Research Progress Concerning a Novel Intraocular Lens for the Prevention of Posterior Capsular Opacification
Abstract
:1. Introduction
1.1. Pathophysiology of PCO
1.2. The Role of IOLs in PCO Prevention
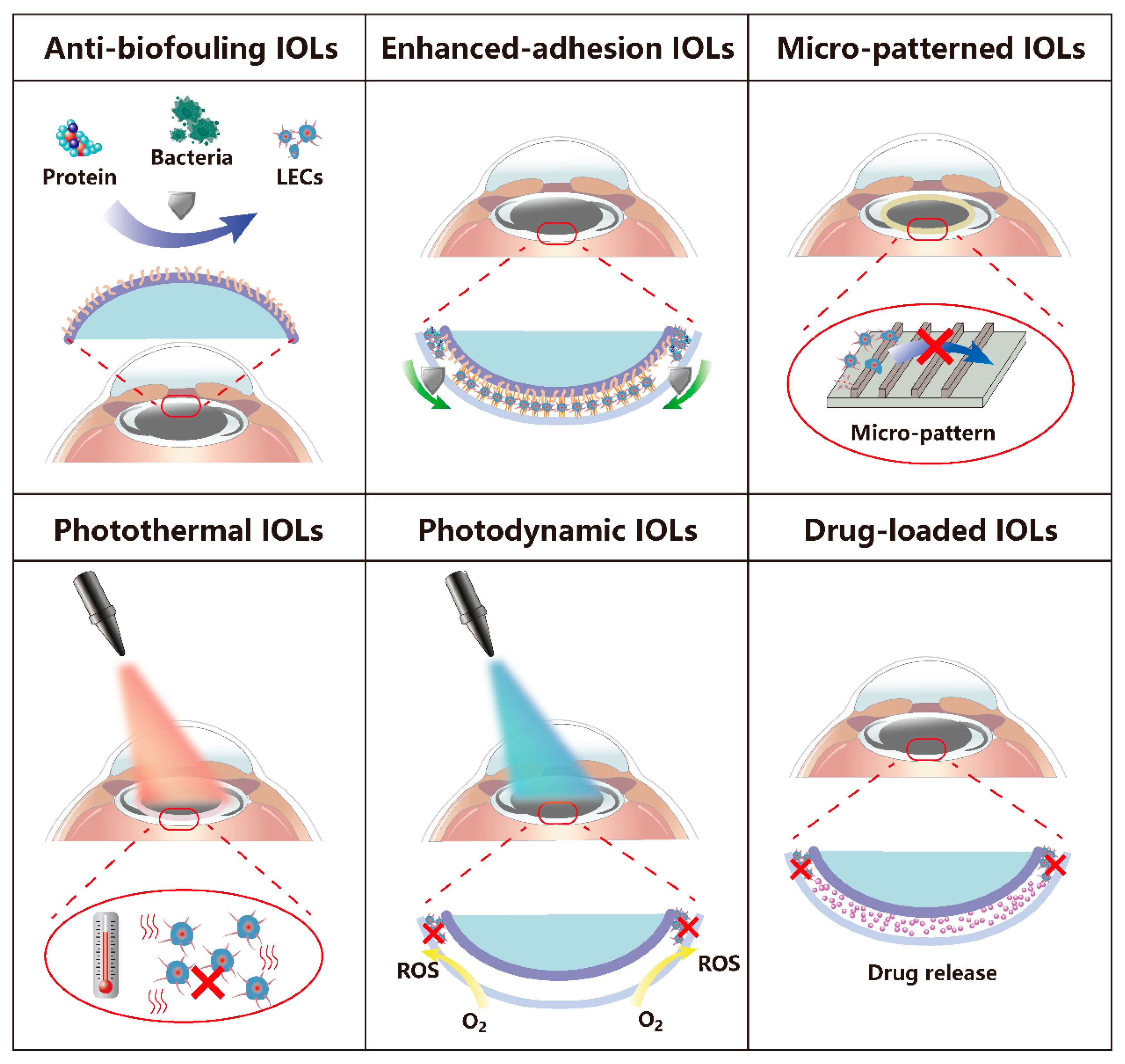
2. The Main Types of IOLs Used for PCO Prophylaxis
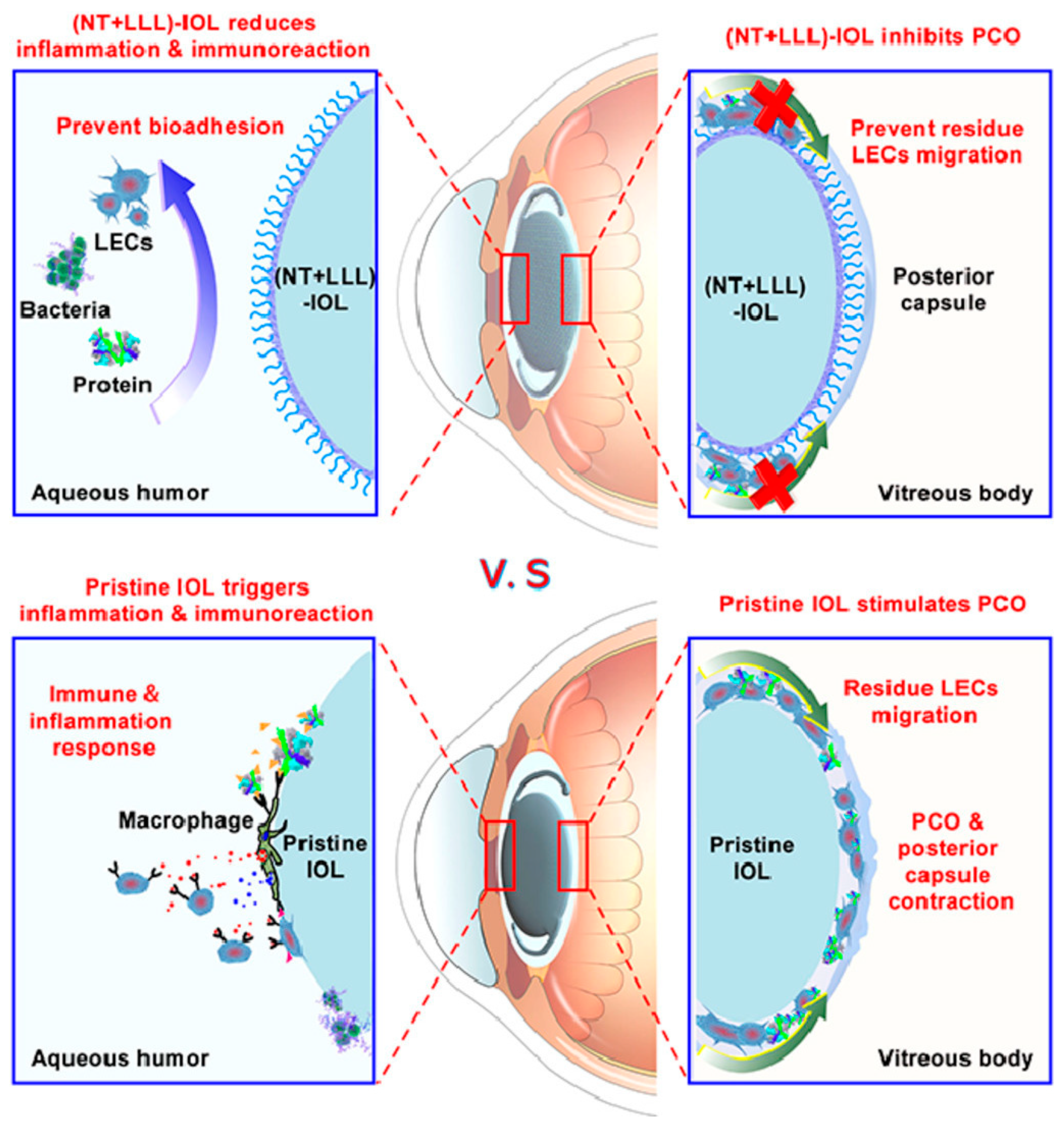
2.1. Anti-Biofouling IOLs
| Composition | Main Fabrication Method | IOL Type | Observation | Prophylaxis Effect | Ref. |
|---|---|---|---|---|---|
| PEG | oxygen plasma-aided activation and grafting polymerization | acrylic IOL (SA60AT, Alcon) | eight weeks in rabbit model | alleviate PCO formation for six weeks, but had no effect afterwards | [31] |
| PPEGMA | oxygen and argon plasma-aided activation and grafting polymerization | acrylic IOL (SN60WF, Alcon) | four months in rabbit model | alleviate PCO formation | [32] |
| PPEGMA | oxygen plasma-aided activation and RAFT grafting polymerization | acrylic IOL (SN60WF, Alcon) | six months in rabbit model | alleviate PCO formation | [17] |
| MPC | RAFT grafting polymerization | acrylic IOL (SN60WF, Alcon) | one month in rabbit model | alleviate PCO formation | [37] |
| MPC/MAA | ammonia plasma-aided activation and grafting polymerization | acrylic IOL (Eyegood Medical Tech.) | eight weeks in rabbit model | alleviate anterior capsular opacification formation, but did not alleviate PCO formation | [38] |
| PSBMA | RAFT grafting polymerization | acrylic IOL (66Vision Tech.) | six months in rabbit model | alleviate PCO formation | [39] |
| HA/CHI | layer-by-layer assembly | acrylic IOL (Alcon) | one month in rabbit model | alleviate CPCO formation not PPCO | [42] |
| PDMS | oxygen plasma-aided activation and chemical vapor deposition | acrylic IOL (Eyebright Medical Tech.) | two months in rabbit model | alleviate PCO formation | [43] |
2.2. Enhanced-Adhesion IOLs
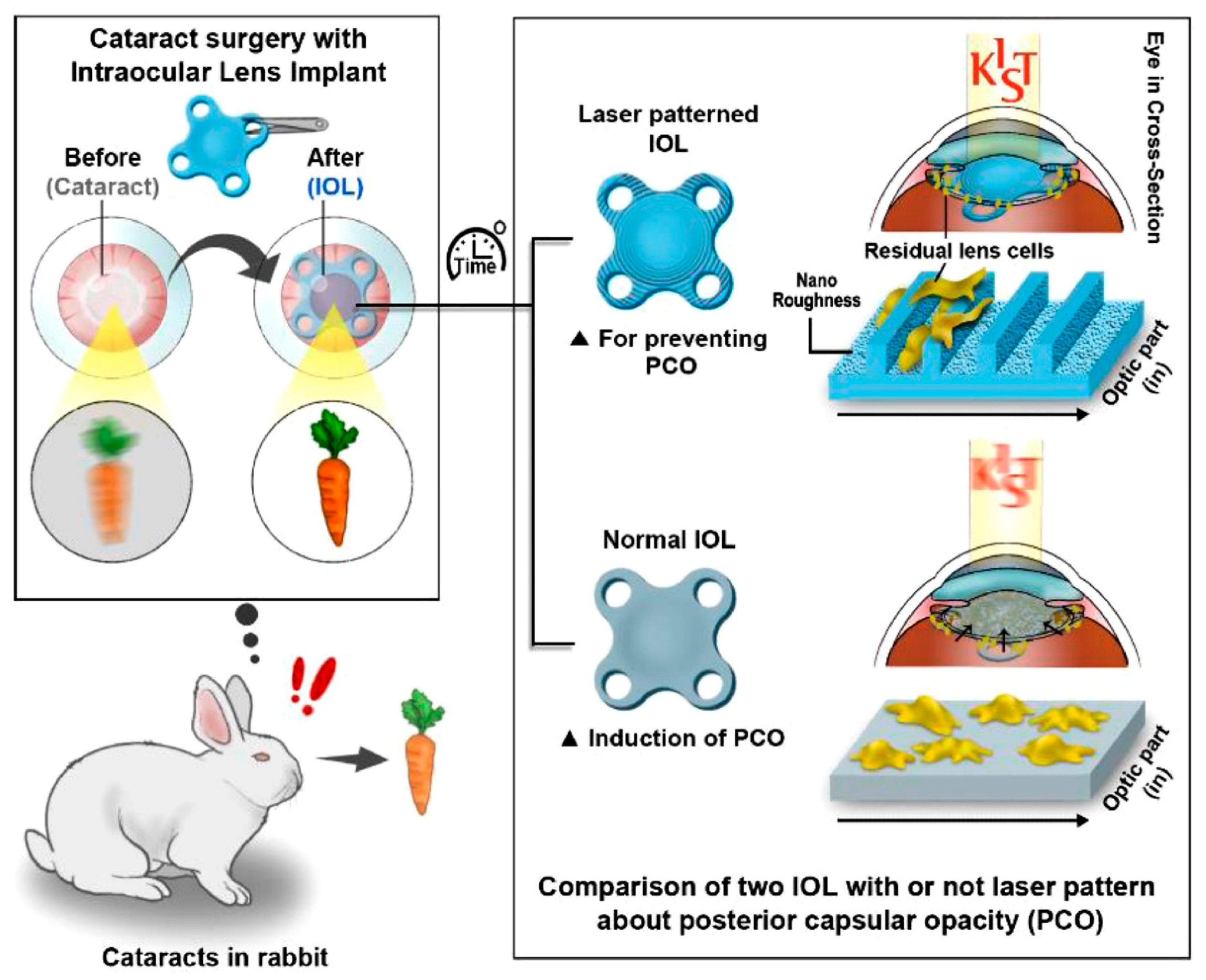
2.3. Micro-Patterned IOLs
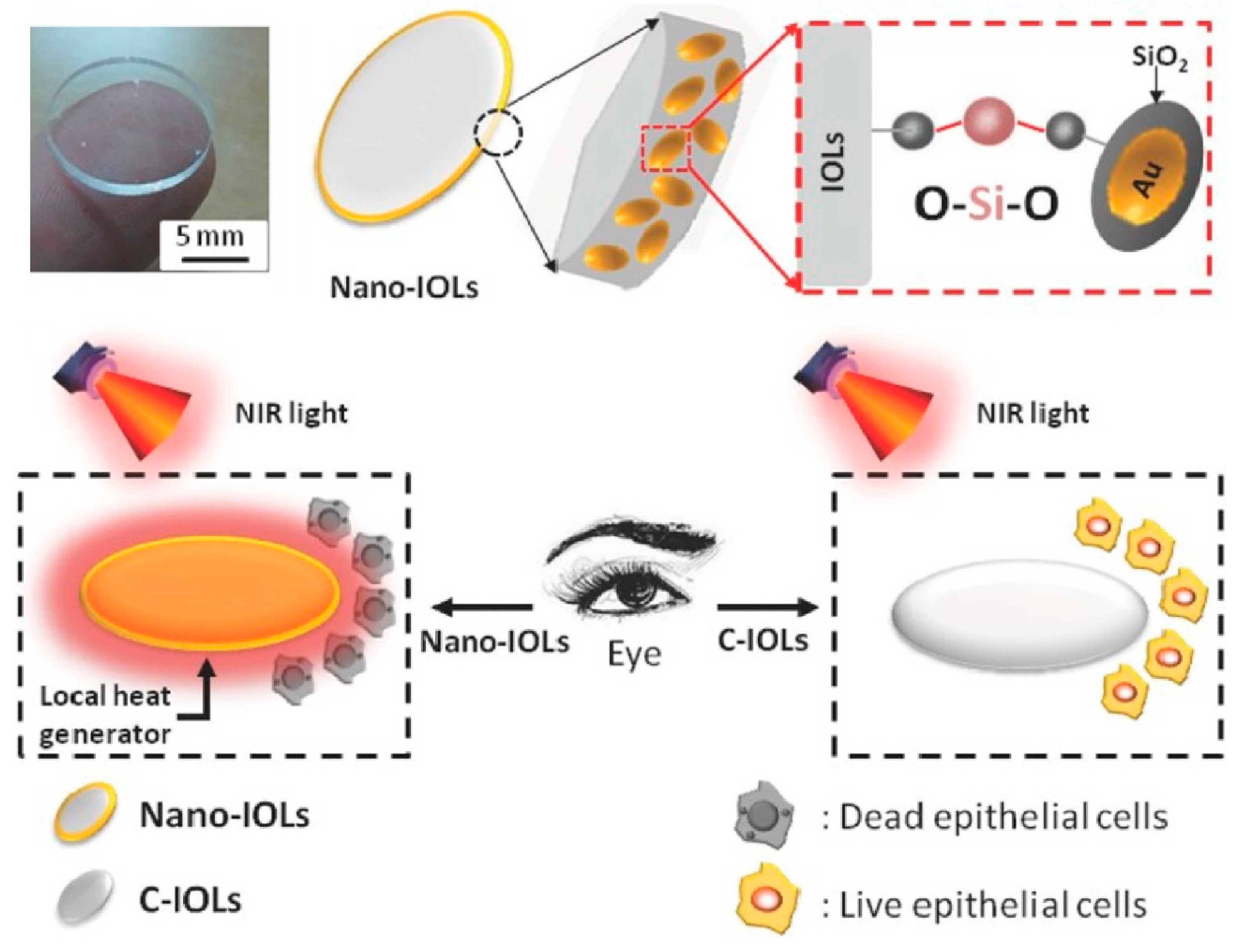
2.4. Photothermal IOLs
| Composition | Mechanism | Main Fabrication Method | IOL Type | Observation | Irradiation Protocol In Vivo | Ref. |
|---|---|---|---|---|---|---|
| Au nanorods/SiO2 | PTT | oxygen plasma-aided activation and immersion | commercial acrylic IOL | thirty days in rabbit model | 808 nm, 3.3 W/cm2, 10 min; once a week | [76] |
| PDA/PEI | PTT | CuSO4/H2O2-triggered rapid deposition | acrylic IOL (66Vision Tech.) | four weeks in rabbit model | 808 nm, 0.3 W/cm2, 10 min; at day 1, 3, 5, 7, 14, 21, and 28 | [78] |
| rGO/PEI | PTT | plasma-aided activation and layer-by-layer self-assembly | acrylic IOL (66Vision Tech.) | four weeks in rabbit model | 808 nm, 2.5 W/cm2, 10 min; three times in the first week, twice in the second week, and once a week in subsequent weeks | [84] |
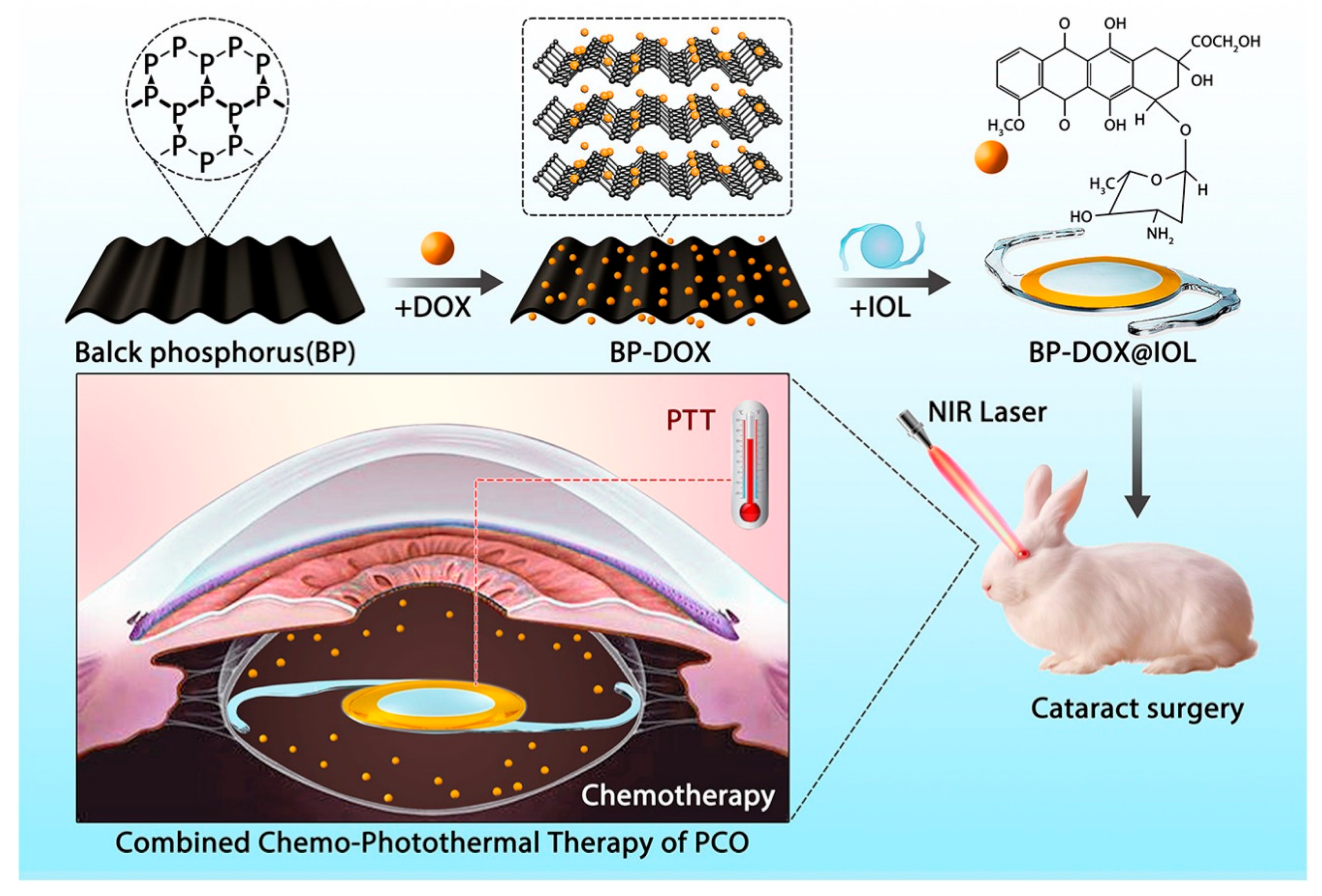
| BP/DOX | PTT and chemotherapy | facial activation and immersion | acrylic IOL (Eyebright Medical Tech.) | four weeks in rabbit model | 808 nm, 1 W/cm2, 3 min; once a week from the second week | [85] |
| ICG/PLGA | PDT | facial activation, electrostatic attraction and immersion | commercial IOL | eight weeks in rabbit model | 785 nm, 120 mW/cm2, 10 min; every day for one month | [86] |
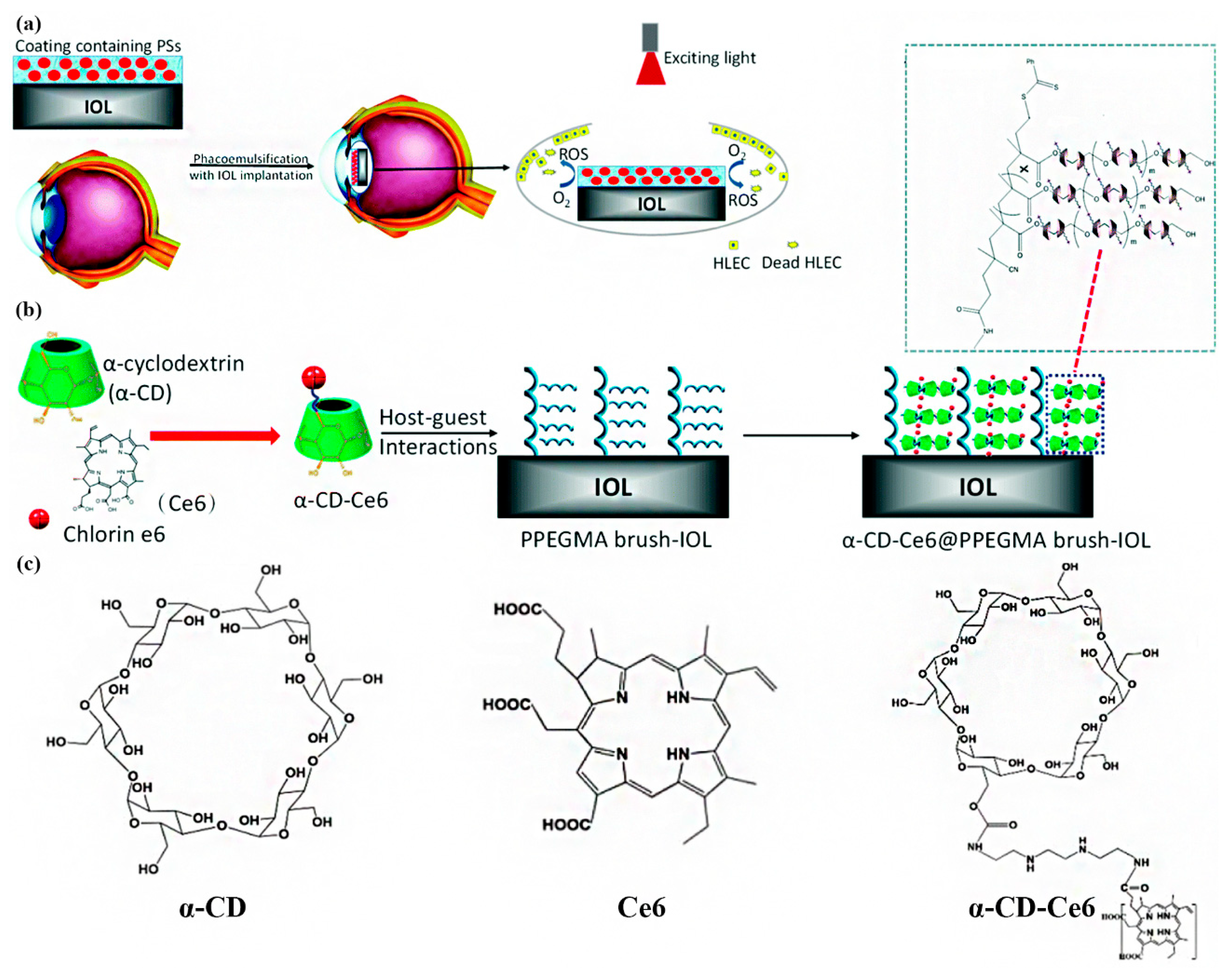
| α-CD-Ce-6/PPEGMA | PDT | RAFT technology and supramolecular self-assembly | acrylic IOL (66Vision Tech.) | two months in rabbit model | 660 nm, 2.4 W/cm2, 2 min; once a day in the first week | [87] |
| Ce-6/PDA | PDT | self-polymerization | acrylic IOL (66Vision Tech.) | four weeks in rabbit model | 660 nm, 2.4 W/cm2, 2 min; once a day for two weeks | [88] |
2.5. Photodynamic IOLs
2.6. Drug-Loaded IOLs
| Drug | Other Composition | Mechanism | Main Loading Method | Loading Dosage | IOL Type | Observation | Ref. |
|---|---|---|---|---|---|---|---|
| CXB | none | not verified in the article | immersion | unclear | acrylic IOL | 56 weeks in dog model | [95] |
| BF | PLGA | inhibit cell migration and TGF-β2-induced EMT | ultrasonic spray technique | ≈100 μg/IOL of BF | acrylic IOL (Wuxi Vision PRO) | four weeks in rabbit model | [96] |
