Forced Degradation Studies to Identify Critical Process Parameters for the Purification of Infectious Measles Virus
Abstract
1. Introduction
2. Materials and Methods
2.1. Virus Production and Analysis of Infectivity
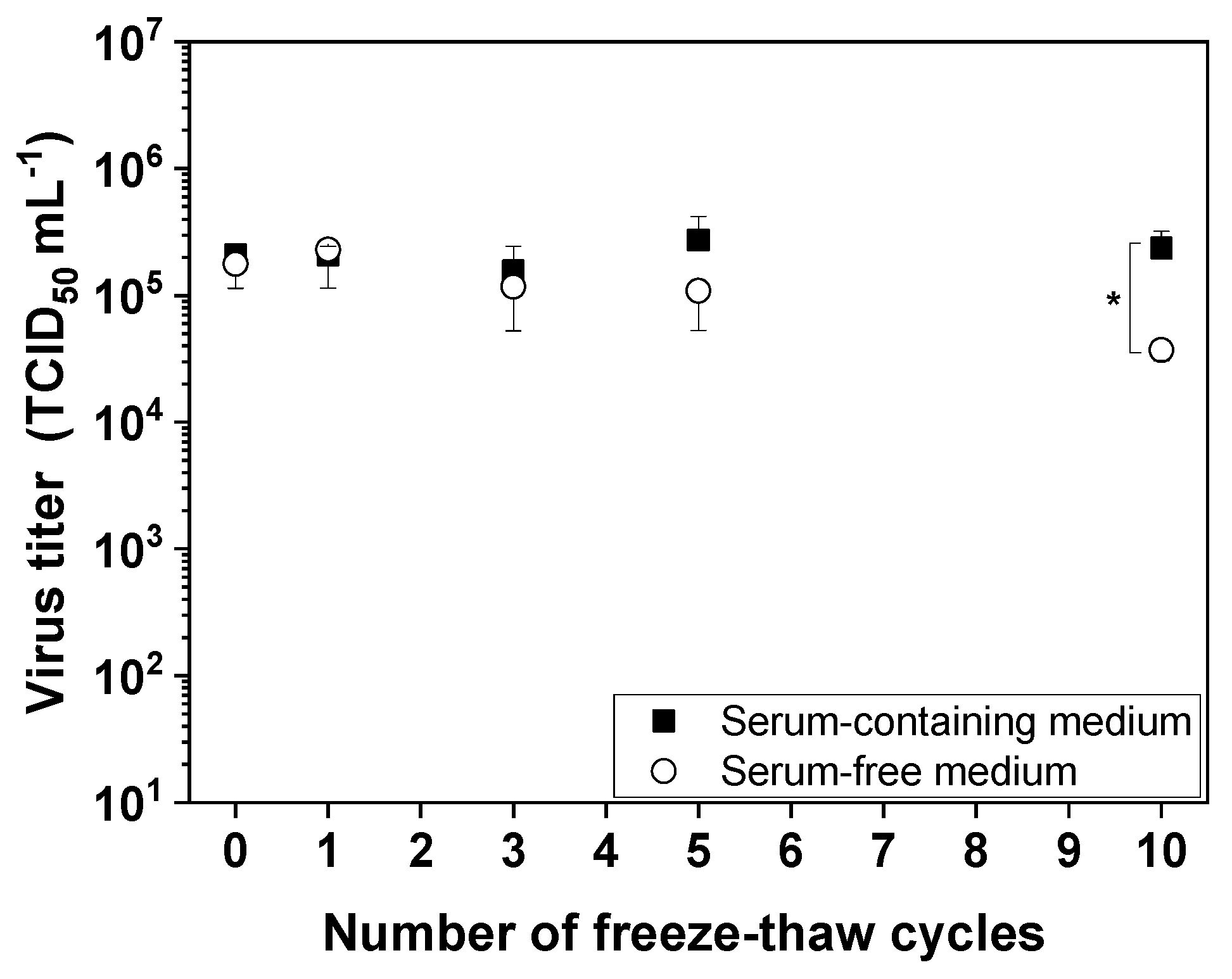
2.2. Influence of Freeze–Thaw Cycles on MV Infectivity
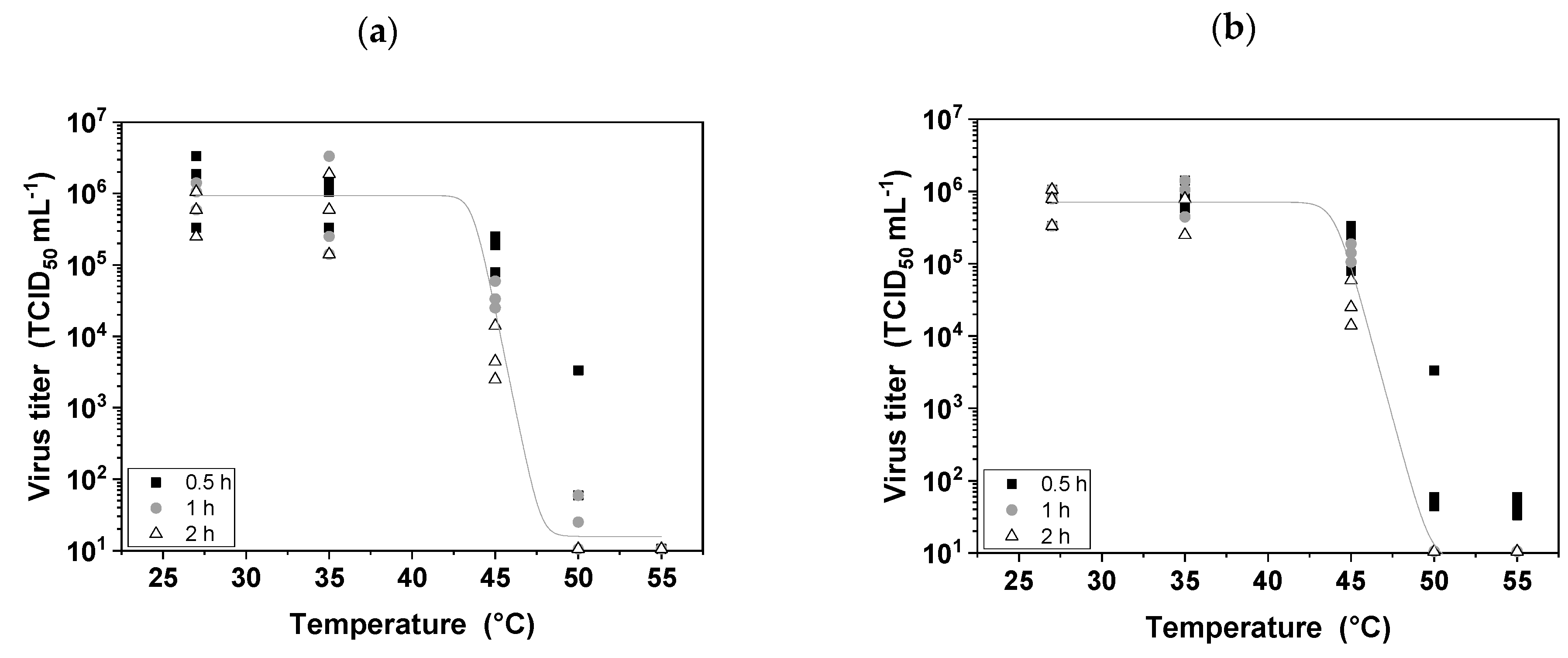
2.3. Influence of Heat on MV Infectivity
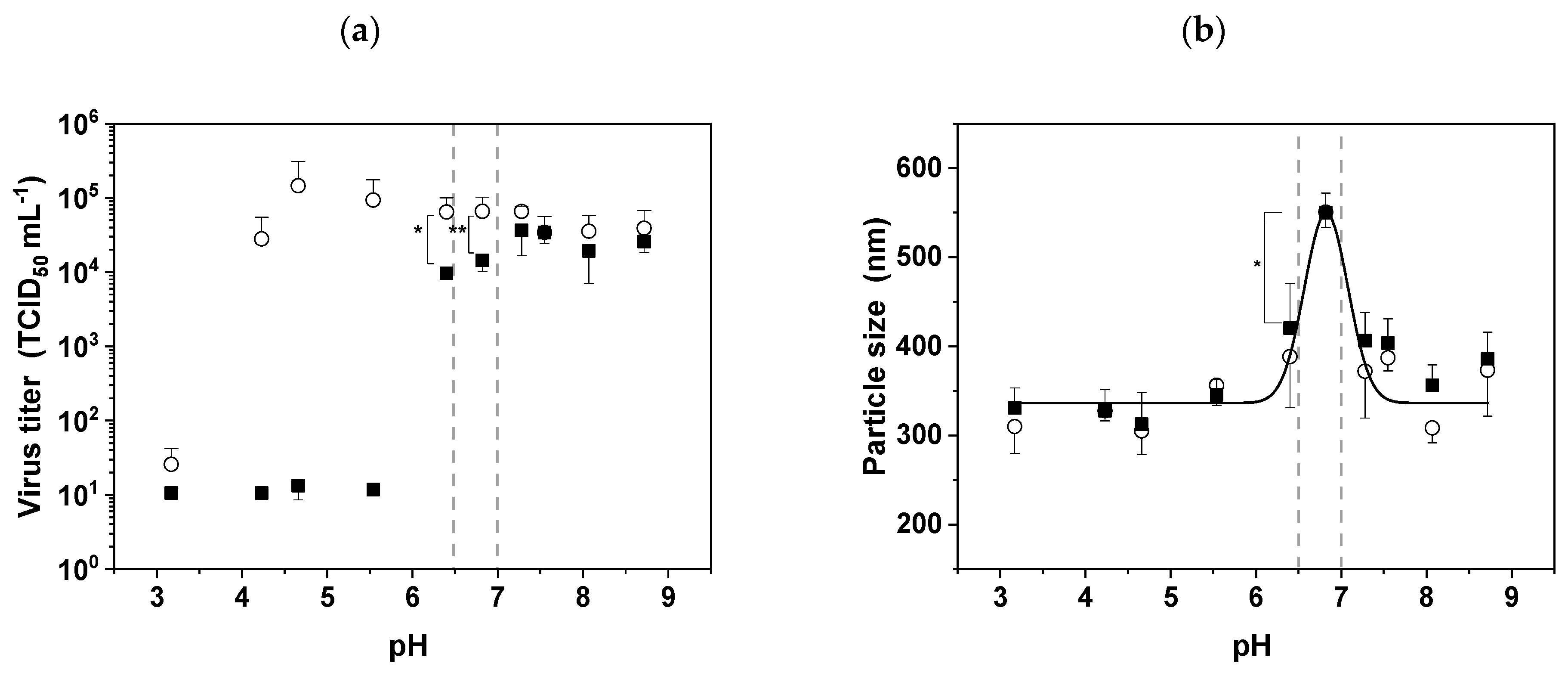
2.4. Influence of pH on MV Infectivity and Aggregation
2.5. Influence of Osmolality and Ionic Strength on MV Infectivity
2.6. Influence of Buffers and Additives on MV Infectivity
2.7. Influences of Shear Stress on MV Infectivity
2.8. Determination of the Shear Rate and Shear Stress
2.9. Statistical Analysis
3. Results
3.1. Freeze–Thaw Stress
3.2. Thermal Stress
3.3. The pI of MV and the Effect of pH Stress
3.4. Chemical Stress
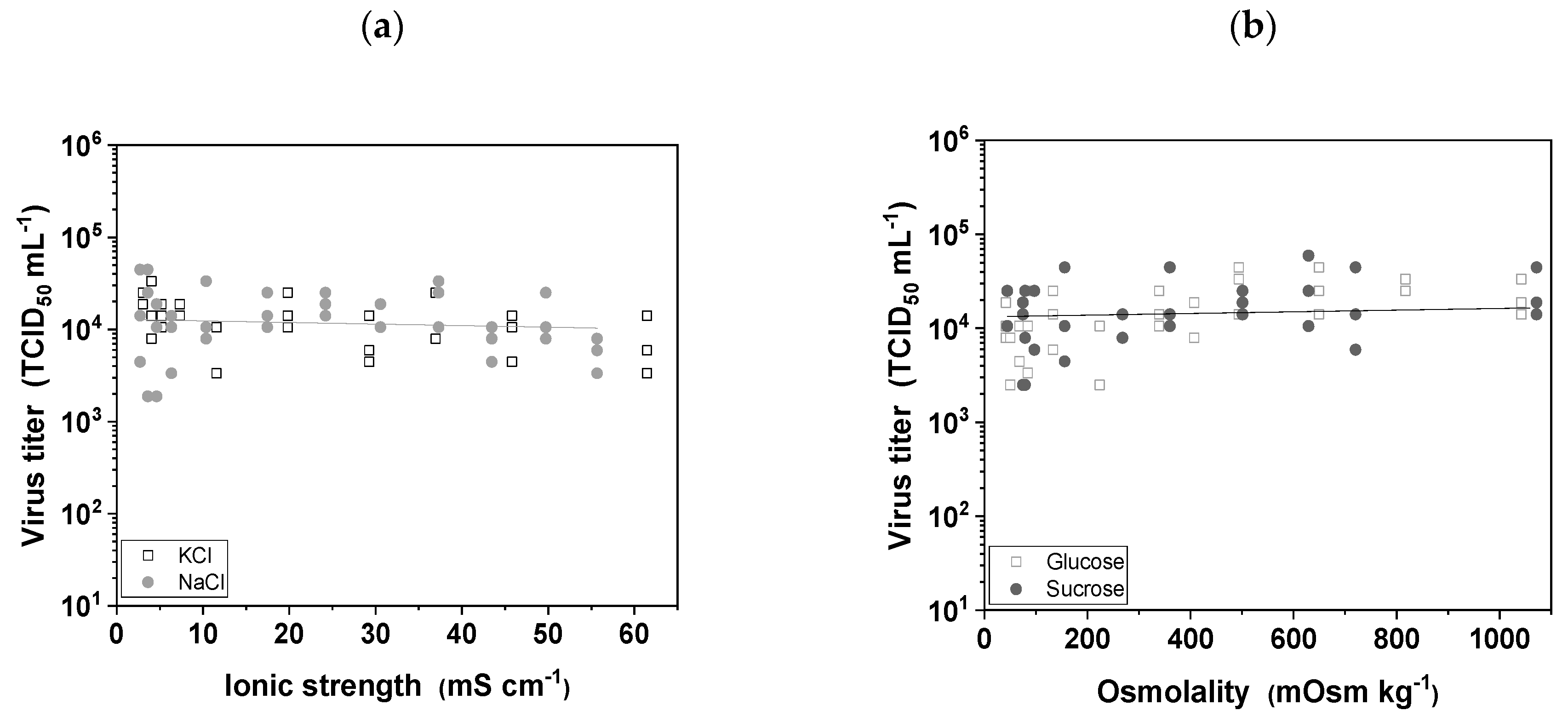
3.4.1. Buffer Ionic Strength and Osmolality
3.4.2. Buffer Components and Additives
3.5. Mechanical Stress
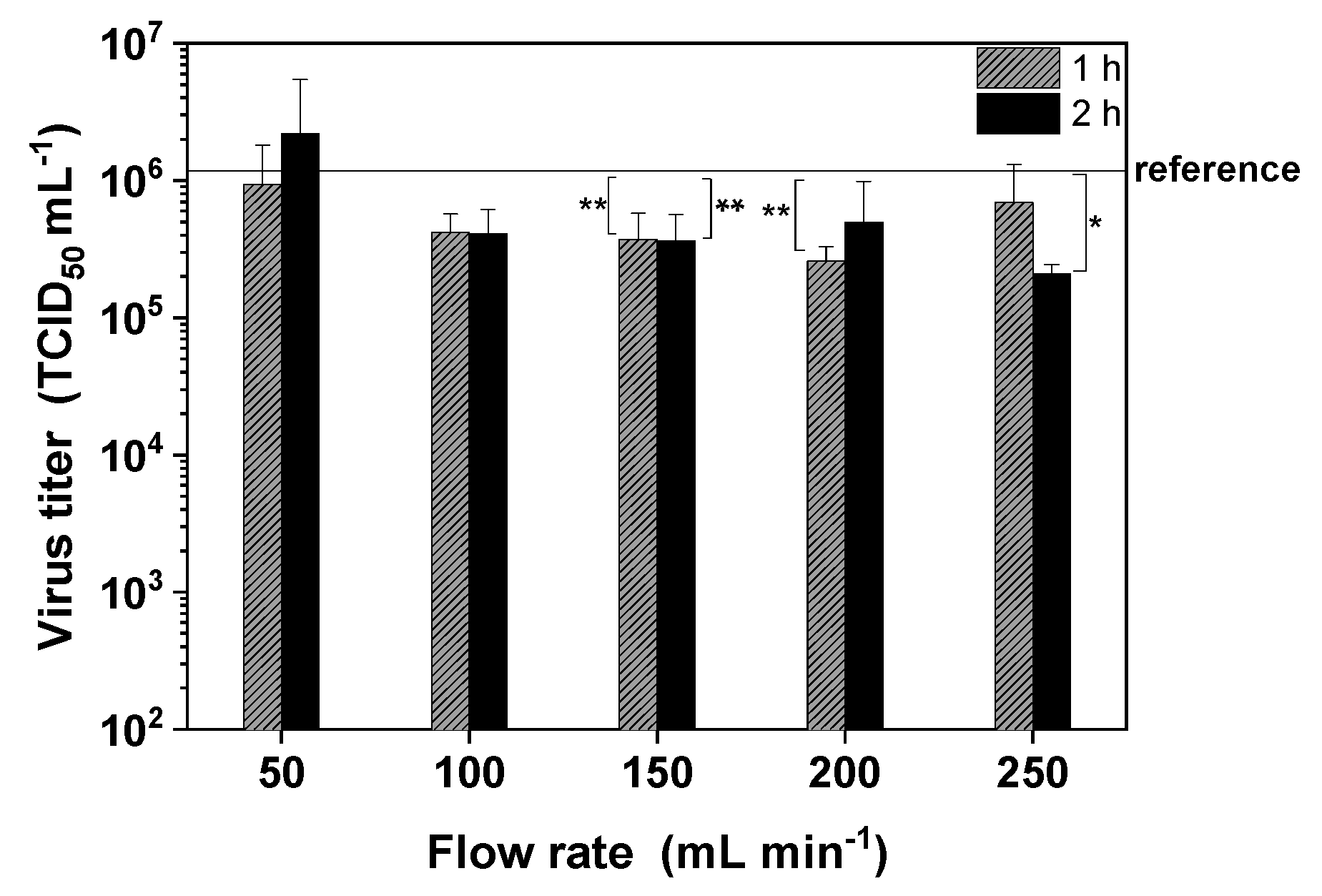
3.5.1. Shear Stress Induced by Pumping
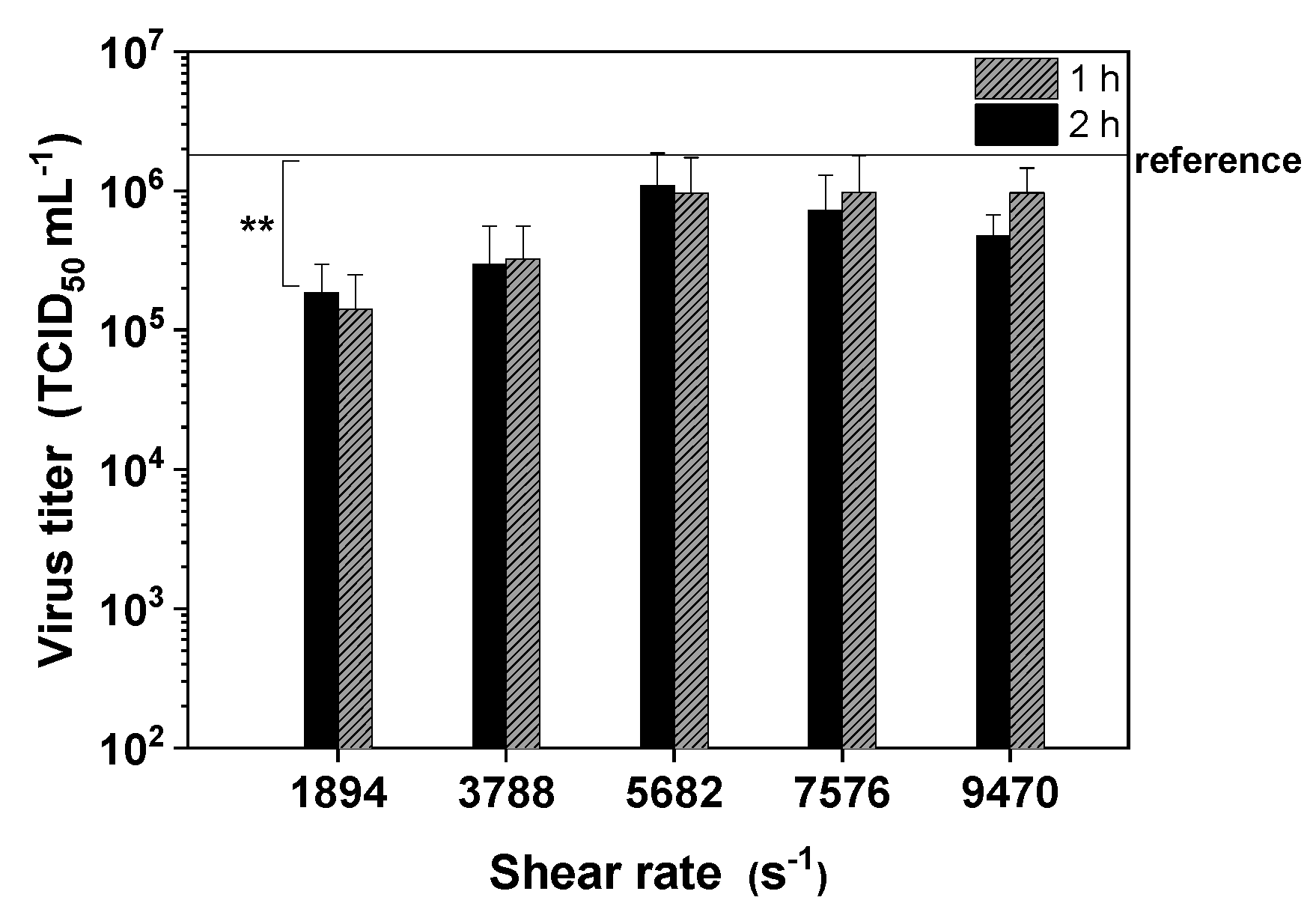
3.5.2. Shear Stress in a TFF Module
4. Discussion
4.1. Up to Five Freeze–Thaw Cycles Cause no Significant MV Inactivation Even in the Absence of Serum
4.2. MV Is Extremely Thermosensitive
4.3. The pI of MV Is ~6.8 and the Virus Is Highly Sensitive to Acidic Media
4.4. MV Tolerates a Broad Range of Buffer Types, Osmolality and Ionic Strength
4.5. Shear Stress in the Membrane Module Has a Significant Impact on Recovery Infectious MV Infectivity
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Ca Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Russell, L.; Peng, K.-W. The emerging role of oncolytic virus therapy against cancer. Chin. Clin. Oncol. 2018, 7, 16. [Google Scholar] [CrossRef] [PubMed]
