Circulation and Molecular Epidemiology of Enteroviruses in Paralyzed, Immunodeficient and Healthy Individuals in Tunisia, a Country with a Polio-Free Status for Decades
Abstract
1. Introduction
2. Material and Methods
2.1. Studied Population and Sampling
2.2. Enterovirus Detection from Stool Samples
2.3. Identification of Viral Isolates
2.3.1. Typing of Nonpolio enteroviruses
2.3.2. Typing of Polioviruses and Identification of VDPVs
3. Results
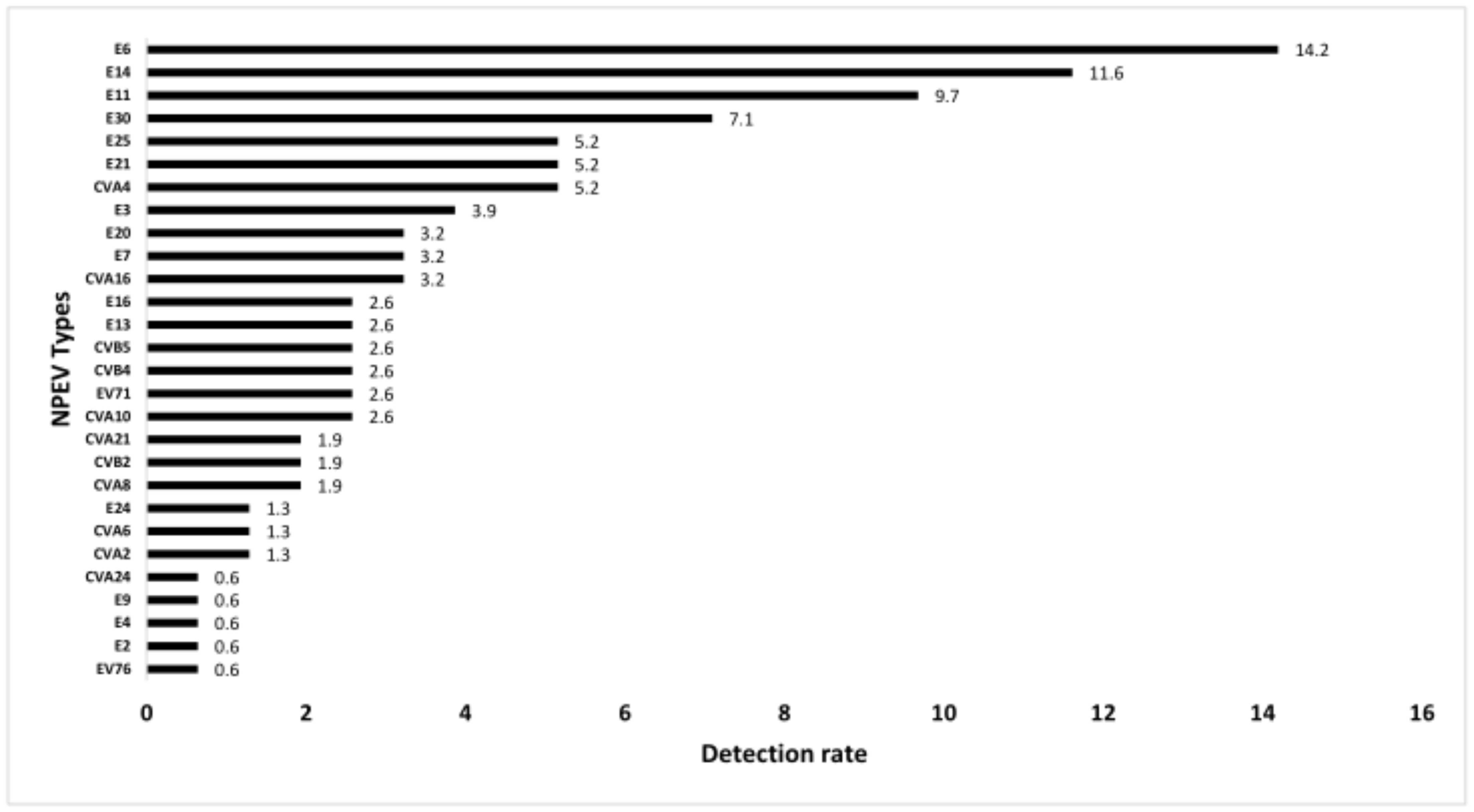
3.1. Nonpolio Enterovirus Detection
3.2. Poliovirus Detection
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jubelt, B.; Lipton, H.L. Enterovirus/Picornavirus infections. Handb. Clin. Neurol. 2014, 123, 379–416. [Google Scholar] [CrossRef] [PubMed]
- Zell, R.; Delwart, E.; Gorbalenya, A.E.; Hovi, T.; King, A.M.Q.; Knowles, N.J.; Lindberg, A.M.; Pallansch, M.A.; Palmenberg, A.C.; Reuter, G.; et al. ICTV Virus Taxonomy Profile: Picornaviridae. J. Gen. Virol. 2017, 98, 2421–2422. [Google Scholar] [CrossRef] [PubMed]
- Tapparel, C.; Siegrist, F.; Petty, T.J.; Kaiser, L. Picornavirus and enterovirus diversity with associated human diseases. Infect. Genet. Evol. 2013, 14, 282–293. [Google Scholar] [CrossRef] [PubMed]
- Morales, M.; Tangermann, R.H.; Wassilak, S.G. Progress toward Polio Eradication—Worldwide, 2015–2016. MMWR. Morb. Mortal. Wkly. Rep. 2016, 65, 470–473. [Google Scholar] [CrossRef]
- Previsani, N.; Singh, H.; Pierre, J.S.; Boualam, L.; Fournier-Caruana, J.; Sutter, R.W.; Zaffran, M. Progress Toward Containment of Poliovirus Type 2—Worldwide, 2017. Morb. Mortal. Wkly. Rep. 2017, 66, 649–652. [Google Scholar] [CrossRef][Green Version]
- Two out of Three Wild Poliovirus Strains Eradicated. Available online: https://polioeradication.org/news-post/two-out-of-three-wild-poliovirus-strains-eradicated/ (accessed on 16 February 2021).
- Centers for Disease Control and Prevention (CDC). Laboratory surveillance for wild and vaccine-derived polioviruses, January 2004–June 2005. MMWR Morb Mortal Wkly Rep. 2005, 54, 958–961. [Google Scholar]
- Kew, O.M.; Sutter, R.W.; De Gourville, E.M.; Dowdle, W.R.; Pallansch, M.A. Vaccine-derived polioviruses and the endgame strategy for global polio eradication. Annu. Rev. Microbiol. 2005, 59, 587–635. [Google Scholar] [CrossRef]
- Dunn, G.; Klapsa, D.; Wilton, T.; Stone, L.; Minor, P.D.; Martin, J. Twenty-Eight Years of Poliovirus Replication in an Immunodeficient Individual: Impact on the Global Polio Eradication Initiative. PLoS Pathog. 2015, 11, e1005114. [Google Scholar] [CrossRef] [PubMed]
