In-Line Aerosol Therapy via Nasal Cannula during Adult and Paediatric Normal, Obstructive, and Restrictive Breathing
Abstract
:1. Introduction
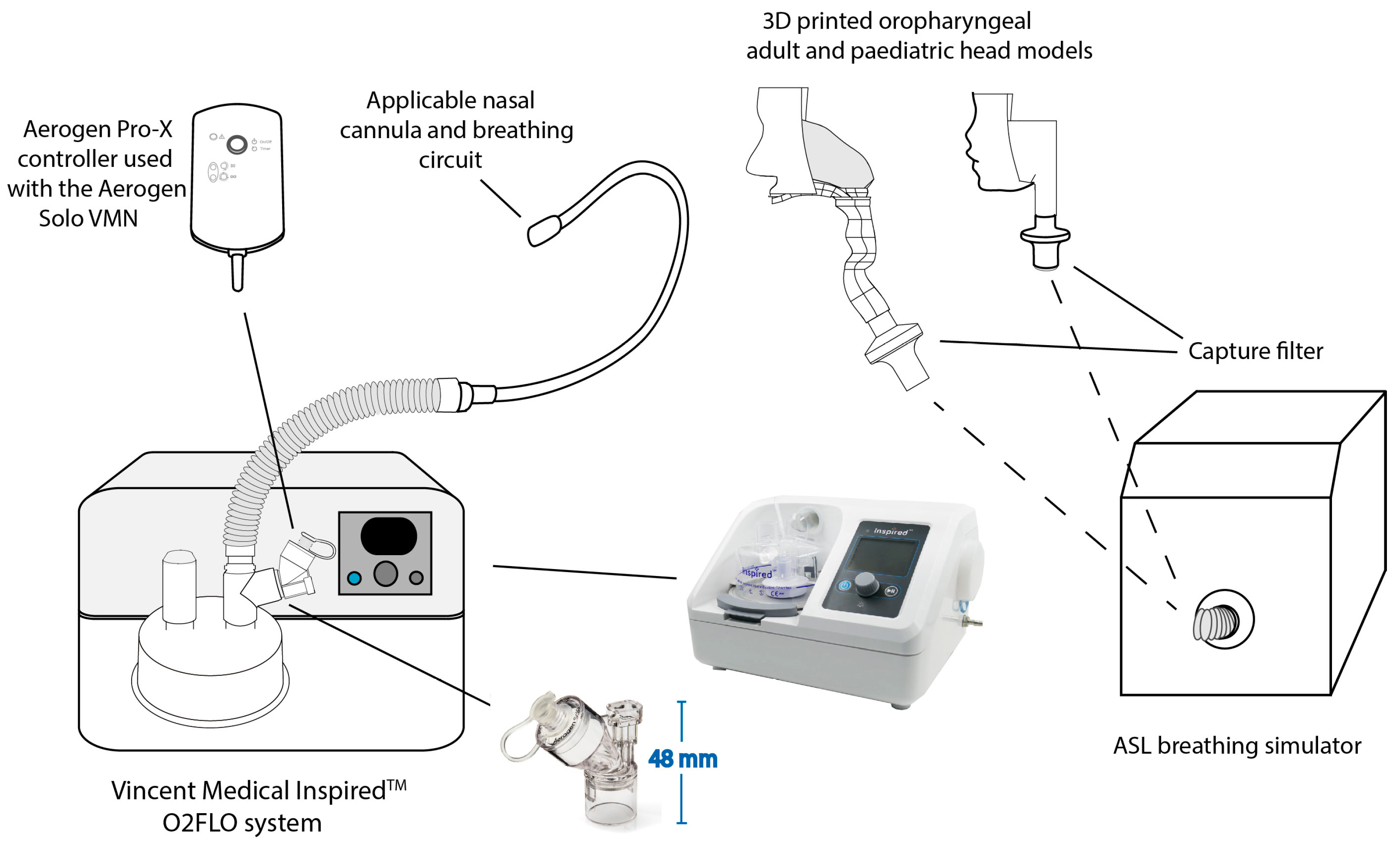
2. Materials and Methods
2.1. Nebuliser
2.2. High-Flow Nasal Therapy System
2.3. Characterisation of Aerosol Dose
3. Results
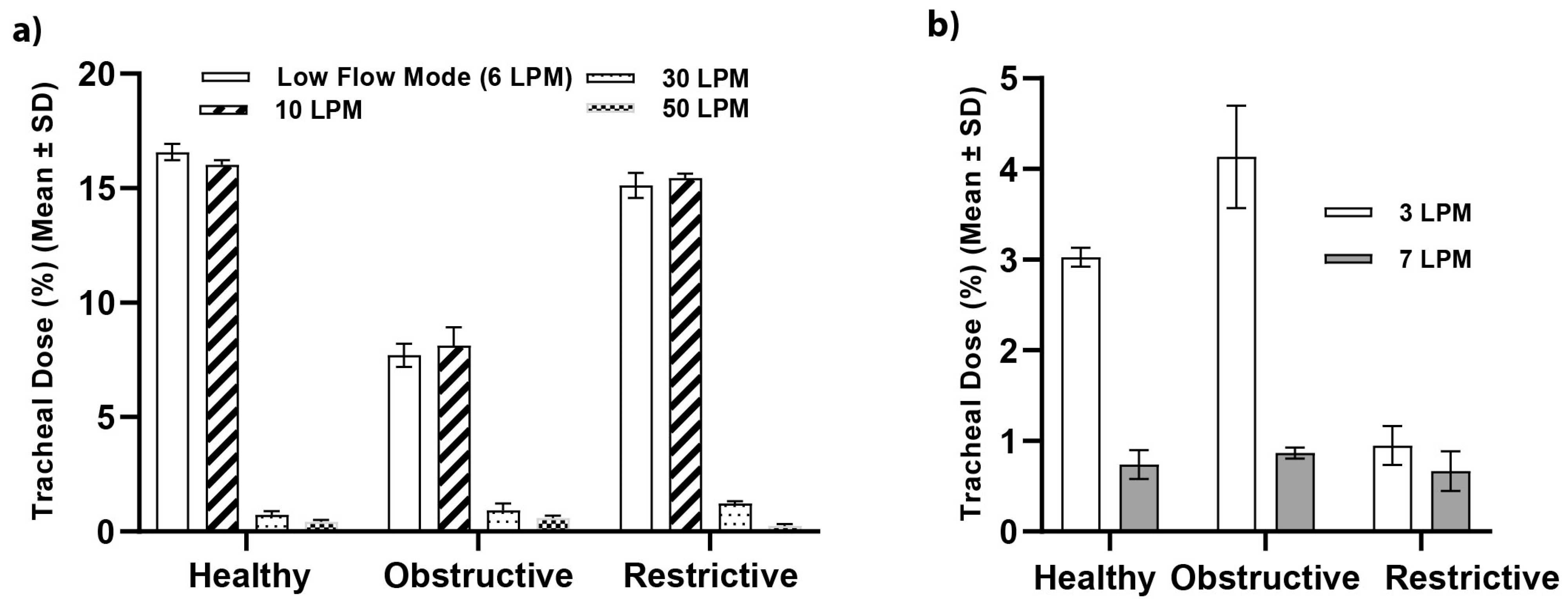
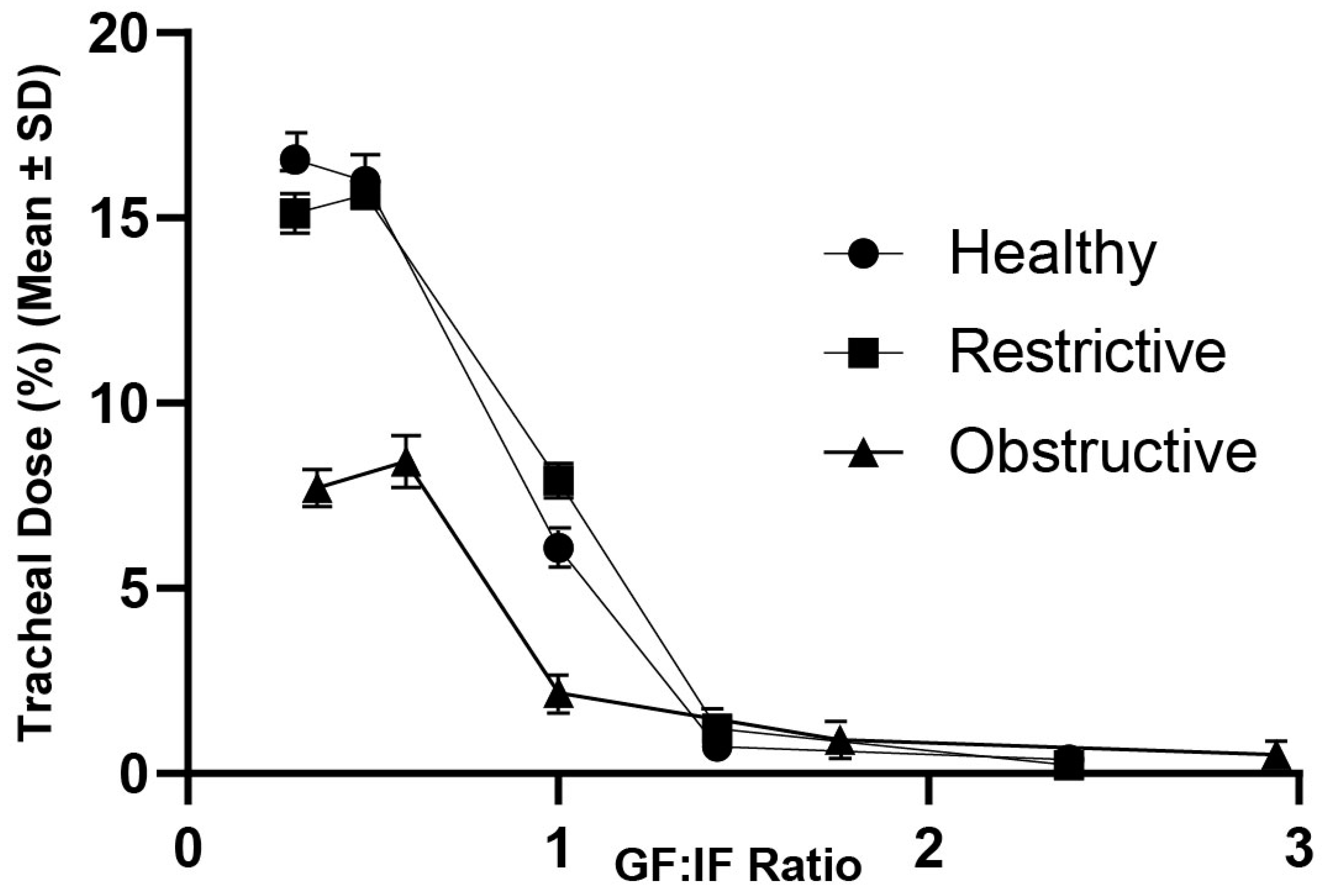
3.1. Tracheal Dose
3.2. Delivery at Peak Inspiratory Flow
3.3. Positive End-Expiratory Pressure
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Geng, W.; Batu, W.; You, S.; Tong, Z.; He, H. High-Flow Nasal Cannula: A Promising Oxygen Therapy for Patients with Severe Bronchial Asthma Complicated with Respiratory Failure. Can. Respir. J. 2020, 2020, 2301712. [Google Scholar] [CrossRef] [PubMed]
- McGinley, B.; Halbower, A.; Schwartz, A.R.; Smith, P.L.; Patil, S.P.; Schneider, H. Effect of a High-Flow Open Nasal Cannula System on Obstructive Sleep Apnea in Children. Pediatrics 2009, 124, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Baravalle-Einaudi, M.; Dufeu, N.; Dupont, C.; Vecellio, L.; Delaisi, B.; Carsin, A.; Dubus, J.-C. Vibrating-mesh nebulizer maintenance by CF patients: Results from a French survey. Pulm. Pharmacol. Ther. 2017, 44, 57–60. [Google Scholar] [CrossRef] [PubMed]
- Elshof, J.; Duiverman, M.L. Clinical Evidence of Nasal High-Flow Therapy in Chronic Obstructive Pulmonary Disease Patients. Respiration 2020, 99, 140–153. [Google Scholar] [CrossRef] [PubMed]
- Madney, Y.M.; Fathy, M.; Elberry, A.A.; Rabea, H.; Abdelrahim, M.E. Aerosol Delivery Through an Adult High-Flow Nasal Cannula Circuit Using Low-Flow Oxygen. Respir. Care 2019, 64, 453–461. [Google Scholar] [CrossRef] [PubMed]
- Colaianni-Alfonso, N.; Montiel, G.; Castro-Sayat, M.; Siroti, C.; Vega, M.L.; Toledo, A.; Haedo, S.; Previgliano, I.; Mazzinari, G.; Alonso-Íñigo, J.M. Combined Noninvasive Respiratory Support Therapies to Treat COVID-19. Respir. Care 2021, 66, 1831–1839. [Google Scholar] [CrossRef] [PubMed]
