Comparative Pathogenicity and Transmissibility of the H7N9 Highly Pathogenic Avian Influenza Virus and the H7N9 Low Pathogenic Avian Influenza Virus in Chickens
Abstract
:1. Introduction
2. Materials and Methods
2.1. Viruses
2.2. Animal Experiment Design
2.3. Collection of Tissues and Swab Specimens from Chickens
2.4. Ethics Statements
3. Results
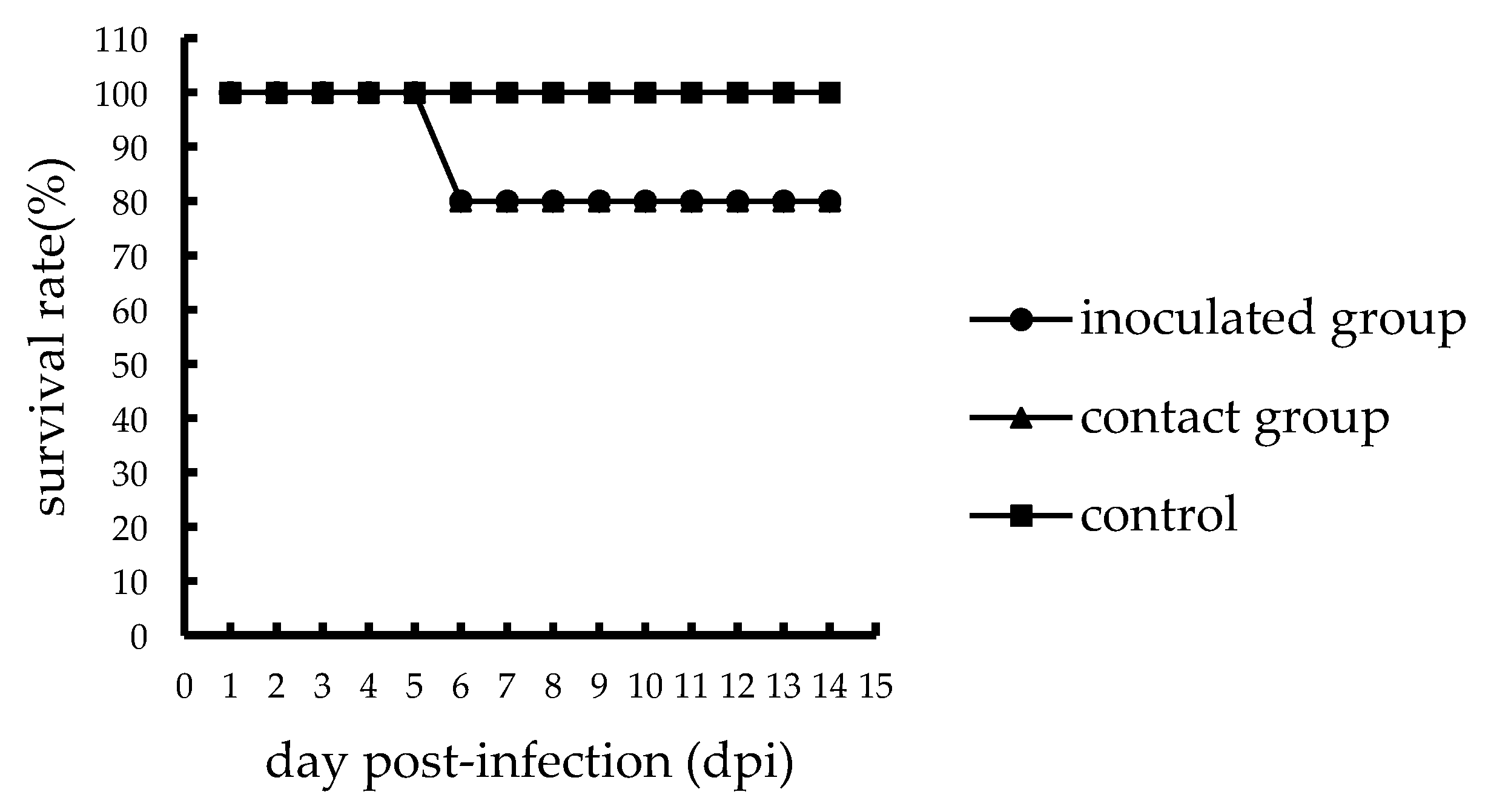
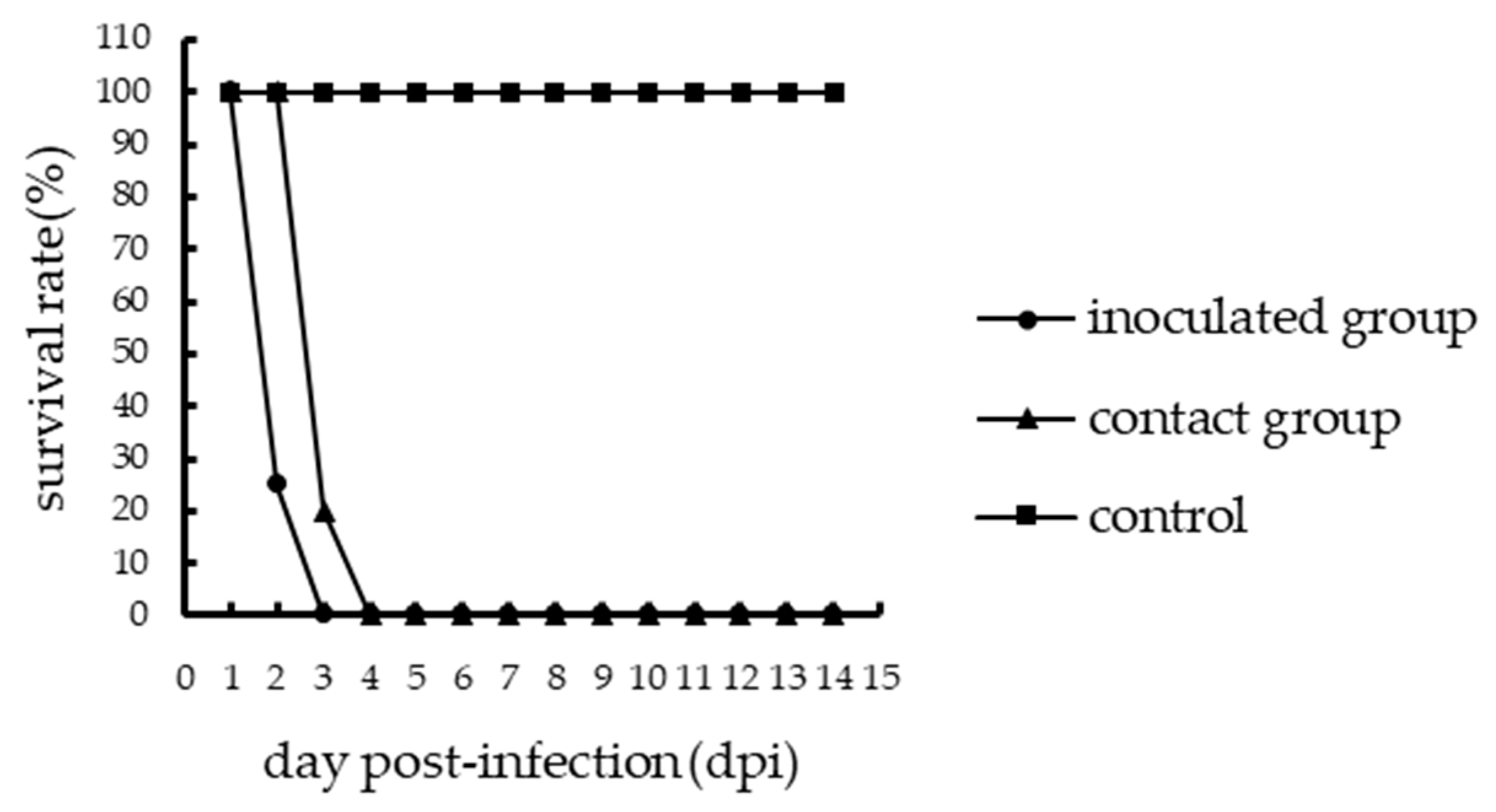
3.1. Pathogenicity of H7N9 AIVs in Chickens
3.2. Viruses Shedding from the Inoculated Chickens
3.3. Transmission of H7N9 AIVs in Chickens
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Webster, R.G.; Bean, W.J.; Gorman, O.T.; Chambers, T.M.; Kawaoka, Y. Evolution and ecology of influenza A viruses. Microbiol. Rev. 1992, 56, 152–179. [Google Scholar]
- Palese, P.; Shaw, M.L. Orthomyxoviridae: The viruses and their replication. In Fields Virology, 5th ed.; Knipe, D.M., Howley, P.M., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2007; pp. 1647–1689. [Google Scholar]
- Fouchier, R.A.; Munster, V.J. Epidemiology of low pathogenic avian influenza viruses in wild birds. Rev. Sci. Tech. 2009, 28, 49–58. [Google Scholar] [CrossRef] [Green Version]
- Kaleta, E.F.; Hergarten, G.; Yilmaz, A. Avian influenza A viruses in birds—An ecological, ornithological and virological view. Dtsch. Tierarztl. Wochenschr. 2005, 112, 448–456. [Google Scholar] [PubMed]
