Pediatric Orally Disintegrating Tablets (ODTs) with Enhanced Palatability Based on Propranolol HCl Coground with Hydroxypropyl-β-Cyclodextrin
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation of Drug:HPβCD Binary Systems
2.3. Drug Assay by UV-Vis Spectrometry
2.4. Preparation of ODTs
2.5. Characterization of ODT Formulations
2.5.1. Disintegration Test According to 11th Ph. Eur.
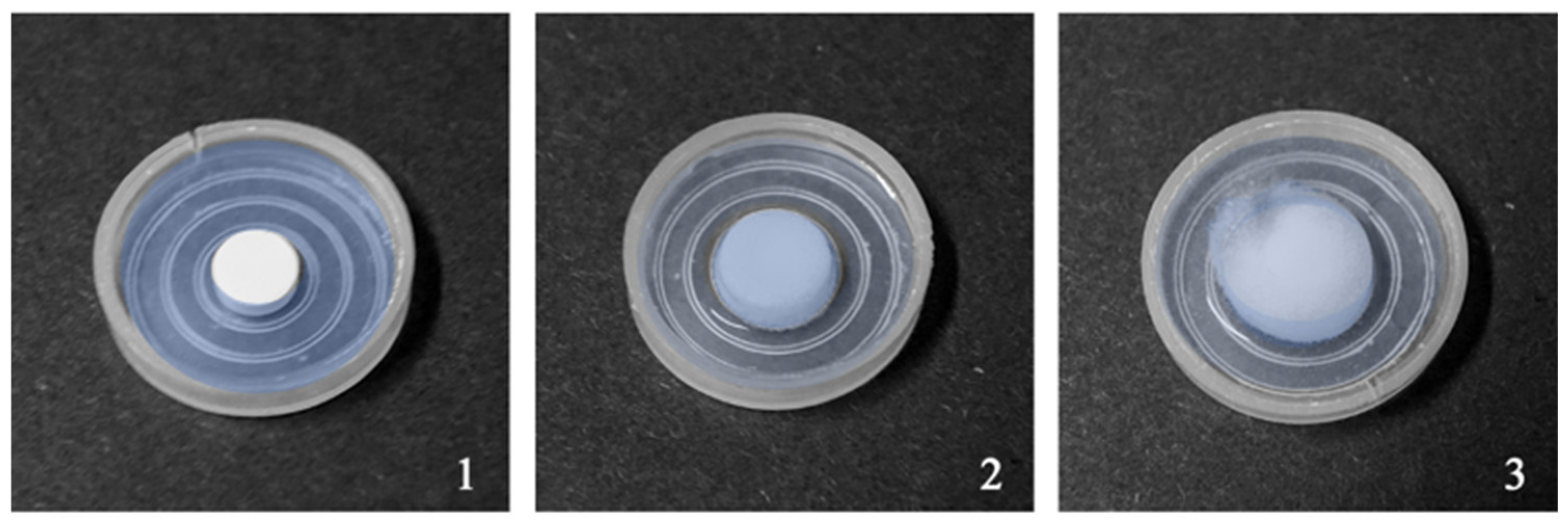
2.5.2. Simulated Wetting Test (SWT)
2.5.3. Disintegration Test on Wire Cloth
2.6. Dissolution Test
2.7. Scanning Electron Microscopy (SEM)
2.8. Electronic Tongue Test (E-Tongue)
3. Results and Discussion
Palatability Studies by E-Tongue
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- EMA, European Medicines Agency, Committee for Medicinal Products for Human Use (CHMP), Paediatric Committee (PDCO), Guideline on Pharmaceutical Development of Medicines for Pediatric Use Reference Number: EMA/CHMP/QWP/805880/2012 Rev. 2. Available online: https://www.ema.europa.eu/en/pharmaceutical-development-medicines-paediatric-use-scientific-guideline (accessed on 7 April 2024).