- Bräunlich, J.; Köhler, M.; Wirtz, H. Nasal highflow improves ventilation in patients with COPD. Int. J. Chronic Obstr. Pulm. Dis. 2016, 11, 1077–1085. [Google Scholar] [CrossRef]
- Onodera, Y.; Akimoto, R.; Suzuki, H.; Okada, M.; Nakane, M.; Kawamae, K. A high-flow nasal cannula system with relatively low flow effectively washes out CO2 from the anatomical dead space in a sophisticated respiratory model made by a 3D printer. Intensiv. Care Med. Exp. 2018, 6, 7. [Google Scholar] [CrossRef]
- Fraser, J.F.; Spooner, A.J.; Dunster, K.R.; Anstey, C.M.; Corley, M. Nasal high flow oxygen therapy in patients with COPD reduces respiratory rate and tissue carbon dioxide while increasing tidal and end-expiratory lung volumes: A randomised crossover trial Research letter. Thorax 2016, 71, 759–761. [Google Scholar] [CrossRef]
- Tian, G.; Hindle, M.; Worth Longest, P. Targeted Lung Delivery of Nasally Administered Aerosols. Aerosol Sci. Technol. 2015, 48, 434–449. [Google Scholar] [CrossRef]
- Li, J.; Tu, M.; Yang, L.; Jing, G.; Fink, J.B.; Burtin, C.; de Andrade, A.D.; Gong, L.; Xie, L.; Ehrmann, S. Worldwide Clinical Practice of High-Flow Nasal Cannula and Concomitant Aerosol Therapy in the Adult ICU Setting. Respir. Care 2021, 66, 1416–1424. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.G.; Gentile, M.A.; Tyler, L.M.; Napolitano, N. High-Flow Nasal Cannula in Pediatric Patients: A Survey of Clinical Practice. Respir. Care 2018, 63, 894–899. [Google Scholar] [CrossRef] [PubMed]
- Murphy, B.; Eain, M.M.G.; Joyce, M.; Fink, J.B.; MacLoughlin, R. Evaluation of aerosol drug delivery with concurrent low- and high-flow nasal oxygen. ERJ Open Res. 2022, 8, 00220–02022. [Google Scholar] [CrossRef] [PubMed]
- Alcoforado, L.; Ari, A.; Barcelar, J.D.M.; Brandão, S.C.S.; Fink, J.B.; De Andrade, A.D. Impact of Gas Flow and Humidity on Trans-Nasal Aerosol Deposition via Nasal Cannula in Adults: A Randomized Cross-Over Study. Pharmaceutics 2019, 11, 320. [Google Scholar] [CrossRef] [PubMed]