- Olsen, B.; Munster, V.J.; Wallensten, A.; Waldenstrom, J.; Osterhaus, A.D.; Fouchier, R.A. Global patterns of influenza a virus in wild birds. Science 2006, 312, 384–388. [Google Scholar] [CrossRef] [PubMed]
- Stein, R.A. H7N9 influenza: Something old, something new. Int. J. Clin. Pract. 2013, 67, 935–938. [Google Scholar] [CrossRef] [PubMed]
- Mei, Z.; Lu, S.; Wu, X.; Shao, L.; Hui, Y.; Wang, J.; Li, T.; Zhang, H.; Wang, X.; Yang, F.; et al. Avian influenza A(H7N9) virus infections, Shanghai, China. Emerg. Infect. Dis. 2013, 19, 1179–1181. [Google Scholar] [CrossRef] [PubMed]
- Lam, T.T.; Zhou, B.; Wang, J.; Chai, Y.; Shen, Y.; Chen, X.; Ma, C.; Hong, W.; Chen, Y.; Zhang, Y.; et al. Dissemination, divergence and establishment of H7N9 influenza viruses in China. Nature 2015, 522, 102–105. [Google Scholar] [CrossRef] [PubMed]
- Avian and Other Zoonotic Influenza. Available online: https://www.who.int/influenza/human_animal_interface/Influenza_Summary_IRA_HA_interface_16December13.pdf?ua=1 (accessed on 10 December 2013).
- Zeng, X.; Tian, G.; Shi, J.; Deng, G.; Li, C.; Chen, H. Vaccination of poultry successfully eliminated human infection with H7N9 virus in China. Sci. Chin. Life Sci. 2018, 61, 1465–1473. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Deng, G.; Liu, P.; Zhou, J.; Guan, L.; Li, W.; Li, X.; Guo, J.; Wang, G.; Fan, J.; et al. Isolation and characterization of H7N9 viruses from live poultry markets—Implication of the source of current H7N9 infection in humans. Chin. Sci. Bull. 2013, 58, 1857–1863. [Google Scholar] [CrossRef]