| 5-FU | CHI | inhibit cell proliferation and promote cell apoptosis | fluorine ion beam-aided activation and immersion | ≈19.55 ± 1.31 mg/IOL of 5-FU | PMMA IOL (CJ55, Rafi Systems) | four weeks in rabbit model | [97] |
| DOX | CHI/TPP/HEP | inhibit cell adhesion, proliferation, and migration | ionic gelation, surficial activation, and layer-by-layer self-assembly | unclear | acrylic IOL (66Vision Tech.) | two months in rabbit model | [98] |
| DOX | PDA/MPC | inhibit cell adhesion, proliferation | self-polymerization and immersion | ≈2.8 μg/IOL of DOX | acrylic IOL (66Vision Tech.) | six weeks in rabbit model | [99] |
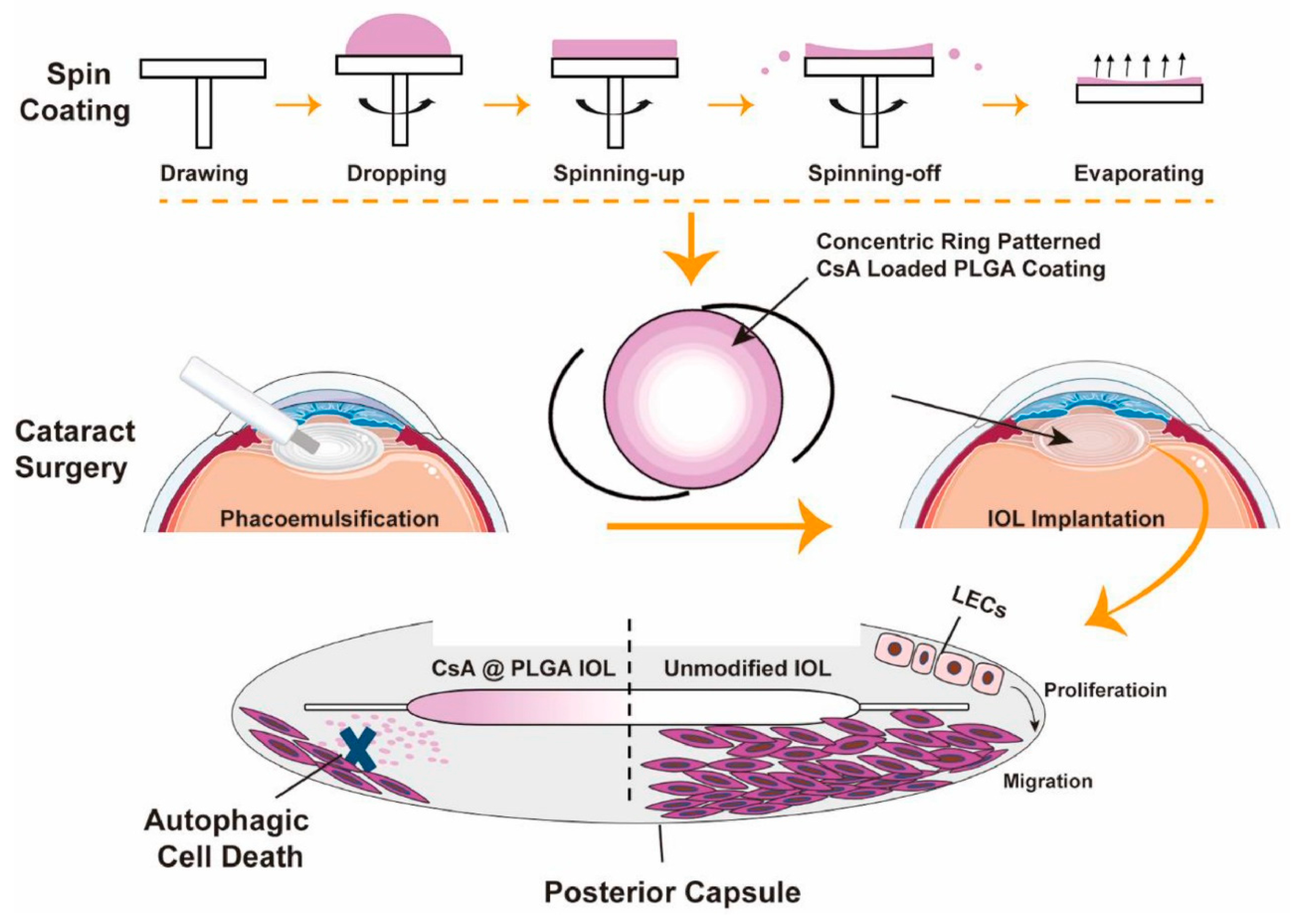
| CsA | PLGA | inhibit cell proliferation and promote autophagy-mediated cell death | spin-coating technique | unclear | acrylic IOL (66Vision Tech.) | four weeks in rabbit model | [104] |
| RAPA | PLGA | not verified in the article | proprietary spray technique | unclear | PMMA IOL (Suzhou Medical Instrument) | three months in rabbit model | [105] |
3. Biosecurity of IOLs in PCO Prophylaxis
4. Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liu, Y.; Wilkins, M.; Kim, T.; Malyugin, B.; Mehta, J.S. Cataracts. Lancet 2017, 390, 600–612. [Google Scholar] [CrossRef]
- Chen, X.; Xu, J.; Chen, X.; Yao, K. Cataract: Advances in Surgery and Whether Surgery Remains the Only Treatment in Future. Adv. Ophthalmol. Pract. Res. 2021, 1, 100008. [Google Scholar] [CrossRef]
- Allen, D.; Vasavada, A. Cataract and Surgery for Cataract. BMJ 2006, 333, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Wormstone, I.M.; Wang, L.; Liu, C.S.C. Posterior Capsule Opacification. Exp. Eye Res. 2009, 88, 257–269. [Google Scholar] [CrossRef]
- Nibourg, L.M.; Gelens, E.; Kuijer, R.; Hooymans, J.M.M.; van Kooten, T.G.; Koopmans, S.A. Prevention of Posterior Capsular Opacification. Exp. Eye Res. 2015, 136, 100–115. [Google Scholar] [CrossRef]
- Medsinge, A.; Nischal, K.K. Pediatric Cataract: Challenges and Future Directions. Clin. Ophthalmol. 2015, 9, 77–90. [Google Scholar] [CrossRef] [Green Version]
- Karahan, E.; Er, D.; Kaynak, S. An Overview of Nd:YAG Laser Capsulotomy. Med. Hypothesis Discov. Innov. Ophthalmol. 2014, 3, 45–50. [Google Scholar]
- Steinert, R.F.; Puliafito, C.A.; Kumar, S.R.; Dudak, S.D.; Patel, S. Cystoid Macular Edema, Retinal Detachment, and Glaucoma after Nd:YAG Laser Posterior Capsulotomy. Am. J. Ophthalmol. 1991, 112, 373–380. [Google Scholar] [CrossRef]
- Wesolosky, J.D.; Tennant, M.; Rudnisky, C.J. Rate of Retinal Tear and Detachment after Neodymium:YAG Capsulotomy. J. Cataract Refract. Surg 2017, 43, 923–928. [Google Scholar] [CrossRef]
- Thompson, J.; Lakhani, N. Cataracts. Prim. Care Clin. Off. Pract. 2015, 42, 409–423. [Google Scholar] [CrossRef]
- Wormstone, I.M.; Wormstone, Y.M.; Smith, A.J.O.; Eldred, J.A. Posterior Capsule Opacification: What’s in the Bag? Prog. Retin. Eye Res. 2021, 82, 100905. [Google Scholar] [CrossRef]
- Amon, M. Biocompatibility of Intraocular Lenses. J. Cataract Refract. Surg. 2001, 27, 178–179. [Google Scholar] [CrossRef]
- Saika, S. Relationship between Posterior Capsule Opacification and Intraocular Lens Biocompatibility. Prog. Retin. Eye Res. 2004, 23, 283–305. [Google Scholar] [CrossRef]
- Özyol, P.; Özyol, E.; Karel, F. Biocompatibility of Intraocular Lenses. Turk. J. Ophthalmol. 2017, 47, 221–225. [Google Scholar] [CrossRef]
- Krall, E.M.; Arlt, E.M.; Jell, G.; Strohmaier, C.; Moussa, S.; Dexl, A.K. Prospective Randomized Intraindividual Comparison of Posterior Capsule Opacification after Implantation of an IOL with and without Heparin Surface Modification. J. Refract. Surg. 2015, 31, 466–472. [Google Scholar] [CrossRef]
- Bozukova, D.; Pagnoulle, C.; De Pauw-Gillet, M.-C.; Desbief, S.; Lazzaroni, R.; Ruth, N.; Jérôme, R.; Jérôme, C. Improved Performances of Intraocular Lenses by Poly(Ethylene Glycol) Chemical Coatings. Biomacromolecules 2007, 8, 2379–2387. [Google Scholar] [CrossRef]