- Calabrese, C.; Annunziata, A.; Mariniello, D.F.; Allocca, V.; Imitazione, P.; Cauteruccio, R.; Simioli, F.; Fiorentino, G. Aerosol delivery through high-flow nasal therapy: Technical issues and clinical benefits. Front. Med. 2023, 9, 1098427. [Google Scholar] [CrossRef] [PubMed]
- Dugernier, J.; Hesse, M.; Jumetz, T.; Bialais, E.; Roeseler, J.; Depoortere, V.; Michotte, J.-B.; Wittebole, X.; Ehrmann, S.; Laterre, P.-F.; et al. Aerosol Delivery with Two Nebulizers Through High-Flow Nasal Cannula: A Randomized Cross-Over Single-Photon Emission Computed Tomography-Computed Tomography Study. J. Aerosol Med. Pulm. Drug Deliv. 2017, 30, 349–358. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Williams, L.; Fink, J.B. The Impact of High-Flow Nasal Cannula Device, Nebulizer Type, and Placement on Trans-Nasal Aerosol Drug Delivery. Respir. Care 2021, 67, 1–8. [Google Scholar] [CrossRef]
- Lellouche, F.; Rousseau, E.; Bouchard, P.-A. Evaluation of the humidification performances of new generation of heated wire humidifiers. Respir. Care 2023, 68, 11352. [Google Scholar] [CrossRef]
- Perry, S.A.; Kesser, K.C.R.; Geller, D.E.; Selhorst, D.M.R.-N.; Rendle, J.K.R.; Hertzog, J.H. Influences of Cannula Size and Flow Rate on Aerosol Drug Delivery Through the Vapotherm Humidified High-Flow Nasal Cannula System. Pediatr. Crit. Care Med. 2013, 14, e250–e256. [Google Scholar] [CrossRef]
- Bennett, G.; Joyce, M.; Sweeney, L.; MacLoughlin, R. In Vitro Study of the Effect of Breathing Pattern on Aerosol Delivery During High-Flow Nasal Therapy. Pulm. Ther. 2019, 5, 43–54. [Google Scholar] [CrossRef]
- Dailey, P.A.; Harwood, R.; Walsh, K.; Fink, J.B.; Thayer, T.; Gagnon, G.; Ari, A. Aerosol delivery trough adult high flow nasal cannula with heliox and oxygen. Respir. Care 2017, 69, 1186–1192. [Google Scholar] [CrossRef] [PubMed]