- Hertel, N.T.; Pedersen, F.K.; Heilmann, C. Coxsackie B3 virus encephalitis in a patient with agammaglobulinaemia. Eur. J. Nucl. Med. Mol. Imaging 1989, 148, 642–643. [Google Scholar] [CrossRef]
- McKinney, J.R.E.; Katz, S.L.; Wilfert, C.M. Chronic Enteroviral Meningoencephalitis in Agammaglobulinemic Patients. Clin. Infect. Dis. 1987, 9, 334–356. [Google Scholar] [CrossRef]
- Cheng, F.W.T.; Chan, P.K.S.; Ho, W.C.S.; Wong, F.Y.W.; Leung, T.F. Recurrent enterovirus encephalitis: Chance or something else? BMJ Case Rep. 2009, 2009. [Google Scholar] [CrossRef] [PubMed]
- Majumdar, M.; Sharif, S.; Klapsa, D.; Wilton, T.; Alam, M.M.; Fernandez-Garcia, M.D.; Rehman, L.; Mujtaba, G.; McAllister, G.; Harvala, H.; et al. Environmental Surveillance Reveals Complex Enterovirus Circulation Patterns in Human Populations. Open Forum Infect. Dis. 2018, 5, ofy250. [Google Scholar] [CrossRef] [PubMed]
- Pons-Salort, M.; Oberste, M.S.; Pallansch, M.A.; Abedi, G.R.; Takahashi, S.; Grenfell, B.T.; Grassly, N.C. The seasonality of nonpolio enteroviruses in the United States: Patterns and drivers. Proc. Natl. Acad. Sci. USA 2018, 115, 3078–3083. [Google Scholar] [CrossRef]
- Bahri, O.; Rezig, D.; Ben Nejma-Oueslati, B.; Ben Yahia, A.; Ben Sassi, J.; Hogga, N.; Sadraoui, A.; Triki, H. Enteroviruses in Tunisia: Virological surveillance over 12 years (1992–2003). J. Med. Microbiol. 2005, 54, 63–69. [Google Scholar] [CrossRef]
- Haddad-Boubaker, S.; Ben Yahia, A.; Bahri, O.; Morel, V.; Balanant, J.; Delpeyroux, F.; Triki, H. Genetic features of polioviruses isolated in Tunisia, 1991–2006. J. Clin. Virol. 2008, 41, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Harvala, H.; Broberg, E.; Benschop, K.; Berginc, N.; Ladhani, S.N.; Susi, P.; Christiansen, C.; McKenna, J.; Allen, D.; Makiello, P.; et al. Recommendations for enterovirus diagnostics and characterisation within and beyond Europe. J. Clin. Virol. 2018, 101, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Rezig, D.; Ben Yahia, A.; Ben Abdallah, H.; Bahri, O.; Triki, H. Molecular characterization of coxsackievirus B5 isolates. J. Med Virol. 2003, 72, 268–274. [Google Scholar] [CrossRef]
- Oberste, M.S.; Maher, K.; Flemister, M.R. Comparison of classic and molecular approaches for the identification of untypeableenteroviruses. J. Clin. Microbiol. 2000, 38, 1170–1174. [Google Scholar] [CrossRef]
- Kumar, S.; Stecher, G.; Tamura, K. MEGA7: Molecular Evolutionary Genetics Analysis Version 7.0 for Bigger Datasets. Mol. Biol. Evol. 2016, 33, 1870–1874. [Google Scholar] [CrossRef]