- Lin, Q.; Tang, J.; Han, Y.; Xu, X.; Hao, X.; Chen, H. Hydrophilic Modification of Intraocular Lens via Surface Initiated Reversible Addition-Fragmentation Chain Transfer Polymerization for Reduced Posterior Capsular Opacification. Colloids Surf. B Biointerfaces 2017, 151, 271–279. [Google Scholar] [CrossRef]
- Lan, X.; Lei, Y.; He, Z.; Yin, A.; Li, L.; Tang, Z.; Li, M.; Wang, Y. A Transparent Hydrophilic Anti-Biofouling Coating for Intraocular Lens Materials Prepared by “Bridging” of the Intermediate Adhesive Layer. J. Mater. Chem. B 2021, 9, 3696–3704. [Google Scholar] [CrossRef]
- Barbour, W.; Saika, S.; Miyamoto, T.; Ohnishi, Y. Biological Compatibility of Polymethyl Methacrylate, Hydrophilic Acrylic and Hydrophobic Acrylic Intraocular Lenses. Ophthalmic Res. 2005, 37, 255–261. [Google Scholar] [CrossRef]
- Lewis, A.C. Interleukin-6 in the Pathogenesis of Posterior Capsule Opacification and the Potential Role for Interleukin-6 Inhibition in the Future of Cataract Surgery. Med. Hypotheses 2013, 80, 466–474. [Google Scholar] [CrossRef]
- Huang, Q.; Cheng, G.P.-M.; Chiu, K.; Wang, G. Surface Modification of Intraocular Lenses. Chin. Med. J. 2016, 129, 206–214. [Google Scholar] [CrossRef] [Green Version]
- Topete, A.; Saramago, B.; Serro, A.P. Intraocular Lenses as Drug Delivery Devices. Int. J. Pharm. 2021, 602, 120613. [Google Scholar] [CrossRef]
- Zhang, R.; Xie, Z. Research Progress of Drug Prophylaxis for Lens Capsule Opacification after Cataract Surgery. J. Ophthalmol. 2020, 2020, 2181685. [Google Scholar] [CrossRef]
- Mylona, I.; Tsinopoulos, I. A Critical Appraisal of New Developments in Intraocular Lens Modifications and Drug Delivery Systems for the Prevention of Cataract Surgery Complications. Pharmaceuticals 2020, 13, 448. [Google Scholar] [CrossRef]
- Cooksley, G.; Lacey, J.; Dymond, M.K.; Sandeman, S. Factors Affecting Posterior Capsule Opacification in the Development of Intraocular Lens Materials. Pharmaceutics 2021, 13, 860. [Google Scholar] [CrossRef]
- Sanchez-Cano, C.; Carril, M. Recent Developments in the Design of Non-Biofouling Coatings for Nanoparticles and Surfaces. Int. J. Mol. Sci. 2020, 21, 1007. [Google Scholar] [CrossRef] [Green Version]
- Leslie, D.C.; Waterhouse, A.; Berthet, J.B.; Valentin, T.M.; Watters, A.L.; Jain, A.; Kim, P.; Hatton, B.D.; Nedder, A.; Donovan, K.; et al. A Bioinspired Omniphobic Surface Coating on Medical Devices Prevents Thrombosis and Biofouling. Nat. Biotechnol. 2014, 32, 1134–1140. [Google Scholar] [CrossRef]
- He, Z.; Yang, X.; Wang, N.; Mu, L.; Pan, J.; Lan, X.; Li, H.; Deng, F. Anti-Biofouling Polymers with Special Surface Wettability for Biomedical Applications. Front. Bioeng. Biotechnol. 2021, 9, 807357. [Google Scholar] [CrossRef]
- Chan, H.-M.; Erathodiyil, N.; Wu, H.; Lu, H.; Zheng, Y.; Ying, J.Y. Calcium Cross-Linked Zwitterionic Hydrogels as Antifouling Materials. Mater. Today Commun. 2020, 23, 100950. [Google Scholar] [CrossRef]
- Kang, S.; Choi, J.A.; Joo, C.-K. Comparison of Posterior Capsular Opacification in Heparin-Surface-Modified Hydrophilic Acrylic and Hydrophobic Acrylic Intraocular Lenses. Jpn. J. Ophthalmol. 2009, 53, 204–208. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.I.; Kim, M.K.; Ko, J.H.; Lee, H.J.; Wee, W.R.; Lee, J.H. The Efficacy of an Acrylic Intraocular Lens Surface Modified with Polyethylene Glycol in Posterior Capsular Opacification. J. Korean Med. Sci. 2007, 22, 502. [Google Scholar] [CrossRef] [Green Version]
- Xu, X.; Tang, J.; Han, Y.; Wang, W.; Chen, H.; Lin, Q. Surface PEGylation of Intraocular Lens for PCO Prevention: An In Vivo Evaluation. J. Biomater. Appl. 2016, 31, 68–76. [Google Scholar] [CrossRef]
- Monge, S.; Canniccioni, B.; Graillot, A.; Robin, J.-J. Phosphorus-Containing Polymers: A Great Opportunity for the Biomedical Field. Biomacromolecules 2011, 12, 1973–1982. [Google Scholar] [CrossRef]
- Shigeta, M.; Tanaka, T.; Koike, N.; Yamakawa, N.; Usui, M. Suppression of Fibroblast and Bacterial Adhesion by MPC Coating on Acrylic Intraocular Lenses. J. Cataract Refract. Surg. 2006, 32, 859–866. [Google Scholar] [CrossRef]