- Caille, V.; Ehrmann, S.; Boissinot, E.; Perrotin, D.; Diot, P.; Dequin, P.-F. Influence of Jet Nebulization and Oxygen Delivery on the Fraction of Inspired Oxygen: An Experimental Model. J. Aerosol Med. Pulm. Drug Deliv. 2009, 22, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Chiang, C.-E.; Li, H.-H.; Rowley, D.D.; Fang, T.-P.; Lin, H.-L. Influence of Aerosol Mask Design on Fugitive Aerosol Concentrations During Nebulization. Respir. Care 2023, 68, 1510–1518. [Google Scholar] [CrossRef]
- Bräunlich, J.; Wirtz, H. Oral Versus Nasal High-Flow Bronchodilator Inhalation in Chronic Obstructive Pulmonary Disease. J. Aerosol Med. Pulm. Drug Deliv. 2018, 31, 248–254. [Google Scholar] [CrossRef] [PubMed]
- Bennett, G.; Joyce, M.; Sweeney, L.; MacLoughlin, R. In Vitro Determination of the Main Effects in the Design of High-Flow Nasal Therapy Systems with Respect to Aerosol Performance. Pulm. Ther. 2018, 4, 73–86. [Google Scholar] [CrossRef] [PubMed]
- Réminiac, F.; Vecellio, L.; Mac Loughlin, R.; Le Pennec, D.; Cabrera, M.; Vourc’H, N.H.; Fink, J.B.; Ehrmann, S. Nasal high flow nebulization in infants and toddlers: An in vitro and in vivo scintigraphic study. Pediatr. Pulmonol. 2016, 52, 337–344. [Google Scholar] [CrossRef]
- Golshahi, L.; Longest, P.W.; Azimi, M.; Syed, A.; Hindle, M. Intermittent Aerosol Delivery to the Lungs During High-Flow Nasal Cannula Therapy. Respir. Care 2014, 59, 1476–1486. [Google Scholar] [CrossRef]
- Ari, A. Aerosol Drug Delivery Through High Flow Nasal Cannula. Curr. Pharm. Biotechnol. 2018, 18, 877–882. [Google Scholar] [CrossRef]
- Li, J.; Gong, L.; Fink, J.B. The Ratio of Nasal Cannula Gas Flow to Patient Inspiratory Flow on Trans-nasal Pulmonary Aerosol Delivery for Adults: An in Vitro Study. Pharmaceutics 2019, 11, 225. [Google Scholar] [CrossRef]
