Attitudes towards Anti-SARS-CoV2 Vaccination among Healthcare Workers: Results from a National Survey in Italy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Questionnaire Development
2.3. Statistical Analysis
3. Results
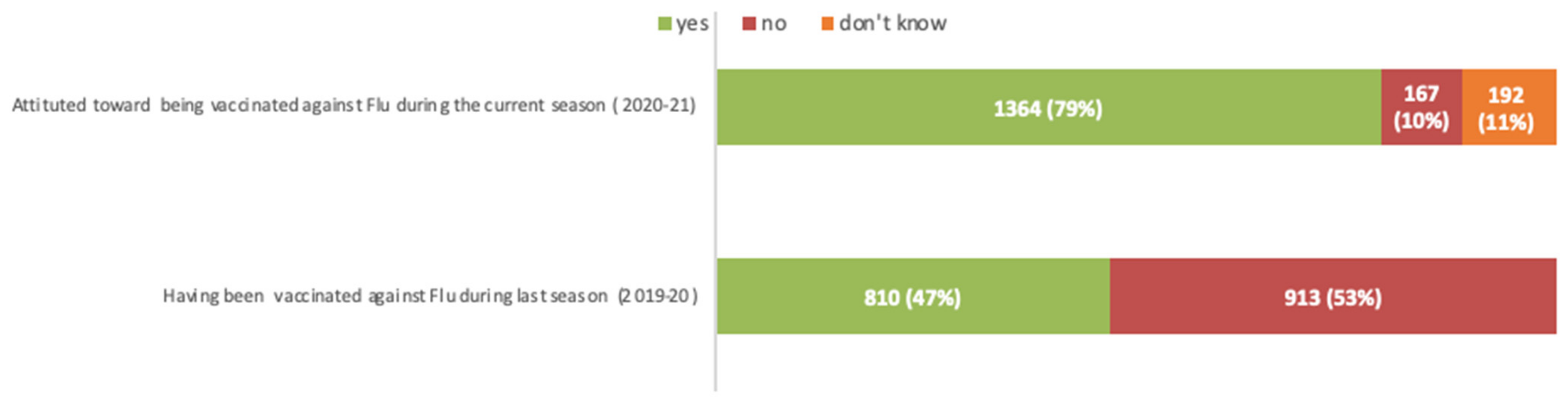