- Oberste, M.S.; Maher, K.; Kilpatrick, D.R.; Flemister, M.R.; Brown, B.A.; Pallansch, M.A. Typing of human enteroviruses by partial sequencing of VP1. J. Clin. Microbiol. 1999, 37, 1288–1293. [Google Scholar] [CrossRef]
- Oberste, M.S.; Maher, K.; Kilpatrick, D.R.; Pallansch, M.A. Molecular Evolution of the Human Enteroviruses: Correlation of Serotype with VP1 Sequence and Application to Picornavirus Classification. J. Virol. 1999, 73, 1941–1948. [Google Scholar] [CrossRef]
- Lukashev, A.N.; Vakulenko, Y.A. Molecular evolution of types in non-polio enteroviruses. J. Gen. Virol. 2017, 98, 2968–2981. [Google Scholar] [CrossRef] [PubMed]
- Yan, D.; Zhang, Y.; Zhu, S.; Chen, N.; Li, X.; Wang, D.; Ma, X.; Zhu, H.; Tong, W.; Xu, W. Limited and localized outbreak of newly emergent type 2 vaccine-derived poliovirus in Sichuan, China. Clin Vaccine Immunol. 2014, 21, 1012–1018. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nix, W.A.; Khetsuriani, N.; Peñaranda, S.; Maher, K.; Venczel, L.; Cselkó, Z.; Freire, M.C.; Cisterna, D.; Lema, C.L.; Rosales, P.; et al. Diversity of picornaviruses in rural Bolivia. J. Gen. Virol. 2013, 94, 2017–2028. [Google Scholar] [CrossRef] [PubMed]
- Sanders, R.; Maher, C.; Aylward, R.B.; Bilous, J.; Schnur, A.; Sato, Y.; Omi, S.; Tangermann, R.H. Development and Coordination of the Polio Laboratory Network in the Western Pacific Region of the World Health Organization. J. Infect. Dis. 1997, 175, S117–S121. [Google Scholar] [CrossRef][Green Version]
- Apostol, L.N.; Suzuki, A.; Bautista, A.; Galang, H.; Paladin, F.J.; Fuji, N.; Lupisan, S.; Olveda, R.; Oshitani, H. Detection of non-polio enteroviruses from 17 years of virological surveillance of acute flaccid paralysis in the Philippines. J. Med. Virol. 2012, 84, 624–631. [Google Scholar] [CrossRef] [PubMed]
- Bessaud, M.; Pillet, S.; Ibrahim, W.; Joffret, M.-L.; Pozzetto, B.; Delpeyroux, F.; Gouandjika-Vasilache, I. Molecular Characterization of Human Enteroviruses in the Central African Republic: Uncovering Wide Diversity and Identification of a New Human Enterovirus A71 Genogroup. J. Clin. Microbiol. 2012, 50, 1650–1658. [Google Scholar] [CrossRef] [PubMed]
- Benschop, K.S.M.; Rahamat-Langendoen, J.C.; Van Der Avoort, H.G.A.M.; Claas, E.C.J.; Pas, S.D.; Schuurman, R.; Verweij, J.J.; Wolthers, K.C.; Niesters, H.G.M.; Koopmans, M.P.G.; et al. VIRO-TypeNed, systematic molecular surveillance of enteroviruses in the Netherlands between 2010 and 2014. Eurosurveillance 2016, 21. [Google Scholar] [CrossRef]
