Change in Nutritional and Biochemical Status in People Living with HIV-1 on Antiretroviral Therapy
Abstract
1. Introduction
2. Materials and Methods
2.1. Group Examined
2.2. Sample Collection
2.3. Physical Nutritional Examination and Anthropometry
- (i)
- The current body weight was measured on a scale with a capacity of 150 kg (accuracy of 100 g; the two groups were weighed barefoot wearing light clothing, without accessories or adornments; the current weight (CW) was compared with the ideal weight (IW) and its usual weight (UW) for the classification of the individual in relation to a nutritional change).
- (ii)
- The height was measured in meters by the technique described by Waitzberg (2001): using a metal stadiometer attached to the scale, without shoes or a hat, standing on the scale platform, with the heels together behind, and the body erect and the heels, buttocks, shoulders and head superficially touching the vertical wall of the measuring device with the line of sight facing the horizon [29].
- (iii)
- (iv)
- Triciptal skinfold (TS): the measurement of the skinfold thickness of the triceps, an appropriate method for determining body fat, was performed according to the procedure described by Augusto (1995) and Kamimura et al., (2005) [30,33]. Its interpretation was according to the standard of normality of Frisancho (1981), and the results were classified according to the reference values by Blackburn and Thornton (1979) [34,35].
2.4. Arm Circumference (AC)
2.5. Arm Muscle Circumference (AMC)
2.6. Bioelectrical Bioimpedance Body Fat (%BF-BIA)
2.7. HIV-1 Plasma Viral Load
2.8. Quantification of TCD4+ and CD8+ Lymphocytes
2.9. Biochemical Tests and Other Laboratory Tests
2.10. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- UNAIDS. Global HIV & AIDS Statistics—Fact Sheet. 2022. Available online: https://www.unaids.org/en/resources/fact-sheet (accessed on 9 June 2022).
- Ministerio de Saude. Boletim Epidemiológico HIV/AIDS. 2021. Available online: http://www.aids.gov.br/pt-br/pub/2021/boletim-epidemiologico-hivaids-2021 (accessed on 2 May 2022).
- Ministerio de Saude. Monitoramento da Infecção Pelo HIV. Available online: http://www.aids.gov.br/pt-br/profissionais-de-saude/hiv/monitoramento-da-infeccao-pelo-hiv (accessed on 2 May 2022).
- Horne, R.; Chapman, S.; Glendinning, E.; Date, H.L.; Guitart, J.; Cooper, V. Mind Matters: Treatment Concerns Predict the Emergence of Antiretroviral Therapy Side Effects in People with HIV. AIDS Behav. 2019, 23, 489–498. [Google Scholar] [CrossRef] [PubMed]
- Peters, B.S.; Conway, K. Therapy for HIV: Past, present, and future. Adv. Dent. Res. 2011, 23, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Dianatinasab, M.; Ghahri, S.; Dianatinasab, A.; Amanat, S.; Fararouei, M. Effects of Exercise on the Immune Function, Quality of Life, and Mental Health in HIV/AIDS Individuals. Adv. Exp. Med. Biol. 2020, 1228, 411–421. [Google Scholar]
- Palich, R. Traitement actuel de l’infection par le VIH. Rev Prat. 2021, 71, 976–982. [Google Scholar] [PubMed]
- Ministério da Saúde do Brasil. Vigitel Brasil 2017 Saúde Suplementar: Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico [Recurso Eletrônico]. 2018. Available online: http://bvsms.saude.gov.br/bvspublicacoes/vigitel_brasil_2017_saude_suplementa.pdf> (accessed on 10 January 2022).