- Huang, X.; Yao, K.; Zhang, Z.; Zhang, Y.; Wang, Y. Uveal and Capsular Biocompatibility of an Intraocular Lens with a Hydrophilic Anterior Surface and a Hydrophobic Posterior Surface. J. Cataract Refract. Surg. 2010, 36, 290–298. [Google Scholar] [CrossRef]
- Huang, X.; Li, H.; Lin, L.; Yao, K. Reduced Silicone Oil Adherence to Silicone Intraocular Lens by Surface Modification with 2-Methacryloyloxyethyl Phosphoryl-Choline. Curr. Eye Res. 2013, 38, 91–96. [Google Scholar] [CrossRef]
- Han, Y.; Xu, X.; Tang, J.; Shen, C.; Lin, Q.; Chen, H. Bottom-up Fabrication of Zwitterionic Polymer Brushes on Intraocular Lens for Improved Biocompatibility. Int. J. Nanomed. 2016, 12, 127–135. [Google Scholar] [CrossRef] [Green Version]
- Tan, X.; Zhan, J.; Zhu, Y.; Cao, J.; Wang, L.; Liu, S.; Wang, Y.; Liu, Z.; Qin, Y.; Wu, M.; et al. Improvement of Uveal and Capsular Biocompatibility of Hydrophobic Acrylic Intraocular Lens by Surface Grafting with 2-Methacryloyloxyethyl Phosphorylcholine-Methacrylic Acid Copolymer. Sci. Rep. 2017, 7, 40462. [Google Scholar] [CrossRef] [Green Version]
- Wang, R.; Xia, J.; Tang, J.; Liu, D.; Zhu, S.; Wen, S.; Lin, Q. Surface Modification of Intraocular Lens with Hydrophilic Poly(Sulfobetaine Methacrylate) Brush for Posterior Capsular Opacification Prevention. J. Ocul. Pharmacol. Ther. 2021, 37, 172–180. [Google Scholar] [CrossRef]
- Necas, J.; Bartosikova, L.; Brauner, P.; Kolar, J. Hyaluronic Acid (Hyaluronan): A Review. Vet. Med. 2008, 53, 397–411. [Google Scholar] [CrossRef] [Green Version]
- Ravi Kumar, M.N.V. A Review of Chitin and Chitosan Applications. React. Funct. Polym. 2000, 46, 1–27. [Google Scholar] [CrossRef]
- Lin, Q.; Xu, X.; Wang, B.; Shen, C.; Tang, J.; Han, Y.; Chen, H. Hydrated Polysaccharide Multilayer as an Intraocular Lens Surface Coating for Biocompatibility Improvements. J. Mater. Chem. B 2015, 3, 3695–3703. [Google Scholar] [CrossRef]
- Wu, Q.; Liu, D.; Chen, W.; Chen, H.; Yang, C.; Li, X.; Yang, C.; Lin, H.; Chen, S.; Hu, N.; et al. Liquid-like Layer Coated Intraocular Lens for Posterior Capsular Opacification Prevention. Appl. Mater. Today 2021, 23, 100981. [Google Scholar] [CrossRef]
- Linnola, R.J.; Holst, A. Evaluation of a 3-Piece Silicone Intraocular Lens with Poly(Methyl Methacrylate) Haptics. J. Cataract Refract. Surg. 1998, 24, 1509–1514. [Google Scholar] [CrossRef]
- Linnola, R.J.; Werner, L.; Pandey, S.K.; Escobar-Gomez, M.; Znoiko, S.L.; Apple, D.J. Adhesion of Fibronectin, Vitronectin, Laminin, and Collagen Type IV to Intraocular Lens Materials in Pseudophakic Human Autopsy Eyes. Part 2: Explanted Intraocular Lenses. J. Cataract Refract. Surg. 2000, 26, 1807–1818. [Google Scholar] [CrossRef]
- Linnola, R.J.; Werner, L.; Pandey, S.K.; Escobar-Gomez, M.; Znoiko, S.L.; Apple, D.J. Adhesion of Fibronectin, Vitronectin, Laminin, and Collagen Type IV to Intraocular Lens Materials in Pseudophakic Human Autopsy Eyes. Part 1: Histological Sections. J. Cataract Refract. Surg. 2000, 26, 1792–1806. [Google Scholar] [CrossRef]
- Linnola, R.J. Sandwich Theory: Bioactivity-Based Explanation for Posterior Capsule Opacification. J. Cataract Refract. Surg. 1997, 23, 1539–1542. [Google Scholar] [CrossRef]
- Heatley, C.J.; Spalton, D.J.; Kumar, A.; Jose, R.; Boyce, J.; Bender, L.E. Comparison of Posterior Capsule Opacification Rates between Hydrophilic and Hydrophobic Single-Piece Acrylic Intraocular Lenses. J. Cataract Refract. Surg. 2005, 31, 718–724. [Google Scholar] [CrossRef]
- Bertrand, V.; Bozukova, D.; Svaldo Lanero, T.; Huang, Y.-S.; Schol, D.; Rosière, N.; Grauwels, M.; Duwez, A.-S.; Jérôme, C.; Pagnoulle, C.; et al. Biointerface Multiparametric Study of Intraocular Lens Acrylic Materials. J. Cataract Refract. Surg. 2014, 40, 1536–1544. [Google Scholar] [CrossRef]
- Katayama, Y.; Kobayakawa, S.; Yanagawa, H.; Tochikubo, T. The Relationship between the Adhesion Characteristics of Acrylic Intraocular Lens Materials and Posterior Capsule Opacification. Ophthalmic Res. 2007, 39, 276–281. [Google Scholar] [CrossRef]
