Towards More Precise Targeting of Inhaled Aerosols to Different Areas of the Respiratory System
Abstract
1. Introduction
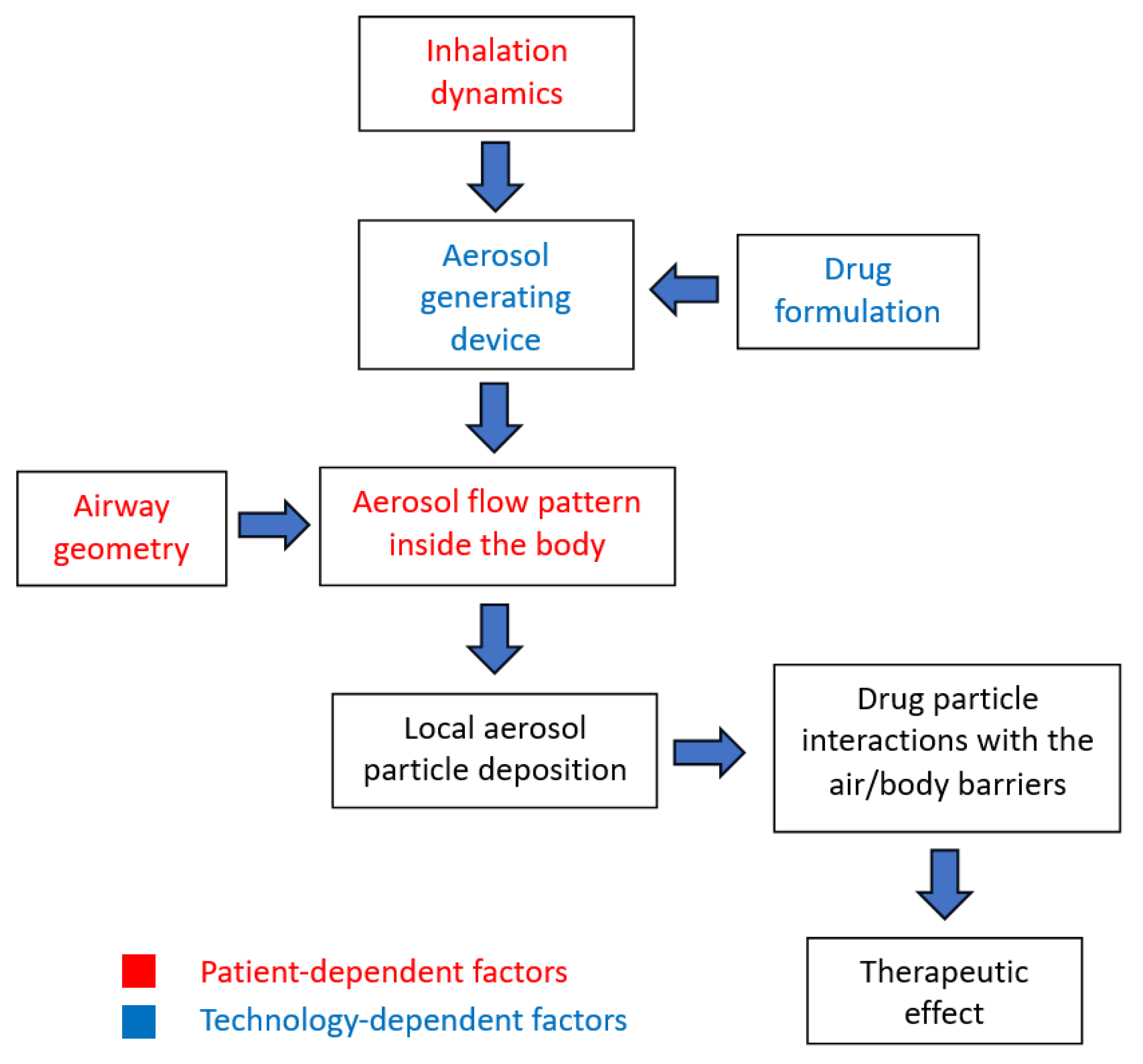
2. Major Factors Influencing the Efficiency of Drug Delivery Using Aerosols
2.1. Basic Concepts of Inhalation Therapy
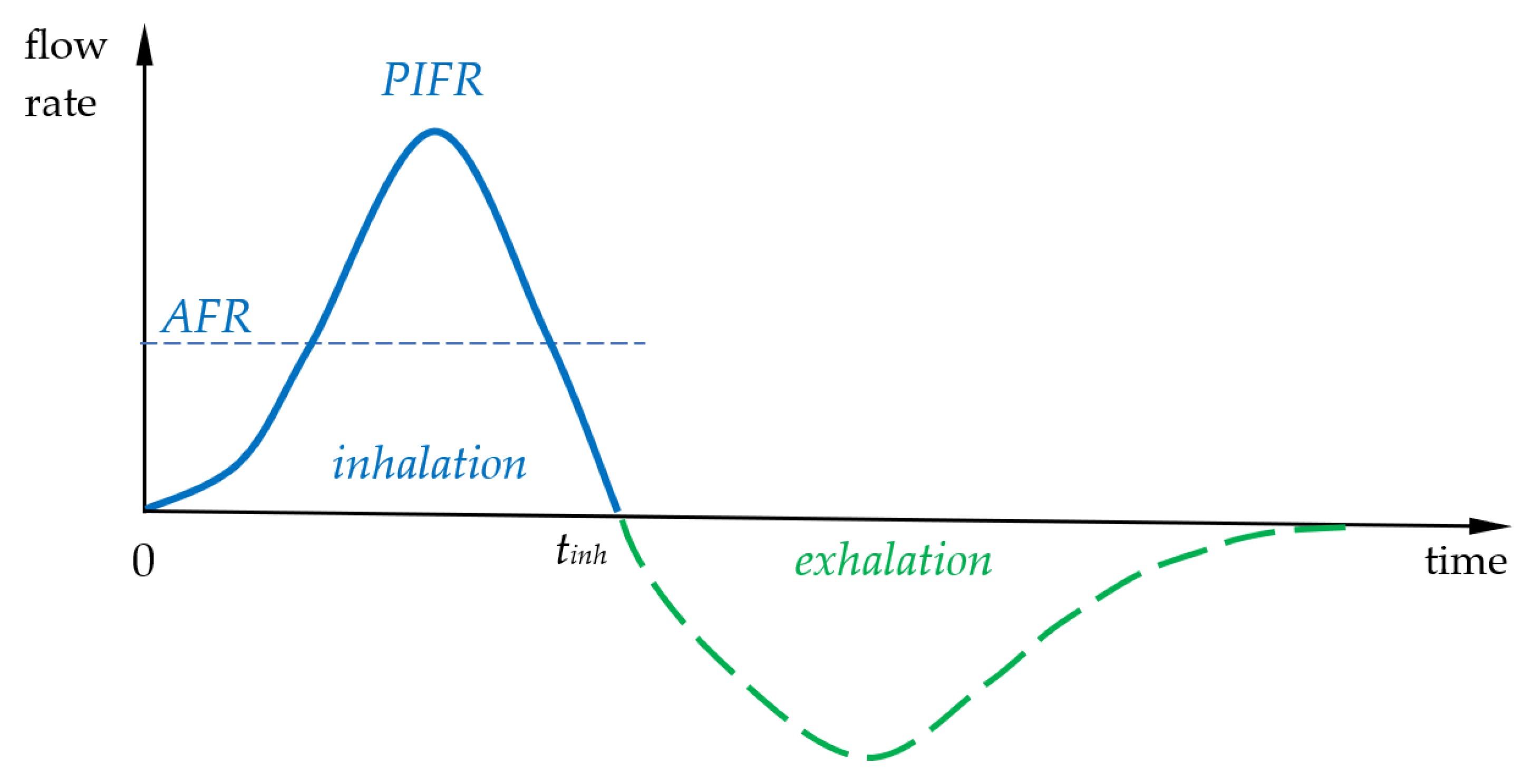
2.2. Inhalation Dynamics and Particle Deposition Mechanisms
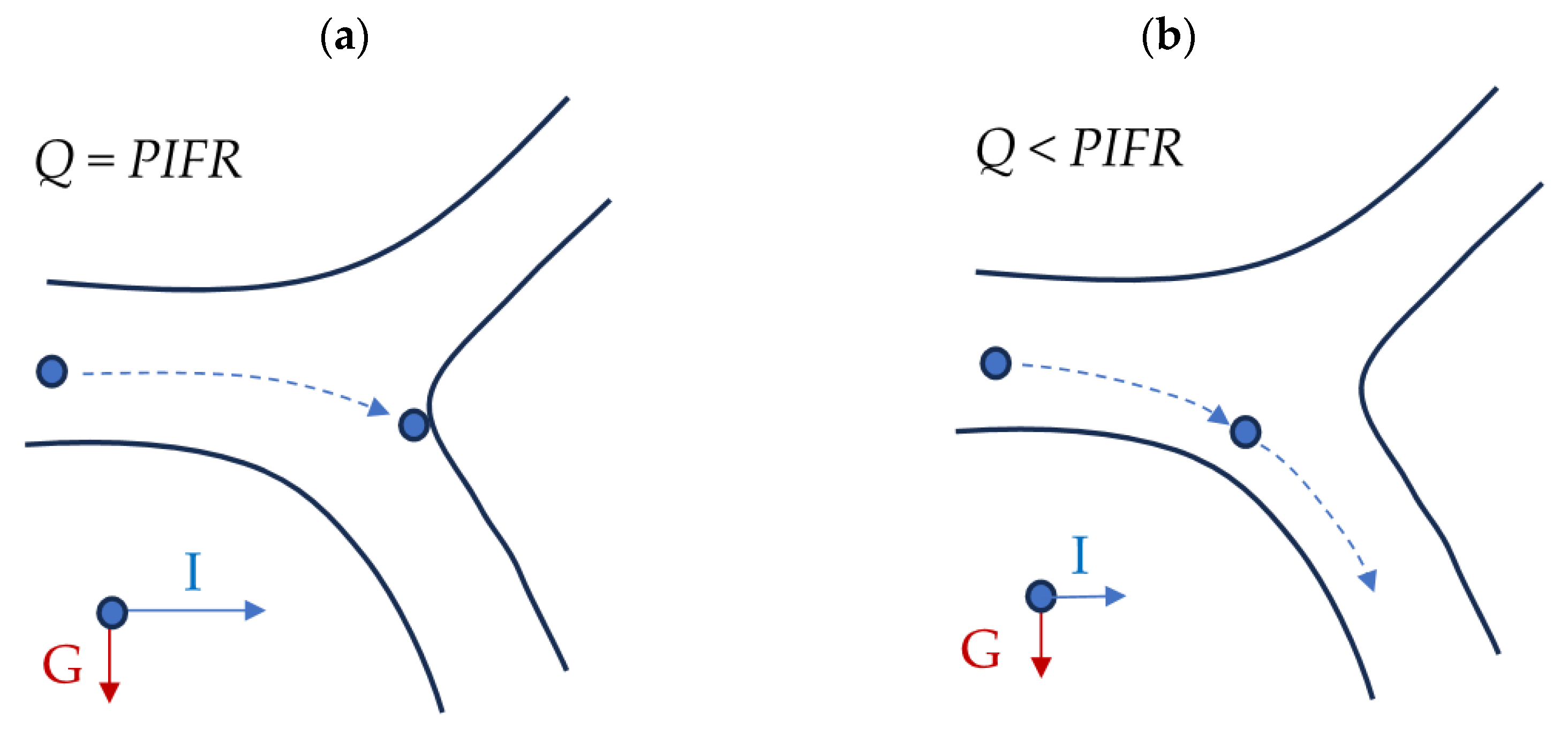
2.3. The Influence of Airway Geometry
3. The Role of the Aerosol-Generating Device and the Form of the Precursor
3.1. Drug Targeting to the Lower Respiratory System
3.2. Drug Targeting to the Nasal Cavity
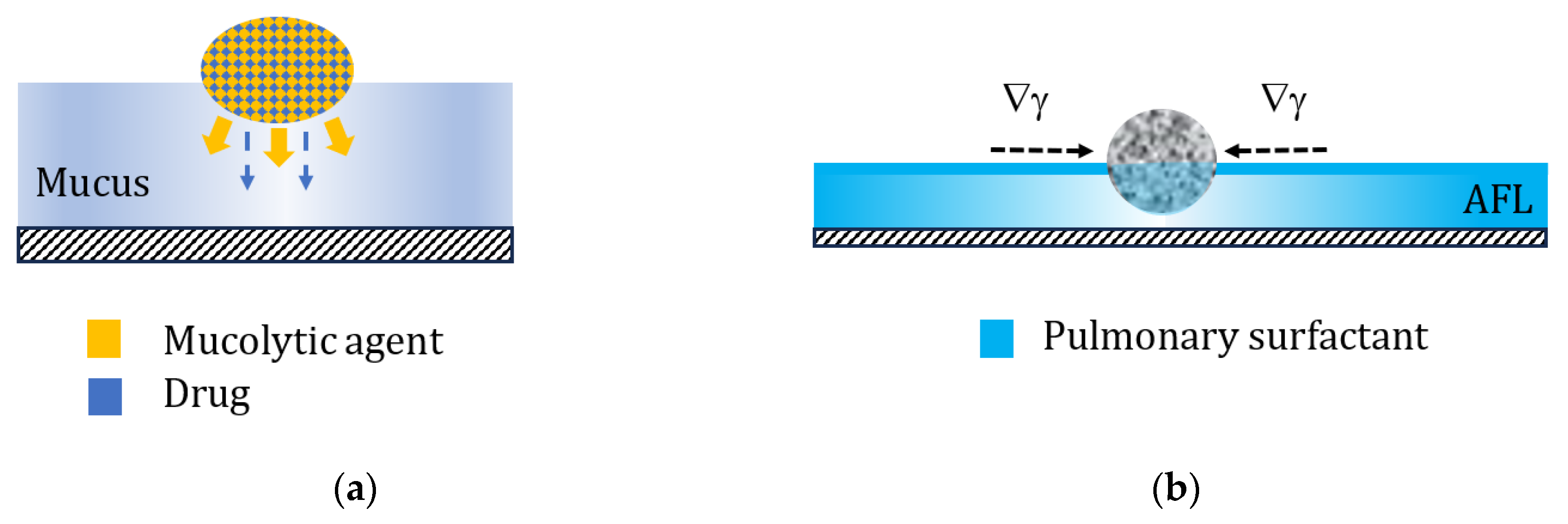
4. Particle–Lung Interaction and the Mass Transfer after Drug Deposition
5. Selected Concepts and Methods of Improvement of Targeted Aerosol Delivery to Different Regions in the Respiratory System
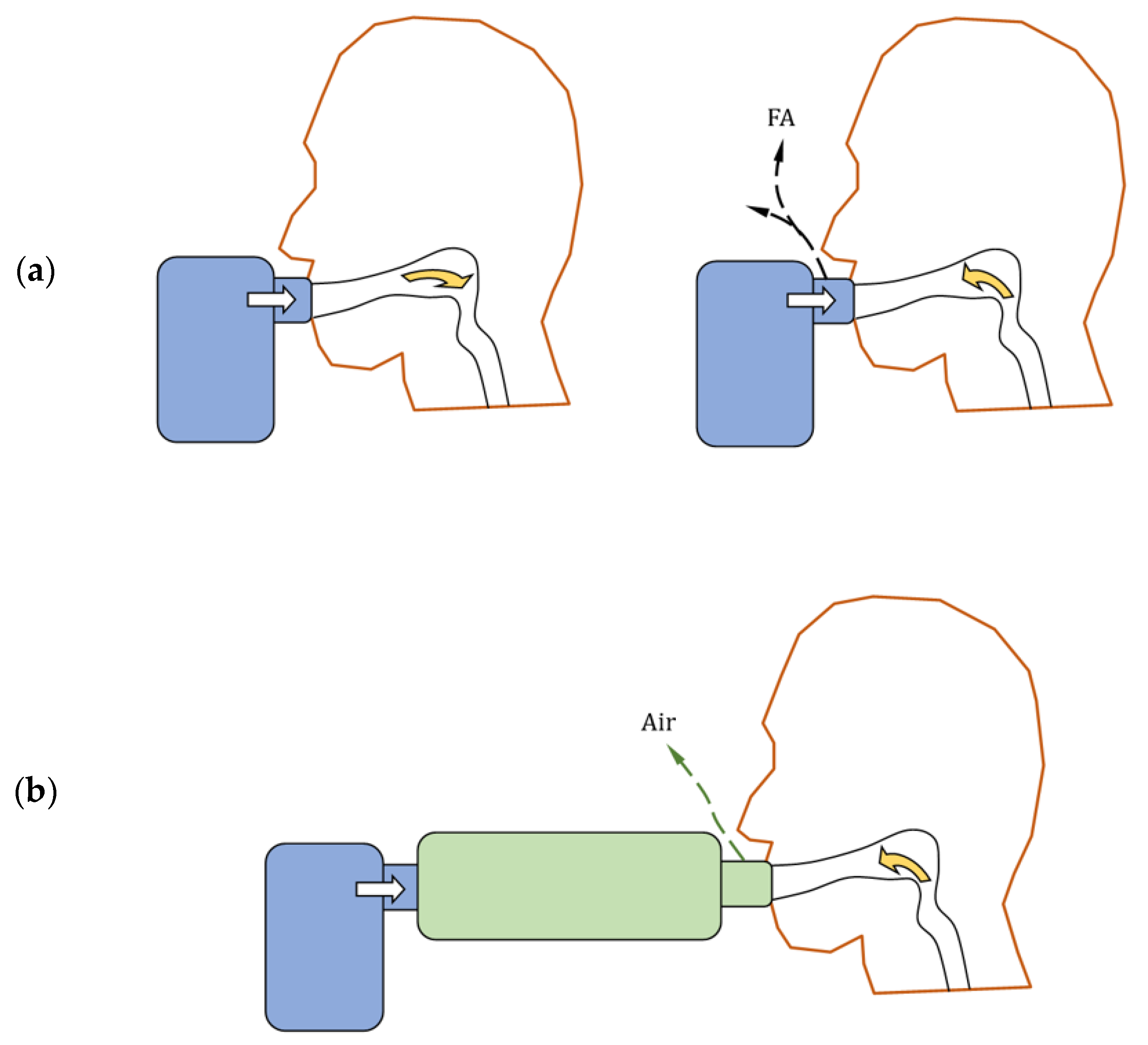
5.1. Nebulizer with a Valved Inhalation Chamber
5.2. Adjusting Aerosol Droplet Size via Physicochemical and Process Parameters of Nebulization
5.3. Targeted Drug Delivery by Functionalized Particles and Non-Conventional Therapeutics
5.4. Better Aerosol Targeting Using Electronic Technologies, Smart Inhalers, and Artificial Intelligence Solutions
6. Conclusions and Future Directions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
References
- Sanders, M. Inhalation therapy: An historical review. Prim. Care Respir. J. 2007, 16, 71–81. [Google Scholar] [CrossRef]
- Stein, S.W.; Thiel, C.G. The history of therapeutic aerosols: A chronological review. J. Aerosol Med. Pulm. Drug Deliv. 2017, 30, 20–41. [Google Scholar] [CrossRef] [PubMed]
- Maccarone, C.; Masiero, S. Spa therapy interventions for post respiratory rehabilitation in COVID-19 subjects: Does the review of recent evidence suggest a role? Environ. Sci. Pollut. Res. 2021, 28, 46063–46066. [Google Scholar] [CrossRef]