- Opanda, S.M.; Wamunyokoli, F.; Khamadi, S.; Coldren, R.; Bulimo, W.D. Genotyping of enteroviruses isolated in Kenya from pediatric patients using partial VP1 region. Springerplus 2016, 5, 1–12. [Google Scholar] [CrossRef][Green Version]
- Fernandez-Garcia, M.D.; Kebe, O.; Fall, A.D.; Ndiaye, K. Identification and molecular characterization of non-polio enteroviruses from children with acute flaccid paralysis in West Africa, 2013–2014. Sci. Rep. 2017, 7, 1–11. [Google Scholar] [CrossRef]
- Holmes, C.W.; Koo, S.S.; Osman, H.; Wilson, S.; Xerry, J.; Gallimore, C.I.; Allen, D.J.; Tang, J.W. Predominance of enterovirus B and echovirus 30 as cause of viral meningitis in a UK population. J. Clin. Virol. 2016, 81, 90–93. [Google Scholar] [CrossRef]
- Guerra, J.A.; Waters, A.; Kelly, A.; Morley, U.; O’Reilly, P.; O’Kelly, E. Seroepidemiological and phylogenetic characterization of neurotropic enteroviruses in Ireland, 2005–2014. J. Med. Virol. 2017, 89, 1550–1558. [Google Scholar] [CrossRef]
- Papa, A.; Skoura, L.; Dumaidi, K.; Spiliopoulou, A.; Antoniadis, A.; Frantzidou, F. Molecular epidemiology of Echovirus 6 in Greece. Eur. J. Clin. Microbiol. Infect. Dis. 2009, 28, 683–687. [Google Scholar] [CrossRef]
- Bailly, J.-L.; Mirand, A.; Henquell, C.; Archimbaud, C.; Chambon, M.; Regagnon, C.; Charbonné, F.; Peigue-Lafeuille, H. Repeated genomic transfers from echovirus 30 to echovirus 6 lineages indicate co-divergence between co-circulating populations of the two human enterovirus serotypes. Infect. Genet. Evol. 2011, 11, 276–289. [Google Scholar] [CrossRef]
- Smura, T.; Kakkola, L.; Blomqvist, S.; Klemola, P.; Parsons, A.; Kallio-Kokko, H.; Savolainen-Kopra, C.; Kainov, D.E.; Roivainen, M. Molecular evolution and epidemiology of echovirus 6 in Finland. Infect. Genet. Evol. 2013, 16, 234–247. [Google Scholar] [CrossRef]
- Tao, Z.; Song, Y.; Wang, H.; Zhang, Y.; Yoshida, H.; Ji, S.; Xu, A.; Song, L.; Liu, Y.; Cui, N.; et al. Intercity Spread of Echovirus 6 in Shandong Province, China: Application of Environmental Surveillance in Tracing Circulating Enteroviruses. Appl. Environ. Microbiol. 2012, 78, 6946–6953. [Google Scholar] [CrossRef][Green Version]
- Benschop, K.S.M.; Geeraedts, F.; Beuvink, B.; Spit, S.A.; Fanoy, E.B.; Claas, E.C.J.; Pas, S.D.; Schuurman, R.; Verweij, J.J.; Bruisten, S.M.; et al. Increase in ECHOvirus 6 infections associated with neurological symptoms in the Netherlands, June to August 2016. Eurosurveillance 2016, 21, 21. [Google Scholar] [CrossRef]