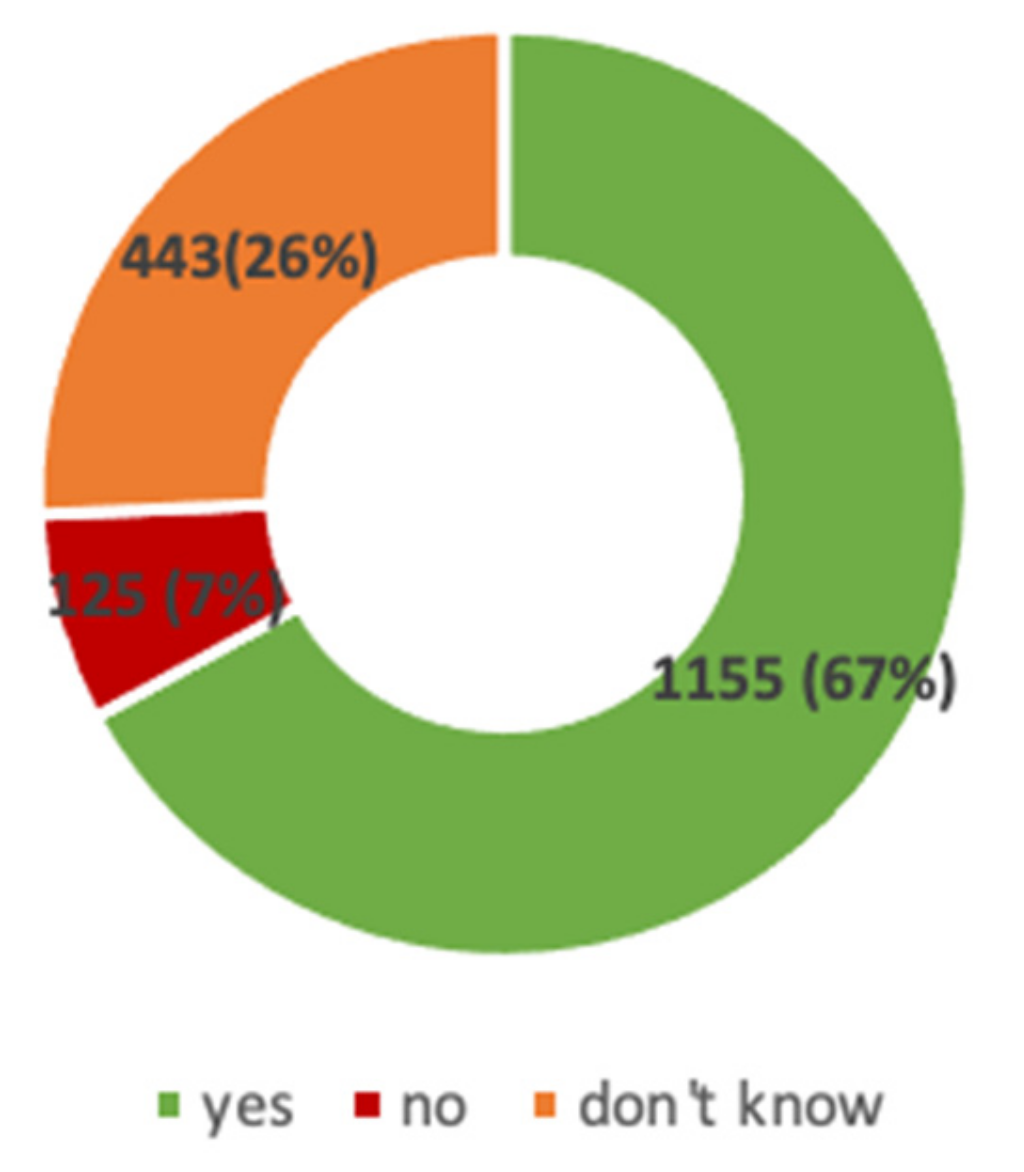
3.1. Attitude and Practice towards Vaccination against Flu and SARS-CoV-2
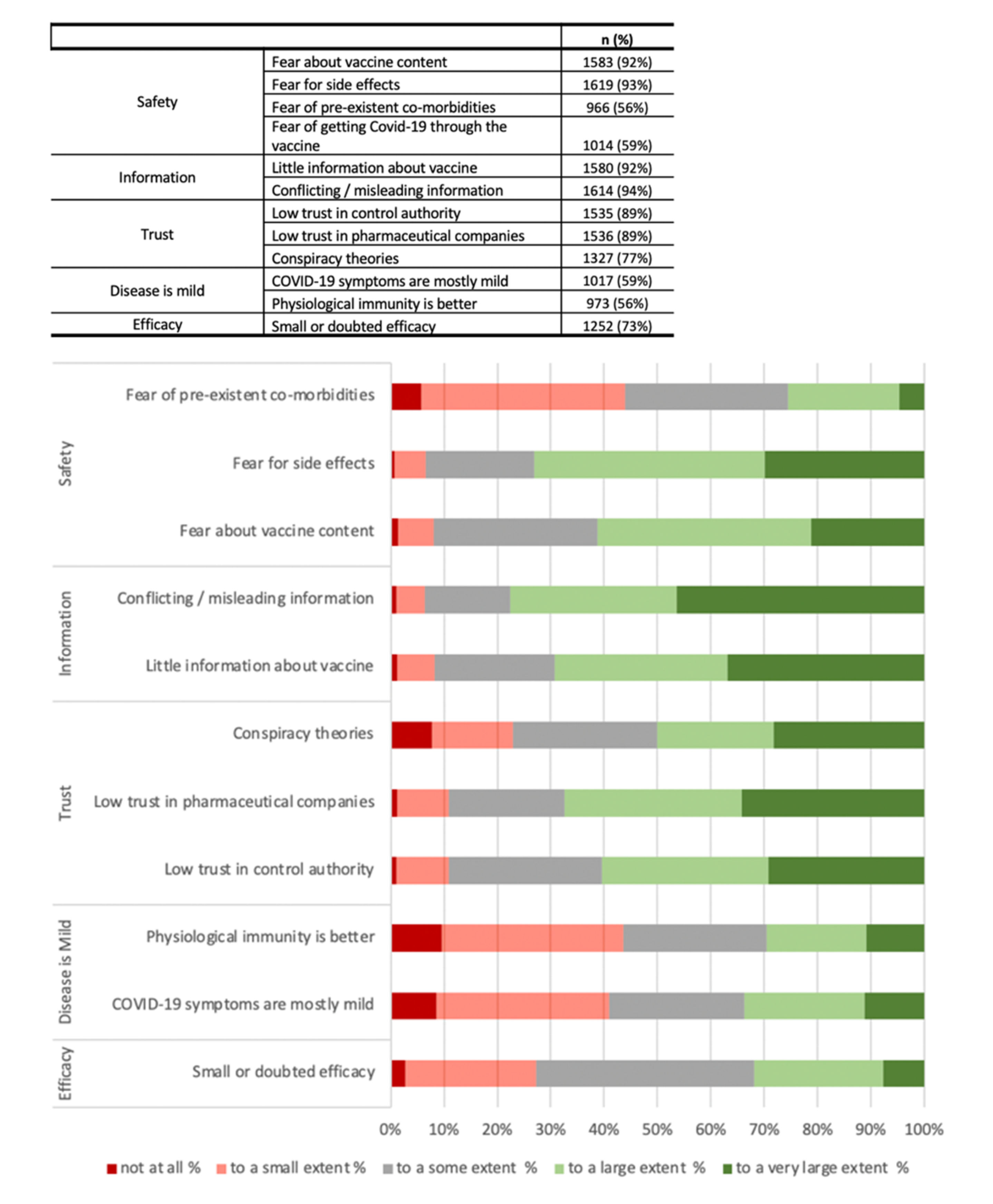
3.2. Predictors of COVID-19 Vaccine Hesitancy
3.3. Vaccine Hesitancy among the General Population
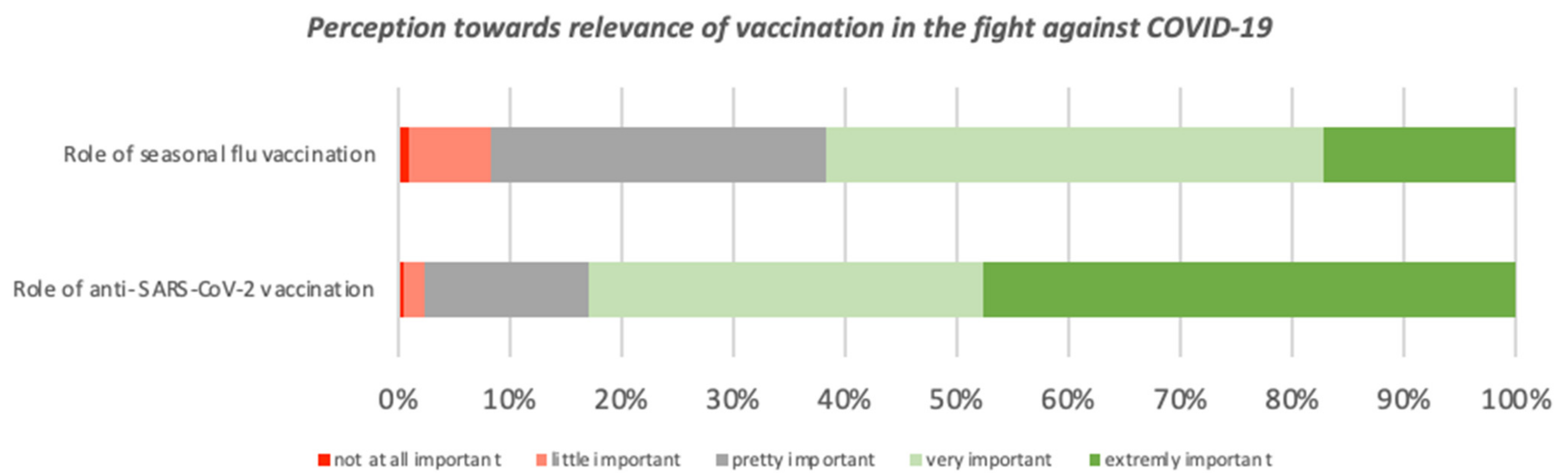
3.4. Perceptions towards Relevance of Vaccinations in the Fight against COVID-19
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Situation Report. 2020. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update---12-january-2021 (accessed on 14 January 2021).