- Kostrzon, M.; Sliwka, A.; Wloch, T.; Szpunar, M.; Ankowska, D.; Nowobilski, R. Subterranean pulmonary rehabilitation in chronic obstructive pulmonary disease. Adv. Exp. Med. Biol. 2019, 1176, 35–46. [Google Scholar] [CrossRef] [PubMed]
- Zając, D.; Russjan, E.; Kostrzon, M.; Kaczyńska, K. Inhalations with brine solution from the ‘Wieliczka’ salt mine diminish airway hyperreactivity and inflammation in a murine model of non-atopic asthma. Int. J. Mol. Sci. 2020, 21, 4798. [Google Scholar] [CrossRef] [PubMed]
- Mohanty, R.R.; Das, S. Inhaled insulin—Current direction of insulin research. J. Clin. Diagn. Res. 2017, 11, OE01–OE02. [Google Scholar] [CrossRef]
- Klonoff, D.C. Afrezza inhaled insulin: The fastest-acting FDA-approved insulin on the market has favorable properties. J. Diabetes Sci. Technol. 2014, 8, 1071–1073. [Google Scholar] [CrossRef]
- Osowicka, M.; Janowiak, P.; Gorzewska, A.; Lichodziejewska-Niemierko, M. Inhaled opioids for cancer pain relief: A narrative review. Medicine 2022, 101, e28921. [Google Scholar] [CrossRef]
- De Berardis, D.; Fornaro, M.; Orsolini, L.; Iasevoli, F.; Tomasetti, C.; De Bartolomeis, A.; Serroni, N.; Valchera, A.; Carano, A.; Vellante, F.; et al. The role of inhaled loxapine in the treatment of acute agitation in patients with psychiatric disorders: A clinical review. Int. J. Mol. Sci. 2017, 18, 349. [Google Scholar] [CrossRef]
- Glenardi, G.; Handayani, T.; Barus, J.; Mangkuliguna, G. Inhaled levodopa (CVT-301) for the treatment of Parkinson disease. A systematic review and meta-analysis of randomized controlled trials. Neurol. Clin. Pract. 2022, 12, 139–148. [Google Scholar] [CrossRef]
- Miragoli, M.; Ceriotti, P.; Iafisco, M.; Vacchiano, M.; Salvarani, N.; Alogna, A.; Carullo, P.; Ramirez-Rodríguez, G.B.; Patrício, T.; Degli Esposti, L.; et al. Inhalation of peptide-loaded nanoparticles improves heart failure. Sci. Transl. Med. 2018, 10, eaan6205. [Google Scholar] [CrossRef] [PubMed]