- Pereira, M.D.; Teixeira, N.S.C.C.A.; Oliveira, I.K.F.; Lima, C.H.R.; Paiva, A.A. Esquema terapêutico e consumo alimentar em pessoas vivendo com HIV/AIDS. Arch. Health Investig. 2019, 8, 7. [Google Scholar] [CrossRef][Green Version]
- Von Roenn, J.H.; Roth, E.L.; Craig, R. HIV-related cachexia: Potential mechanisms and treatment. Oncology 1992, 49, 50–54. [Google Scholar] [CrossRef]
- Adal, M.; Howe, R.; Kassa, D.; Aseffa, A.; Petros, B. Malnutrition and lipid abnormalities in antiretroviral naïve HIV-infected adults in Addis Ababa: A cross-sectional study. PLoS ONE 2018, 13, e0195942. [Google Scholar] [CrossRef]
- Fernandes, J.F.L.; Costa, V.V.L.; Xavier, B.M.; Santos, O.V. Efeito da orientação alimentar sobre o perfil nutricional em pessoas vivendo com AIDS. Braz. J. Dev. 2021, 7, 76504–76519. [Google Scholar] [CrossRef]
- Reyskens, K.M.; Fisher, T.L.; Schisler, J.C.; O’Connor, W.G.; Rogers, A.B.; Willis, M.S.; Planesse, C.; Boyer, F.; Rondeau, P.; Bourdon, E.; et al. Cardio-metabolic effects of HIV protease inhibitors (lopinavir/ritonavir). PLoS ONE 2013, 8, e73347. [Google Scholar] [CrossRef]
- Noubissi, E.C.; Katte, J.C.; Sobngwi, E. Diabetes and HIV. Curr. Diabetes Rep. 2018, 18, 125. [Google Scholar] [CrossRef]
- Santos, M.A.; Muller, E.V.; Martins, C.M. Efeitos Metabólicos da Terapia Antirretroviral em Mulheres vivendo com HIV/AIDS. Res. Soc. Dev. 2022, 11, e58811125409. [Google Scholar] [CrossRef]
- Shubber, Z.; Calmy, A.; Andrieux-Meyer, I.; Vitoria, M.; Renaud-Théry, F.; Shaffer, N.; Hargreaves, S.; Mills, E.J.; Ford, N. Adverse events associated with nevirapine and efavirenz-based first-line antiretroviral therapy: A systematic review and meta-analysis. AIDS 2013, 27, 1403–1412. [Google Scholar] [CrossRef]
- Burgos, M.G.P.A.; Dias, C.A. Síndrome da imunodeficiência adquirida (AIDS). In Tratado de Nutrição e Dietoterapia; Rossi, L., Poltronieri, F., Eds.; Guanabara Koogan: Rio de Janeiro, Brazil, 2019; pp. 864–878. [Google Scholar]
- Saghayam, S.; Wanke, C. The impact of nutritional status and nutrition supplementation on outcomes along the HIV treatment cascade in the resource-limited setting. Curr. Opin. HIV AIDS 2015, 10, 472–476. [Google Scholar] [CrossRef] [PubMed]
- Knobel, H.; Domingo, P.; Suarez-Lozano, I.; Gutierrez, F.; Estrada, V.; Palacios, R.; Antela, A.; Blanco, J.R.; Fulladosa, X.; Refollo, E.; et al. Rate of cardiovascular, renal and bone disease and their major risks factors in HIV-infected individuals on antiretroviral therapy in Spain. Enferm. Infecc. Microbiol. Clin. 2019, 37, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Estrada, V.; Bernardino, J.I.; Masiá, M.; Iribarren, J.A.; Ortega, A.; Lozano, F.; Miralles, C.; Olalla, J.; Santos, J.; Elías, M.J.; et al. Cardiovascular risk factors and lifetime risk estimation in HIV-infected patients under antiretroviral treatment in Spain. HIV Clin. Trials 2015, 16, 57–65. [Google Scholar] [CrossRef]