- Taguchi, S.; Fukuhara, H.; Homma, Y.; Todo, T. Current status of clinical trials assessing oncolytic virus therapy for urological cancers. Int. J. Urol. 2017, 24, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Eissa, I.R.; Bustos-Villalobos, I.; Ichinose, T.; Matsumura, S.; Naoe, Y.; Miyajima, N.; Morimoto, D.; Mukoyama, N.; Zhiwen, W.; Tanaka, M.; et al. The Current Status and Future Prospects of Oncolytic Viruses in Clinical Trials against Melanoma, Glioma, Pancreatic, and Breast Cancers. Cancers 2018, 10, 356. [Google Scholar] [CrossRef] [PubMed]
- Bluming, A.Z.; Ziegler, J.L. Regression of Burkitt’s lymphoma in association with measles infection. Lancet 1971, 2, 105–106. [Google Scholar] [CrossRef]
- Russell, S.J.; Federspiel, M.J.; Peng, K.-W.; Tong, C.; Dingli, D.; Morice, W.G.; Lowe, V.; O’Connor, M.K.; Kyle, R.A.; Leung, N.; et al. Remission of disseminated cancer after systemic oncolytic virotherapy. Mayo Clin. Proc. 2014, 89, 926–933. [Google Scholar] [CrossRef] [PubMed]
- Aref, S.; Bailey, K.; Fielding, A. Measles to the Rescue: A Review of Oncolytic Measles Virus. Viruses 2016, 8, 294. [Google Scholar] [CrossRef] [PubMed]
- Langfield, K.K.; Walker, H.J.; Gregory, L.C.; Federspiel, M.J. Manufacture of measles viruses. Methods Mol. Biol. 2011, 737, 345–366. [Google Scholar] [CrossRef] [PubMed]
- Weiss, K.; Salzig, D.; Röder, Y.; Gerstenberger, J.; Mühlebach, M.D.; Cichutek, K.; Pörtner, R.; Czermak, P. Influences of Process Conditions on Measles Virus Stability. Am. J. Biochem. Biotechnol. 2013, 9, 243–254. [Google Scholar] [CrossRef][Green Version]
- Weiss, K.; Gerstenberger, J.; Salzig, D.; Mühlebach, M.D.; Cichutek, K.; Pörtner, R.; Czermak, P. Oncolytic measles viruses produced at different scales under serum-free conditions. Eng. Life Sci. 2015, 15, 425–436. [Google Scholar] [CrossRef]