- Newman, S.P. Drug delivery to the lungs: Challenges and opportunities. Ther. Deliv. 2017, 8, 647–661. [Google Scholar] [CrossRef] [PubMed]
- Clark, A.R. Half a century of technological advances in pulmonary drug delivery: A personal perspective. Front. Drug. Deliv. 2022, 2, 871147. [Google Scholar] [CrossRef]
- Laube, B.L.; Janssens, H.M.; de Jongh, F.H.C.; Devadason, S.G.; Dhand, R.; Diot, P.; Everard, M.L.; Horvath, I.; Navalesi, P.; Voshaar, T.; et al. What the pulmonary specialist should know about the new inhalation therapies. Eur. Resp. J. 2011, 37, 1308–1417. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.S. Mechanisms of pharmaceutical aerosol deposition in the respiratory tract. AAPS PharmSciTech. 2014, 15, 630–640. [Google Scholar] [CrossRef]
- Hofmann, W. Modelling inhaled particle deposition in the human lung—A review. J. Aerosol Sci. 2011, 42, 693–724. [Google Scholar] [CrossRef]
- Longest, P.W.; Holbrook, L.T. In silico models of aerosol delivery to the respiratory tract—Development and applications. Adv. Drug Del. Rev. 2012, 64, 296–311. [Google Scholar] [CrossRef]
- Mutuku, J.K.; Hou, W.-C.; Chen, W.-H. An overview of experiments and numerical simulations on airflow and aerosols deposition in human airways and the role of bioaerosol motion in COVID-19 transmission. Aerosol Air Quality Res. 2020, 20, 1172–1196. [Google Scholar] [CrossRef]
- Marple, V.A.; Olson, B.A.; Santhanakrishnan, K.; Roberts, D.L.; Mitchell, J.P.; Hudson-Curtis, B.L. Next generation pharmaceutical impactor: A new impactor for pharmaceutical inhaler testing. Part III. extension of archival calibration to 15 L/min. J. Aerosol Med. 2004, 17, 335–343. [Google Scholar] [CrossRef]
- MPPD: Multiple-Path Particle Dosimetry Model (MPPD v 3.04), Applied Research Associates, Inc. Available online: https://www.ara.com/mppd/ (accessed on 28 November 2023).
