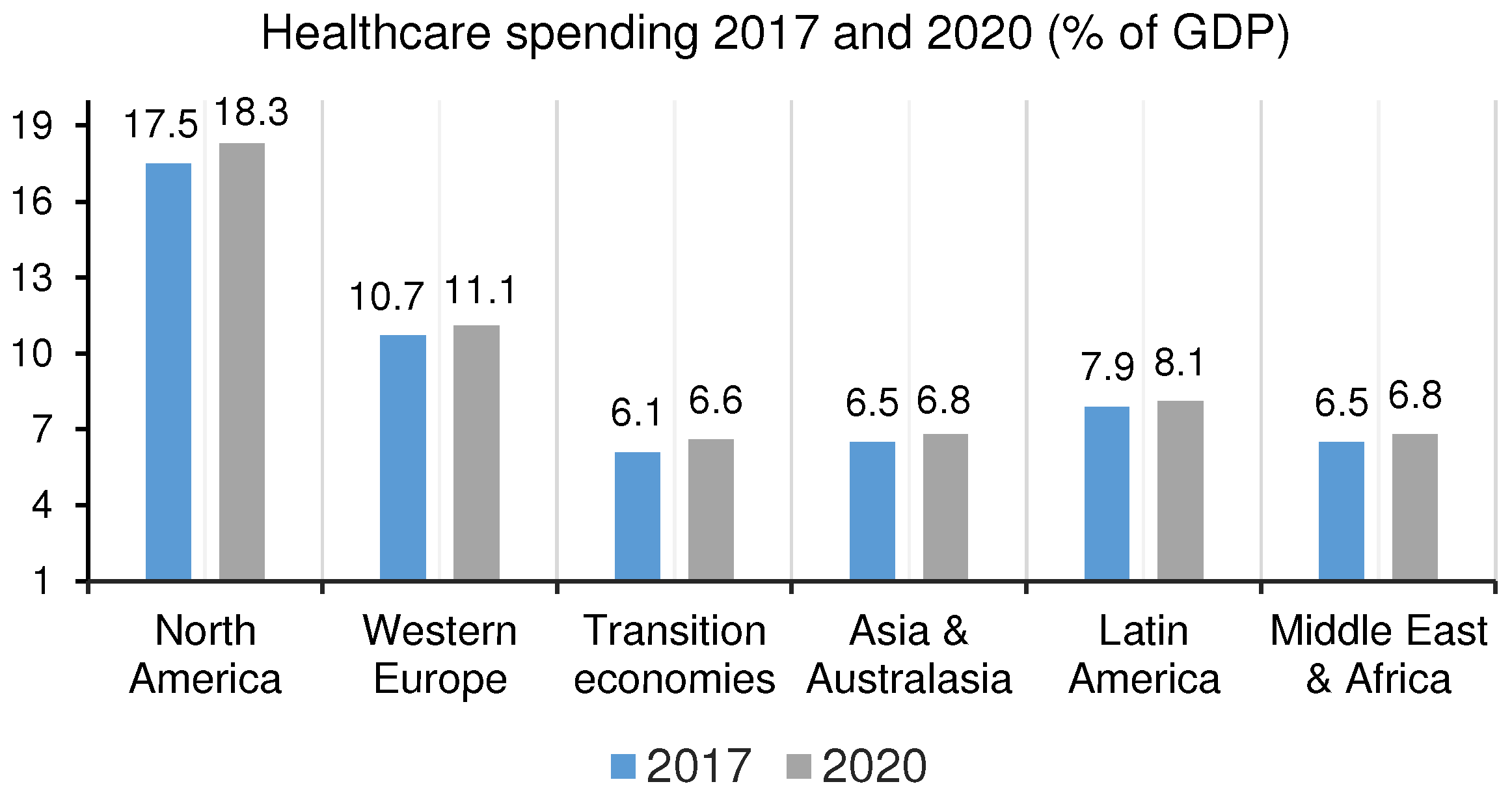
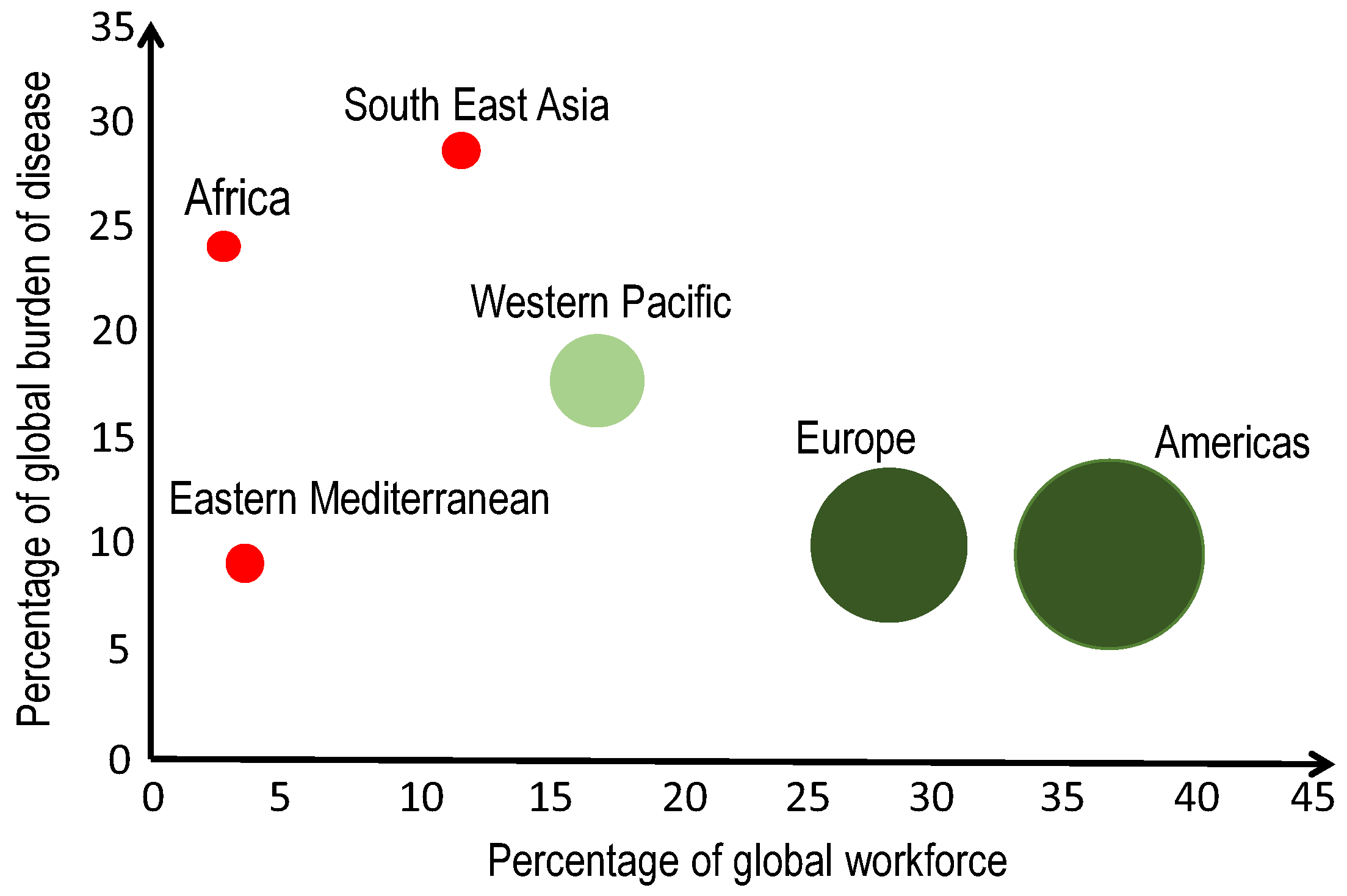
2.5. Resource Constraints
2.6. Problems with Healthcare Information Systems
2.7. Lack of a Data-Driven Culture
2.8. Healthcare Disparities
3. How Technologies Can Fix the Current Healthcare System
3.1. Various Health Advances with IoT
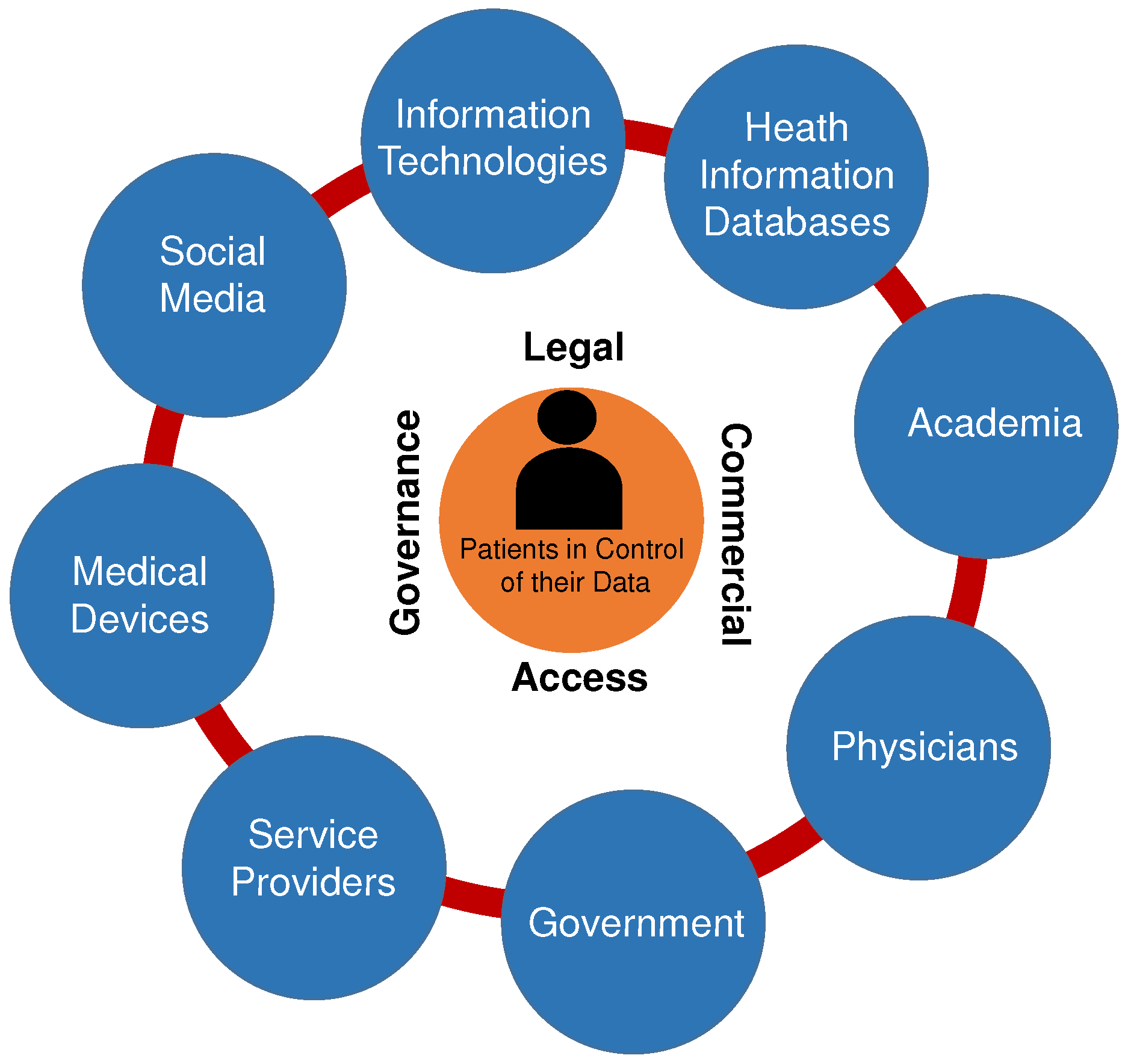
3.2. Big Data for Healthcare
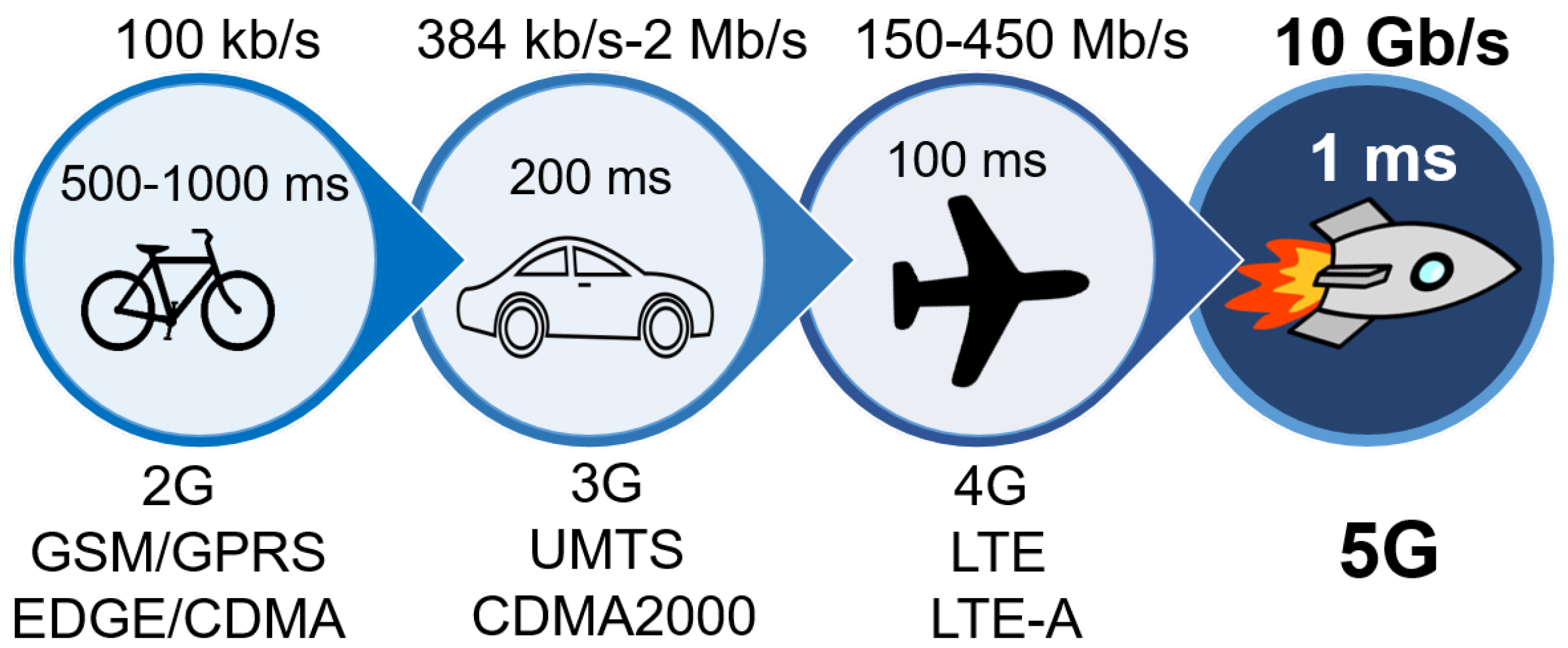
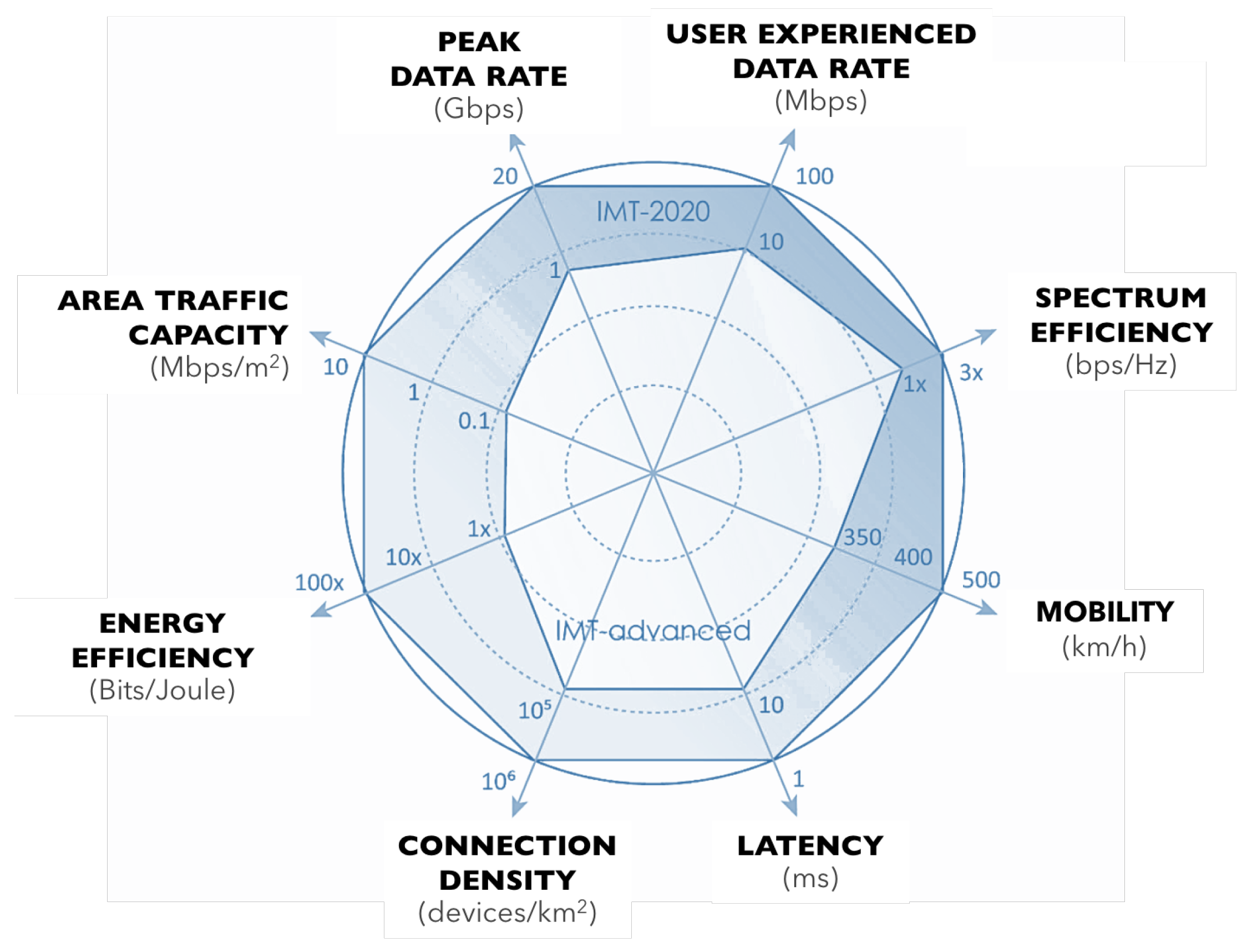
3.3. (Wireless) Connectivity
3.4. Artificial Intelligence and Machine Learning
3.5. Disruptive Health Innovations
3.5.1. Ingestible Sensors
3.5.2. Wearable Sensors to Wireless Charging Implants