- Grein, T.A.; Schwebel, F.; Kress, M.; Loewe, D.; Dieken, H.; Salzig, D.; Weidner, T.; Czermak, P. Screening different host cell lines for the dynamic production of measles virus. Biotechnol. Prog. 2017, 33, 989–997. [Google Scholar] [CrossRef] [PubMed]
- Grein, T.A.; Loewe, D.; Dieken, H.; Salzig, D.; Weidner, T.; Czermak, P. High titer oncolytic measles virus production process by integration of dielectric spectroscopy as online monitoring system. Biotechnol. Bioeng. 2018, 115, 1186–1194. [Google Scholar] [CrossRef] [PubMed]
- Grein, T.A.; Loewe, D.; Dieken, H.; Weidner, T.; Salzig, D.; Czermak, P. Aeration and Shear Stress are Critical Process Parameters for the Production of Oncolytic Measles Virus. Front. Bioeng. Biotechnol. 2019. accepted. [Google Scholar] [CrossRef] [PubMed]
- Firquet, S.; Beaujard, S.; Lobert, P.-E.; Sané, F.; Caloone, D.; Izard, D.; Hober, D. Survival of Enveloped and Non-Enveloped Viruses on Inanimate Surfaces. Microbes Environ. 2015, 30, 140–144. [Google Scholar] [CrossRef] [PubMed]
- Fraise, A.P.; Maillard, J.-Y.; Sattar, S. Russell, Hugo & Ayliffe’s Principles and Practice of Disinfection, Preservation, and Sterilization, 5th ed.; Wiley-Blackwell: Chichester, UK, 2013; ISBN 9781299158573. [Google Scholar]
- Schaechter, M. Encyclopedia of Microbiology, 3rd ed.; Schaechter, M., Ed.; Elsevier: Amsterdam, The Netherland, 2009; ISBN 9780123739391. [Google Scholar]
- Hansen, L.J.J.; Daoussi, R.; Vervaet, C.; Remon, J.-P.; de Beer, T.R.M. Freeze-drying of live virus vaccines: A review. Vaccine 2015, 33, 5507–5519. [Google Scholar] [CrossRef] [PubMed]