- BBC News. Covid-19 Pandemic: Tracking the Global Coronavirus Outbreak. Available online: https://www.bbc.com/news/world-51235105 (accessed on 28 October 2020).
- Chou, R.; Dana, T.; Buckley, D.I.; Selph, S.; Fu, R.; Totten, A.M. Epidemiology of and Risk Factors for Coronavirus Infection in Health Care Workers. Ann. Intern. Med. 2020, 173, 120–136. [Google Scholar] [CrossRef]
- Li, Y.; Campbell, H.; Kulkarni, D.; Harpur, A.; Nundy, M.; Wang, X.; Nair, H. The temporal association of introducing and lifting non-pharmaceutical interventions with the time-varying reproduction number (R) of SARS-CoV-2: A modelling study across 131 countries. Lancet Infect. Dis. 2020, 20, 30785–30794. [Google Scholar] [CrossRef]
- Delamater, P.L.; Street, E.J.; Leslie, T.F.; Yang, Y.T.; Jacobsen, K.H. Complexity of the Basic Reproduction Number (R0). Emerg. Infect. Dis. 2019, 25, 1–4. [Google Scholar] [CrossRef]
- Cowling, B.J.; Ali, S.T.; Ng, T.W.Y.; Tsang, T.K.; Li, J.C.M.; Fong, M.W.; Liao, Q.; Kwan, M.Y.; Lee, S.L.; Chiu, S.S.; et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. Lancet Public Heal. 2020, 5, e279–e288. [Google Scholar] [CrossRef]
- Organisation for Economic Cooperation and Development. OECD Employment Outlook 2020: Worker Security and the COVID-19 Crisis. 2020. Available online: https://www.oecd-ilibrary.org/employment/oecd-employment-outlook-2020_1686c758-en (accessed on 15 January 2021).
- Flaxman, S.; Mishra, S.; Gandy, A.; Unwin, H.J.T.; Mellan, T.A.; Coupland, H.; Whittaker, C.; Zhu, H.; Berah, T.; Eaton, J.W.; et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature 2020, 584, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Jeyanathan, M.; Afkhami, S.; Smaill, F.; Miller, M.S.; Lichty, B.D.; Xing, Z. Immunological considerations for COVID-19 vaccine strategies. Nat. Rev. Immunol. 2020, 20, 615–632. [Google Scholar] [CrossRef]
- Omer, S.B.; Yildirim, I.; Forman, H.P. Herd Immunity and Implications for SARS-CoV-2 Control. JAMA 2020, 324, 2095–2096. [Google Scholar] [CrossRef]
- World Health Organization. 2020. Available online: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines (accessed on 4 November 2020).
- Ministero Della Salute. Report Vaccini Anti COVID-19. Available online: https://app.powerbi.com/view?r=eyJrIjoiMzg4YmI5NDQtZDM5ZC00ZTIyLTgxN2MtOTBkMWM4MTUyYTg0IiwidCI6ImFmZDBhNzVjLTg2NzEtNGNjZS05MDYxLTJjYTBkOTJlNDIyZiIsImMiOjh9 (accessed on 4 January 2021).
- Plotkin, S. History of vaccination. Proc. Natl. Acad. Sci. USA 2014, 111, 12283–12287. [Google Scholar] [CrossRef]
- E Andre, F.; Booy, R.; Bock, H.L.; Clemens, J.; Datta, S.K.; John, T.J.; Lee, B.W.; Lolekha, S.; Peltola, H.; A Ruff, T.; et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull. World Heal. Organ. 2008, 86, 140–146. [Google Scholar] [CrossRef]
- Larson, H.J.; Cooper, L.Z.; Eskola, J.; Katz, S.L.; Ratzan, S. Addressing the vaccine confidence gap. Lancet 2011, 378, 526–535. [Google Scholar] [CrossRef]
- Dubé, E.; Laberge, C.; Guay, M.; Bramadat, P.; Roy, R.; Bettinger, J.A. Vaccine hesitancy. Hum. Vaccines Immunother. 2013, 9, 1763–1773. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Vaccine hesitancy among healthcare workers and their patients in Europe–A qualitative study; ECDC: Stockholm, Sweden, 2015. [Google Scholar]
- Ministero della Salute. Parliamo di Esitazione; Traduzione e adattamento di Let’s talk about hesitancy; ECDC: Stockholm, Sweden, 14 January 2016. Available online: http://www.salute.gov.it/imgs/C_17_opuscoliPoster_366_allegato.pdf (accessed on 14 January 2021).