- Jaitli, A.; Roy, J.; Chatila, A.; Liao, J.; Tang, L. Role of Fibronectin and IOL Surface Modification in IOL: Lens Capsule Interactions. Exp. Eye Res. 2022, 221, 109135. [Google Scholar] [CrossRef]
- Arita, T.; Lin, L.R.; Susan, S.R.; Reddy, V.N. Enhancement of Differentiation of Human Lens Epithelium in Tissue Culture by Changes in Cell-Substrate Adhesion. Investig. Ophthalmol. Vis. Sci. 1990, 31, 2395–2404. [Google Scholar]
- Matsushima, H.; Iwamoto, H.; Mukai, K.; Obara, Y. Active Oxygen Processing for Acrylic Intraocular Lenses to Prevent Posterior Capsule Opacification. J. Cataract Refract. Surg. 2006, 32, 1035–1040. [Google Scholar] [CrossRef]
- Nakanishi, J.; Kikuchi, Y.; Takarada, T.; Nakayama, H.; Yamaguchi, K.; Maeda, M. Photoactivation of a Substrate for Cell Adhesion under Standard Fluorescence Microscopes. J. Am. Chem. Soc. 2004, 126, 16314–16315. [Google Scholar] [CrossRef]
- Farukhi, A.M.; Werner, L.; Kohl, J.C.; Gardiner, G.L.; Ford, J.R.; Cole, S.C.; Vasavada, S.A.; Noristani, R.; Mamalis, N. Evaluation of Uveal and Capsule Biocompatibility of a Single-Piece Hydrophobic Acrylic Intraocular Lens with Ultraviolet–Ozone Treatment on the Posterior Surface. J. Cataract Refract. Surg. 2015, 41, 1081–1087. [Google Scholar] [CrossRef]
- Ruoslahti, E.; Pierschbacher, M.D. New Perspectives in Cell Adhesion: RGD and Integrins. Science 1987, 238, 491–497. [Google Scholar] [CrossRef]
- Danhier, F.; Le Breton, A.; Préat, V. RGD-Based Strategies to Target Alpha(v) Beta(3) Integrin in Cancer Therapy and Diagnosis. Mol. Pharm. 2012, 9, 2961–2973. [Google Scholar] [CrossRef]
- Huang, Y.-S.; Bertrand, V.; Bozukova, D.; Pagnoulle, C.; Labrugère, C.; De Pauw, E.; De Pauw-Gillet, M.-C.; Durrieu, M.-C. RGD Surface Functionalization of the Hydrophilic Acrylic Intraocular Lens Material to Control Posterior Capsular Opacification. PLoS ONE 2014, 9, e114973. [Google Scholar] [CrossRef] [Green Version]
- Ruoslahti, E. RGD and Other Recognition Sequences for Integrins. Annu. Rev. Cell. Dev. Biol. 1996, 12, 697–715. [Google Scholar] [CrossRef]
- Nishi, O.; Nishi, K.; Wickström, K. Preventing Lens Epithelial Cell Migration Using Intraocular Lenses with Sharp Rectangular Edges. J. Cataract Refract. Surg. 2000, 26, 1543–1549. [Google Scholar] [CrossRef]
- Cheng, J.; Wei, R.; Cai, J.; Xi, G.; Zhu, H.; Li, Y.; Ma, X. Efficacy of Different Intraocular Lens Materials and Optic Edge Designs in Preventing Posterior Capsular Opacification: A Meta-Analysis. Am. J. Ophthalmol. 2007, 143, 428–436. [Google Scholar] [CrossRef]
- Kohnen, T.; Fabian, E.; Gerl, R.; Hunold, W.; Hütz, W.; Strobel, J.; Hoyer, H.; Mester, U. Optic Edge Design as Long-Term Factor for Posterior Capsular Opacification Rates. Ophthalmology 2008, 115, 1308–1313, 1314.e1–3. [Google Scholar] [CrossRef]
- McHugh, K.J.; Saint-Geniez, M.; Tao, S.L. Topographical Control of Ocular Cell Types for Tissue Engineering: Topographical Control of Ocular Cell Types. J. Biomed. Mater. Res. 2013, 101, 1571–1584. [Google Scholar] [CrossRef] [Green Version]
- Xia, N.; Thodeti, C.K.; Hunt, T.P.; Xu, Q.; Ho, M.; Whitesides, G.M.; Westervelt, R.; Ingber, D.E. Directional Control of Cell Motility through Focal Adhesion Positioning and Spatial Control of Rac Activation. FASEB J. 2008, 22, 1649–1659. [Google Scholar] [CrossRef] [Green Version]
- Magin, C.M.; May, R.M.; Drinker, M.C.; Cuevas, K.H.; Brennan, A.B.; Reddy, S.T. Micropatterned Protective Membranes Inhibit Lens Epithelial Cell Migration in Posterior Capsule Opacification Model. Trans. Vis. Sci. Technol. 2015, 4, 9. [Google Scholar] [CrossRef] [Green Version]
- Kramer, G.D.; Werner, L.; MacLean, K.; Farukhi, A.; Gardiner, G.L.; Mamalis, N. Evaluation of Stability and Capsular Bag Opacification with a Foldable Intraocular Lens Coupled with a Protective Membrane in the Rabbit Model. J. Cataract Refract. Surg. 2015, 41, 1738–1744. [Google Scholar] [CrossRef]
- Ellis, N.; Werner, L.; Balendiran, V.; Shumway, C.; Jiang, B.; Mamalis, N. Posterior Capsule Opacification Prevention by an Intraocular Lens Incorporating a Micropatterned Membrane on the Posterior Surface. J. Cataract Refract. Surg. 2020, 46, 6. [Google Scholar] [CrossRef]