- Sviben, D.; Forcic, D.; Ivancic-Jelecki, J.; Halassy, B.; Brgles, M. Recovery of infective virus particles in ion-exchange and hydrophobic interaction monolith chromatography is influenced by particle charge and total-to-infective particle ratio. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2017, 1054, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Hasija, M.; Li, L.; Rahman, N.; Ausar, S.F. Forced degradation studies: An essential tool for the formulation development of vaccines. VDT 2013, 11. [Google Scholar] [CrossRef]
- Food and Drug Administration. International Conference on Harmonisation. Guidance on Q11 Development and Manufacture of Drug Substances; availability. Notice. Fed. Regist. 2012, 77, 69634–69635. [Google Scholar]
- Pramod, K.; Tahir, M.A.; Charoo, N.A.; Ansari, S.H.; Ali, J. Pharmaceutical product development: A quality by design approach. Int. J. Pharm. Investig. 2016, 6, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.P. Forced degradation studies: Current trends and future perspectives for protein-based therapeutics. Expert Rev. Proteom. 2016, 13, 651–658. [Google Scholar] [CrossRef]
- Kärber, G. Beitrag zur kollektiven Behandlung pharmakologischer Reihenversuche. Arch. F. Exp. Pathol. Pharmakol. 1931, 162, 480–483. [Google Scholar] [CrossRef]
- Reed, L.J.; Muench, H. A simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 1938, 27, 493–497. [Google Scholar] [CrossRef]
- Navaratnarajah, C.K.; Kumar, S.; Generous, A.; Apte-Sengupta, S.; Mateo, M.; Cattaneo, R. The measles virus hemagglutinin stalk: Structures and functions of the central fusion activation and membrane-proximal segments. J. Virol. 2014, 88, 6158–6167. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kozlowski, L.P. IPC—Isoelectric Point Calculator. Biol. Direct 2016, 11, 55. [Google Scholar] [CrossRef] [PubMed]