- Schrier, L.; Hadjipanayis, A.; Stiris, T.; Ross-Russell, R.I.; Valiulis, A.; Turner, M.A.; Zhao, W.; De Cock, P.; De Wildt, S.N.; Allegaert, K.; et al. Off-Label Use of Medicines in Neonates, Infants, Children, and Adolescents: A Joint Policy Statement by the European Academy of Paediatrics and the European Society for Developmental Perinatal and Pediatric Pharmacology. Eur. J. Pediatr. 2020, 179, 839–847. [Google Scholar] [CrossRef]
- Zahn, J.; Hoerning, A.; Trollmann, R.; Rascher, W.; Neubert, A. Manipulation of Medicinal Products for Oral Administration to Paediatric Patients at a German University Hospital: An Observational Study. Pharmaceutics 2020, 12, 583. [Google Scholar] [CrossRef]
- Wiedey, R.; Kokott, M.; Breitkreutz, J. Orodispersible Tablets for Pediatric Drug Delivery: Current Challenges and Recent Advances. Expert Opin. Drug Deliv. 2021, 18, 1873–1890. [Google Scholar] [CrossRef]
- Golhen, K.; Buettcher, M.; Kost, J.; Huwyler, J.; Pfister, M. Meeting Challenges of Pediatric Drug Delivery: The Potential of Orally Fast Disintegrating Tablets for Infants and Children. Pharmaceutics 2023, 15, 1033. [Google Scholar] [CrossRef]
- Kean, E.A.; Adeleke, O.A. Orally Disintegrating Drug Carriers for Paediatric Pharmacotherapy. Eur. J. Pharm. Sci. 2023, 182, 106377. [Google Scholar] [CrossRef]
- Boateng, J. Drug Delivery Innovations to Address Global Health Challenges for Pediatric and Geriatric Populations (Through Improvements in Patient Compliance). J. Pharm. Sci. 2017, 106, 3188–3198. [Google Scholar] [CrossRef]
- Ghourichay, M.P.; Kiaie, S.H.; Nokhodchi, A.; Javadzadeh, Y. Formulation and Quality Control of Orally Disintegrating Tablets (ODTs): Recent Advances and Perspectives. Biomed. Res. Int. 2021, 2021, 6618934. [Google Scholar] [CrossRef]
- Comoglu, T.; Dilek Ozyilmaz, E. Orally disintegrating tablets and orally disintegrating mini tablets—novel dosage forms for pediatric use. Pharm. Dev. Technol. 2019, 24, 902–914. [Google Scholar] [CrossRef]
- Nayak, A.K.; Manna, K. Current Developments in Orally Disintegrating Tablet Technology. J. Pharma. Educ. Res. 2011, 2, 21–34. [Google Scholar]
- Chinwala, M. Recent Formulation Advances and Therapeutic Usefulness of Orally Disintegrating Tablets (ODTs). Pharmacy 2020, 8, 186. [Google Scholar] [CrossRef]
- Wagner-Hattler, L.; Kiene, K.; Bielicki, J.; Pfister, M.; Puchkov, M.; Huwyler, J. High Acceptability of an Orally Dispersible Tablet Formulation by Children. Children 2021, 8, 194. [Google Scholar] [CrossRef]
- Vikas, Y.; Sandeep, K.; Braham, D.; Manjusha, C.; Budwhar, V. Cyclodextrin Complexes: An Approach to Improve the Physicochemical Properties of Drugs and Applications of Cyclodextrin Complexes. Asian J. Pharm. 2018, 2 (Suppl. S12), S394. [Google Scholar]
- Jansook, P.; Ogawa, N.; Loftsson, T. Cyclodextrins: Structure, Physicochemical Properties and Pharmaceutical Applications. Int. J. Pharm. 2018, 535, 272–284. [Google Scholar] [CrossRef]
- Adamkiewicz, L.; Szeleszczuk, Ł. Review of Applications of Cyclodextrins as Taste-Masking Excipients for Pharmaceutical Purposes. Molecules 2023, 28, 6964. [Google Scholar] [CrossRef]