- Miravitlles, K.; Auladell-Rispau, A.; Monteagudo, M.; Vázquez-Niebla, J.C.; Mohammed, J.; Nuñez, A.; Urrútia, G. Systematic review on long-term adverse effects of inhaled corticosteroids in the treatment of COPD. Eur. Respir. Rev. 2021, 30, 210075. [Google Scholar] [CrossRef]
- Sonnenberg, A.H.; Taylor, E.; Mondoñedo, J.R.; Jawde, S.B.; Amin, S.D.; Song, J.; Grinstaff, M.W.; Suki, B. Breath hold facilitates targeted deposition of aerosolized droplets in a 3D printed bifurcating airway tree. Ann. Biomed. Eng. 2021, 49, 812–821. [Google Scholar] [CrossRef] [PubMed]
- Khajeh-Hosseini-Dalasm, N.; Longest, P.W. Deposition of particles in the alveolar airways: Inhalation and breath-hold with pharmaceutical aerosols. J. Aerosol Sci. 2015, 79, 15–30. [Google Scholar] [CrossRef] [PubMed]
- Pleil, J.D.; Ariel Geer Wallace, M.; Davis, M.D.; Matty, C.M. The physics of human breathing: Flow, timing, volume, and pressure parameters for normal, on-demand, and ventilator respiration. J. Breath Res. 2021, 15, 042002. [Google Scholar] [CrossRef]
- Kiasadegh, M.; Emdad, H.; Ahmadi, G.; Abouali, O. Transient numerical simulation of airflow and fibrous particles in a human upper airway model. J. Aerosol. Sci. 2020, 140, 105480. [Google Scholar] [CrossRef]
- Sosnowski, T.R.; Moskal, A.; Gradoń, L. Dynamics of oro-pharyngeal aerosol transport and deposition with the realistic flow pattern. Inhalation Toxicol. 2006, 18, 773–780. [Google Scholar] [CrossRef]
- Finlay, W.H. The Mechanics of Inhaled Pharmaceutical Aerosols: An Introduction; Elsevier Science: Amsterdam, The Netherlands, 2001. [Google Scholar]
- Pomerenk, O.; Segura, S.C.; Cao, F.; Wu, J.; Ristroph, L. Hydrodynamics of finite-length pipes at intermediate Reynolds numbers. J. Fluid Mech. 2023, 959, A28. [Google Scholar] [CrossRef]
- Moskal, A.; Gradoń, L. Temporary and spatial deposition of aerosol particles in the upper human airways during breathing cycle. J. Aerosol Sci. 2002, 33, 1525–1539. [Google Scholar] [CrossRef]
- Li, Z.; Kleinstreuer, C.; Zhang, Z. Particle deposition in the human tracheobronchial airways due to transient inspiratory flow patterns. J. Aerosol. Sci. 2007, 38, 625–644. [Google Scholar] [CrossRef]
- Se, C.M.K.; Inthavong, K.; Tu, J. Unsteady particle deposition in a human nasal cavity during inhalation. J. Comput. Multiphase Flows 2010, 2, 207–218. [Google Scholar] [CrossRef]
- Naseri, A.; Shaghaghian, S.; Abouali, O.; Ahmadi, G. Numerical investigation of transient transport and deposition of microparticles under unsteady inspiratory flow in human upper airways. Respir. Physiol. Neurobiol. 2017, 244, 56–72. [Google Scholar] [CrossRef]
- Sosnowski, T.R.; Moskal, A.; Gradoń, L. Mechanims of aerosol particle deposition in the oro-pharynx under non-steady airflow. Ann. Occup. Hyg. 2007, 51, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.L.; Tawhai, M.H.; McLennan, G.; Hoffman, E.A. Characteristics of the turbulent laryngeal jet and its effect on airflow in the human intra-thoracic airways. Respir. Physiol. Neurobiol. 2007, 157, 295–309. [Google Scholar] [CrossRef] [PubMed]
- Xi, J.; Longest, P.W.; Martonen, T.B. Effects of the laryngeal jet on nano- and microparticle transport and deposition in an approximate model of the upper tracheobronchial airways. J. Appl. Physiol. 2008, 104, 1761–1777. [Google Scholar] [CrossRef] [PubMed]
- Gaddam, M.G.; Santhanakrishnan, A. Effects of varying inhalation duration and respiratory rate on human airway flow. Fluids 2021, 6, 221. [Google Scholar] [CrossRef]
- Kadota, K.; Matsumoto, K.; Uchiyama, H.; Tobita, S.; Maeda, M.; Maki, D.; Kinehara, Y.; Tachibana, I.; Sosnowski, T.R.; Tozuka, Y. In silico evaluation of particle transport and deposition in the airways of individual patients with chronic obstructive pulmonary disease. Eur. J. Pharm. Biopharm. 2022, 174, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Haddrell, A.E.; Lewis, D.; Church, T.; Vehring, R.; Murnane, D.; Reid, J.P. Pulmonary aerosol delivery and the importance of growth dynamics. Ther. Deliv. 2017, 8, 1051–1061. [Google Scholar] [CrossRef]
- Wiedmann, T.S.; Ravichandran, A. Ultrasonic nebulization system for respiratory drug delivery. Pharm. Dev. Technol. 2001, 6, 83–89. [Google Scholar] [CrossRef]
- Dalby, R.; Spallek, M.; Voshaar, T. A review of the development of Respimat Soft Mist Inhaler. Int. J. Pharm. 2004, 283, 1–9. [Google Scholar] [CrossRef]
- Ijsebaert, J.C.; Geerse, K.B.; Marijnissen, J.C.M.; Lammers, J.-W.J.; Zanen, P. Electro-hydrodynamic atomization of drug solutions for inhalation purposes. J. Appl. Physiol. 2001, 91, 2735–2741. [Google Scholar] [CrossRef]
- Qi, A.; Friend, J.R.; Yeo, L.Y.; Morton, D.A.V.; McIntosh, M.P.; Spiccia, L. Miniature inhalation therapy platform using surface acoustic wave microfuidic atomization. Lab Chip 2009, 9, 2184–2193. [Google Scholar] [CrossRef]
- Gac, J.; Sosnowski, T.R.; Gradoń, L. Turbulent flow energy for aerosolization of powder particles. J. Aerosol Sci. 2008, 39, 113–126. [Google Scholar] [CrossRef]
- Kamin, W.E.S.; Genz, T.; Roeder, S.; Scheuch, G.; Trammer, T.; Juenemann, R.; Cloes, R.M. Mass output and particle size distribution of glucocorticosteroids emitted from different inhalation devices depending on various inspiratory parameters. J. Aerosol Med. 2002, 15, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Tamadondar, M.R.; Salehi, K.; Abrahamsson, P.; Rasmuson, A. The role of fine excipient particles in adhesive mixtures for inhalation. AIChE J. 2021, 67, e17150. [Google Scholar] [CrossRef]
- Hejduk, A.; Urbańska, A.; Osiński, A.; Łukaszewicz, P.; Domański, M.; Sosnowski, T.R. Technical challenges in obtaining an optimized powder/DPI combination for inhalation delivery of a bi-component generic drug. J. Drug Deliv. Sci. Technol. 2018, 44, 406–414. [Google Scholar] [CrossRef]