- Wickramasinghe, S.R.; Kalbfuss, B.; Zimmermann, A.; Thom, V.; Reichl, U. Tangential flow microfiltration and ultrafiltration for human influenza A virus concentration and purification. Biotechnol. Bioeng. 2005, 92, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Mahler, H.-C.; Friess, W.; Grauschopf, U.; Kiese, S. Protein aggregation: Pathways, induction factors and analysis. J. Pharm. Sci. 2009, 98, 2909–2934. [Google Scholar] [CrossRef] [PubMed]
- Lashmar, U.T.; Vanderburgh, M.; Little, S.J. Bulk Freeze–Thawing of Macromolecules. BioProcess Int. 2007, 44–54. [Google Scholar]
- Pikal-Cleland, K.A.; Cleland, J.L.; Anchordoquy, T.J.; Carpenter, J.F. Effect of glycine on pH changes and protein stability during freeze–thawing in phosphate buffer systems. J. Pharm. Sci. 2002, 91, 1969–1979. [Google Scholar] [CrossRef]
- Cao, E.; Chen, Y.; Cui, Z.; Foster, P.R. Effect of freezing and thawing rates on denaturation of proteins in aqueous solutions. Biotechnol. Bioeng. 2003, 82, 684–690. [Google Scholar] [CrossRef]
- Kissmann, J.; Ausar, S.F.; Rudolph, A.; Braun, C.; Cape, S.P.; Sievers, R.E.; Federspiel, M.J.; Joshi, S.B.; Middaugh, C.R. Stabilization of measles virus for vaccine formulation. Hum. Vaccines 2014, 4, 350–359. [Google Scholar] [CrossRef]
- Kim, S.-G.; Ran, G.S.; Kwon, H.-C.; Hwang, T.-H. Effect of NaCl on the Stability of Oncolytic Vaccinia Virus. J. Life Sci. 2016, 26, 23–33. [Google Scholar] [CrossRef][Green Version]
- Greiff, D.; Blumenthal, H.; Chiga, M.; Pinkerton, H. The effects on biological materials of freezing and drying by vacuum sublimation: II. Effect on Influenza virus. J. Exp. Med. 1954, 100, 89–101. [Google Scholar] [CrossRef]
- Ghobadloo, S.M.; Gargaun, A.; Casselman, R.; Muharemagic, D.; Berezovski, M.V. Aptamer-facilitated cryoprotection of viruses. Acs Med. Chem. Lett. 2014, 5, 1240–1244. [Google Scholar] [CrossRef]