- Zhang, Q.; Shi, J.; Deng, G.; Guo, J.; Zeng, X.; He, X.; Kong, H.; Gu, C.; Li, X.; Liu, J.; et al. H7N9 influenza viruses are transmissible in ferrets by respiratory droplet. Science 2013, 341, 410–414. [Google Scholar] [CrossRef]
- Yang, L.; Zhu, W.; Li, X.; Chen, M.; Wu, J.; Yu, P.; Qi, S.; Huang, Y.; Shi, W.; Dong, J.; et al. Genesis and Spread of Newly Emerged Highly Pathogenic H7N9 Avian Viruses in Mainland China. J. Virol. 2017, 91, e01277–e01317. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Yang, L.; Zhu, W.; Zhang, Y.; Zou, S.; Bo, H.; Gao, R.; Dong, J.; Huang, W.; Guo, J.; et al. Two Outbreak Sources of Influenza A (H7N9) Viruses Have Been Established in China. J. Virol. 2016, 90, 5561–5573. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, N.; Sun, M.; Wang, W.; Ouyang, G.; Chen, Z.; Zhang, Y.; Zhao, B.; Wu, S.; Huang, J.; Sun, H.; et al. Avian Influenza (H7N9) Viruses Co-circulating among Chickens, Southern China. Emerg Infect. Dis. 2017, 23, 2000–2102. [Google Scholar] [CrossRef] [PubMed]
- Avian Influenza Portal. Available online: http://www.oie.int/en/animal-health-in-the-world/avian-influenza portal (accessed on 26 March 2019).
- Avian and Other Zoonotic Influenza. Available online: https://www.who.int/influenza/human_animal_interface/Influenza_Summary_IRA_HA_interface_24_06_2019.pdf?ua=1 (accessed on 24 June 2019).