3.5.3. Robot-Assisted Therapy and Surgery
3.5.4. Open Source EHR/EMR Systems
3.5.5. Point-Of-Care Testing
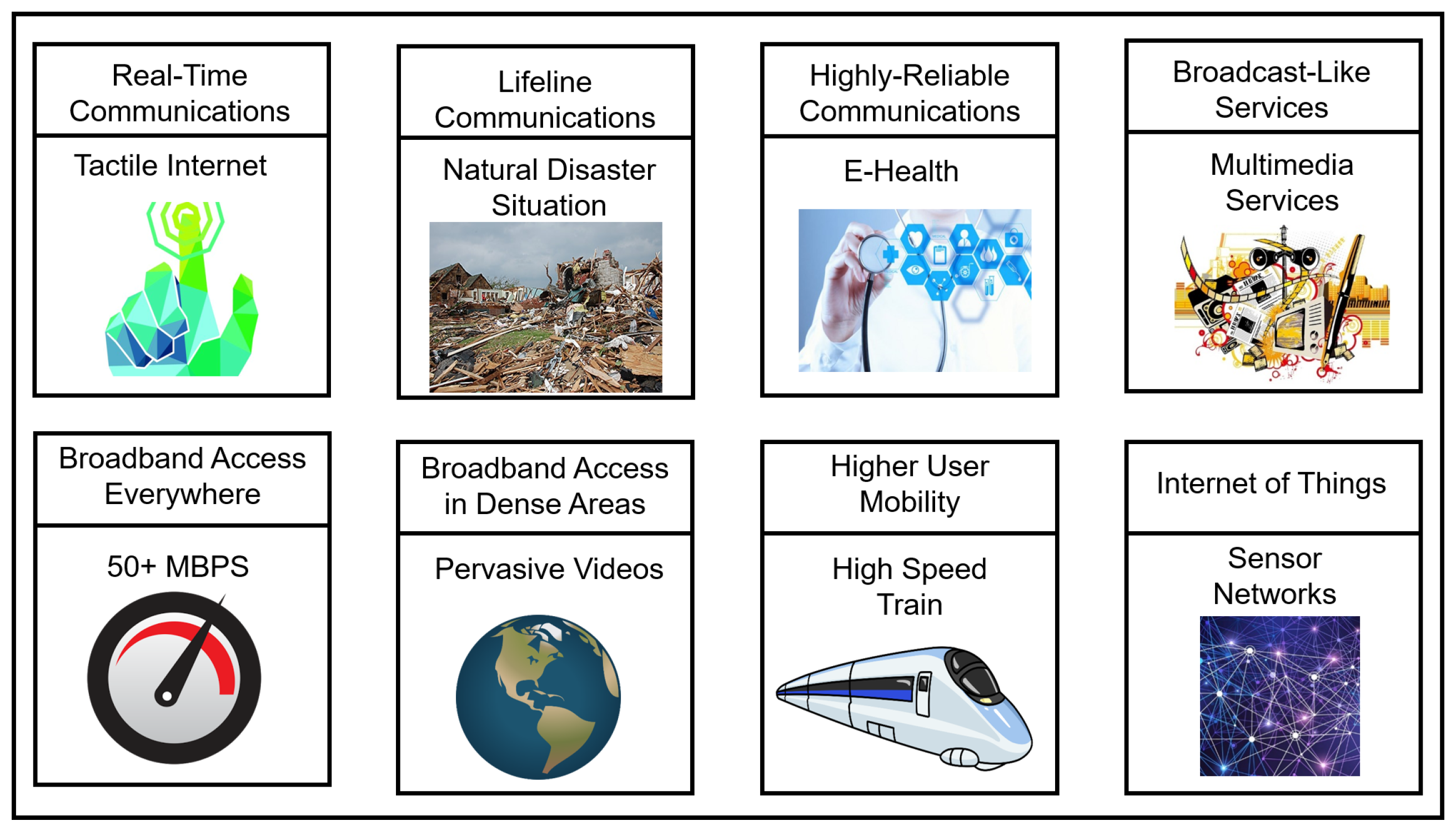
4. 5G and Healthcare Opportunities
4.1. Mobile Devices and Tablets can Help Leverage AI, Big Data and Connectivity
4.2. 5G and Universal Coverage
4.3. In-Home Health Monitoring
4.4. Virtual Reality + Haptic/Tactile Internet
4.5. Internet of Medical Skills
5. Case Study: Economic Benefits of 5G-Enabled Healthcare Solutions
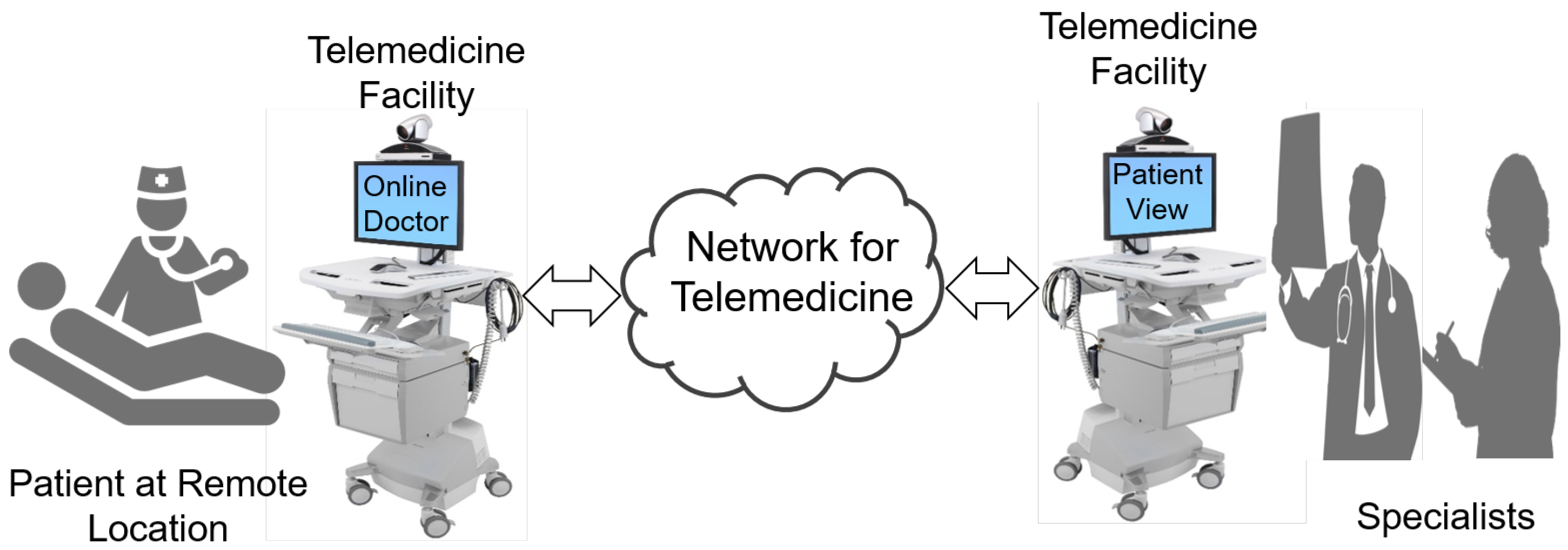
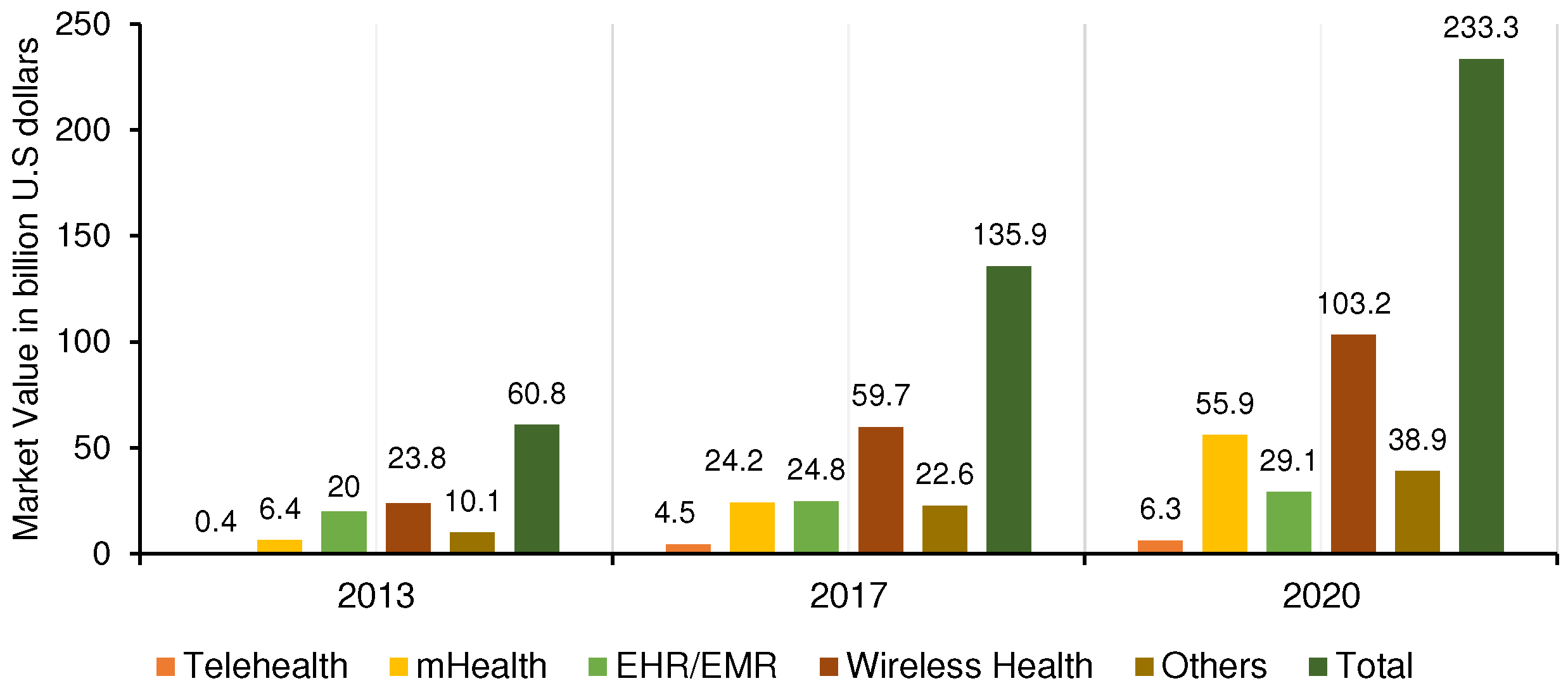
5.1. Cost Saving with Mobile Health and Telemedicine
5.2. Economic Benefits of IoT