- Saeed, M.; Zaidi, S.Z.; Naeem, A.; Masroor, M.; Sharif, S.; Shaukat, S.; Angez, M.; Khan, A. Epidemiology and clinical findings associated with enteroviral acute flaccid paralysis in Pakistan. BMC Infect. Dis. 2007, 7, 6. [Google Scholar] [CrossRef] [PubMed]
- Tao, Z.; Wang, H.; Liu, Y.; Li, Y.; Jiang, P.; Liu, G.; Lin, X.; Li, M.; Wang, S.; Ji, F.; et al. Non-Polio Enteroviruses from Acute Flaccid Paralysis Surveillance in Shandong Province, China, 1988–2013. Sci. Rep. 2014, 4, 6167. [Google Scholar] [CrossRef] [PubMed]
- Österback, R.; Kalliokoski, T.; La¨hdesma¨ki, T.; Peltola, V.; Ruuskanen, O.; Waris, M. Echovirus 30 meningitis epidemic followed by an outbreak-specific RT-qPCR. J. Clin.Virol. 2015, 69, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Yarmolskaya, M.S.; Shumilina, E.Y.; Ivanova, O.E.; Drexler, J.F.; Lukashev, A.N. Molecular epidemiology of echoviruses 11 and 30 in Russia: Different properties of genotypes within an enterovirus serotype. Infect. Genet. Evol. 2015, 30, 244–248. [Google Scholar] [CrossRef]
- Richter, J.; Koptides, D.; Tryfonos, C.; Christodoulou, C. Molecular typing of enteroviruses associated with viral meningitis in Cyprus, 2000–2002. J. Med. Microbiol. 2006, 55, 1035–1041. [Google Scholar] [CrossRef] [PubMed]
- Li, H.-G.; Lao, Q. The pulmonary complications associated with EV71-infected hand–foot–mouth disease. Radiol. Infect. Dis. 2017, 4, 137–142. [Google Scholar] [CrossRef]
- Mbaeyi, C.; Wadood, Z.M.; Moran, T.; Ather, F.; Stehling-Ariza, T.; Nikulin, J.; Al Safadi, M.; Iber, J.; Zomahoun, L.; Abourshaid, N.; et al. Strategic Response to an Outbreak of Circulating Vaccine-Derived Poliovirus Type 2—Syria, 2017-2018. Morb. Mortal. Wkly. Rep. 2018, 67, 690–694. [Google Scholar] [CrossRef] [PubMed]
- Immunization Systems Management Group of the Global Polio Eradication Initiative. Introduction of Inactivated Poliovirus Vaccine and Switch from Trivalent to Bivalent Oral Poliovirus Vaccine—Worldwide, 2013–2016. MMWR Morb. Mortal. Wkly. Rep. 2015, 64, 699–702. [Google Scholar]
- Ma, Y.; Wang, X.; Zhou, X.; Lv, P.; Wang, H.; Song, J.; Song, C.; Sun, Z. Poliovirus Detection and Genetic Characteristic from Sewage in Heilongjiang Province from 2013 to 2016. Jpn. J. Infect. Dis. 2018, 71, 442–447. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhu, S.L.; Zhao, R. Study of VP1 region gene code of Sabin-Like strain in acute flaccid paralysis (AFP) clinical case of China. Chin. J. Virol. 2004, 20, 28–33. [Google Scholar]