- Black, F.L. Growth and stability of measles virus. Virology 1959, 7, 184–192. [Google Scholar] [CrossRef]
- Arita, M.; Matumoto, M. Heat Inactivation of Measles Virus. Jpn. J. Microbiol. 1968, 12, 121–122. [Google Scholar] [CrossRef]
- Michalsky, R.; Pfromm, P.H.; Czermak, P.; Sorensen, C.M.; Passarelli, A.L. Effects of temperature and shear force on infectivity of the baculovirus Autographa californica M nucleopolyhedrovirus. J. Virol. Methods 2008, 153, 90–96. [Google Scholar] [CrossRef]
- Scholtissek, C. Stability of infectious influenza A viruses at low pH and at elevated temperature. Vaccine 1985, 3, 215–218. [Google Scholar] [CrossRef]
- Grein, T.A.; Michalsky, R.; Vega López, M.; Czermak, P. Purification of a recombinant baculovirus of Autographa californica M nucleopolyhedrovirus by ion exchange membrane chromatography. J. Virol. Methods 2012, 183, 117–124. [Google Scholar] [CrossRef]
- Polson, A.; Turner, G.S. pH stability and purification of lumpy skin disease virus. J. Gen. Microbiol. 1954, 11, 228–235. [Google Scholar] [CrossRef][Green Version]
- Herzer, S.; Beckett, P.; Wegman, T.; Moore, P. Isoelectric titration curves of viral particles as an evaluation tool for ion exchange chromatography. Life Sci. News 2003, 13. [Google Scholar]
- Michen, B.; Graule, T. Isoelectric points of viruses. J. Appl. Microbiol. 2010, 109, 388–397. [Google Scholar] [CrossRef]
- Wolff, M.W.; Reichl, U. Downstream processing of cell culture-derived virus particles. Expert Rev. Vaccines 2011, 10, 1451–1475. [Google Scholar] [CrossRef]
- Brakke, M.K. Stability of purified barley stripe mosaic virus. Virology 1962, 17, 131–142. [Google Scholar] [CrossRef]
