Bone Replacement Materials and Techniques Used for Achieving Vertical Alveolar Bone Augmentation
Abstract
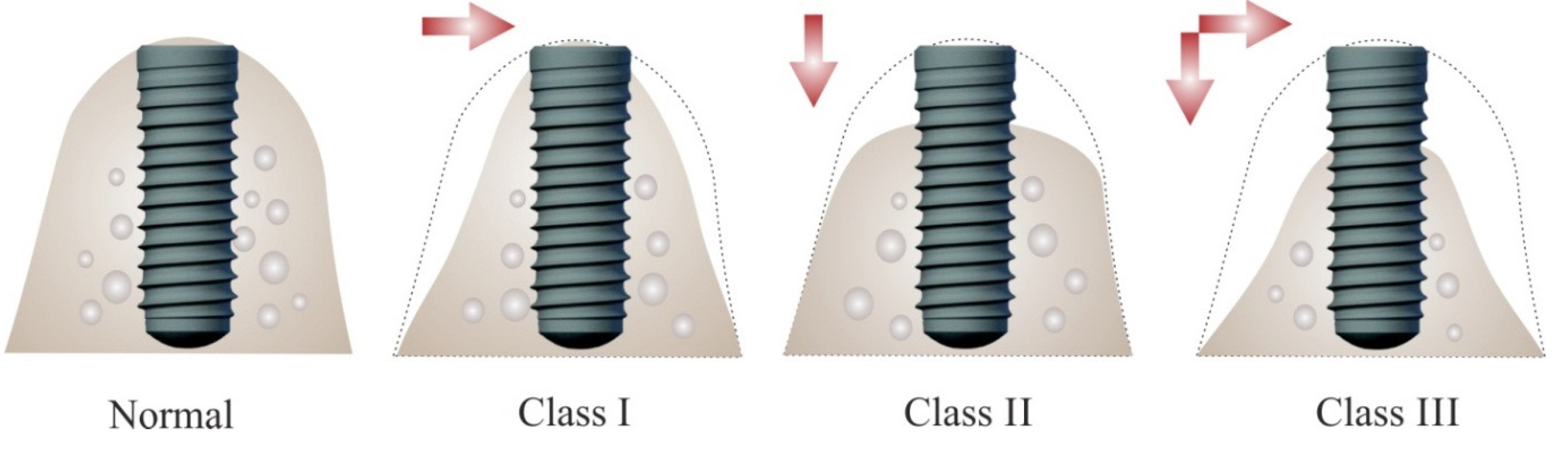
:1. Introduction
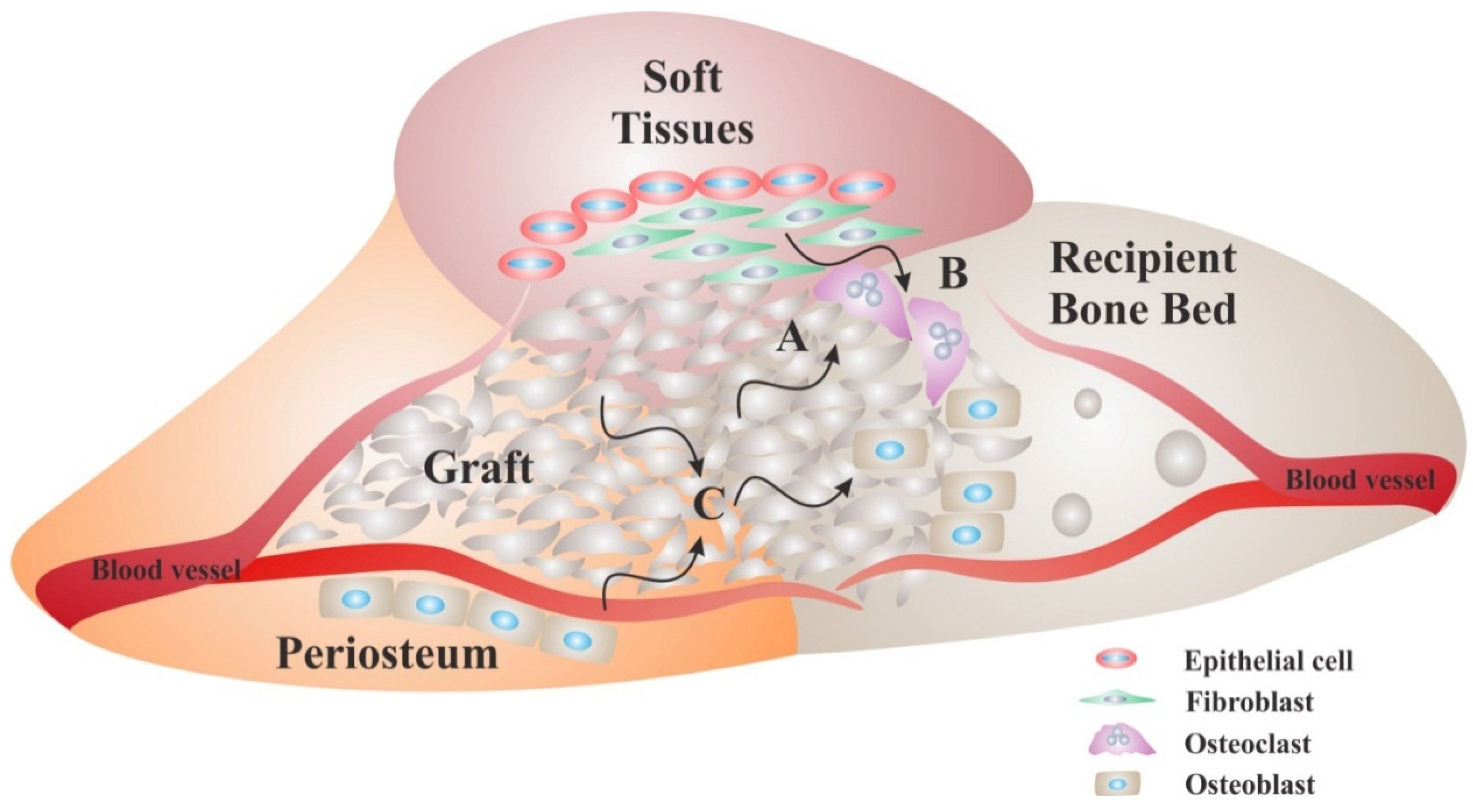
2. Principles of Bone Regeneration
2.1. Basic Multicellular Units
2.2. Space Maintenance
2.3. Osteogenesis
2.4. Osteoconduction
2.5. Osteoinduction
3. Techniques for Vertical Bone Augmentation
3.1. Osteoperiosteal Flap Techniques
3.2. Distraction Osteogenesis
3.3. Block Graft Techniques
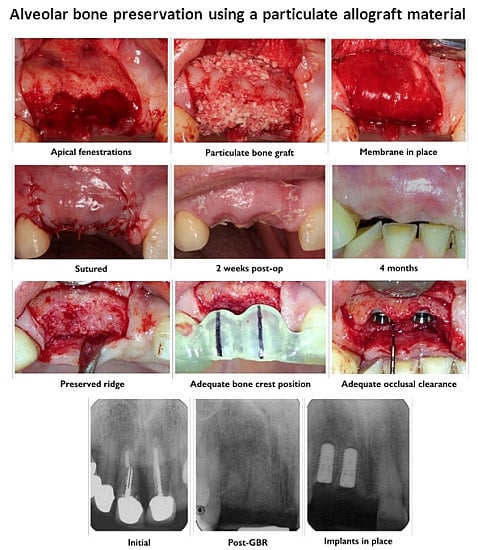
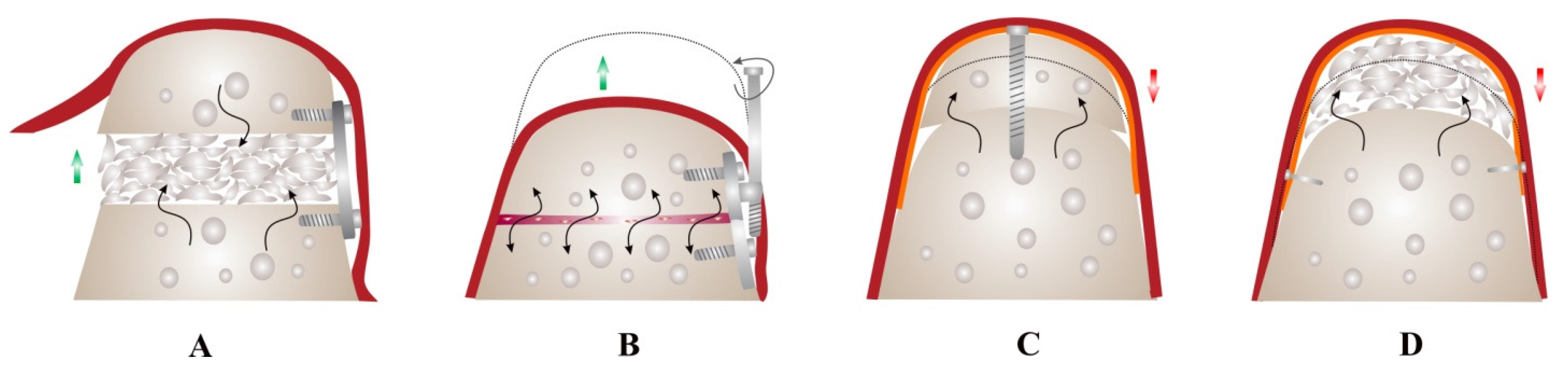
3.4. Guided Bone Regeneration
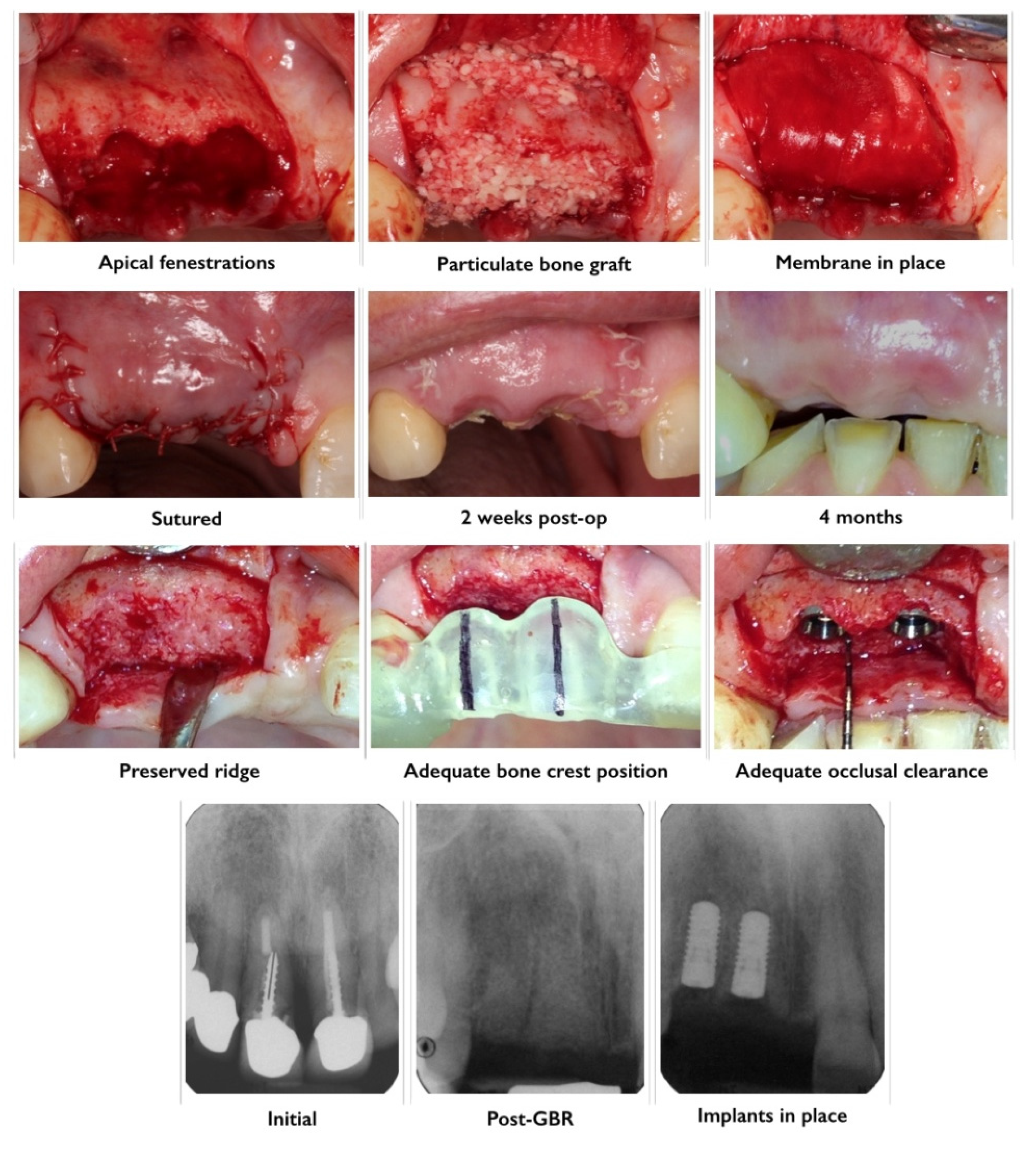
3.5. Minimally Invasive Approaches to GBR
4. Natural Transplants and Synthetic Bone Replacement Graft Tissues and Biomaterials
| Human bone sources | Non-human natural sources | Synthetic sources (Alloplasts) | ||
|---|---|---|---|---|
| Autografts | Allografts | Xenografts | Bioactive glasses | Bioceramics |
| -Extra oral sites | -Fresh frozen bone | -Bovine Hydroxyapatite | – | -Hydroxyapatite |
| -Intra oral sites | -Freeze dried bone allograft (FDBA) | -Coralline calcium carbonate | – | -Other calcium phosphates (Tricalcium phosphate, brushite, monetite) |
| – | -Demineralized freeze dried bone allograft (FDBA) | – | – | |
4.1. Autografts
| Advantages | Disadvantages |
|---|---|
| Biocompatible | Need for additional surgery to procure the tissue |
| Osteoinductive | Increase in operative time and cost |
| Osteoconductive | Donor site morbidity and postoperative pain |
| High osteogeniec potential | Increased risk of fracture to donor site |