- Réminiac, F.; Vecellio, L.; Heuzé-Vourc’H, N.; Petitcollin, A.; Respaud, R.; Cabrera, M.; Le Pennec, D.; Diot, P.; Ehrmann, S.; Bräunlich, J.; et al. Aerosol Therapy in Adults Receiving High Flow Nasal Cannula Oxygen Therapy. J. Aerosol Med. Pulm. Drug Deliv. 2016, 29, 134–141. [Google Scholar] [CrossRef]
- MacLoughlin, R.J.; Higgins, B.D.; Laffey, J.G.; O’Brien, T. Optimized Aerosol Delivery to a Mechanically Ventilated Rodent. J. Aerosol Med. Pulm. Drug Deliv. 2009, 22, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Xi, J.; Si, X.; Longest, W. Electrostatic Charge Effects on Pharmaceutical Aerosol Deposition in Human Nasal–Laryngeal Airways. Pharmaceutics 2014, 6, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Rygg, A.; Longest, P.W.; Roche, N.; Dekhuijzen, P.R.; Mehta, R.; Montembault, M.; Warren, F.; Gupta, A.; Brealey, N.; Moore, A.; et al. Absorption and Clearance of Pharmaceutical Aerosols in the Human Nose: Development of a CFD Model. J. Aerosol Med. Pulm. Drug Deliv. 2016, 29, 416–431. [Google Scholar] [CrossRef]
- IngMar Medical. Simulator Software, 1st ed.; Patient Model References. ASL 5000 Breath; IngMar Medical: Pittsburgh, PA, USA, 2015; pp. 1–13. [Google Scholar]
- Gallagher, L.; Joyce, M.; Murphy, B.; Eain, M.M.G.; MacLoughlin, R. The Impact of Head Model Choice on the In Vitro Evaluation of Aerosol Drug Delivery. Pharmaceutics 2021, 14, 24. [Google Scholar] [CrossRef] [PubMed]
- Bhashyam, A.R.; Wolf, M.T.; Marcinkowski, A.L.; Saville, A.; Thomas, K.; Carcillo, J.A.; Corcoran, T.E. Aerosol Delivery through Nasal Cannulas: An In Vitro Study. J. Aerosol Med. Pulm. Drug Deliv. 2008, 21, 181–188. [Google Scholar] [CrossRef]
- Bauer, A.; McGlynn, P.; Bovet, L.L.; Mims, P.L.; Curry, L.A.; Hanrahan, J.P. The influence of breathing pattern during nebulization on the delivery of arformoterol using a breath simulator. Respir. Care 2009, 54, 1488–1492. [Google Scholar]
- Pisani, L.; Vega, M.L. Use of Nasal High Flow in Stable COPD: Rationale and Physiology. COPD J. Chronic Obstr. Pulm. Dis. 2017, 14, 346–350. [Google Scholar] [CrossRef]