- Williams, A.; Frasca, V. Ion-exchange chromatography. Curr. Protoc. Protein Sci. 2001, 15. [Google Scholar] [CrossRef]
- Rapp, F.; Butel, J.S.; Wallis, C. Protection of Measles Virus by Sulfate Ions against Thermal Inactivation. J. Bacteriol. 1965, 90, 132–135. [Google Scholar]
- Sviben, D.; Forčić, D.; Kurtović, T.; Halassy, B.; Brgles, M. Stability, biophysical properties and effect of ultracentrifugation and diafiltration on measles virus and mumps virus. Arch. Virol. 2016, 161, 1455–1467. [Google Scholar] [CrossRef]
- Arakawa, T.; Ejima, D.; Tsumoto, K.; Obeyama, N.; Tanaka, Y.; Kita, Y.; Timasheff, S.N. Suppression of protein interactions by arginine: A proposed mechanism of the arginine effects. Biophys. Chem. 2007, 127, 1–8. [Google Scholar] [CrossRef]
- Arakawa, T.; Tsumoto, K.; Nagase, K.; Ejima, D. The effects of arginine on protein binding and elution in hydrophobic interaction and ion-exchange chromatography. Protein Expr. Purif. 2007, 54, 110–116. [Google Scholar] [CrossRef]
- Lange, C.; Rudolph, R. Suppression of protein aggregation by L-arginine. Curr. Pharm. Biotechnol. 2009, 10, 408–414. [Google Scholar] [CrossRef]
- Mulholland, J.W.; Shelton, J.C.; Luo, X.Y. Blood flow and damage by the roller pumps during cardiopulmonary bypass. J. Fluids Struct. 2005, 20, 129–140. [Google Scholar] [CrossRef]
- Michalsky, R.; Passarelli, A.L.; Pfromm, P.H.; Czermak, P. Concentration of the baculovirus Autographa californica M nucleopolyhedrovirus (AcMNPV) by ultrafiltration. Desalination 2010, 250, 1125–1127. [Google Scholar] [CrossRef]
| Protein | Domain | Length (Amino Acids) | Theoretical (Average) pI |
|---|---|---|---|
| Fusion (P69353.1) | Extracellular | 471 | 7.4 |
| Hemagglutinin (P08362.1) | Extracellular | 559 | 6.2 |
| Buffer | Concentration (mM) | Log10 TCID50 mL−1 |