| Adequate mechanical strength | Limited amount of tissue can be procured |
| Available in both cortical and cancellous types | High variability in quality of harvested bone tissue |
4.2. Allografts
4.2.1. Fresh or Frozen Iliac Cancellous Bone and Marrow Allografts
4.2.2. Mineralized Freeze-Dried Bone Allografts
4.2.3. Demineralized Freeze-Dried Bone Allografts
4.3. Xenografts
4.4. Alloplasts
4.4.1. Tricalcium Phosphate
4.4.2. Synthetic Hydroxyapatite
4.4.3. Bioactive Glasses
4.4.4. Dicalcium Phosphates
5. Developments and the Future of Bone Augmentation
6. Conclusions
Author Contributions
Conflicts of Interest
References
- Rocchietta, I.; Fontana, F.; Simion, M. Clinical outcomes of vertical bone augmentation to enable dental implant placement: A systematic review. J. Clin. Periodontol. 2008, 35, 203–215. [Google Scholar] [CrossRef] [PubMed]
- Tamimi, F.; Torres, J.; Al-Abedalla, K.; Lopez-Cabarcos, E.; Alkhraisat, M.H.; Bassett, D.C.; Gbureck, U.; Barralet, J.E. Osseointegration of dental implants in 3D-printed synthetic onlay grafts customized according to bone metabolic activity in recipient site. Biomaterials 2014, 35, 5436–5445. [Google Scholar] [CrossRef] [PubMed]
- Lipkowitz, R. An overview of the osseointegration of dental implants. J. Mass. Dent. Soc. 1989, 38, 173–175. [Google Scholar] [PubMed]
- Lipkowitz, R.D.; Berger, J.R.; Gold, B. The osseointegration of dental implants. An overview. NY State Dent. J. 1989, 55, 32–34. [Google Scholar]
- Goto, T. Osseointegration and dental implants. Clin. Calcium 2014, 24, 265–271. [Google Scholar] [PubMed]