- Ranella, A.; Barberoglou, M.; Bakogianni, S.; Fotakis, C.; Stratakis, E. Tuning Cell Adhesion by Controlling the Roughness and Wettability of 3D Micro/Nano Silicon Structures. Acta Biomater. 2010, 6, 2711–2720. [Google Scholar] [CrossRef]
- Lee, B.L.-P.; Jeon, H.; Wang, A.; Yan, Z.; Yu, J.; Grigoropoulos, C.; Li, S. Femtosecond Laser Ablation Enhances Cell Infiltration into Three-Dimensional Electrospun Scaffolds. Acta Biomater. 2012, 8, 2648–2658. [Google Scholar] [CrossRef] [Green Version]
- Jeon, H.; Koo, S.; Reese, W.M.; Loskill, P.; Grigoropoulos, C.P.; Healy, K.E. Directing Cell Migration and Organization via Nanocrater-Patterned Cell-Repellent Interfaces. Nat. Mater. 2015, 14, 918–923. [Google Scholar] [CrossRef] [Green Version]
- Simitzi, C.; Efstathopoulos, P.; Kourgiantaki, A.; Ranella, A.; Charalampopoulos, I.; Fotakis, C.; Athanassakis, I.; Stratakis, E.; Gravanis, A. Laser Fabricated Discontinuous Anisotropic Microconical Substrates as a New Model Scaffold to Control the Directionality of Neuronal Network Outgrowth. Biomaterials 2015, 67, 115–128. [Google Scholar] [CrossRef] [PubMed]
- Jun, I.; Chung, Y.-W.; Heo, Y.-H.; Han, H.-S.; Park, J.; Jeong, H.; Lee, H.; Lee, Y.B.; Kim, Y.-C.; Seok, H.-K.; et al. Creating Hierarchical Topographies on Fibrous Platforms Using Femtosecond Laser Ablation for Directing Myoblasts Behavior. ACS Appl. Mater. Interfaces 2016, 8, 3407–3417. [Google Scholar] [CrossRef] [PubMed]
- Seo, Y.; Kim, S.; Lee, H.S.; Park, J.; Lee, K.; Jun, I.; Seo, H.; Kim, Y.J.; Yoo, Y.; Choi, B.C.; et al. Femtosecond Laser Induced Nano-Textured Micropatterning to Regulate Cell Functions on Implanted Biomaterials. Acta Biomater. 2020, 116, 138–148. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhang, W.; Ji, W.; Wang, J.; Wang, N.; Wu, W.; Wu, Q.; Hou, X.; Hu, W.; Li, L. Near Infrared Photothermal Conversion Materials: Mechanism, Preparation, and Photothermal Cancer Therapy Applications. J. Mater. Chem. B 2021, 9, 7909–7926. [Google Scholar] [CrossRef]
- Ye, Y.; He, J.; Qiao, Y.; Qi, Y.; Zhang, H.; Santos, H.A.; Zhong, D.; Li, W.; Hua, S.; Wang, W.; et al. Mild Temperature Photothermal Assisted Anti-Bacterial and Anti-Inflammatory Nanosystem for Synergistic Treatment of Post-Cataract Surgery Endophthalmitis. Theranostics 2020, 10, 8541–8557. [Google Scholar] [CrossRef]
- Lin, Y.-X.; Hu, X.-F.; Zhao, Y.; Gao, Y.-J.; Yang, C.; Qiao, S.-L.; Wang, Y.; Yang, P.-P.; Yan, J.; Sui, X.-C.; et al. Photothermal Ring Integrated Intraocular Lens for High-Efficient Eye Disease Treatment-Supply. Adv. Mater. 2017, 29, 1701617. [Google Scholar] [CrossRef]
- Xu, J.; Yao, K.; Xu, Z. Nanomaterials with a Photothermal Effect for Antibacterial Activities: An Overview. Nanoscale 2019, 11, 8680–8691. [Google Scholar] [CrossRef]
- Xu, J.; Li, H.; Hu, D.; Zhang, X.; Wang, W.; Ji, J.; Xu, Z.; Yao, K. Intraocular Lens with Mussel-Inspired Coating for Preventing Posterior Capsule Opacification via Photothermal Effect. ACS Appl. Bio Mater. 2021, 4, 3579–3586. [Google Scholar] [CrossRef]
- Yang, K.; Feng, L.; Shi, X.; Liu, Z. Nano-Graphene in Biomedicine: Theranostic Applications. Chem. Soc. Rev. 2013, 42, 530–547. [Google Scholar] [CrossRef]
- Dash, B.S.; Jose, G.; Lu, Y.-J.; Chen, J.-P. Functionalized Reduced Graphene Oxide as a Versatile Tool for Cancer Therapy. Int. J. Mol. Sci. 2021, 22, 2989. [Google Scholar] [CrossRef]
- Robinson, J.T.; Tabakman, S.M.; Liang, Y.; Wang, H.; Casalongue, H.S.; Vinh, D.; Dai, H. Ultrasmall Reduced Graphene Oxide with High Near-Infrared Absorbance for Photothermal Therapy. J. Am. Chem. Soc. 2011, 133, 6825–6831. [Google Scholar] [CrossRef]
- An, W.; Zhang, Y.; Zhang, X.; Li, K.; Kang, Y.; Akhtar, S.; Sha, X.; Gao, L. Ocular Toxicity of Reduced Graphene Oxide or Graphene Oxide Exposure in Mouse Eyes. Exp. Eye Res. 2018, 174, 59–69. [Google Scholar] [CrossRef]