- Katewongsa, P.; Lertsuphotvanit, N.; Phaechamud, T. Cetirizine Dihydrochloride, Beta-Cyclodextrin Inclusion Complex by Ethanol Kneading for Taste Masking. Indian. J. Pharm. Sci. 2017, 79, 758–767. [Google Scholar] [CrossRef]
- Alopaeus, J.F.; Göbel, A.; Breitkreutz, J.; Sande, S.A.; Tho, I. Investigation of Hydroxypropyl-β-Cyclodextrin Inclusion Complexation of Two Poorly Soluble Model Drugs and Their Taste-Sensation—Effect of Electrolytes, Freeze-Drying and Incorporation into Oral Film Formulations. J. Drug Deliv. Sci. Technol. 2021, 61, 102245. [Google Scholar] [CrossRef]
- Commey, K.L.; Nakatake, A.; Enaka, A.; Nakamura, R.; Nishi, K.; Tsukigawa, K.; Ikeda, H.; Yamaguchi, K.; Iohara, D.; Hirayama, F.; et al. Study of the Structural Chemistry of the Inclusion Complexation of 4-Phenylbutyrate and Related Compounds with Cyclodextrins in Solution: Differences in Inclusion Mode with Cavity Size Dependency. Int. J. Mol. Sci. 2023, 24, 15091. [Google Scholar] [CrossRef]
- Commey, K.L.; Enaka, A.; Nakamura, R.; Yamamoto, A.; Tsukigawa, K.; Nishi, K.; Iohara, D.; Hirayama, F.; Otagiri, M.; Yamasaki, K. Development of α-Cyclodextrin-Based Orally Disintegrating Tablets for 4-Phenylbutyrate. Pharmaceutics 2024, 16, 82. [Google Scholar] [CrossRef]
- EMA/CHMP/333892/2013 Committee for Human Medicinal Products (CHMP). Available online: www.ema.europa.eu/en/documents/scientific-guideline/questions-and-answers-cyclodextrins-used-excipients-medicinal-products-human-use_en.pdf (accessed on 5 May 2024).
- Jug, M.; Mura, P.A. Grinding as Solvent-Free Green Chemistry Approach for Cyclodextrin Inclusion Complex Preparation in the Solid State. Pharmaceutics 2018, 10, 189. [Google Scholar] [CrossRef]
- Barton, A.L.; Moffett, B.S.; Valdes, S.O.; Miyake, C.; Kim, J.J. Efficacy and Safety of High-Dose Propranolol for the Management of Infant Supraventricular Tachyarrhythmias. J. Pediatr. 2015, 166, 115–118. [Google Scholar] [CrossRef]
- Pacifici, G.M. Clinical Pharmacology of Propranolol in Infants and Children. J. Clin. Lab. Res. 2021, 3, 1–9. [Google Scholar] [CrossRef]
- Cirri, M.; Mura, P.; Benedetti, S.; Buratti, S. Development of a Hydroxypropyl-β-Cyclodextrin-Based Liquid Formulation for the Oral Administration of Propranolol in Pediatric Therapy. Pharmaceutics 2023, 15, 2217. [Google Scholar] [CrossRef]
- Salunke, S.; Brandys, B.; Giacoia, G.; Tuleu, C. The STEP (Safety and Toxicity of Excipients for Paediatrics) Database: Part 2—The Pilot Version. Int. J. Pharm. 2013, 457, 310–322. [Google Scholar] [CrossRef]
- Batchelor, H.K.; Fotaki, N.; Klein, S. Paediatric Oral Biopharmaceutics: Key Considerations and Current Challenges. Adv. Drug Deliv. Rev. 2014, 73, 102–126. [Google Scholar] [CrossRef]
- Rouaz, K.; Chiclana-Rodríguez, B.; Nardi-Ricart, A.; Suñé-Pou, M.; Mercadé-Frutos, D.; Suñé-Negre, J.M.; Pérez-Lozano, P.; García-Montoya, E. Excipients in the Paediatric Population: A Review. Pharmaceutics 2021, 13, 387. [Google Scholar] [CrossRef]