- Better asset utilization results in a $2.5 trillion cost reduction
- Greater employees’ productivity causes a benefit of $2.5 trillion
- Improved supply chain management eliminates waste of $2.7 trillion
- Improved customer experience adding more customers equivalent to $3.7 trillion
- Reduced time to market of $3.0 trillion
5.3. Economic Benefits with Big Data Analytics
- Tracking high-cost patients, reducing adverse events, lowering readmissions and treatment optimization [69]
- Reduction of healthcare expenditure by predictive modelling [70]
- Better earlier detection of medical conditions [71]
- Reduce the development costs for pharmaceutical companies [72]
- Lower costs through better patient interventions [68]
- Big data analytics could reduce the time required for research study by predicting the patients that would most likely comply with the studies [71]
5.4. Economic Impacts of AI
6. Technology for Healthcare: Challenges/Pitfalls
6.1. Will Computers Replace Doctors?
6.2. Technological Revolution Needed or Behavioural Revolution?
6.3. Bias in Humans and Data: The Perennial Bugbear
6.4. Cost Barriers for 5G
6.5. How to Incentivize 5G Healthcare?
6.6. Security and Privacy for 5G-Enabled Healthcare
7. Conclusions
“In the next ten years, data sciences and software will do more for medicine than all of the biological sciences together.”—Vinod Khosla [28]
Author Contributions
Conflicts of Interest
References
- Economists’ Declaration on Universal Health Coverage. Available online: http://www.healthforall.org/economists-declaration/ (accessed on 7 December 2017).
- McGinnis, J.M.; Stuckhardt, L.; Saunders, R.; Smith, M. (Eds.) Best Care at Lower Cost: The Path to Continuously Learning Health Care in America; National Academies Press: Washington, DC, USA, 2013. [Google Scholar]
- Deloitte. Global Health Care Outlook: Making Progress against Persistent Challenges; Deloitte: New York, NY, USA, 2017; Available online: https://goo.gl/pMq4HS (accessed on 5 October 2017).