- Domingo, P.; Suarez-Lozano, I.; Gutierrez, F.; Estrada, V.; Knobel, H.; Palacios, R.; Antela, A.; Blanco, J.R.; Fulladosa, X.; VACH. Predictive factors of renal impairment in HIV-infected patients on antiretroviral therapy: Results from the VACH longitudinal cohort study. Nefrologia 2019, 39, 497–505. [Google Scholar] [CrossRef]
- Mendes, E.L.; Andaki, A.C.R.; Amorim, P.R.S.; Natali, A.J.; Brito, C.J.; Paula, S.O. Treinamento físico para indivíduos HIV positivo submetidos à HAART: Efeitos sobre parâmetros antropométricos e funcionais. Rev. Bras. Med. Esporte 2013, 19, 16–21. [Google Scholar] [CrossRef][Green Version]
- Guira, O.; Tiéno, H.; Diendéré, A.E.; Sagna, Y.; Diallo, I.; Yaméogo, B.; Zoungrana, L.; Yaméogo, T.M.; Bognounou, R.; Drabo, J.Y. Features of Metabolic Syndrome and Its Associated Factors during Highly Active Antiretroviral Therapy in Ouagadougou (Burkina Faso). J. Int. Assoc. Provid. AIDS Care 2016, 15, 159–163. [Google Scholar] [CrossRef]
- Zhang, X.; Jiang, X.; Lu, H.; Shen, F.; Wang, J. Dyslipidaemia and Intima-Media Thickness of Carotid Arteries in Thirty-Five HIV/AIDS Patients Receiving Highly Active Antiretroviral Therapy. Int. J. Biomed. Sci. 2009, 5, 125–158. [Google Scholar]
- Henry, K.; Melroe, H.; HuebescH, J.; Hermundson, J.; Simpson, J. Atorvastatin and gemfibrozil for protease-inhibitor-related lipid abnormalities. Lancet 1998, 352, 1031–1032. [Google Scholar] [CrossRef]
- Purnell, J.Q.; Zambon, A.; Knopp, R.H.; Pizzuti, D.J.; Achari, R.; Leonard, J.M.; Locke, C.; Brunzell, J.D. Effect of ritonavir on lipids and post- heparin lipase activities in normal subjects. AIDS 2000, 14, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Mannarino, I.C. Dietoterapia. In Terapia Nutricional; Augusto, A.L.P., Alves, D.C., Mannarino, I.C., Gerude, M., Eds.; Atheneu: São Paulo, Brazil, 1995; pp. 201–204. [Google Scholar]
- Ferrini, M.T.; Waitzberg, D.L. Exame Físico e Antropometria. In Nutrição Enteral e Parenteral na Prática Clínica; Waitzberg, D.L., Ed.; Atheneu: Rio de Janeiro, Brazil, 1997; pp. 255–276. [Google Scholar]
- Waitzberg, D.L. Nutrição Oral Enteral e Parenteral na Prática Clínica; Atheneu: São Paulo, Brazil, 2001; 1857p. [Google Scholar]
- Kamimura, M.A.; Baxmann, A.; Sampaio, L.R.; Cuppari, L. Avaliação nutricional. In Guia de Nutrição: Nutrição Clínica no Adulto; Cuppari, L., Ed.; Manole: São Paulo, Brazil, 2005; pp. 89–115. [Google Scholar]
- Blackburn, G.L.; Bistrian, B.R.; Maini, B.S.; Chalamm, H.T.; Smith, M.F. Nutritional and melabolic assessment of the hospitalized patient. J. Parenter. Enter. Nutr. 1977, 1, 11–22. [Google Scholar] [CrossRef] [PubMed]
- WHO. Obesity: Preventing and Managing the Global Epidemic; WHO: Geneva, Switzerland, 1997; Available online: https://apps.who.int/iris/handle/10665/63854 (accessed on 10 March 2022).