- Javed, F.; Ahmed, H.B.; Crespi, R.; Romanos, G.E. Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Int. Med. Appl. Sci. 2013, 5, 162–167. [Google Scholar]
- Khoury, F.; Buchmann, R. Surgical therapy of peri-implant disease: A 3-year follow-up study of cases treated with 3 different techniques of bone regeneration. J. Periodontol. 2001, 72, 1498–1508. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Grusovin, M.G.; Kwan, S.; Worthington, H.V.; Coulthard, P. Interventions for replacing missing teeth: Bone augmentation techniques for dental implant treatment. Cochrane Database Syst. Rev. 2008. [Google Scholar] [CrossRef]
- Liu, J.; Kerns, D.G. Mechanisms of guided bone regeneration: A review. Open Dent. J. 2014, 8, 56–65. [Google Scholar] [CrossRef] [PubMed]
- Van der Weijden, F.; Dell’Acqua, F.; Slot, D.E. Alveolar bone dimensional changes of post-extraction sockets in humans: A systematic review. J. Clin. Periodontol. 2009, 36, 1048–1058. [Google Scholar] [CrossRef] [PubMed]
- Schropp, L.; Wenzel, A.; Kostopoulos, L.; Karring, T. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. Int. J. Periodontics Restor. Dent. 2003, 23, 313–323. [Google Scholar]
- Tallgren, A. The continuing reduction of the residual alveolar ridges in complete denture wearers: A mixed-longitudinal study covering 25 years. 1972. J. Prosthet. Dent. 2003, 89, 427–435. [Google Scholar] [CrossRef]
- Carlsson, G.E.; Thilander, H.; Hedegard, B. Histologic changes in the upper alveolar process after extractions with or without insertion of an immediate full denture. Acta Odontol. Scand. 1967, 25, 21–43. [Google Scholar] [CrossRef] [PubMed]