- Garofalo, E.; Bruni, A.; Pelaia, C.; Cammarota, G.; Murabito, P.; Biamonte, E.; Abdalla, K.; Longhini, F.; Navalesi, P. Evaluation of a New Interface Combining High-Flow Nasal Cannula and CPAP. Respir. Care 2019, 64, 1231–1239. [Google Scholar] [CrossRef]
| Adult | Paediatric | |||||
|---|---|---|---|---|---|---|
| Healthy | Obstructive | Restrictive | Healthy | Obstructive | Restrictive | |
| Breath Rate (BPM) | 15 | 22 | 15 | 20 | 20 | 30 |
| Tidal Volume (mL) | 500 | 270 | 500 | 300 | 350 | 70 |
| I:E Ratio | 1.0:1.0 | 1.0:2.5 | 1.0:1.0 | 1.0:2.0 | 1.0:1.8 | 1.0:2.85 |
| Compliance (L/cmH2O) | 0.05 | 0.080 | 0.04 | 0.01 | 0.08 | 0.05 |
| Resistance (cmH20/L/S) | 5 | 20 | 20 | 30 | 5 | 25 |
| GF:IF ratio | 0.29–2.38 | 0.35–2.94 | 0.29–2.38 | - | - | - |
| Low Flow Mode (6 LPM) (Mean ± SD) | 10 LPM (Mean ± SD) | p-Value | |
|---|---|---|---|
| Healthy | 16.58 ± 0.36 | 15.99 ± 0.71 | 0.344 |
| Obstructive | 7.70 ± 0.51 | 8.42 ± 0.70 | 0.253 |
| Restrictive | 15.12 ± 0.54 | 15.63 ± 0.30 | 0.573 |
| Adult | ||
|---|---|---|
| Peak Flow (LPM) | Tracheal Dose (%) (Mean ± SD) | |
| Healthy | 21 | 6.09 ± 0.18 |
| Restrictive | 21 | 7.90 ± 0.48 |
| Obstructive | 17 | 2.17 ± 0.21 |
| Low Flow (6 LPM) | ||||
|---|---|---|---|---|
| PEEP (cm H2O) | ||||
| Lung Health | Pre-nebulisation | During | Post nebulisation | P-value |
| Healthy | 0.113 ± 0.003 | 0.122 ± 0.009 | 0.115 ± 0.012 | 0.472 |
| Restrictive | 0.065 ± 0.002 | 0.072 ± 0.002 | 0.065 ± 0.005 | 0.077 |
| Obstructive | 0.130 ± 0.006 | 0.163 ± 0.011 | 0.158 ± 0.008 | 0.033 |
| 10 LPM | ||||
| Healthy | 0.139 ± 0.004 | 0.141 ± 0.007 | 0.147 ± 0.006 | 0.084 |
| Restrictive | 0.069 ± 0.009 | 0.061 ± 0.007 | 0.060 ± 0.002 | 0.086 |
| Obstructive | 0.246 ± 0.008 | 0.264 ± 0.009 | 0.267 ± 0.009 | 0.005 |
| 30 LPM | ||||
| Healthy | 0.740 ± 0.033 | 0.767 ± 0.029 | 0.773 ± 0.028 | 0.227 |
| Restrictive | 0.512 ± 0.016 | 0.525 ± 0.014 | 0.527 ± 0.011 | 0.240 |