- Augusto, A.L.P. Indicações do suporte nutricional. As bases da alimentação enteral. In Terapia Nutricional; Augusto, A.L.P., Alves, D.C., Mannarino, I.C., Gerude, M., Eds.; Atheneu: São Paulo, Brazil, 1995; pp. 38–53. [Google Scholar]
- Frisancho, A.R. New norms of upper limb fat and muscle áreas for assessent of nutritional status. Am. J. Clin. Nutr. 1981, 34, 2540–2545. [Google Scholar] [CrossRef] [PubMed]
- Blackburn, L.L.; Thornton, P.A. Nutritional assessment of the hospitalized patients. Med. Clin. 1979, 63, 1103–1115. [Google Scholar] [CrossRef]
- De Carvalho, B.F.; Policarpo, S.; Moreira, A.C. Nutritional status and quality of life in HIV-infected patients. Nutr. Hosp. 2017, 34, 923–933. [Google Scholar] [CrossRef]
- Santo, R.E.; Grinsztejn, B.; Peres, W.A.F.; Brito, P.D. Bioimpedância e antropometria na determinação da composição corporal em homens portadores de HIV. Rev. Bras. Nutr. Clin. 2016, 31, 60–64. [Google Scholar]
- Lagathu, C.; Béréziat, V.; Gorwood, J.; Fellahi, S.; Bastard, J.P.; Vigouroux, C.; Boccara, F.; Capeau, J. Metabolic complications affecting adipose tissue, lipid and glucose metabolism associated with HIV antiretroviral treatment. Expert Opin. Drug Saf. 2019, 18, 829–840. [Google Scholar] [CrossRef]
- Howard, B.V.; Ruotolo, G.; Robbins, D.C. Obesity and dyslipidemia. Endocrinol. Metab. Clin. N. Am. 2003, 32, 855–867. [Google Scholar] [CrossRef]
- Bailin, S.S.; Gabriel, C.L.; Wanjalla, C.N.; Koethe, J.R. Obesity and Weight Gain in Persons with HIV. Curr. HIV/AIDS Rep. 2020, 17, 138–150. [Google Scholar] [CrossRef]
- Morse, C.G.; McLaughlin, M.; Matthews, L.; Proschan, M.; Thomas, F.; Gharib, A.M.; Abu-Asab, M.; Orenstein, A.; Engle, R.E.; Hu, X.; et al. Nonalcoholic Steatohepatitis and Hepatic Fibrosis in HIV-1-Monoinfected Adults with Elevated Aminotransferase Levels on Antiretroviral Therapy. Clin. Infect. Dis. 2015, 60, 1569–1578. [Google Scholar] [CrossRef]
- Post, F. Adverse events: ART and the kidney: Alterations in renal function and renal toxicity. J. Int. AIDS Soc. 2014, 17, 19513. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Mellors, J.; Ruan, P.; Mc Mahon, D.; Keller, D.; Lederman, M.M. Viral dynamics and their relations to baseline factors and longer term virologic responses in treatment-naive HIV-1 infected patients receiving abacavir in combination with HIV-1 protease inhibitors. J. Acquir. Immune Defic. Syndr. 