- Häyrinen, K.; Saranto, K.; Nykänen, P. Definition, structure, content, use and impacts of electronic health records: A review of the research literature. Int. J. Med. Inform. 2008, 77, 291–304. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, D. Universal access to health care for all: Exploring road map. Indian J. Community Med. 2012, 37, 69. [Google Scholar] [CrossRef] [PubMed]
- Savedoff, W.D. A Moving Target: Universal Access to Healthcare Services in Latin America and the Caribbean; Technical Report; Inter-American Development Bank: Washington, DC, USA, 2009. [Google Scholar]
- Latif, S.; Rana, R.; Qadir, J.; Imran, M.; Younis, S. Mobile Health in the Developing World: Review of Literature and Lessons from A Case Study. IEEE Access 2017, 5, 11540–11556. [Google Scholar] [CrossRef]
- World Health Organization. The Global Burden of Chronic; World Health Organization: Geneva, Switzerland; Available online: https://goo.gl/2vilov (accessed on 11 November 2017).
- Priester, R.; Kane, R.L.; Totten, A.M. How the current system fails people with chronic illnesses. In Proceedings of the Meeting the Challenge of Chronic Illness, Johns Hopkins University, Baltimore, MD, USA, 25 April 2005; pp. 1–19. [Google Scholar]
- World Health Organization. Global Health and Aging; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- He, W.; Goodkind, D.; Kowal, P. An Aging World: 2015; United States Census Bureau: Suitland, MD, USA, 2016.
- Naicker, S.; Plange-Rhule, J.; Tutt, R.C.; Eastwood, J.B. Shortage of healthcare workers in developing countries—Africa. Ethn. Dis. 2009, 19, 60. [Google Scholar]
- World Health Organization. Global Health Workforce Shortage to Reach 12.9 Million in Coming Decades; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Istepanian, R.S.; Woodward, B. M-Health: Fundamentals and Applications; John Wiley & Sons: Hoboken, NJ, USA, 2016. [Google Scholar]
- Brook, R.H. Possible outcomes of comparative effectiveness research. JAMA 2009, 302, 194–195. [Google Scholar] [CrossRef] [PubMed]
- Dickman, S.L.; Woolhandler, S.; Bor, J.; McCormick, D.; Bor, D.H.; Himmelstein, D.U. Health spending for low-, middle-, and high-income Americans, 1963–2012. Health Aff. 2016, 35, 1189–1196. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, B. Poverty and poor health: Can health care reform narrow the rich-poor gap? Focus 2011, 28, 12. [Google Scholar]
- Aloi, G.; Caliciuri, G.; Fortino, G.; Gravina, R.; Pace, P.; Russo, W.; Savaglio, C. A mobile multi-technology gateway to enable IoT interoperability. In Proceedings of the IEEE Conference on Internet-of-Things Design and Implementation, Berlin, Germany, 4–8 April 2016. [Google Scholar]
- Bahga, A.; Madisetti, V. Internet of Things: A hands-on Approach; VPT: Blacksburg, VA, USA, 2014. [Google Scholar]
- Islam, S.R.; Kwak, D.; Kabir, M.H.; Hossain, M.; Kwak, K.S. The internet of things for health care: A comprehensive survey. IEEE Access 2015, 3, 678–708. [Google Scholar] [CrossRef]
- Ali, A.; Qadir, J.; ur Rasool, R.; Sathiaseelan, A.; Zwitter, A.; Crowcroft, J. Big data for development: Applications and techniques. Big Data Anal. 2016, 1, 2. [Google Scholar] [CrossRef]
- Gulamhussen, A.; Hirt, R.; Ruckebier, M.; Orban de Xivry, J.; Marcerou, G.; Melis, J. Big data in healthcare: What options are there to put the patients in control of their data? In Proceedings of the EIT Foundation Annual Innovation Forum, Brussels, Belgium, 26 March 2013. [Google Scholar]
- Costa, F.F. Big data in biomedicine. Drug Discov. Today 2014, 19, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Lazakidou, A. Wireless Technologies for Ambient Assisted Living and Healthcare: Systems and Applications: Systems and Applications; IGI Global: Hershey, PA, USA, 2010. [Google Scholar]
- Khoumbati, K. Handbook of Research on Advances in Health Informatics and Electronic Healthcare Applications: Global Adoption and Impact of Information Communication Technologies: Global Adoption and Impact of Information Communication Technologies; IGI Global: Hershey, PA, USA, 2009. [Google Scholar]
- Ng, H.; Sim, M.; Tan, C.M.; Wong, C. Wireless technologies for telemedicine. BT Technol. J. 2006, 24, 130–137. [Google Scholar] [CrossRef]
- Mahmoodi, M.C.T.; Dohler, M.A.L.M. 5G IoT Industry Verticals and Network Requirements. In Powering the Internet of Things with 5G Networks; IGI Global: Hershey, PA, USA, 2017; Chapter 6; p. 148. [Google Scholar]
- Khosla, V. 20-Percent Doctor Included: Speculations & Musings of a Technology Optimist. Available online: https://goo.gl/DrDg6G (accessed on 7 December 2017).
- Sundar. Google CEO Sundar Pichai on How AI Can Help Improve Healthcare in Rural India. Available online: https://goo.gl/2ZgKuS (accessed on 5 October 2017).
- Artificial Intelligence Can Spot Skin Cancer. Available online: https://goo.gl/5znxBD (accessed on 7 December 2017).
- The Opportunities & Challenges of AI in Healthcare. Available online: https://goo.gl/DAi5yQ (accessed on 5 October 2017).
- Hafezi, H.; Robertson, T.L.; Moon, G.D.; Au-Yeung, K.Y.; Zdeblick, M.J.; Savage, G.M. An ingestible sensor for measuring medication adherence. IEEE Trans. Biomed. Eng. 2015, 62, 99–109. [Google Scholar] [CrossRef] [PubMed]
- Belknap, R.; Weis, S.; Brookens, A.; Au-Yeung, K.Y.; Moon, G.; DiCarlo, L.; Reves, R. Feasibility of an ingestible sensor-based system for monitoring adherence to tuberculosis therapy. PLoS ONE 2013, 8, e53373. [Google Scholar] [CrossRef] [PubMed]
- Andreu-Perez, J.; Leff, D.R.; Ip, H.M.; Yang, G.Z. From wearable sensors to smart implants—Toward pervasive and personalized healthcare. IEEE Trans. Biomed. Eng. 2015, 62, 2750–2762. [Google Scholar] [CrossRef] [PubMed]
- Memory Implants for Brain Long-Term Memories. Available online: https://goo.gl/aWgSvV (accessed on 7 December 2017).