- Nomoto, A.; Omata, T.; Toyoda, H.; Kuge, S.; Horie, H.; Kataoka, Y.; Genba, Y.; Nakano, Y.; Imura, N. Complete nucleotide sequence of the attenuated poliovirus Sabin 1 strain genome. Proc. Natl. Acad. Sci. USA 1982, 79, 5793–5797. [Google Scholar] [CrossRef] [PubMed]
- Ren, R.B.; Moss, E.G.; Racaniello, V.R. Identification of two determinants that attenuate vaccine-related type II poliovirus. J. Virol. 1991, 65, 1377–1382. [Google Scholar] [CrossRef] [PubMed]
| Number of Individuals per Year (Stool Samples) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinical Status | Total Studied Individuals (Stool Samples) | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 |
| Paralytic cases | 607 (1296) | 49 (109) | 60 (129) | 42 (85) | 58 (126) | 48 (101) | 56 (123) | 41 (86) | 43 (91) | 61 (126) | 87 (184) | 62 (136) |
| Healthy contacts | 825 (825) | 154 (154) | 96 (96) | 60 (60) | 65 (65) | 34 (34) | 85 (85) | 30 (30) | 60 (60) | 80 (80) | 61 (61) | 100 (100) |
| Immunodeficients | 290 (614) | 14 (22) | 18 (36) | 53 (118) | 61 (138) | 20 (61) | 23 (50) | 19 (37) | 41 (83) | 21 (35) | 11 (20) | 9 (14) |
| TOTAL | 1722 (2735) | 217 (285) | 174 (261) | 155 (263) | 184 (329) | 102 (196) | 164 (258) | 90 (153) | 144 (234) | 162 (241) | 104 (265) | 171 (250) |
| Species | Types | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | CV-A2 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 2 |
| CV-A4 | 0 | 0 | 0 | 0 | 3 | 0 | 1 | 1 | 1 | 0 | 2 | 8 | |
| CV-A6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 2 | |
| CV-A8 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 2 | 0 | 0 | 3 | |
| CV-A10 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 3 | 4 | |
| CV-A16 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 2 | 5 | |
| EV-A71 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 2 | 0 | 4 | |
| EV-A76 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | |
| B | CV-B2 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| CV-B4 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 1 | 4 | |
| CVB5 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | |
| E2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | |
| E3 | 3 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 6 | |
| E4 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | |
| E6 | 0 | 0 | 5 | 4 | 10 | 0 | 0 | 0 | 3 | 0 | 0 | 22 | |
| E7 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 3 | 1 | 5 | |
| E9 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | |
| E11 | 1 | 3 | 0 | 7 | 0 | 0 | 2 | 0 | 0 | 0 | 2 | 15 | |
| E13 | 0 | 0 | 0 | 3 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 4 | |