2003, 33, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Louie, M.; Hogan, C.; Di Mascio, M.; Hurley, A.; Simon, V.; Rooney, J.; Ruiz, N.; Brun, S.; Sun, E.; Perelson, A.S.; et al. Determining the relative efficacy of highly active antiretroviral therapy. J. Infect. Dis. 2003, 187, 896–900. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Van Leth, F.; Huisamen, C.B.; Badaro, R.; Vandercam, B.; De Wet, J.; Montaner, J.S.G.; Hall, D.B.; Wit, F.W.N.M.; Lange, J.M.A. Plasma HIV-1 RNA decline within the first two weeks of treatment is comparable for nevirapine, efavirenz, or both drugs combined and is not predictive of long-term virologic efficacy. J. Acquir. Immune Defic. Syndr. 2005, 38, 296–300. [Google Scholar]
- Moltó, J.; Ruiz, L.; Marta Valle, M.; Martinez-Picado, J.; Bonjoch, A.; Bravo, I.; Negredo, E.; Heilek-Sneider, G.; Clotet, B. Increased antiretroviral potency by the addition of enfuvirtide to a four-drug regimen in antiretroviral naive, HIV-infected patients. Antivir. Ther. 2006, 11, 47–51. [Google Scholar] [CrossRef]
- Kumar, V.; Singh, J.A. Prospective Study on Impact of Early Initiation of Antiretroviral Therapy in Human Immunodeficiency Virus-Positive Adults on Immunological Status and Adverse Events. J. Glob. Infect. Dis. 2019, 11, 73–79. [Google Scholar] [CrossRef]
- Schuelter-Trevisol, F.; Pucci, P.; Justino, A.Z.; Pucci, N.; Silva, A.C.B. Perfil epidemiológico dos pacientes com HIV atendidos no Sul do Estado de Santa Catarina, Brasil, em 2010. Epidemiol. Serviços Saúde 2013, 22, 87–94. [Google Scholar] [CrossRef]
- Silva, V.S.S.; Mori, R.M.S.C.; Guimarães, S.M. Alterações nutricionais em pacientes com lipodistrofia associada ao HIV/AIDS de uma Unidade de Referência do município de Belém—Pará. DST-J. Bras. Doenças Sex. Transm. 2012, 24, 233–238. [Google Scholar] [CrossRef]
- Braga, L.A.; Silva, C.A.B. Avaliação nutricional e metabólica de pacientes com HIV em uso da terapia antirretroviral no nordeste do Brasil. Rev. Bras. Promoção Saúde RBPS 2010, 23, 368–373. [Google Scholar]
- Passone, C.M.S. Antropometria na prática clínica. RUBS 2005, 1, 25–32. [Google Scholar]