- Strickley, R.G. Pediatric Oral Formulations: An Updated Review of Commercially Available Pediatric Oral Formulations Since 2007. J. Pharm. Sci. 2019, 108, 1335–1365. [Google Scholar] [CrossRef]
- Park, J.H.; Holman, K.M.; Bish, G.M.; Grieger, D.G.; Ramlose, D.S.; Herman, C.J.; Hu, S.H. An Alternative to the USP Disintegration Test for Orally Disintegrating Tablets. Pharm. Technol. 2008, 32. [Google Scholar]
- Shukla, D. Mouth Dissolving Tablets II: An Overview of Evaluation Techniques. Sci. Pharm. 2009, 77, 327–341. [Google Scholar] [CrossRef]
- Motohiro, O.; Hayakawa, E.; Ito, K.; Tokuno, M.; Morimoto, K.; Watanabe, K. Intrabuccally Rapidly Disintegrating Tablet. Patent US20010014340A1, 16 August 2001. [Google Scholar]
- Cho, S.; Moazzem, M.S. Recent Applications of Potentiometric Electronic Tongue and Electronic Nose in Sensory Evaluation. Prev. Nutr. Food Sci. 2022, 27, 354–364. [Google Scholar] [CrossRef]
- Wasilewski, T.; Migoń, D.; Gębicki, J.; Kamysz, W. Critical Review of Electronic Nose and Tongue Instruments Prospects in Pharmaceutical Analysis. Anal. Chim. Acta. 2019, 1077, 14–29. [Google Scholar] [CrossRef]
- Late, S.; Yu, Y.; Banga, A. Effects of Disintegration-Promoting Agent, Lubricants and Moisture Treatment on Optimized Fast Disintegrating Tablets. Int. J. Pharm. 2009, 365, 4–11. [Google Scholar] [CrossRef]
- ICH Harmonization for Better Health—EMA/CPMP/ICH/82072/2006. ICHQ2 (R2) Guideline on Validation of Analytical Procedures. 24 March 2022. Available online: https://www.ema.europa.eu/en/ich-q2r2-validation-analytical-procedures-scientific-guideline (accessed on 17 May 2024).
- European Pharmacopoeia, Council of Europe; 11th ed.; Strasbourg, 2022. Available online: https://www.edqm.eu/en/european-pharmacopoeia-ph.-eur.-11th-edition (accessed on 17 May 2024).
- Brniak, W.; Jachowicz, R.; Pelka, P. The Practical Approach to the Evaluation of Methods Used to Determine the Disintegration Time of Orally Disintegrating Tablets (ODTs). Saudi Pharm. J. 2015, 23, 437–443. [Google Scholar] [CrossRef]
- Cilurzo, F.; Cupone, I.E.; Minghetti, P.; Buratti, S.; Gennari, C.G.M.; Montanari, L. Diclofenac Fast-Dissolving Film: Suppression of Bitterness by a Taste-Sensing System. Drug Dev. Ind. Pharm. 2011, 37, 252–259. [Google Scholar] [CrossRef]
- Kobayashi, Y.; Habara, M.; Ikezazki, H.; Chen, R.; Naito, Y.; Toko, K. Advanced Taste Sensors Based on Artificial Lipids with Global Selectivity to Basic Taste Qualities and High Correlation to Sensory Scores. Sensors 2010, 10, 3411–3443. [Google Scholar] [CrossRef]
- Abdi, H.; Williams, L.J. Principal Component Analysis. WIREs Comput. Stat. 2010, 2, 433–459. [Google Scholar] [CrossRef]
- Mishra, S.; Sarkar, U.; Taraphder, S.; Datta, S.; Swain, D.; Saikhom, R.; Panda, S.; Laishram, M. Principal Component Analysis. Int. J. Livest. Res. 2017, 7, 60–78. [Google Scholar] [CrossRef]
- Challener, C.A. Development of Coprocessed Excipients. Pharm. Technol. 2022, 46, 24–26. [Google Scholar]
- Food and Drug Administration, Center for Drug Evaluation and Research, Dec. 2008, Guidance For Industry Orally Disin-Tegrating Tablets. Available online: www.fda.gov/media/70877/download (accessed on 18 May 2024).