- Cassidy, J.P.; Amin, N.; Marino, M.; Gotfried, M.; Meyer, T.; Sommerer, K.; Baughman, R.A. Insulin lung deposition and clearance following Technosphere® insulin inhalation powder administration. Pharm. Res. 2011, 28, 2157–2164. [Google Scholar] [CrossRef] [PubMed]
- Gradoń, L.; Sosnowski, T.R. Formation of particles for dry powder inhalers. Adv. Powder Technol. 2014, 25, 43–55. [Google Scholar] [CrossRef]
- Xia, Y.; Su, Y.; Wang, Q.; Yang, C.; Tang, B.; Zhang, Y.; Tu, J.; Shen, Y. Preparation, characterization, and pharmacodynamics of insulin-loaded fumaryl diketopiperazine microparticle dry powder inhalation. Drug Deliv. 2019, 26, 650–660. [Google Scholar] [CrossRef]
- Sturm, R. A computer model for the simulation of nonspherical particle dynamics in the human respiratory tract. Phys. Res. Int. 2012, 2012, e142756. [Google Scholar] [CrossRef][Green Version]
- Shachar-Berman, L.; Ostrovski, Y.; De Rosis, A.; Kassinos, S.; Sznitman, J. Transport of ellipsoid fibers in oscillatory shear flows: Implications for aerosol deposition in deep airways. Eur. J. Pharm. Sci. 2018, 113, 145–151. [Google Scholar] [CrossRef]
- Shukla, S.K.; Sarode, A.; Kanabar, D.D.; Muth, A.; Kunda, N.K.; Mitragotri, S.; Gupta, V. Bioinspired particle engineering for non-invasive inhaled drug delivery to the lungs. Mater. Sci. Eng. C Mater. Biol. Appl. 2021, 128, 112324. [Google Scholar] [CrossRef]
- Li, J.; Fink, J.B.; MacLoughlin, R.; Dhand, R. A narrative review on trans-nasal pulmonary aerosol delivery. Crit. Care 2020, 24, 506. [Google Scholar] [CrossRef]
- Mac Giolla Eain, M.; MacLoughlin, R. In-Line Aerosol therapy via nasal cannula during adult and paediatric normal, obstructive, and restrictive breathing. Pharmaceutics 2023, 15, 2679. [Google Scholar] [CrossRef] [PubMed]
- Price, D.B.; Pearce, L.; Powell, S.R.; Shirley, J.; Sayers, M.K. Handling and acceptability of the Easi-Breathe device compared with a conventional metered dose inhaler by patients and practice nurses. Int. J. Clin. Pract. 1999, 53, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Worth, H. A comparison of HFA-BDP Autohaler with budesonide Turbuhaler in asthma control of adult patients with mild to moderately severe disease. Respir. Med. 2000, 94 (Suppl. D), S27–S30. [Google Scholar] [CrossRef] [PubMed]
- Dinh, K.; Myers, D.J.; Glazer, M.; Shmidt, T.; Devereaux, C.; Simis, K.; Noymer, P.D.; He, M.; Choosakul, C.; Chen, Q.; et al. In vitro aerosol characterization of Staccato® Loxapine. Int. J. Pharm. 2011, 403, 101–108. [Google Scholar] [CrossRef]
- Pritchard, J.N. Nebulized drug delivery in respiratory medicine: What does the future hold? Ther. Deliv. 2017, 8, 391–399. [Google Scholar] [CrossRef]
- Calabrese, C.; Annunziata, A.; Mariniello, D.F.; Allocca, V.; Imitazione, P.; Cauteruccio, R.; Simioli, F.; Fiorentino, G. Aerosol delivery through high-flow nasal therapy: Technical issues and clinical benefits. Front. Med. 2023, 9, 1098427. [Google Scholar] [CrossRef] [PubMed]
- Azouz, W.; Chrystyn, H. Clarifying the dilemmas about inhalation techniques for dry powder inhalers: Integrating science with clinical practice. Prim. Care Respir. J. 2012, 21, 208–213. [Google Scholar] [CrossRef][Green Version]
- Dorosz, A.; Urbankowski, T.; Zieliński, K.; Michnikowski, M.; Krenke, R.; Moskal, A. Modeling of inhalation profiles through dry powder inhaler in healthy adults and asthma patients as a prerequisite for further in vitro and in silico studies. J. Aerosol Med. Pulm. Drug Deliv. 2022, 35, 91–103. [Google Scholar] [CrossRef]
- Azouz, W.; Chetcuti, P.; Hosker, H.S.; Saralaya, D.; Stephenson, J.; Chrystyn, H. The inhalation characteristics of patients when they use different dry powder inhalers. J. Aerosol Med. Pulm. Drug. Deliv. 2015, 28, 35–42. [Google Scholar] [CrossRef]
- Dorosz, A.; Urbankowski, T.; Zieliński, K.; Michnikowski, M.; Krenke, R.; Moskal, A. Inhalation profiles through a dry powder inhaler: Relation between inhalation technique and spirometric measures. J. Aerosol Med. Pulm. Drug Deliv. 2021, 34, 346–357. [Google Scholar] [CrossRef] [PubMed]
- Dykewicz, M.S.; Hamilos, D.L. Rhinitis and sinusitis. J. Allergy Clin. Immunol. 2010, 125 (Suppl. S2), S103–S115. [Google Scholar] [CrossRef]
- Sosnowski, T.R.; Rapiejko, P.; Sova, J.; Dobrowolska, K. Impact of physicochemical properties of nasal spray products on drug deposition and transport in the pediatric nasal cavity model. Int. J. Pharm. 2020, 574, 118911. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, K.; Van Strien, J.; Singh, N.; Inthavong, K. Primary break-up and atomization characteristics of a nasal spray. PLoS ONE 2020, 15, e0236063. [Google Scholar] [CrossRef]
- Kolanjiyil, A.V.; Alfaifi, A.; Aladwani, G.; Golshahi, L.; Longest, W. Importance of spray-wall interaction and post-deposition liquid motion in the transport and delivery of pharmaceutical nasal sprays. Pharmaceutics 2022, 14, 956. [Google Scholar] [CrossRef] [PubMed]
- Sosnowski, T.R.; Dobrowolska, K. Aerodynamically driven translocation of non-Newtonian fluids: The relevance for intranasal drug delivery. Chem. Eng. Transact. 2021, 86, 1207–1212. [Google Scholar] [CrossRef]
- Möller, W.; Schuschnig, U.; Meyer, G.; Häussinger, K.; Keller, M.; Junge-Hülsing, B.; Mentzel, H. Ventilation and aerosolized drug delivery to the paranasal sinuses using pulsating airflow—A preliminary study. Rhinology 2009, 46, 213–220. [Google Scholar] [CrossRef]
- Pari Sinus 2. Available online: https://www.pari.com/int/products/nose-and-nasal-sinuses/pari-sinus2-int/ (accessed on 19 November 2023).