- Zhang, C.; Guo, Q.; Tong, Z.; Chen, S.; Mao, Z.; Yu, Y. Thin Film Nanoarchitectonics of Layer-by-Layer Assembly with Reduced Graphene Oxide on Intraocular Lens for Photothermal Therapy of Posterior Capsular Opacification. J. Colloid Interface Sci. 2022, 619, 348–358. [Google Scholar] [CrossRef]
- Mao, Y.; Yu, S.; Kang, Y.; Zhang, D.; Wu, S.; Zhang, J.; Xiong, Y.; Li, M.; Zhang, J.; Wang, J.; et al. CuInS/ZnS Quantum Dots Modified Intraocular Lens for Photothermal Therapy of Posterior Capsule Opacification. Exp. Eye Res. 2021, 202, 108282. [Google Scholar] [CrossRef]
- Mao, Y.; Li, M.; Wang, J.; Wang, K.; Zhang, J.; Chen, S.; Liu, X.; Liang, Q.; Gao, F.; Wan, X. NIR-Triggered Drug Delivery System for Chemo-Photothermal Therapy of Posterior Capsule Opacification. J. Control. Release 2021, 339, 391–402. [Google Scholar] [CrossRef]
- Zhang, Z.; Huang, W.; Lei, M.; He, Y.; Yan, M.; Zhang, X.; Zhao, C. Laser-Triggered Intraocular Implant to Induce Photodynamic Therapy for Posterior Capsule Opacification Prevention. Int. J. Pharm. 2016, 498, 1–11. [Google Scholar] [CrossRef]
- Tang, J.; Liu, S.; Han, Y.; Wang, R.; Xia, J.; Chen, H.; Lin, Q. Surface Modification of Intraocular Lenses via Photodynamic Coating for Safe and Effective PCO Prevention. J. Mater. Chem. B 2021, 9, 1546–1556. [Google Scholar] [CrossRef]
- Qie, J.; Wen, S.; Han, Y.; Liu, S.; Shen, L.; Chen, H.; Lin, Q. A Polydopamine-Based Photodynamic Coating on the Intraocular Lens Surface for Safer Posterior Capsule Opacification Conquering. Biomater. Sci. 2022, 10, 2188–2197. [Google Scholar] [CrossRef]
- Correia, J.H.; Rodrigues, J.A.; Pimenta, S.; Dong, T.; Yang, Z. Photodynamic Therapy Review: Principles, Photosensitizers, Applications, and Future Directions. Pharmaceutics 2021, 13, 1332. [Google Scholar] [CrossRef]
- Koh, H.J.; Kang, S.J.; Lim, S.J.; Chu, Y.K.; Lee, S.C.; Kwon, O.W.; Kim, H.B. The Effect of Photodynamic Therapy with Rose Bengal on Posterior Capsule Opacification in Rabbit Eyes. Ophthalmic Res. 2002, 34, 107–112. [Google Scholar] [CrossRef]
- Van Tenten, Y.; Schuitmaker, H.J.; De Groot, V.; Willekens, B.; Vrensen, G.F.J.M.; Tassignon, M.-J. A Preliminary Study on the Prevention of Posterior Capsule Opacification by Photodynamic Therapy with Bacteriochlorin A in Rabbits. Ophthalmic Res. 2002, 34, 113–118. [Google Scholar] [CrossRef]
- Jiang, J.; Shihan, M.H.; Wang, Y.; Duncan, M.K. Lens Epithelial Cells Initiate an Inflammatory Response Following Cataract Surgery. Investig. Ophthalmol. Vis. Sci. 2018, 59, 4986–4997. [Google Scholar] [CrossRef] [Green Version]
- Chandler, H.L.; Barden, C.A.; Lu, P.; Kusewitt, D.F.; Colitz, C.M.H. Prevention of Posterior Capsular Opacification through Cyclooxygenase-2 Inhibition. Mol. Vis. 2007, 13, 677–691. [Google Scholar]
- Davis, J.L.; Yi, N.Y.; Salmon, J.H.; Charlton, A.N.; Colitz, C.M.H.; Gilger, B.C. Sustained-Release Celecoxib from Incubated Acrylic Intraocular Lenses Suppresses Lens Epithelial Cell Growth in an Ex Vivo Model of Posterior Capsule Opacity. J. Ocul. Pharmacol. Ther. 2012, 28, 359–368. [Google Scholar] [CrossRef] [Green Version]
- Brookshire, H.L.; English, R.V.; Nadelstein, B.; Weigt, A.K.; Gift, B.W.; Gilger, B.C. Efficacy of COX-2 Inhibitors in Controlling Inflammation and Capsular Opacification after Phacoemulsification Cataract Removal. Vet. Ophthalmol. 2015, 18, 175–185. [Google Scholar] [CrossRef]
- Zhang, X.; Lai, K.; Li, S.; Wang, J.; Li, J.; Wang, W.; Ni, S.; Lu, B.; Grzybowski, A.; Ji, J.; et al. Drug-Eluting Intraocular Lens with Sustained Bromfenac Release for Conquering Posterior Capsular Opacification. Bioact. Mater. 2021, 9, 343–357. [Google Scholar] [CrossRef]
- Huang, X.; Wang, Y.; Cai, J.; Ma, X.; Li, Y.; Cheng, J.; Wei, R. Sustained Release of 5-Fluorouracil from Chitosan Nanoparticles Surface Modified Intra Ocular Lens to Prevent Posterior Capsule Opacification: An In Vitro and In Vivo Study. J. Ocul. Pharmacol. Ther. 2013, 29, 208–215. [Google Scholar] [CrossRef]