- Barrière, J.; Vanjak, D.; Kriegel, I.; Otto, J.; Peyrade, F.; Estève, M.; Chamorey, E. Acceptance of the 2009 A(H1N1) influenza vaccine among hospital workers in two French cancer centers. Vaccine 2010, 28, 7030–7034. [Google Scholar] [CrossRef] [PubMed]
- Verger, P.; Fressard, L.; Collange, F.; Gautier, A.; Jestin, C.; Launay, O.; Raude, J.; Pulcini, C.; Peretti-Watel, P. Vaccine Hesitancy Among General Practitioners and Its Determinants During Controversies: A National Cross-sectional Survey in France. EBioMedicine 2015, 2, 891–897. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Dedoukou, X.; Patrinos, S.; Maragos, A.; Poufta, S.; Gargalianos, P.; Lazanas, M. Determinants of intention to get vaccinated against novel (pandemic) influenza A H1N1 among health-care workers in a nationwide survey. J. Infect. 2010, 61, 252–258. [Google Scholar] [CrossRef]
- Johns Hopkins University Coronavirus Resource Center. COVID-19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. 2020. Available online: https://coronavirus.jhu.edu/map.html (accessed on 14 January 2021).
- Felice, C.; Di Tanna, G.L.; Zanus, G.; Grossi, U. Impact of COVID-19 Outbreak on Healthcare Workers in Italy: Results from a National E-Survey. J. Community Heal. 2020, 45, 675–683. [Google Scholar] [CrossRef]
- Reproduction number (R) and growth rate (r) of the COVID-19 epidemic in the UK: Methods of estimation, data sources, causes of heterogeneity, and use as a guide in policy formulation; The Royal Society: London, UK, 2020.
- Holzmann, H.; Wiedermann, U. Mandatory vaccination: Suited to enhance vaccination coverage in Europe? Eurosurveillance 2019, 24, 1900376. [Google Scholar] [CrossRef] [PubMed]
- Neumann-Böhme, S.; Varghese, N.E.; Sabat, I.; Barros, P.P.; Brouwer, W.; Van Exel, J.; Schreyögg, J.; Stargardt, T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur. J. Heal. Econ. 2020, 21, 977–982. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2020, 20, 1–4. [Google Scholar] [CrossRef]
- Dubé, E.; Vivion, M.; E MacDonald, N. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: Influence, impact and implications. Expert Rev. Vaccines 2015, 14, 99–117. [Google Scholar] [CrossRef]
- Trogen, B.; Oshinsky, D.; Caplan, A. Adverse Consequences of Rushing a SARS-CoV-2 Vaccine: Implications for Public Trust. JAMA 2020, 323, 2460–2461. [Google Scholar] [CrossRef]
- Rubin, E.J.; Longo, D.L. SARS-CoV-2 Vaccination—An Ounce (Actually, Much Less) of Prevention. N. Engl. J. Med. 2020, 383, 2677–2678. [Google Scholar] [CrossRef] [PubMed]
- Murri, R.; Segala, F.V.; Del Vecchio, P.; Cingolani, A.; Taddei, E.; Micheli, G.; Fantoni, M. COVID II Columbus Group. Social media as a tool for scientific updating at the time of COVID pandemic: Results from a national survey in Italy. PLoS ONE 2020, 15, e0238414. [Google Scholar] [CrossRef] [PubMed]
- Wood, S.; Schulman, K. Beyond Politics—Promoting Covid-19 Vaccination in the United States. N. Engl. J. Med. 2021, 384, e23. [Google Scholar] [CrossRef]
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Marc, G.P.; Moreira, E.D.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N. Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Total Participants (n = 1723) | Intent to Be Vaccinated | p-Value | ||