- Florkiewicz, E.; Taff, J.; Taff, M.; Sosnowski, T.R. Process intensification in medical applications—Use of vibroaerosols for enhanced drug delivery into the paranasal sinuses. In Proceedings of the Abstracts of 8th European Conference of Process Intensification, Warsaw, Poland, 31 May 2023–2 June 2023; p. 38. [Google Scholar]
- Murgia, X.; de Souza Carvalho, C.; Lehr, C.-M. Overcoming the pulmonary barrier: New insights to improve the efficiency of inhaled therapeutics. Eur. J. Nanomed. 2014, 6, 157–169. [Google Scholar] [CrossRef]
- Odziomek, M.; Sosnowski, T.R.; Gradoń, L. Conception, preparation and properties of functional carrier particles for pulmonary drug delivery. Int. J. Pharm. 2012, 433, 51–59. [Google Scholar] [CrossRef]
- Odziomek, M.; Sosnowski, T.R.; Gradoń, L. The influence of Functional Carrier Particles (FCPs) on the molecular transport rate through the reconstructed bronchial mucus—In vitro studies. Transp. Porous Media 2015, 106, 439–454. [Google Scholar] [CrossRef][Green Version]
- Thakur, A.J.; Kaundle, B.; Singh, I. Mucoadhesive drug delivery systems in respiratory diseases. In Targeting Chronic Inflammatory Lung Diseases Using Advanced Drug Delivery Systems; Dua, K., Hansbro, P.N., Wadhwa, R., Haghi, L., Pont, L.G., Wiliams, K.A., Eds.; Academic Press: Cambridge, MA, USA, 2020; pp. 475–491. [Google Scholar] [CrossRef]
- Gradoń, L.; Podgórski, A. Hydrodynamical model of pulmonary clearance. Chem. Eng. Sci. 1989, 44, 741–749. [Google Scholar] [CrossRef]
- Sosnowski, T.R. Particles on the lung surface—Physicochemical and hydrodynamic effects. Curr. Opin. Coll. Interf. Sci. 2018, 36, 1–9. [Google Scholar] [CrossRef]
- Agudelo, C.W.; Samaha, G.; Garcia-Arcos, I. Alveolar lipids in pulmonary disease. A review. Lipids Health Dis. 2020, 19, 122. [Google Scholar] [CrossRef] [PubMed]
- Gradoń, L.; Podgórski, A. Displacement of alveolar macrophages in air space of human lung. Med. Biol. Eng. Comput. 1995, 33, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Sosnowski, T.R.; Gradoń, L.; Iskandar, F.; Okuyama, K. Interaction of deposited aerosol particles with the alveolar liquid layer. In Optimization of Aerosol Drug Delivery; Gradoń, L., Marijnissen, J., Eds.; Kluwer Academic Publishers: Dordrecht, The Netherlands, 2003; pp. 205–216. [Google Scholar]
- Sosnowski, T.R.; Janeczek, K.; Grzywna, K.; Emeryk, A. Mass and volume balances of nebulization process for the determination of the expected dose of liquid medicines delivered by inhalation. Chem. Process. Eng. 2021, 47, 253–261. [Google Scholar] [CrossRef]
- Sosnowski, T.R.; Vilkotsky, A.I.; Emeryk, A. Vibrating mesh nebulizers with a valved inhalation chamber for increased drug delivery to the lower airways. In Respiratory Drug Delivery 2022; Dalby, R.N., Peart, J., Suman, J.D., Young, P.M., Traini, D., Watts, A., Eds.; RDD Online: Richmond, VA, USA, 2022; Volume 1, pp. 551–554. [Google Scholar]
- Sarhan, R.M.; Elberry, A.A.; Abdelwahab, N.S.; Rabea, H.; Salem, M.N.; Abdelrahim, M.E. Effect of a nebulizer holding chamber on aerosol delivery. Respir. Care 2018, 63, 1125–1131. [Google Scholar] [CrossRef] [PubMed]
- Aerogen Ultra. Available online: https://www.aerogen.com/products/aerogen-ultra (accessed on 19 November 2023).
- IntecMedical. Available online: https://www.intecmedical.pl/inhalator-membranowy-siateczkowy-intec-twister-mesh.html (accessed on 19 November 2023).
- Auramedical. Available online: https://www.aura-medical.com/product/aura-portable-nebulizer/ (accessed on 19 November 2023).
- Intec Medical. Available online: https://www.intecmedical.pl/inhalator-membranowo-siateczkowy-turbo-mesh.html (accessed on 19 November 2023).
- Sosnowski, T.R. Mesh nebulizer with an inhalation chamber. Presented at the 24th Conference of Allergologists, Pulmonologists and Clinical Immunologists, Lublin, Poland, 8–10 September 2023, unpublished. [Google Scholar]
- Pari. Available online: https://www.pari.com/int/inhalation-therapy/background-on-inhalation/ (accessed on 19 November 2023).
- Flaem. Available online: https://www.flaem.eu/en/products/aerosol-therapy-lower-airways/4neb (accessed on 19 November 2023).
- Petrocheilou, A.; Tanou, K.; Kalampouka, E.; Malakasioti, G.; Giannios, C.; Kaditis, A.G. Viral croup: Diagnosis and a treatment algorithm. Pediatr. Pulmonol. 2014, 49, 421–429. [Google Scholar] [CrossRef]
- McCallion, O.N.M.; Taylor, K.M.G.; Thomas, M.; Taylor, A.J. Nebulization of fluids of different physicochemical properties with air-jet and ultrasonic nebulizers. Pharm. Res. 1995, 12, 1682–1688. [Google Scholar] [CrossRef]
- McCallion, O.N.M.; Patel, M.J. Viscosity effects on nebulisation of aqueous solutions. Int. J. Pharm. 1996, 130, 245–249. [Google Scholar] [CrossRef]
- Beck-Broichsitter, M.; Oesterheld, N. Electrolyte type and nozzle composition affect the process of vibrating membrane nebulization. Eur. J. Pharm. Biopharm. 2017, 119, 11–16. [Google Scholar] [CrossRef]
- Beck-Broichsitter, M.; Oesterheld, N.; Knuedeler, M.-C.; Seeger, W.; Schmeh, I.T. On the correlation of output rate and aerodynamic characteristics in vibrating-mesh-based aqueous aerosol delivery. Int. J. Pharm. 2014, 461, 34–37. [Google Scholar] [CrossRef]
- Dobrowolska, K.E.; Kinowska, M.; Sosnowski, T.R. Nebulization of solutions containing guar gum as a viscosity modifier of natural origin. In Respiratory Drug Delivery 2022; Dalby, R.N., Peart, J., Suman, J.D., Young, P.M., Traini, D., Watts, A., Eds.; RDD Online: Richmond, VA, USA, 2022; Volume 1, pp. 541–544. [Google Scholar]
- Pulmicort Respules 0.5 mg. Available online: https://www.medicines.org.uk/emc/product/880/smpc (accessed on 28 November 2023).
- Dobrowolska, K.; Miros, M.; Sosnowski, T.R. Impact of natural-based viscosity modifiers of inhalation drugs on the dynamic surface properties of the pulmonary surfactant. Materials 2023, 16, 1975. [Google Scholar] [CrossRef] [PubMed]
- Broniarz-Press, L.; Sosnowski, T.R.; Matuszak, M.; Ochowiak, M.; Jabłczyńska, K. The effect of shear and extensional viscosities on atomization of Newtonian and non-Newtonian fluids in ultrasonic inhaler. Int. J. Pharm. 2015, 485, 41–49. [Google Scholar] [CrossRef]
- Steckel, H.; Eskandar, F. Factors affecting aerosol performance during nebulization with jet and ultrasonic nebulizers. Eur. J. Pharm. Sci. 2003, 19, 443–455. [Google Scholar] [CrossRef]
- Chang, K.H.; Park, B.J.; Nam, K.C. Aerosolization performance of immunoglobulin G by jet and mesh nebulizers. AAPS PharmSciTech 2023, 24, 125. [Google Scholar] [CrossRef]
- Gautam, U.S.; Asrican, R.; Sempowski, G.D. Targeted dose delivery of Mycobacterium tuberculosis in mice using silicon antifoaming agent via aerosol exposure system. PLoS ONE 2022, 17, e0276130. [Google Scholar] [CrossRef] [PubMed]
- Heijerman, H.; Westerman, E.; Conway, S.; Touw, D. Inhaled medication and inhalation devices for lung disease in patients with cystic fibrosis: A European consensus. J. Cystic Fibrosis 2009, 8, 295–315. [Google Scholar] [CrossRef]
- Beck-Broichsitter, M. Aerosol production by vibrating membrane technology: Analysis of the electrolyte effect on generated droplet size and nebulizer output rate. J. Pharm. Sci. 2017, 106, 2168–2172. [Google Scholar] [CrossRef] [PubMed]
- Ochowiak, M.; Kasperkowiak, A.; Doligalski, M.; Sosnowski, T.; Matuszak, M.; Włodarczak, S.; Markowska, M.; Krupińska, A.; Jabłczyńska, K. The thermostated medical jet nebulizer: Aerosol characteristics. Int. J. Pharm. 2019, 567, 118475. [Google Scholar] [CrossRef]
- Dorosz, A.; Moskal, A.; Sosnowski, T.R. Dynamics of aerosol generation and flow during inhalation for improved in vitro-in vivo correlation (IVIVC) of pulmonary medicines. Chem. Proc. Eng. New Front. 2023, 44, e39. [Google Scholar] [CrossRef]