- Taylor, R.H.; Menciassi, A.; Fichtinger, G.; Dario, P. Medical robotics and computer-integrated surgery. In Springer Handbook of Robotics; Springer: Berlin, Germany, 2008; pp. 1199–1222. [Google Scholar]
- Liu, H.; Lawrie, T.A.; Lu, D.; Song, H.; Wang, L.; Shi, G. Robot-Assisted Surgery in Gynaecology. Cochrane Libr. 2014. Available online: https://goo.gl/LZMD8E (accessed on 7 December 2017).
- Ding, J.; Lim, Y.J.; Solano, M.; Shadle, K.; Park, C.; Lin, C.; Hu, J. Giving patients a lift-the robotic nursing assistant (RoNA). In Proceedings of the IEEE International Conference on Technologies for Practical Robot Applications (TePRA), Woburn, MA, USA, 14–15 April 2014; pp. 1–5. [Google Scholar]
- Pugia, M.J.; Lott, J.A.; Clark, L.W.; Parker, D.R.; Wallace, J.F.; Willis, T.W. Comparison of urine dipsticks with quantitative methods for microalbuminuria. Eur. J. Clin. Chem. Clin. Biochem. 1997, 35, 693–700. [Google Scholar] [PubMed]
- Herbert, S.; Edwards, S.; Carrick, G.; Copas, A.; Sandford, C.; Amphlett, M.; Benn, P. Evaluation of PIMA point-of-care CD4 testing in a large UK HIV service. Sex. Transm. Infect. 2012, 88, 413–417. [Google Scholar] [CrossRef] [PubMed]
- St John, A.; Price, C.P. Existing and emerging technologies for point-of-care testing. Clin. Biochem. Rev. 2014, 35, 155–167. [Google Scholar] [PubMed]
- Alliance, N. 5G White Paper-Executive Version; White Paper; ngmn Ltd.: Berkshire, UK, 2014; Available online: https://goo.gl/iErufs (accessed on 7 December 2017).
- Aijaz, A.; Dohler, M.; Aghvami, A.H.; Friderikos, V.; Frodigh, M. Realizing the tactile internet: Haptic communications over next generation 5G cellular networks. IEEE Wirel. Commun. 2017, 24, 82–89. [Google Scholar] [CrossRef]
- Andrews, J.G.; Buzzi, S.; Choi, W.; Hanly, S.V.; Lozano, A.; Soong, A.C.; Zhang, J.C. What will 5G be? IEEE J. Sel. Areas Commun. 2014, 32, 1065–1082. [Google Scholar] [CrossRef]
- Latif, S.; Pervez, F.; Usama, M.; Qadir, J. Artificial Intelligence as an Enabler for Cognitive Self-Organizing Future Networks. arXiv. 2017. arXiv:1702.02823. Available online: https://arxiv.org/pdf/1702.02823.pdf (accessed on 7 December 2017).
- Sarda, B. Vision from Orange Healthcare on 5G. Available online: https://goo.gl/ozgqg8 (accessed on 7 December 2017).
- 5G Infrastructure Association. 5G PPP White Paper on EHealth Vertical Sector; 5G Infrastructure Association: Brussels, Belgium, 2015. [Google Scholar]
- West, D.M. How 5G technology enables the health internet of things. Brook. Cent. Technol. Innov. 2016, 3, 1–20. [Google Scholar]
- Charting the Course to 5G. Available online: https://goo.gl/jZ9Sjg (accessed on 7 December 2017).
- Global Mobile Suppliers Association. The Road to 5G: Drivers, Applications, Requirements and Technical Development; GSA: Farnham, UK, 2015; Volume 3, Available online: https://goo.gl/Umxhzi (accessed on 7 December 2017).
- Onireti, O.; Qadir, J.; Imran, M.A.; Sathiaseelan, A. Will 5G See its Blind Side? Evolving 5G for Universal Internet Access. In Proceedings of the 2016 Workshop on Global Access to the Internet for All, Florianopolis, Brazil, 22–26 August 2016; pp. 1–6. Available online: https://arxiv.org/pdf/1603.09537.pdf (accessed on 7 December 2017).
- Deloitte. Global Health Care Sector Outlook; Deloitte: New York, NY, USA, 2017. [Google Scholar]
- Economist Intelligence Unit. World Industry Outlook Healthcare and Pharmaceuticals; Economist Intelligence Unit: London, UK, 2014. [Google Scholar]
- Programme, G.C.L. Socio-Economic Impact of mHealth: An Assessment Report for the European Union; GSMA: London, UK, 2013; Available online: https://goo.gl/prRLVK (accessed on 7 December 2017).
- World Health Organization. The World Health Report 2006: Working Together for Health; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Boston Consulting Group. The Socio-Economic Impact of mHealth; Boston Consulting Group, Commissioned by Telenor Group: Boston, MA, USA, 2012; Available online: https://goo.gl/vdqP1h (accessed on 7 December 2017).
- Research and Markets. Global Telemedicine Market Size, Share, Development, Growth and Demand Forecast to 2022. Available online: https://www.researchandmarkets.com/research/w27w2j/global (accessed on 5 October 2017).
- Thuemmler, C.; Bai, C. Health 4.0: How Virtualization and Big Data are Revolutionizing Healthcare; Springer: Berlin, Germany, 2017. [Google Scholar]
- Deloitte. Connected Health How Digital Technology is Transforming Health and Social Care; Deloitte: New York, NY, USA, 2015. [Google Scholar]
- Well, A. Telehealth Index: 2016 Employer Banchmark Survey. 2016. Available online: https://goo.gl/KGbEoE (accessed on 5 October 2017).
- International Telecommunication Union (ITU), I.T.U. ICT Facts and Figures 2017. 2017. Available online: https://goo.gl/xGKzac (accessed on 7 December 2017).
- Bradley, J.; Barbier, J.; Handler, D. Embracing the Internet of Everything to Capture Your Share of $14.4 Trillion; White Paper; Cisco: San Jose, CA, USA, 2013. [Google Scholar]
- Just 3.3 Million Fitness Trackers were Sold in the US in the Past Year. Available online: https://goo.gl/3Jb4p1 (accessed on 30 September 2017).
- IoT Heading for Mass Adoption by 2019 Driven by Better-Than-Expected Business Results. Available online: https://goo.gl/22UZ8e (accessed on 30 September 2017).