| Obstructive | 0.790 ± 0.041 | 0.810 ± 0.032 | 0.814 ± 0.026 | 0.510 |
| 50 LPM | ||||
| Healthy | 1.785 ± 0.098 | 1.825 ± 0.046 | 1.853 ± 0.041 | 0.308 |
| Restrictive | 1.279 ± 0.117 | 1.306 ± 0.078 | 1.322 ± 0.063 | 0.749 |
| Obstructive | 1.525 ± 0.091 | 1.552 ± 0.070 | 1.574 ± 0.058 | 0.593 |
| 3 LPM | ||||
|---|---|---|---|---|
| PEEP (cm H2O) | ||||
| Lung Health | Pre-nebulisation | During | Post nebulisation | P-value |
| Healthy | 5.010 ± 0.067 | 5.032 ± 0.375 | 5.334 ± 0.085 | 0.075 |
| Restrictive | 0.899 ± 0.045 | 0.923 ± 0.061 | 0.935 ± 0.052 | 0.565 |
| Obstructive | 5.345 ± 0.290 | 5.620 ± 0.294 | 5.579 ± 0.289 | 0.308 |
| 7 LPM | ||||
| Healthy | 8.710 ± 1.177 | 9.137 ± 1.590 | 9.073 ± 1.649 | 0.888 |
| Restrictive | 3.841 ± 0.431 | 4.056 ± 0.296 | 4.089 ± 0.244 | 0.464 |
| Obstructive | 10.254 ± 0.371 | 10.528 ± 0.108 | 10.661 ± 0.259 | 0.089 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mac Giolla Eain, M.; MacLoughlin, R. In-Line Aerosol Therapy via Nasal Cannula during Adult and Paediatric Normal, Obstructive, and Restrictive Breathing. Pharmaceutics 2023, 15, 2679. https://doi.org/10.3390/pharmaceutics15122679
Mac Giolla Eain M, MacLoughlin R. In-Line Aerosol Therapy via Nasal Cannula during Adult and Paediatric Normal, Obstructive, and Restrictive Breathing. Pharmaceutics. 2023; 15(12):2679. https://doi.org/10.3390/pharmaceutics15122679
Chicago/Turabian StyleMac Giolla Eain, Marc, and Ronan MacLoughlin. 2023. "In-Line Aerosol Therapy via Nasal Cannula during Adult and Paediatric Normal, Obstructive, and Restrictive Breathing" Pharmaceutics 15, no. 12: 2679. https://doi.org/10.3390/pharmaceutics15122679
APA StyleMac Giolla Eain, M., & MacLoughlin, R. (2023). In-Line Aerosol Therapy via Nasal Cannula during Adult and Paediatric Normal, Obstructive, and Restrictive Breathing. Pharmaceutics, 15(12), 2679. https://doi.org/10.3390/pharmaceutics15122679