- Montigaud, Y.; Georges, Q.; Leclerc, L.; Clotagatide, A.; Louf-Durier, A.; Pourchez, J.; Prévôt, N.; Périnel-Ragey, S. Impact of gas humidification and nebulizer position under invasive ventilation: Preclinical comparative study of regional aerosol deposition. Sci. Rep. 2023, 13, 11056. [Google Scholar] [CrossRef] [PubMed]
- Ostrovski, Y.; Hofemeier, P.; Sznitman, J. Augmenting regional and targeted delivery in the pulmonary acinus using magnetic particles. Int. J. Nanomed. 2016, 11, 3385–3395. [Google Scholar] [CrossRef]
- Ebrahimi, S.; Shamloo, A.; Alishiri, M.; Mofrad, Y.M.; Akherati, F. Targeted pulmonary drug delivery in coronavirus disease (COVID-19) therapy: A patient-specific in silico study based on magnetic nanoparticles-coated microcarriers adhesion. Int. J. Pharm. 2021, 609, 121133. [Google Scholar] [CrossRef]
- Dames, P.; Gleich, B.; Flemmer, A.; Hajek, K.; Seidl, N.; Wiekhorst, F.; Eberbeck, D.; Bittmann, I.; Bergemann, C.; Weyh, T.; et al. Targeted delivery of magnetic aerosol droplets to the lung. Nat. Nanotechnol. 2007, 2, 495–499. [Google Scholar] [CrossRef]
- Upadhyay, D.; Scalia, S.; Vogel, R.; Wheate, N.; Salama, R.O.; Young, P.M.; Traini, D.; Chrzanowski, W. Magnetised thermo responsive lipid vehicles for targeted and controlled lung drug delivery. Pharm Res. 2012, 29, 2456–2467. [Google Scholar] [CrossRef] [PubMed]
- Saadat, M.; Manshadi, M.K.D.; Mohammadi, M.; Zare, M.J.; Zarei, M.; Kamali, R.; Sanati-Nezhad, A. Magnetic particle targeting for diagnosis and therapy of lung cancers. J. Control. Release 2020, 328, 776–791. [Google Scholar] [CrossRef]
- Knap, K.; Kwiecień, K.; Reczyńska-Kolman, K.; Pamuła, E. Inhalable microparticles as drug delivery systems to the lungs in a dry powder formulations. Regener. Biomat. 2023, 10, rbac099. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zheng, H.; Li, X.; Su, J.; Qin, L.; Sun, Y.; Guo, C.; Beck-Broichsitter, M.; Moehwald, M.; Chen, L.; et al. Phospholipid-modified poly(lactide-co-glycolide) microparticles for tuning the interaction with alveolar macrophages: In vitro and in vivo assessment. Eur. J. Pharm. Biopharm. 2019, 143, 70–79. [Google Scholar] [CrossRef]
- Li, J.; Zheng, H.; Xu, E.-Y.; Moehwald, M.; Chen, L.; Zhang, X.; Mao, S. Inhalable PLGA microspheres: Tunable lung retention and systemic exposure via polyethylene glycol modification. Acta Biomater. 2021, 123, 325–334. [Google Scholar] [CrossRef]
- Scalia, S.; Haghi, M.; Losi, V.; Trotta, V.; Young, P.M.; Traini, D. Quercetin solid lipid microparticles: A flavonoid for inhalation lung delivery. Eur. J. Pharm. Sci. 2013, 49, 278–285. [Google Scholar] [CrossRef]
- Alhajj, N.; O’Reilly, N.J.; Cathcart, H. Leucine as an excipient in spray dried powder for inhalation. Drug Disc. Today 2021, 26, 2384–2396. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Harinck, L.; Lokras, A.G.; Gerde, P.; Selg, E.; Sjöberg, C.-O.; Franzyk, H.; Thakur, A.; Foged, C. Leucine improves the aerosol performance of dry powder inhaler formulations of siRNA-loaded nanoparticles. Int. J. Pharm. 2022, 621, 121758. [Google Scholar] [CrossRef] [PubMed]
- Ógáin, O.N.; Li, J.; Tajber, L.; Corrigan, O.I.; Healy, A.M. Particle engineering of materials for oral inhalation by dry powder inhalers. I—Particles of sugar excipients (trehalose and raffinose) for protein delivery. Int. J. Pharm. 2011, 405, 23–35. [Google Scholar] [CrossRef]
- Sosnowski, T.R.; Gradoń, L. Modification of inhalable powders by pulmonary surfactant components adsorbed on droplets during spray-drying process. Coll. Surf. A Physicochem. Eng. Asp. 2010, 365, 56–61. [Google Scholar] [CrossRef]
- Jabłczyńska, K.; Janczewska, M.; Kulikowska, A.; Sosnowski, T.R. Preparation and characterization of biocompatible polymer particles as potential nanocarriers for inhalation therapy. Int. J. Polymer Sci. 2015, 2015, 763020. [Google Scholar] [CrossRef]
- Bisserier, M.; Sun, X.-Q.; Fazal, S.; Turnbull, I.C.; Bonnet, S.; Hadri, L. Novel insights into the therapeutic potential of lung-targeted gene transfer in the most common respiratory diseases. Cells 2022, 11, 984. [Google Scholar] [CrossRef]
- Agent, P.; Parrott, H. Inhaled therapy in cystic fibrosis: Agents, devices and regimens. Breathe 2015, 11, 110–118. [Google Scholar] [CrossRef]
- Rowe, S.; Zuckerman, J.; Dorgan, D.; Lascano, J.; McCoy, K.; Jain, M.; Schechter, M.; Lommatzsch, S.; Indihar, V.; Lechtzin, N.; et al. Inhaled mRNA therapy for treatment of cystic fibrosis: Interim results of a randomized, double-blind, placebo-controlled phase 1/2 clinical study. J. Cystic Fibr. 2023, 22, 656–664. [Google Scholar] [CrossRef]
- Zarogoulidis, P.; Darwiche, K.; Hohenforst-Schmidt, W.; Huang, H.; Li, Q.; Freitag, L.; Zarogoulidis, K. Inhaled gene therapy in lung cancer: Proof-of-concept for nano-oncology and nanobiotechnology in the management of lung cancer. Future Oncol. 2013, 9, 1171–1794. [Google Scholar] [CrossRef]
- Ichikawa, M.; Muramatsu, N.; Matsunaga, W.; Ishikawa, T.; Okuda, T.; Okamoto, H.; Gotoh, A. Effects of inhalable gene transfection as a novel gene therapy for non-small cell lung cancer and malignant pleural mesothelioma. Sci. Rep. 2022, 12, 8634. [Google Scholar] [CrossRef]
- Storti, C.; Le Noci, V.; Sommariva, M.; Tagliabue, E.; Balsari, A.; Sfondrini, L. Aerosol delivery in the treatment of lung cancer. Curr. Cancer Drug Target. 2015, 15, 604–612. [Google Scholar] [CrossRef]
- Wang, X.; Xie, Z.; Zhao, J.; Zhu, Z.; Yang, C.; Liu, Y. Prospects of inhaled phage therapy for combatting pulmonary infections. Front. Cell. Infect. Microbiol. 2021, 11, 758392. [Google Scholar] [CrossRef]
- Sosnowski, T.R.; Kurowska, A.; Butruk, B.; Jabłczyńska, K. Spraying of cell colloids in medical atomizers. Chem. Eng. Transact. 2013, 32, 2257–2262. [Google Scholar]
- Zambrano, G.M.T.; Ahmed, Y.M.; Carmenate, Y.V.; Elsadawy, M.E. Stem cell nebulization therapy for COVID-19 infection: Radiological and clinical outcomes. Egypt J. Radiol. Nucl. Med. 2021, 52, 115. [Google Scholar] [CrossRef]
- Kikidis, D.; Konstantinos, V.; Tzovaras, D.; Usmani, O.S. The digital asthma patient: The history and future of inhaler based health monitoring devices. J. Aerosol Med. Pulm. Drug Deliv. 2016, 29, 219–232. [Google Scholar] [CrossRef]
- Mosnaim, G.S.; Greiwe, J.; Jariwala, S.P.; Pleasants, R.; Merchant, R. Digital inhalers and remote patient monitoring for asthma. J. Allergy Clin. Immunol. Pract. 2022, 10, 2525–2533. [Google Scholar] [CrossRef] [PubMed]
- Zhao, M.; Hoti, K.; Wang, H.; Raghu, A.; Katabi, D. Assessment of medication self-administration using artificial intelligence. Nat. Med. 2021, 27, 727–735. [Google Scholar] [CrossRef] [PubMed]
- Denyer, J.; Dyche, T. The Adaptive Aerosol Delivery (AAD) technology: Past, present, and future. J. Aerosol Med. Pulm. Drug Deliv. 2010, 23 (Suppl. 1), S1–S10. [Google Scholar] [CrossRef] [PubMed]
- Roszczyk, P.; Sosnowski, T.; Moskal, A.; Klucz, E.; Srutek, M.; Bujnowski, S.; Wirwicki, M.; Wisniewski, W.; Klucz, K. Capsule Inhaler, Method for Monitoring Intake of a Substance, Computer Program and Computer Program. Product. Patent LU501909B1, 1 December 2022. [Google Scholar]
- Xiroudaki, S.; Schoubben, A.; Giovagnoli, S.; Rekkas, D.M. Dry Powder Inhalers in the digitalization era: Current status and future perspectives. Pharmaceutics 2021, 13, 1455. [Google Scholar] [CrossRef]
- Häußermann, S.; Arendsen, L.J.; Pritchard, J.N. Smart dry powder inhalers and intelligent adherence management. Adv. Drug Deliv. Rev. 2022, 191, 114580. [Google Scholar] [CrossRef] [PubMed]
- I-neb AAD System. Battery-Powered Drug Delivery Device. Available online: https://www.philips.co.uk/healthcare/product/HC85167/i-neb-battery-powered-drug-delivery-system (accessed on 28 November 2023).