- Bernstein, S.; Cooke, J.; Fotek, P.; Wang, H.L. Vertical bone augmentation: Where are we now? Implant Dent. 2006, 15, 219–228. [Google Scholar] [CrossRef] [PubMed]
- Tolman, D.E. Advanced residual ridge resorption: Surgical management. Int. J. Prosthodont. 1993, 6, 118–125. [Google Scholar] [PubMed]
- Tonetti, M.S.; Hammerle, C.H. Advances in bone augmentation to enable dental implant placement: Consensus report of the sixth european workshop on periodontology. J. Clin. Periodontol. 2008, 35, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, Z.A.; Javaid, M.A.; Abdallah, M.N. Bone replacement graft materials in dentistry. In Dental Biomaterials (Principle and Its Application), 2nd ed.; Khurshid, Z., Zafar, S.Z., Eds.; Paramount Publishing Enterprise: Karachi, Pakistan, 2013. [Google Scholar]
- Sheikh, Z.; Abdallah, M.N.; Hamdan, N.; Javaid, M.A.; Khurshid, Z. Barrier membranes for tissue regeneration and bone augmentation techniques in dentistry. In Handbook of Oral Biomaterials; Matilinna, K.P., Ed.; Pan Stanford Publishing: Singapore, Singapore, 2014. [Google Scholar]
- Tevlin, R.; McArdle, A.; Atashroo, D.; Walmsley, G.G.; Senarath-Yapa, K.; Zielins, E.R.; Paik, K.J.; Longaker, M.T.; Wan, D.C. Biomaterials for craniofacial bone engineering. J. Dent. Res. 2014, 93, 1187–1195. [Google Scholar] [CrossRef] [PubMed]
- McAllister, B.S.; Haghighat, K. Bone augmentation techniques. J. Periodontol. 2007, 78, 377–396. [Google Scholar] [CrossRef] [PubMed]