|---|---|---|
| PBS (reference) | 5.69 ± 0.19 | |
| Tris | 20 | 5.44 ± 0.07 |
| 100 | 5.69 ± 0.26 | |
| HEPES | 20 | 5.73 ± 0.26 |
| 100 | 5.65 ± 0.13 | |
| Phosphate buffer | 20 | 5.61 ± 0.19 |
| 100 | 5.44 ± 0.14 | |
| Citrate-phosphate buffer | 20 | 5.48 ± 0.07 |
| 100 | 5.48 ± 0.14 |
| Additive | Concentration (M) | Log10 TCID50 mL−1 |
|---|---|---|
| NaCl | 0.5 | 5.4 ± 0.1 |
| 1 | 5.5 ± 0.1 | |
| 2 | 5.8 ± 0.2 | |
| CaCl2 | 0.375 | 5.7 ± 0.3 |
| 0.75 | 5.0 ± 0.1 * | |
| 1.5 | 2.0 ± 0.1 * | |
| MgSO4 | 0.375 | 5.8 ± 0.4 |
| 0.75 | 5.0 ± 0.3 * | |
| 1.5 | 4.6 ± 0.1 * | |
| L-Arginine | 0.1 | 5.6 ± 0.1 |
| 0.2 | 5.4 ± 0.1 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Loewe, D.; Häussler, J.; Grein, T.A.; Dieken, H.; Weidner, T.; Salzig, D.; Czermak, P. Forced Degradation Studies to Identify Critical Process Parameters for the Purification of Infectious Measles Virus. Viruses 2019, 11, 725. https://doi.org/10.3390/v11080725
Loewe D, Häussler J, Grein TA, Dieken H, Weidner T, Salzig D, Czermak P. Forced Degradation Studies to Identify Critical Process Parameters for the Purification of Infectious Measles Virus. Viruses. 2019; 11(8):725. https://doi.org/10.3390/v11080725
Chicago/Turabian StyleLoewe, Daniel, Julian Häussler, Tanja A. Grein, Hauke Dieken, Tobias Weidner, Denise Salzig, and Peter Czermak. 2019. "Forced Degradation Studies to Identify Critical Process Parameters for the Purification of Infectious Measles Virus" Viruses 11, no. 8: 725. https://doi.org/10.3390/v11080725
APA StyleLoewe, D., Häussler, J., Grein, T. A., Dieken, H., Weidner, T., Salzig, D., & Czermak, P. (2019). Forced Degradation Studies to Identify Critical Process Parameters for the Purification of Infectious Measles Virus. Viruses, 11(8), 725. https://doi.org/10.3390/v11080725