- Sutthapitaksakul, L.; Thanawuth, K.; Huanbutta, K.; Sriamornsak, P. Effect of a Superdisintegrant on Disintegration of Orally Disintegrating Tablets Determined by Simulated Wetting Test and in Vitro Disintegration Test. Pharmazie 2022, 77, 287–290. [Google Scholar] [CrossRef]
- Desai, S.; Poddar, A.; Sawant, K. Formulation of Cyclodextrin Inclusion Complex-Based Orally Disintegrating Tablet of Eslicarbazepine Acetate for Improved Oral Bioavailability. Mater. Sci. Eng. C 2016, 58, 826–834. [Google Scholar] [CrossRef]
- Al-Gethmy, H.A.; Fahmy, U.A.; Alhakamy, N.A.; Ahmed, O.A.A.; El-Say, K.M. Optimization of the Factors Affecting the Absorption of Vardenafil from Oral Disintegrating Tablets: A Clinical Pharmacokinetic Investigation. Pharmaceutics 2019, 11, 11. [Google Scholar] [CrossRef]
- Liu, T.; Wan, X.; Luo, Z.; Liu, C.; Quan, P.; Cun, D.; Fang, L. A Donepezil/Cyclodextrin Complexation Orodispersible Film: Effect of Cyclodextrin on Taste-Masking Based on Dynamic Process and in Vivo Drug Absorption. Asian J. Pharm. Sci. 2019, 14, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Musuc, A.M.; Anuta, V.; Atkinson, I.; Popa, V.T.; Sarbu, I.; Mircioiu, C.; Abdalrb, G.A.; Mitu, M.A.; Ozon, E.A. Development and Characterization of Orally Disintegrating Tablets Containing a Captopril-Cyclodextrin Complex. Pharmaceutics 2020, 12, 744. [Google Scholar] [CrossRef] [PubMed]
- PEARLITOL® Flash Co-Processed Mannitol Starch. Available online: https://www.roquette.com/innovation-hub/pharma/product-profile-pages/pearlitol-flash-co-processed-mannitol-starch (accessed on 20 May 2024).
- Rosenplenter, K.; Nöhle, U. Polyole. In Handbuch Süßungsmittel. Eigenschaften und Anwendung; Behr’s Verlag: Hamburg, Germany, 2007; Volume 7, p. S398. [Google Scholar]




| Code | Compression Time (s) | Pearlitol® Flash (% w/w) | Ludiflash® (% w/w) | Pharmaburst® 500 (% w/w) | Na Stearyl Fumarate (% w/w) | Hardness (Kg) | SWT Time (s) | Disint. Time (min) |
|---|---|---|---|---|---|---|---|---|
| I | 10 | 95 | - | - | 5 | 9 ± 1 | 31 ± 3 | <3 |
| II | 10 | - | 95 | - | 5 | 9.5 ± 0.5 | 42 ± 2 | <3 |
| III | 10 | - | - | 95 | 5 | 10 ± 1 | 45 ± 4 | <3 |
| IV | 5 | 95 | - | - | 5 | 8.5 ± 0.5 | 16 ± 2 | <3 |
| V | 5 | - | 95 | - | 5 | 9 ± 0.5 | 25 ± 2 | <3 |
| VI | 5 | - | - | 95 | 5 | 9 ± 0 | 28 ± 3 | <3 |
| Code | Explotab® (%) | Pure Drug (x) or GR | Compression Time (s) | Hardness (Kg) | SWT Time (s) | Wire Cloth Time (min) | Disintegration Time (min) |