- Gomes, T.B.; Lourival, N.B.S. Perfil nutricional dos pacientes HIV positivo do município de Apucarana (Pr). Rev. Saúde E Pesqui. 2016, 9, 83–92. [Google Scholar] [CrossRef]
- Rothman, K.J. BMI-related errors in the measurement of obesity. Int. J. Obes. 2008, 3, S56–S59. [Google Scholar] [CrossRef] [PubMed]
- WHO. A Healthy Lifestyle—WHO Recommendations. 2010. Available online: https://www.who.int/europe/news-room/fact-sheets/item/a-healthy-lifestyle---who-recommendations (accessed on 22 September 2022).
- Del Moral-Trinidad, L.E.; Romo-González, T.; Carmona Figueroa, Y.P.; Barranca Enríquez, A.; Palmeros Exsome, C.; Campos-Uscanga, Y. Potential for body mass index as a tool to estimate body fat in young people. Enferm. Clin. 2021, 31, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Jaime, P.C.; Florindo, A.A.; Latorre, M.R.D.O.; Brasil, B.G.; Santos, E.C.M.; Segurado, A.A.C. Prevalência de sobrepeso e obesidade abdominal em indivíduos portadores de HIV/AIDS, em uso de terapia anti-retroviral de alta potência. Rev. Bras. Epidemiol. 2004, 7, 65–72. [Google Scholar] [CrossRef]
- Silva, E.F.R.; Lewi, D.S.; Vedovato, G.M.; Garcia, V.R.S.; Tenore, S.B.; Bassichetto, K.C. Estado nutricional, clínico e padrão alimentar de pessoas vivendo com HIV/Aids em assistência ambulatorial no município de São Paulo. Rev. Bras. Epidemiol. 2010, 13, 677–688. [Google Scholar] [CrossRef]
- Ladeira, P.O.C.; Silva, D.C.G. Estado Nutricional e perfil alimentar de pacientes assistidos pelo programa de DST/AIDS e hepatites virais de um centro de saúde de Itaperuna-RJ. DST-J. Bras. Doenças Sex. Transm. 2012, 24, 28–31. [Google Scholar] [CrossRef]
- Jacobson, D.L.; Knox, T.; Spiegelman, D.; Skinner, S.; Gorbach, S.; Wanke, C. Prevalence of, evolution of, and risk factors for fat atrophy and fat deposition in a cohort of HIV-infected men and women. Clin. Infect. Dis. 2005, 40, 1837–1845. [Google Scholar] [CrossRef]

| Epidemiological Variables | n | % |
|---|---|---|
| Sex | ||
| Male | 30 | 71.4 |
| Female | 12 | 28.6 |
| Age range | ||
| 19 to 29 years | 21 | 50.0 |
| 30 to 39 years | 15 | 35.7 |
| 40 to 57 years | 6 | 14.3 |
| Education | ||
| Incomplete elementary school | 6 | 14.3 |
| Complete elementary school | 3 | 7.1 |
| Incomplete high school | 3 | 7.1 |
| Complete high school | 21 | 50 |
| Incomplete higher education | 5 | 11.9 |