- Han, Y.; Tang, J.; Xia, J.; Wang, R.; Qin, C.; Liu, S.; Zhao, X.; Chen, H.; Lin, Q. Anti-Adhesive and Antiproliferative Synergistic Surface Modification of Intraocular Lens for Reduced Posterior Capsular Opacification. Int. J. Nanomed. 2019, 14, 9047–9061. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.; Zhao, X.; Tang, J.; Han, Y.; Lin, Q. Drug-Eluting Hydrophilic Coating Modification of Intraocular Lens via Facile Dopamine Self-Polymerization for Posterior Capsular Opacification Prevention. ACS Biomater. Sci. Eng. 2021, 7, 1065–1073. [Google Scholar] [CrossRef]
- Huang, H.; Zhu, S.; Liu, D.; Wen, S.; Lin, Q. Antiproliferative Drug-Loaded Multi-Functionalized Intraocular Lens for Reducing Posterior Capsular Opacification. J. Biomater. Sci. Polym. Ed. 2021, 32, 735–748. [Google Scholar] [CrossRef]
- Wertheimer, C.; Kueres, A.; Siedlecki, J.; Braun, C.; Kassumeh, S.; Wolf, A.; Mayer, W.; Priglinger, C.; Priglinger, S.; Eibl-Lindner, K. The Intraocular Lens as a Drug Delivery Device for an Epidermal Growth Factor–Receptor Inhibitor for Prophylaxis of Posterior Capsule Opacification. Acta Ophthalmol. 2018, 96, e874–e882. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kassumeh, S.; Kueres, A.; Hillenmayer, A.; von Studnitz, A.; Elhardt, C.; Ohlmann, A.; Priglinger, S.G.; Wertheimer, C.M. Development of a Drug-Eluting Intraocular Lens to Deliver Epidermal Growth Factor Receptor Inhibitor Gefitinib for Posterior Capsule Opacification Prophylaxis. Eur. J. Ophthalmol. 2021, 31, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Teng, H.; Zhang, H.; Tian, F.; Gu, H.Q.; Liu, X.; Sun, J. The study of cyclosporin A modified intraocular lens preventing posterior capsular opacification in rabbit eyes. Zhonghua Yan Ke Za Zhi 2016, 52, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Lu, D.; Han, Y.; Liu, D.; Chen, S.; Qie, J.; Qu, J.; Lin, Q. Centrifugally Concentric Ring-Patterned Drug-Loaded Polymeric Coating as an Intraocular Lens Surface Modification for Efficient Prevention of Posterior Capsular Opacification. Acta Biomater. 2021, 128, 327–341. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Zhang, Y.; Ma, H.; Zhang, C.; Fu, S. Comparison of Posterior Capsule Opacification in Rabbit Eyes Receiving Different Administrations of Rapamycin. Graefe’s Arch. Clin. Exp. Ophthalmol. 2014, 252, 1111–1118. [Google Scholar] [CrossRef]
- Ongkasin, K.; Masmoudi, Y.; Wertheimer, C.M.; Hillenmayer, A.; Eibl-Lindner, K.H.; Badens, E. Supercritical Fluid Technology for the Development of Innovative Ophthalmic Medical Devices: Drug Loaded Intraocular Lenses to Mitigate Posterior Capsule Opacification. Eur. J. Pharm. Biopharm. 2020, 149, 248–256. [Google Scholar] [CrossRef]
- Lee, E.H.; Joo, C.K. Role of Transforming Growth Factor-Beta in Transdifferentiation and Fibrosis of Lens Epithelial Cells. Investig. Ophthalmol. Vis. Sci. 1999, 40, 2025–2032. [Google Scholar]
- Sun, C.; Teng, W.; Cui, J.; Huang, X.; Yao, K. The Effect of Anti-TGF-Β2 Antibody Functionalized Intraocular Lens on Lens Epithelial Cell Migration and Epithelial–Mesenchymal Transition. Colloids Surf. B Biointerfaces 2014, 113, 33–42. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.; Zhang, C.; Chen, S.; Hu, J.; Shen, L.; Yu, Y. Research Progress Concerning a Novel Intraocular Lens for the Prevention of Posterior Capsular Opacification. Pharmaceutics 2022, 14, 1343. https://doi.org/10.3390/pharmaceutics14071343
Zhang Y, Zhang C, Chen S, Hu J, Shen L, Yu Y. Research Progress Concerning a Novel Intraocular Lens for the Prevention of Posterior Capsular Opacification. Pharmaceutics. 2022; 14(7):1343. https://doi.org/10.3390/pharmaceutics14071343
Chicago/Turabian StyleZhang, Yidong, Chengshou Zhang, Silong Chen, Jianghua Hu, Lifang Shen, and Yibo Yu. 2022. "Research Progress Concerning a Novel Intraocular Lens for the Prevention of Posterior Capsular Opacification" Pharmaceutics 14, no. 7: 1343. https://doi.org/10.3390/pharmaceutics14071343
APA StyleZhang, Y., Zhang, C., Chen, S., Hu, J., Shen, L., & Yu, Y. (2022). Research Progress Concerning a Novel Intraocular Lens for the Prevention of Posterior Capsular Opacification. Pharmaceutics, 14(7), 1343. https://doi.org/10.3390/pharmaceutics14071343