|---|---|---|---|---|---|
| No or not Sure (n = 568) | Yes (n = 1155) | ||||
| Sex (n, %) | Female | 920 (53) | 303 (33) | 617 (67) | 0.999 |
| Male | 803 (47) | 265 (33) | 538 (67) | ||
| Age group (n, %) | <30 | 762 (44) | 184 (24) | 578 (76) | <0.0001 |
| 30–40 | 527 (31) | 205 (39) | 322 (61) | ||
| 41–50 | 200 (12) | 107 (54) | 93 (47) | ||
| 51–60 | 106 (6) | 47 (44) | 59 (56) | ||
| >60 years | 128 (7) | 25 (20) | 103 (80) | ||
| Geografic Area (n, %) | Central Italy | 385 (22) | 119 (31) | 266 (69) | 0.2443 |
| Northern Italy | 622 (36) | 197 (32) | 425 (68) | ||
| Southern Italy and Islands | 716 (42) | 252 (35) | 464 (65) | ||
| Occupational profile (n, %) | Specialised Medical Doctor | 337 (20) | 103 (31) | 234 (69) | <0.0001 |
| Medical resident | 259 (15) | 55 (21) | 204 (79) | ||
| Medical Doctor | 544 (32) | 131 (24) | 413 (76) | ||
| General Practitioner | 135 (8) | 49 (37) | 85 (63) | ||
| GP trainee | 70 (4) | 16 (23) | 54 (77) | ||
| Non-MD health professional | 378 (22) | 214 (57) | 164 (43) | ||
| Area of work (n, %) | Surgical | 86 (11) | 26 (30) | 60 (70) | 0.3731 |
| Clinical | 356 (44) | 95 (27) | 261 (73) | ||
| Non-clinical | 154 (19) | 37 (24) | 117 (76) | ||
| Primary health care | 205 (26) | 65 (32) | 140 (68) | ||
| Length of service (n, %) | <10 y | 1249 (72) | 364 (29) | 885 (71) | <0.0001 |
| >10 y | 474 (28) | 204 (43) | 270 (57) | ||
| Self-perceived risk (n, %) | Previous or current SARS-CoV-2 infection | 87 (5) | 33 (38) | 54 (62) | 0.3491 |
| Previous or current SARS-CoV-2 Infection in family members or close contacts | 626 (36) | 213 (34) | 413 (66) | 0.4888 | |
| Rating self-perceived health status (mean, SD) | 8.5 (1.3) | 8.4 (1.4) | 8.68 (1.3) | - | |
| Self-perceived higher risk of contagion or bad outcome for COVID-19 due to health status | 275 (16) | 106 (19) | 169 (15) | 0.0357 | |
| People at risk between close contacts or cohabitants (n, %) | Over > 65 | 987 (57) | 299 (30) | 688 (70) | 0.0071 |
| Children < 12 | 440 (26) | 166 (38) | 274 (62) | ||
| People with disability or current serious disease | 244 (14) | 72 (30) | 172 (70) | ||
| Immunocompromised or in treatment with immunosuppressors | 220 (13) | 57 (26) | 162 (74) | ||
| Trust in Current Containment Measures (Mean, SD) | 6 (1.9) | 5.8 (1.9) | 6.07 (1.9) | - | |
| Information sources on SARS-CoV-2 vaccination (n, %) | Scientific Literature | 1202 (70) | 335 (28) | 867 (72) | <0.0001 |
| Expert opinions | 851 (49) | 275 (33) | 569 (67) | ||
| Scientific meeting | 669 (39) | 186 (28) | 485 (72) | ||
| Media | 273 (16) | 65 (24) | 208 (76) | ||
| Facebook group | 276 (16) | 120 (43) | 156 (57) | ||
| Journal and website | 382 (22) | 132 (35) | 250 (65) | ||
| Attitude towards patients recommendation (n, %) | would recomment | 1219 (71) | 17 (20) | 1046 (91) | <0.0001 |
| uncertain | 405 (24) | 32 (57) | 84 (7) | ||
| would not recommend | 99 (6) | 74 (13) | 25 (2) | ||
| Self-Reported Reasons of Vaccine Hesitancy | n (%) | |
|---|---|---|
| Safety | Fear about vaccine content | 455 (80%) |