| Complete higher education | 4 | 9.6 |
| Family income | ||
| <1 minimum wage | 4 | 9.6 |
| 1 to 3 minimum wages | 33 | 78.5 |
| 4 to 6 minimum wages | 4 | 9.6 |
| No information | 1 | 2.3 |
| Marital status | ||
| Single | 26 | 62 |
| Married | 15 | 35.7 |
| No information | 1 | 2.3 |
| Professionally active | ||
| Yes | 28 | 66.7 |
| No | 14 | 33.3 |
| Smoking | ||
| Yes | 14 | 33.3 |
| No | 28 | 66.7 |
| Alcoholism | ||
| Yes | 30 | 71.4 |
| No | 10 | 23.8 |
| No information | 2 | 4.8 |
| Physical activity | ||
| Yes | 6 | 14.3 |
| No | 36 | 85.7 |
| Comorbidities | ||
| Yes | 14 | 33.3 |
| No | 28 | 66.7 |
| Laboratory variables | Median | IQR |
| Total Cholesterol | 131.8 * | 30.8 ** |
| LDL | 70.8 * | 21.3 ** |
| HDL | 36.0 | 9.5 |
| Triglycerides | 109.5 | 78.8 |
| AST | 22.0 | 14.0 |
| ALT | 10.0 | 26.0 |
| Urea | 27.0 | 9.5 |
| Creatinine | 0.7 | 0.1 |
| LTCD4+/µL | 355.8 * | 216.3 ** |
| LTCD8+/µL | 926.5 | 670.7 |
| Nutritional status | Median | IQR |
| TS | 10.8 | 9.7 |
| AMC | 25.7 | 4.6 |
| BMI | 23.5 * | 3.4 ** |
| AC | 29.2 * | 3.2 ** |
| % BF-BIA | 21.1 * | 8.6 ** |
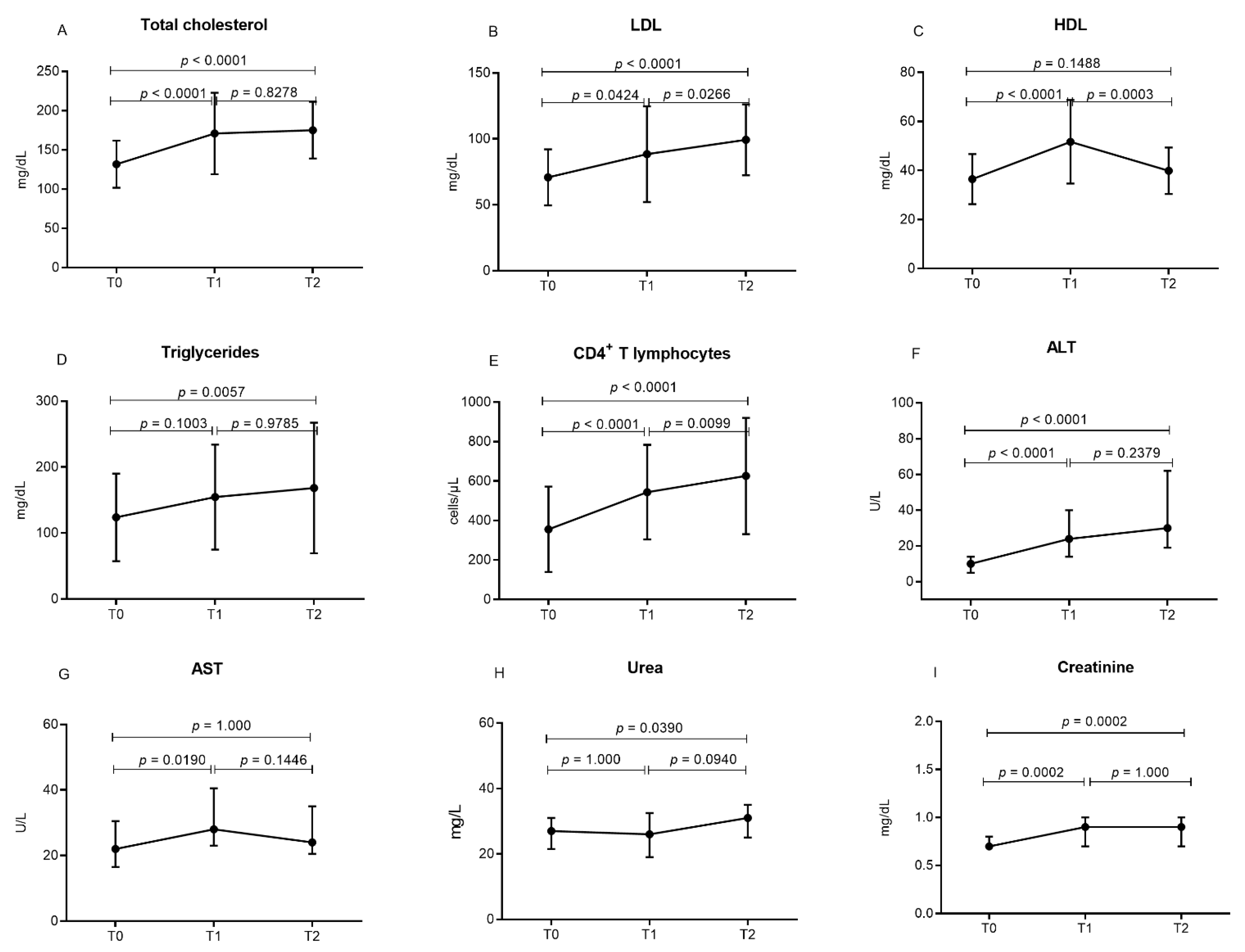
| Variables | T0 | T1 | T2 | ||||
|---|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | Median | IQR | p-Value | |
| Biochemical | |||||||
| Total Cholesterol | 131.8 * | 30.8 ** | 171.0 * | 51.9 ** | 175.1 * | 36.2 ** | <0.0001 a |
| LDL | 70.8 * | 21.3 ** | 88.4 * | 36.3 ** | 99. 3 * | 26.8 ** | <0.0001 a |
| HDL | 36.0 | 9.5 | 48.0 | 20.5 | 38.5 | 13.8 | <0.0001 b |
| Triglycerides | 109.5 | 78.8 | 142.0 | 107.0 | 146.0 | 134.6 | 0.0062 b |
| AST | 22.0 | 14.0 | 28.0 | 7.5 | 24.0 | 14.5 | 0.0172 b |
| ALT | 10.0 | 26.0 | 24.0 | 26.0 | 30.0 | 43.0 | <0.0001 b |
| Urea | 27.0 | 9.5 | 27.0 | 9.5 | 26.0 | 13.5 | 0.0234 b |
| Creatinine | 0.7 | 0.1 | 0.9 | 0.3 | 0.9 | 0.3 | <0.0001 b |
| Immunological | |||||||
| LTCD4+/µL | 355.8 * | 216.3 ** | 544.1 * | 239.3 ** | 626.1 * | 294.5** | <0.0001 a |
| LTCD8+/µL | 926.5 | 670.7 | 811.0 | 417.0 | 796.0 | 529.7 | 0.7079 b |
| CVlog10—Copies/mL | T0 n (%) | T1 n (%) | T2 n (%) |
|---|---|---|---|
| <1.61 | 0 (0.0) | 32 (76.2) | 37 (88.1) |
| 1.61–3.0 | 0 (0.0) | 5 (11.9) | 2 (4.8) |
| 3.1–5.0 | 33 (78.6) | 4 (9.5) | 3 (7.1) |
| >5.0 | 9 (21.4) | 1 (2.4) | 0 (0.0) |
| T0 | T1 | T2 | |||||