- Jiao, P.; Wei, L.; Song, Y.; Cui, J.; Song, H.; Cao, L.; Yuan, R.; Luo, K.; Liao, M. D701N mutation in the PB2 protein contributes to the pathogenicity of H5N1 avian influenza viruses but not transmissibility in guinea pigs. Front. Microbiol. 2014, 5, 642. [Google Scholar] [CrossRef]
- Yuan, R.; Cui, J.; Zhang, S.; Cao, L.; Liu, X.; Kang, Y.; Song, Y.; Gong, L.; Jiao, P.; Liao, M. Pathogenicity and transmission of H5N1 avian influenza viruses in different birds. Vet. Microbiol. 2014, 168, 50–59. [Google Scholar] [CrossRef]
- Chen, H.; Deng, G.; Li, Z.; Tian, G.; Li, Y.; Jiao, P.; Zhang, L.; Liu, Z.; Webster, R.G.; Yu, K.; et al. Evolution of H5N1 influenza viruses in ducks in southern China. Proc. Natl. Acad. Sci. USA 2004, 101, 10452–10457. [Google Scholar] [CrossRef]
- Li, Z.; Jiang, Y.; Jiao, P.; Wang, A.; Zhao, F.; Tian, G.; Wang, X.; Yu, K.; Bu, Z.; Chen, H. The NS1 Gene Contributes to the Virulence of H5N1 Avian Influenza Viruses. J. Virol. 2006, 80, 11115–11123. [Google Scholar] [CrossRef] [Green Version]
- Reed, L.E.L.; Muench, H. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 1938, 27, 493–497. [Google Scholar]
- Avian and Other Zoonotic Influenza. Available online: https://www.who.int/influenza/human_animal_interface/Influenza_Summary_IRA_HA_interface_06_13_2016.pdf?ua=1 (accessed on 13 June 2016).
- Keun, B.K.; Eun, H.P.; Jung, Y.; Heui, M.K.; Young, M.K.; Jeong, C.K.; Ji, A.K.; Hyun, S.K.; Sang, H.S. Transmissibility of novel H7N9 and H9N2 avian influenza viruses between chickens and ferrets. Virology 2014, 450, 316–323. [Google Scholar]
- Pantin-Jackwood, M.J.; Miller, P.J.; Spackman, E.; Swayne, D.E.; Susta, L.; Costa-Hurtado, M.; Suarez, D.L. Role of poultry in the spread of novel H7N9 influenza virus in China. J. Virol. 2014, 88, 5381–5390. [Google Scholar] [CrossRef]
- Roy, C.I.; Yeddula, S.G.R.; Kim, S.H. Pathogenicity and Transmissibility of North American H7 Low Pathogenic Avian Influenza Viruses in Chickens and Turkeys. Viruses 2019, 11, 163. [Google Scholar] [Green Version]
- Post, J.; de Geus, E.D.; Vervelde, L.; Cornelissen, J.B.; Rebel, J.M. Systemic distribution of different low pathogenic avian influenza (LPAI) viruses in chicken. Virol. J. 2013, 10, 23. [Google Scholar] [CrossRef] [PubMed]
- Jiao, P.; Song, Y.; Huang, J.; Xiang, C.; Cui, J.; Wu, S.; Qu, N.; Wang, N.; Ouyang, G.; Liao, M. H7N9 Avian Influenza Virus Is Efficiently Transmissible and Induces an Antibody Response in Chickens. Front. Immunol. 2018, 9, 789. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Deng, G.; Kong, H.; Gu, C.; Ma, S.; Yin, X.; Zeng, X.; Cui, P.; Chen, Y.; Yang, H.; et al. H7N9 virulent mutants detected in chickens in China pose an increased threat to humans. Cell Res. 2017, 27, 1409–1421. [Google Scholar] [CrossRef] [Green Version]
- Kalthoff, D.; Bogs, J.; Grund, C.; Tauscher, K.; Teifke, J.P.; Starick, E.; Harder, T.; Beer, M. Avian influenza H7N9/13 and H7N7/13: A comparative virulence study in chickens, pigeons, and ferrets. J. Virol. 2014, 88, 9153–9165. [Google Scholar] [CrossRef]