| Fear for side effects | 482 (85%) | |
| Fear of pre-existent co-morbidities | 253 (45%) | |
| Fear of getting Covid-19 through the vaccine | 234 (41%) | |
| Information | Little information about vaccine | 441 (78%) |
| Conflicting/misleading information | 390 (69%) | |
| Trust | Low trust in control authority | 332 (58%) |
| Low trust in pharmaceutical companies | 329 (58%) | |
| Conspiracy theories | 75 (13%) | |
| Complacency | COVID-19 symptoms are mostly mild | 117 (21%) |
| Physiological immunity is better | 148 (26%) | |
| Efficacy | Small or doubted efficacy | 433 (76%) |
| Univariate Analysis * | Multivariate Analysis ° | ||||
|---|---|---|---|---|---|
| OR (95% CI) | p-Value | aOR (95%CI) | p-Value | ||
| Sex | Male | 0.99 (0.82–1.21) | 0.999 | 1.02 (0.79–1.32) | 0.19 |
| Age group | <30 y | 0.47 (0.39–0.58) | <0.0001 | 0.58 (0.41–0.83) | <0.0001 |
| Geografic Area | Northen Italy | 0.91 (0.74–1.12) | 0.3443 | 0.95 (0.73–1.24) | 0.46 |
| Occupational profile | Health Professionals | 3.65 (2.87–4.63) | <0.0001 | 1.82 (1.31–2.50) | <0.0001 |
| Area of work | Clinical | 1.454 (1.11–1.88) | 0.004 | 1.072 (0.76–1.48) | 0.06 |
| Length of service | >10 y | 1.83 (1.47–2.28) | <0.0001 | 1.32 (0.82–2.19) | 0.02 |
| Previous or current SARS-CoV-2 infection | 1.25 (0.81–1.97) | 0.3491 | 1.22 (0.68–2.13) | 0.53 | |
| Previous or current SARS-CoV-2 Infection in family members or close contacts | 1.08 (0.87–1.32) | 0.888 | 0.99 (0.76–1.29) | 0.02 | |
| Rating self-perceived health status (mean, SD) | 0.81 (0.83–1.32) | 0.03 | 0.99 (0.89–1.10) | 0.02 | |
| Information sources on SARS-CoV 2 | Facebook group | 1.71 (1.3–2.22) | <0.0001 | 1.48 (1.06–2.07) | <0.0001 |
| Seasonal flu vaccination | Flu vaccination during last season | 0.28 (0.22–0.35) | <0.0001 | 0.37 (0.29–0.48) | <0.0001 |
| Intention towards Flu vaccination for the current season | 0.66 (0.43–0.98) | <0.0001 | 0.79 (0.61–1.02) | 0.02 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Gennaro, F.; Murri, R.; Segala, F.V.; Cerruti, L.; Abdulle, A.; Saracino, A.; Bavaro, D.F.; Fantoni, M. Attitudes towards Anti-SARS-CoV2 Vaccination among Healthcare Workers: Results from a National Survey in Italy. Viruses 2021, 13, 371. https://doi.org/10.3390/v13030371
Di Gennaro F, Murri R, Segala FV, Cerruti L, Abdulle A, Saracino A, Bavaro DF, Fantoni M. Attitudes towards Anti-SARS-CoV2 Vaccination among Healthcare Workers: Results from a National Survey in Italy. Viruses. 2021; 13(3):371. https://doi.org/10.3390/v13030371
Chicago/Turabian StyleDi Gennaro, Francesco, Rita Murri, Francesco Vladimiro Segala, Lorenzo Cerruti, Amina Abdulle, Annalisa Saracino, Davide Fiore Bavaro, and Massimo Fantoni. 2021. "Attitudes towards Anti-SARS-CoV2 Vaccination among Healthcare Workers: Results from a National Survey in Italy" Viruses 13, no. 3: 371. https://doi.org/10.3390/v13030371
APA StyleDi Gennaro, F., Murri, R., Segala, F. V., Cerruti, L., Abdulle, A., Saracino, A., Bavaro, D. F., & Fantoni, M. (2021). Attitudes towards Anti-SARS-CoV2 Vaccination among Healthcare Workers: Results from a National Survey in Italy. Viruses, 13(3), 371. https://doi.org/10.3390/v13030371