|---|---|---|---|---|---|---|---|
| 1-A | - | x | 5 | 9 ± 0.5 | 18 ± 1 | <3 | <3 |
| 2-A | - | x | 3 | 8 ± 0.5 | 17 ± 2 | <3 | <3 |
| 3-A | - | x | 1 | 7 ± 0 | 14 ± 2 | <3 | <3 |
| 1-B | - | GR | 5 | 13 ± 1 | >30 | >3 | >3 |
| 2-B | - | GR | 3 | 13 ± 1 | >30 | >3 | >3 |
| 3-B | - | GR | 1 | 13 ± 1 | >30 | >3 | >3 |
| 4-A | 8 | x | 5 | 9 ± 0.5 | 21 ± 0 | <3 | <3 |
| 5-A | 8 | x | 3 | 8 ± 0.5 | 18 ± 1 | <3 | <3 |
| 6-A | 8 | x | 1 | 7 ± 0.5 | 16 ± 1 | <3 | <3 |
| 4-B | 8 | GR | 5 | 14 ± 0.5 | >30 | >3 | >3 |
| 5-B | 8 | GR | 3 | 14 ± 0.5 | >30 | >3 | >3 |
| 6-B | 8 | GR | 1 | 13 ± 0.5 | >30 | >3 | >3 |
| 7-A | 16 | x | 5 | 8 ± 0.5 | 28 ± 2 | <3 | <3 |
| 8-A | 16 | x | 3 | 7 ± 1 | 22 ± 0 | <3 | <3 |
| 9-A | 16 | x | 1 | 6 ± 0 | 18 ± 2 | <3 | <3 |
| 7-B | 16 | GR | 5 | 14 ± 0 | >30 | >3 | >3 |
| 8-B | 16 | GR | 3 | 14 ± 1 | >30 | >3 | >3 |
| 9-B | 16 | GR | 1 | 14 ± 0.5 | >30 | >3 | >3 |
| Code | Explotab®(%) | Compression Time (s) | Hardness (Kg) | SWT Time (s) | Disintegration Time (min) | Weight (mg ± s.d.) | Friability % |
|---|---|---|---|---|---|---|---|
| 6′ B′ | 8 | 1 | 7 | >30 | <3 | 301.5 ± 0.9 | 0.7 |
| 9′ B′ | 16 | 1 | 6 | >30 | <3 | 300.8 ± 1.2 | 0.85 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cirri, M.; Mura, P.A.; Maestrelli, F.; Benedetti, S.; Buratti, S. Pediatric Orally Disintegrating Tablets (ODTs) with Enhanced Palatability Based on Propranolol HCl Coground with Hydroxypropyl-β-Cyclodextrin. Pharmaceutics 2024, 16, 1351. https://doi.org/10.3390/pharmaceutics16111351
Cirri M, Mura PA, Maestrelli F, Benedetti S, Buratti S. Pediatric Orally Disintegrating Tablets (ODTs) with Enhanced Palatability Based on Propranolol HCl Coground with Hydroxypropyl-β-Cyclodextrin. Pharmaceutics. 2024; 16(11):1351. https://doi.org/10.3390/pharmaceutics16111351
Chicago/Turabian StyleCirri, Marzia, Paola A. Mura, Francesca Maestrelli, Simona Benedetti, and Susanna Buratti. 2024. "Pediatric Orally Disintegrating Tablets (ODTs) with Enhanced Palatability Based on Propranolol HCl Coground with Hydroxypropyl-β-Cyclodextrin" Pharmaceutics 16, no. 11: 1351. https://doi.org/10.3390/pharmaceutics16111351
APA StyleCirri, M., Mura, P. A., Maestrelli, F., Benedetti, S., & Buratti, S. (2024). Pediatric Orally Disintegrating Tablets (ODTs) with Enhanced Palatability Based on Propranolol HCl Coground with Hydroxypropyl-β-Cyclodextrin. Pharmaceutics, 16(11), 1351. https://doi.org/10.3390/pharmaceutics16111351