|---|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | Median | IQR | p-Value | |
| TS | 10.8 | 9.7 | 11.6 | 8.6 | 12.1 | 8.4 | 0.0027 b |
| AMC | 25.7 | 4.6 | 25.8 | 5.6 | 26.6 | 5.3 | 0.0917 b |
| BMI | 23.5 * | 3.4 ** | 24.2 * | 4.1 ** | 24.6 * | 4.2 ** | 0.0036 a |
| AC | 29.2 * | 3.2 ** | 29.3 * | 4.1 ** | 30.3 * | 3.9 ** | 0.0028 a |
| % BF-BIA | 21.1 * | 8.6 ** | 22.4 * | 8.8 ** | 22.6 * | 9.7 ** | 0.7164 a |
| Therapeutic | Start of ART | T1 | T2 |
|---|---|---|---|
| Schemes | n = 42 (%) | n = 42 (%) | n = 42 (%) |
| ITRN + ITRNN | 41 (97.6) | 38 (90.5) * | 37 (88.1) ** |
| 3TC + TDF + EFV | |||
| ITRN + IP | 01 (2.4) | 04 (9.5) | 03 (7.1) *** |
| 3TC + TDF + ATV/r | |||
| TRN + II + IP | - | - | 01 (2.4) |
| 3TC + TDF + DRV/r + DTG | |||
| II + IP | - | - | 01 (2.4) |
| DRV/r + DTG |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Souza, R.G.; Lima, S.S.; Pinto, A.C.; Souza, J.S.; Moura, T.C.F.; da Silva Graça Amoras, E.; Machado, L.F.A.; Guerreiro, J.F.; Vallinoto, A.C.R.; Queiroz, M.A.F.; et al. Change in Nutritional and Biochemical Status in People Living with HIV-1 on Antiretroviral Therapy. Viruses 2022, 14, 2573. https://doi.org/10.3390/v14112573
de Souza RG, Lima SS, Pinto AC, Souza JS, Moura TCF, da Silva Graça Amoras E, Machado LFA, Guerreiro JF, Vallinoto ACR, Queiroz MAF, et al. Change in Nutritional and Biochemical Status in People Living with HIV-1 on Antiretroviral Therapy. Viruses. 2022; 14(11):2573. https://doi.org/10.3390/v14112573
Chicago/Turabian Stylede Souza, Ranilda Gama, Sandra Souza Lima, Andresa Corrêa Pinto, Jacqueline Silva Souza, Tuane Carolina Ferreira Moura, Ednelza da Silva Graça Amoras, Luiz Fernando Almeida Machado, João Farias Guerreiro, Antonio Carlos Rosário Vallinoto, Maria Alice Freitas Queiroz, and et al. 2022. "Change in Nutritional and Biochemical Status in People Living with HIV-1 on Antiretroviral Therapy" Viruses 14, no. 11: 2573. https://doi.org/10.3390/v14112573
APA Stylede Souza, R. G., Lima, S. S., Pinto, A. C., Souza, J. S., Moura, T. C. F., da Silva Graça Amoras, E., Machado, L. F. A., Guerreiro, J. F., Vallinoto, A. C. R., Queiroz, M. A. F., & Ishak, R. (2022). Change in Nutritional and Biochemical Status in People Living with HIV-1 on Antiretroviral Therapy. Viruses, 14(11), 2573. https://doi.org/10.3390/v14112573