| E14 | 0 | 0 | 4 | 11 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 18 | |
| E16 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | |
| E20 | 0 | 0 | 0 | 0 | 0 | 5 | 0 | 0 | 0 | 0 | 0 | 5 | |
| E21 | 1 | 5 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 8 | |
| E24 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | |
| E25 | 0 | 0 | 0 | 0 | 2 | 2 | 0 | 0 | 4 | 0 | 0 | 8 | |
| E30 | 0 | 0 | 0 | 5 | 2 | 1 | 0 | 2 | 0 | 0 | 1 | 11 | |
| C | CV-A21 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 3 |
| CV-A24 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | |
| Total | 6 | 12 | 18 | 30 | 22 | 14 | 3 | 11 | 11 | 16 | 12 | 155 | |
| Positivity Rate | 2.1 | 4.6 | 6.8 | 9.1 | 11.2 | 5.4 | 2.0 | 4.7 | 4.6 | 6.0 | 4.8 |
| N° of Stool Samples | N° of Positive Polioviruses Per Clinical Status Per Year | Total N° | Positivity Rate | |||
|---|---|---|---|---|---|---|
| PV1 | PV2 | PV3 | ||||
| AFP * | 1296 | 7 | 4 | 8 | 19 | 1.5 |
| Healthy contacts | 825 | 4 | 3 | 4 | 11 | 1.3 |
| Patients with PIDs ** | 614 | 14 | 16 | 12 | 42 | 6.8 |
| Total | 2735 | 25 | 23 | 24 | 72 | 2.6 |
| 2007 | 285 | 0 | 6 | 0 | 6 | 2.1 |
| 2008 | 261 | 1 | 1 | 2 | 4 | 1.5 |
| 2009 | 263 | 5 | 3 | 2 | 10 | 3.8 |
| 2010 | 329 | 6 | 2 | 4 | 12 | 3.6 |
| 2011 | 196 | 0 | 2 | 1 | 3 | 1.5 |
| 2012 | 258 | 1 | 5 | 2 | 8 | 3.1 |
| 2013 | 153 | 5 | 0 | 0 | 5 | 3.3 |
| 2014 | 234 | 3 | 4 | 3 | 10 | 4.3 |
| 2015 | 241 | 1 | 0 | 3 | 4 | 1.7 |
| 2016 | 265 | 0 | 0 | 4 | 4 | 1.5 |
| 2017 | 250 | 3 | 0 | 3 | 6 | 2.4 |
| Total | 2735 | 25 | 23 | 24 | 72 | 2.6 |
| Serotype | Isolated Strains | N° of mutations in the Entire VP1 Region | Synonymous Mutations | Nonsynonymous Mutations | Amino Acid Changes | N° of Mixed Bases | Position(s) of Mixed Base(s) | Final N° of Nucleotide Changes |
|---|---|---|---|---|---|---|---|---|
| Type 1 | PV1 *-S326-PIDs +-TUN-09 | 5 | C2722U, G2740A | G2749A, A2775G, A2795G | Ile90Met, Lys99Arg, Thr106Ala | 7 | C2544Y a, G2701R b, U2731W c, C2752Y, U2872Y, C3088Y, G3376R | 12 |
| PV1-S358-PIDs-TUN-09 | 14 | G2678A, C2722U, G2740A, C2761U, U2767C, U2872C, U3154C, G3292A, G3371A, G3376A | C2544U, G2749A, A2775G, A2795G | Thr22Met, Ile90Met, Lys99Arg, Thr106Ala, | 0 | 14 | ||
| PV1-S047-PIDs-TUN-10 | 11 | U2569C, C2722U, G2740A, U2872C, C3144U, G3292A, G3376A | C2544U, G2749A, A2775G, A2795G | Thr22Met, Ile90Met, Lys99Arg, Thr106Ala, | 0 | 11 | ||
| PV1-S200-PIDs-TUN-13 | 6 | U2779C, C2968U, A3033U, U3352C | A2747U, G2776U | Ile90Leu, Lys99Asn | 5 | G2620R, U2626Y, G2957R, A3079Y, U3169Y | 11 | |