- Breelib Inhalation System. Available online: https://www.vectura.com/wp-content/uploads/2023/03/DAW-00058-08.pdf (accessed on 28 November 2023).
- AKITA® JET Inhalation System. Instructions for Use. Available online: https://www.vectura.com/wp-content/uploads/2022/06/daw-00025-06.pdf (accessed on 28 November 2023).
- Fischer, A.; Stegemann, J.; Scheuch, G.; Siekmeier, R. Novel devices for individualized controlled inhalation can optimize aerosol therapy in efficacy, patient care and power of clinical trials. Eur. J. Med. Res. 2009, 14 (Suppl. 4), 71–77. [Google Scholar] [CrossRef]
- Cipolla, D.; Chan, H.-K.; Schuster, J.; Farina, D. Personalized medicine: Development of inhalation systems tailored to the individual. Ther. Deliv. 2010, 1, 667–682. [Google Scholar] [CrossRef] [PubMed]
- Komalla, V.; Wong, C.Y.J.; Sibum, I.; Muellinger, B.; Nijdam, W.; Chaugule, V.; Soria, J.; Ong, H.X.; Buchmann, N.A.; Traini, D. Advances in soft mist inhalers. Expert Opin. Drug Deliv. 2023, 20, 1055–1070. [Google Scholar] [CrossRef] [PubMed]
- Hailie Smart Inhaler. Available online: https://www.hailie.com/ (accessed on 28 November 2023).
- Findair One Add-On Devices. Available online: https://findair.eu/products/findair-one-addons.html (accessed on 28 November 2023).
- Propeller Health. Available online: https://propellerhealth.com/our-platform/ (accessed on 28 November 2023).
- CapMedic—Simplifying Respiratory Care by Correct and Regular Inhaler Use. Available online: https://capmedicinhaler.com/ (accessed on 28 November 2023).
- Amiko. Upgrading Respiratory Care with Digital Medicines. Available online: https://www.amiko.io/ (accessed on 28 November 2023).
- Digihaler. Available online: https://www.digihaler.com/ (accessed on 28 November 2023).



| Pressurized Metered Dose Inhalers (pMDIs) | Dry Powder Inhalers (DPIs) | Nebulizers | Other (Examples) |
|---|---|---|---|
| Hand-actuated | Single dose (capsule) | Pneumatic (jet) | Soft mist inhaler (Respimat® SMI, Ingelheim Boehringer, Ingelheim am Rhein, Germany) [40] |
| Breath-actuated (mechanical) [55,56] | Containing pre-metered doses (on blister) | Ultrasonic
| Thermal vaporization (sublimation/resublimation) breath actuated inhaler (Staccato®, Alexza Pharmaceuticals, Mountain View, CA, USA) [57] |
| They can be used both with or without holding chamber (or spacer) | Metering the dose from powder reservoir |
| Name of the System | Basic Characteristics | ‘Smart’ Functions |
|---|---|---|
| Group 1: Nebulizers and fine mist inhalers | ||
| I-neb® AAD® (Adaptive Aerosol Delivery) [138] | Hand-held VMN system with electronic interface which measures pressure changes in the airflow | The system sets the duration of aerosol pulse to deliver the drug only in the first phase of inspiration by continuously adapting to changes in breathing pattern. It maximizes the delivered dose and minimizes drug losses [134]. |
| Breelib™ [139] | Breath-activated VMN | The system controls the flow and inhaled volume to maximize the dose delivered to deep lung regions. |
| Akita® Jet [140] | Electronic system used to optimize drug delivery from the jet nebulizer | The system guides the patient to inhale with a required inspiratory flow rate and time, increasing the targeted drug delivery to deep lung regions [141]. |
| AERx® | Fine mist aerosol inhaler with breath control technology. Drug dose is delivered one or two breaths from single-use AERx Strip | The system releases aerosol during the first phase of inhalation and controls the inhalation flow, increasing the targeted drug delivery to deep lung regions. The system with AERx Strip may be a platform for personalized aerosol therapy [142,143]. |
| Group 2: Attachable (add-on) devices/accessories/sensors for pMDIs and DPIs | ||
| Hailie® [144] | Electronic attachable sensor for several models of pMDI or DPI | The sensor records time/date each actuation of pMDI or DPI. Some versions may also detect inhaler shaking prior to use and flow during inhalation. |
| FindAir® One [145] | Electronic module attached to the top of pMDI or on some DPIs | The sensor transmits the information regarding the inhaler use to the mobile phone application. |
| Propeller® [146] | Electronic module attached to the top of pMDI | The sensor detects and records the time of actuation of pMDIs or DPIs. |
| Capmedic® [147] | Electronic module attached to the top of pMDI | The sensor records shaking, the upright position of pMDI, proper timing of the actuation, the and duration of inhalation. It also records the time of pMDI actuation. |
| Respiro® [148] | Electronic attachable sensor | The sensor records the actuation and flow of inhalation in DPIs or pMDIs. |
| Group 3: DPIs—built-in systems | ||
| Digihaler® [149] | Electronic built-in sensor | The sensor records each actuation and the flow of inhalation. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sosnowski, T.R. Towards More Precise Targeting of Inhaled Aerosols to Different Areas of the Respiratory System. Pharmaceutics 2024, 16, 97. https://doi.org/10.3390/pharmaceutics16010097
Sosnowski TR. Towards More Precise Targeting of Inhaled Aerosols to Different Areas of the Respiratory System. Pharmaceutics. 2024; 16(1):97. https://doi.org/10.3390/pharmaceutics16010097
Chicago/Turabian StyleSosnowski, Tomasz R. 2024. "Towards More Precise Targeting of Inhaled Aerosols to Different Areas of the Respiratory System" Pharmaceutics 16, no. 1: 97. https://doi.org/10.3390/pharmaceutics16010097
APA StyleSosnowski, T. R. (2024). Towards More Precise Targeting of Inhaled Aerosols to Different Areas of the Respiratory System. Pharmaceutics, 16(1), 97. https://doi.org/10.3390/pharmaceutics16010097