- Castillo, A.; Thierer, A.D. Projecting the Growth and Economic Impact of the Internet of Things; George Mason University: Arlington, VA, USA, 2015. [Google Scholar] [CrossRef]
- Smart Healthcare—Technavio Publishes Top Market Drivers and Trends. Available online: https://goo.gl/ycJZZB (accessed on 30 September 2017).
- Commission, E. Enter the Data Economy: EU Policies for a Thriving Data Ecosystem. Available online: https://goo.gl/Tskzka (accessed on 30 September 2017).
- Schaeffer, C.; Haque, A.; Booton, L.; Halleck, J.; Coustasse, A. Big Data Management in United States Hospitals: Benefits and Barriers. 2016. Available online: https://goo.gl/U1ZADX (accessed on 7 December 2017).
- Bates, D.W.; Saria, S.; Ohno-Machado, L.; Shah, A.; Escobar, G. Big data in health care: Using analytics to identify and manage high-risk and high-cost patients. Health Aff. 2014, 33, 1123–1131. [Google Scholar] [CrossRef] [PubMed]
- Wills, M.J. Decisions through data: Analytics in healthcare. J. Healthc. Manag. 2015, 59, 254–262. [Google Scholar] [CrossRef]
- Jee, K.; Kim, G.H. Potentiality of big data in the medical sector: Focus on how to reshape the healthcare system. Healthc. Inform. Res. 2013, 19, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Chute, C.G.; Ullman-Cullere, M.; Wood, G.M.; Lin, S.M.; He, M.; Pathak, J. Some experiences and opportunities for big data in translational research. Genet. Med. 2013, 15, 802–809. [Google Scholar] [CrossRef] [PubMed]
- Raghupathi, W.; Raghupathi, V. Big data analytics in healthcare: Promise and potential. Health Inform. Sci. Syst. 2014, 2, 3. [Google Scholar] [CrossRef] [PubMed]
- IBM. Data-Driven Healthcare Organizations Use Big Data Analytics for Big Gains; White Paper; IBM: Armonk, NY, USA, 2013. [Google Scholar]
- Manyika, J.; Chui, M.; Brown, B.; Bughin, J.; Dobbs, R.; Roxburgh, C.; Byers, A.H. Big Data: The Next Frontier for Innovation, Competition, and Productivity. 2011. Available online: https://goo.gl/xomLS8 (accessed on 7 December 2017).
- Accenture. Artificial Intelligence: Healthcare’s New Nervous System. 2017. Available online: https://goo.gl/9tKKQ7 (accessed on 7 December 2017).
- Jennifer. See How Artificial Intelligence can Improve Medical Diagnosis and Healthcare. Available online: https://goo.gl/yr2jYu (accessed on 5 October 2017).
- Artificial Intelligence Future Growth. Available online: https://goo.gl/kNqGyB (accessed on 7 December 2017).
- Sullivan, F. Cognitive Computing and Artificial Intelligence Systems in Healthcare. 2015. Available online: https://goo.gl/w9gtox (accessed on 7 December 2017).
- Winters, B.; Custer, J.; Galvagno, S.M.; Colantuoni, E.; Kapoor, S.G.; Lee, H.; Goode, V.; Robinson, K.; Nakhasi, A.; Pronovost, P.; et al. Diagnostic errors in the intensive care unit: A systematic review of autopsy studies. BMJ Qual. Saf. 2012, 21, 894–902. [Google Scholar] [CrossRef] [PubMed]
- Dimitrov, D.V. Systems patientomics: The virtual in-silico patient. New Horiz. Transl. Med. 2014, 2, 1–4. [Google Scholar] [CrossRef]
- Singh, H.; Graber, M. Reducing diagnostic error through medical home-based primary care reform. JAMA 2010, 304, 463–464. [Google Scholar] [CrossRef] [PubMed]
- Khosla, V. Technology Will Replace 80% of What Doctors Do. 2012. Available online: https://goo.gl/2UVJcv (accessed on 5 October 2017).
- Adult Obesity Facts. Available online: https://goo.gl/TwVsUi (accessed on 7 December 2017).
- Ryan, P. Integrated theory of health behavior change: Background and intervention development. Clin. Nurse Spec. CNS 2009, 23, 161–172. [Google Scholar] [CrossRef] [PubMed]
- Ryan, R.M.; Patrick, H.; Deci, E.L.; Williams, G.C. Facilitating health behaviour change and its maintenance: Interventions based on self-determination theory. Eur. Health Psychol. 2008, 10, 2–5. [Google Scholar]
- Nutbeam, D.; Harris, E.; Wise, W. Theory in a Nutshell: A Practical Guide to Health Promotion Theories; McGraw-Hill: New York, NY, USA, 2010. [Google Scholar]
- Schneeweiss, S. Learning from big health care data. N. Engl. J. Med. 2014, 370, 2161–2163. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, S. The Laws of Medicine: Field Notes from an Uncertain Science; Simon and Schuster: New York, NY, USA, 2015. [Google Scholar]
- Agyapong, P.K.; Iwamura, M.; Staehle, D.; Kiess, W.; Benjebbour, A. Design considerations for a 5G network architecture. IEEE Commun. Mag. 2014, 11, 65–75. [Google Scholar] [CrossRef]
- Zhou, J.; Cao, Z.; Dong, X.; Vasilakos, A.V. Security and privacy for cloud-based IoT: Challenges. IEEE Commun. Mag. 2017, 55, 26–33. [Google Scholar] [CrossRef]

© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Latif, S.; Qadir, J.; Farooq, S.; Imran, M.A. How 5G Wireless (and Concomitant Technologies) Will Revolutionize Healthcare? Future Internet 2017, 9, 93. https://doi.org/10.3390/fi9040093
Latif S, Qadir J, Farooq S, Imran MA. How 5G Wireless (and Concomitant Technologies) Will Revolutionize Healthcare? Future Internet. 2017; 9(4):93. https://doi.org/10.3390/fi9040093
Chicago/Turabian StyleLatif, Siddique, Junaid Qadir, Shahzad Farooq, and Muhammad Ali Imran. 2017. "How 5G Wireless (and Concomitant Technologies) Will Revolutionize Healthcare?" Future Internet 9, no. 4: 93. https://doi.org/10.3390/fi9040093
APA StyleLatif, S., Qadir, J., Farooq, S., & Imran, M. A. (2017). How 5G Wireless (and Concomitant Technologies) Will Revolutionize Healthcare? Future Internet, 9(4), 93. https://doi.org/10.3390/fi9040093