| Type 2 | PV2-S177-PIDs-TUN-14 | 9 | G2502A, A2518G, C2560U, A2628G, A2718G, C2787U, A2992G, G3093A, U3111C | 0 | 9 | |||
| PV2-S293-PIDs-TUN-07 | 3 | G3048A | C2540U, U2909C | Pro20Leu, Ile143Thr | 6 | U2499Y, G2625R, C2706Y, A2838R, G2892R, A3375R | 8 | |
| PV2-S294-PIDs-TUN-07 | 3 | G3048A | C2540U, U2909C | Pro20Leu, Ile143Thr | 6 | U2499Y, G2625R, C2706Y, A2838R, G2892R, A3375R | 10 | |
| PV2-S297-PIDs-TUN-07 | 5 | U2523C, C2595U, G2694A, U2814A | U2909C | Ile143Thr | 1 | A3122R | 6 | |
| PV2-S001-PIDs-TUN-08 | 4 | G2892A, G3048A | C2540U, U2909C | Pro20Leu, Ile143Thr | 4 | U2499Y, G2625R, C2706Y, A3375R | 8 | |
| Type 3 | PV3-S335-AFP |-TUN-16 | 2 | C2637U, U2790C | Ala54Val, Met105Thr | 8 | U2503W, A2716R, U2876Y, G2888K d, A2897R, A3017R, G3107K, A3232R | 10 | |
| PV3-S011-AFP-TUN-17 | 10 | U2860C, U3205A, U3364C | C2637U, U2790C, G2888U, A2897G, A3017G, A3111G, G3334U | Ala54Val, Met105Thr, Ala137Ser, Ala138Ser, Ile181Val, Lys212Arg, Arg286Ser | 1 | G2866R | 11 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chouikha, A.; Rezig, D.; Driss, N.; Abdelkhalek, I.; Ben Yahia, A.; Touzi, H.; Meddeb, Z.; Ben Farhat, E.; Yahyaoui, M.; Triki, H. Circulation and Molecular Epidemiology of Enteroviruses in Paralyzed, Immunodeficient and Healthy Individuals in Tunisia, a Country with a Polio-Free Status for Decades. Viruses 2021, 13, 380. https://doi.org/10.3390/v13030380
Chouikha A, Rezig D, Driss N, Abdelkhalek I, Ben Yahia A, Touzi H, Meddeb Z, Ben Farhat E, Yahyaoui M, Triki H. Circulation and Molecular Epidemiology of Enteroviruses in Paralyzed, Immunodeficient and Healthy Individuals in Tunisia, a Country with a Polio-Free Status for Decades. Viruses. 2021; 13(3):380. https://doi.org/10.3390/v13030380
Chicago/Turabian StyleChouikha, Anissa, Dorra Rezig, Nadia Driss, Ichrak Abdelkhalek, Ahlem Ben Yahia, Henda Touzi, Zina Meddeb, Essia Ben Farhat, Mahrez Yahyaoui, and Henda Triki. 2021. "Circulation and Molecular Epidemiology of Enteroviruses in Paralyzed, Immunodeficient and Healthy Individuals in Tunisia, a Country with a Polio-Free Status for Decades" Viruses 13, no. 3: 380. https://doi.org/10.3390/v13030380
APA StyleChouikha, A., Rezig, D., Driss, N., Abdelkhalek, I., Ben Yahia, A., Touzi, H., Meddeb, Z., Ben Farhat, E., Yahyaoui, M., & Triki, H. (2021). Circulation and Molecular Epidemiology of Enteroviruses in Paralyzed, Immunodeficient and Healthy Individuals in Tunisia, a Country with a Polio-Free Status for Decades. Viruses, 13(3), 380. https://doi.org/10.3390/v13030380