- Vidaña, B.; Dolz, R.; Busquets, N.; Ramis, A.; Sánchez, R.; Rivas, R.; Valle, R.; Cordón, I.; Solanes, D.; Martínez, J.; et al. Transmission and immunopathology of the avian influenza virus A/Anhui/1/2013 (H7N9) human isolate in three commonly commercialized avian species. Zoonoses Public Health 2018, 65, 312–321. [Google Scholar] [CrossRef]
- Spackman, E.; Pantin-Jackwood, M.; Swayne, D.E.; Suarez, D.L.; Kapczynski, D.R. Impact of route of exposure and challenge dose on the pathogenesis of H7N9 low pathogenicity avian influenza virus in chickens. Virology 2015, 477, 72–81. [Google Scholar] [CrossRef] [Green Version]
| Strains | Titer (log10EID50) | Time d | Virus Replication (log10EID50/0.1mL) c in | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Brain | Kidneys | Livers | Lungs | Spleen | Trachea | Ileum | Bursa of Fabricius | Pancreas | |||
| A46 | 8 | 1 dpi | <1.5 | 2.08 ± 0.29 | 1.58 ± 0.14 | 3.17 ± 1.38 | <1.5 | 3 ± 1.3 | <1.5 | <1.5 | 1.67 ± 0.14 |
| 3 dpi | 2 ± 0.43 | 3.5 ± 1.73 | 1.83 ± 0.38 | 4.92 ± 1.61 | 1.75 ± 0.43 | 4.08 ± 0.72 | 2.83 ± 2.31 | 2.5 ± 1 | 2.08 ± 1.01 | ||
| Q29 | 8.32 | 1 dpi | 5.67 ± 0.72 e | 6.58 ± 1.04 e | 4.25 ± 0.5 e | 6.42 ± 0.76 f | <1.5 | 5.25 ± 1 | 5.08 ± 0.76 e | 4.33 ± 0.52 e | <1.5 |
| 3 dpi | 7.5 ± 0.75 e | 8.25 ± 1.56 f | 7.25 ± 0.5 e | 8.17 ± 1.15 f | 4.75 ± 0.66 e | 6.67 ± 1.01 f | 3.75 ± 1.56 | 6.83 ± 0.58 e | 5.58 ± 0.88 f | ||
| Days Post-Inoculation (log10EID50/0.1mL) ± SD a | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Host | Strains | 11 dpi f | 3 dpi | 5 dpi | 7 dpi | 9 dpi | 11 dpi | 13 dpi | ||||||||
| Oro e | Clo e | Oro. | Clo. | Oro. | Clo. | Oro. | Clo. | Oro. | Clo. | Oro. | Clo. | Oro. | Clo. | |||
| CK d | A46 | Ino b | 2.22 ± 0.57 | 2.38 ± 0.18 | 2.06 ± 0.38 | 3.75 | 2.33 ± 0.14 | 2.13 ± 0.53 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 |
| 8/11 | 2/11 | 4/8 | 1/8 | 3/5 | 2/5 | |||||||||||
| Con c | 0/5 | 0/5 | 1.75 | 1.75 | 2.0 ± 0.35 | 3.5 | 2.5 | 2.5 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | ||
| 1/5 | 1/5 | 2/5 | 1/5 | 1/4 | 1/4 | |||||||||||
| Q29 | Ino. | 2.38 ± 0.18 | 2.21 ± 0.25 | 2.88 ± 0.53 | 3.13 ± 0.53 | - | - | - | - | - | - | - | - | - | - | |
| 2/11 | 6/11 | 2/2 | 2/2 | |||||||||||||
| Con. | 0/5 | 0/5 | 2.56 ± 0.24 | 5.38 ± 0.18 | - | - | - | - | - | - | - | - | - | - | ||
| 4/5 | 2/5 | |||||||||||||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, H.; Zhang, K.; Ye, X.; Wang, W.; Wu, W.; Wang, X.; Guan, Y.; He, Z.; Wang, Y.; Jiao, P. Comparative Pathogenicity and Transmissibility of the H7N9 Highly Pathogenic Avian Influenza Virus and the H7N9 Low Pathogenic Avian Influenza Virus in Chickens. Viruses 2019, 11, 1047. https://doi.org/10.3390/v11111047
Yu H, Zhang K, Ye X, Wang W, Wu W, Wang X, Guan Y, He Z, Wang Y, Jiao P. Comparative Pathogenicity and Transmissibility of the H7N9 Highly Pathogenic Avian Influenza Virus and the H7N9 Low Pathogenic Avian Influenza Virus in Chickens. Viruses. 2019; 11(11):1047. https://doi.org/10.3390/v11111047
Chicago/Turabian StyleYu, Hao, Kunpeng Zhang, Xumeng Ye, Wenqing Wang, Wenbo Wu, Xia Wang, Yun Guan, Zhuoliang He, Yong Wang, and Peirong Jiao. 2019. "Comparative Pathogenicity and Transmissibility of the H7N9 Highly Pathogenic Avian Influenza Virus and the H7N9 Low Pathogenic Avian Influenza Virus in Chickens" Viruses 11, no. 11: 1047. https://doi.org/10.3390/v11111047