- Chiapasco, M.; Zaniboni, M.; Rimondini, L. Autogenous onlay bone grafts vs. Alveolar distraction osteogenesis for the correction of vertically deficient edentulous ridges: A 2–4-year prospective study on humans. Clin. Oral Implant. Res. 2007, 18, 432–440. [Google Scholar]
- Sacco, A.G.; Chepeha, D.B. Current status of transport-disc-distraction osteogenesis for mandibular reconstruction. Lancet Oncol. 2007, 8, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Von Arx, T.; Buser, D. Horizontal ridge augmentation using autogenous block grafts and the guided bone regeneration technique with collagen membranes: A clinical study with 42 patients. Clin. Oral Implant. Res. 2006, 17, 359–366. [Google Scholar] [CrossRef]
- Von Arx, T.; Hardt, N.; Wallkamm, B. The time technique: A new method for localized alveolar ridge augmentation prior to placement of dental implants. Int. J. Oral Maxillofac. Implant. 1996, 11, 387–394. [Google Scholar]
- Roccuzzo, M.; Ramieri, G.; Bunino, M.; Berrone, S. Autogenous bone graft alone or associated with titanium mesh for vertical alveolar ridge augmentation: A controlled clinical trial. Clin. Oral Implant. Res. 2007, 18, 286–294. [Google Scholar] [CrossRef]
- Karsenty, G. Transcriptional control of skeletogenesis. Ann. Rev. Genomics Hum. Genet. 2008, 9, 183–196. [Google Scholar] [CrossRef]
- Nakashima, K.; Zhou, X.; Kunkel, G.; Zhang, Z.; Deng, J.M.; Behringer, R.R.; de Crombrugghe, B. The novel zinc finger-containing transcription factor osterix is required for osteoblast differentiation and bone formation. Cell 2002, 108, 17–29. [Google Scholar] [CrossRef] [PubMed]
- Ornitz, D.M.; Marie, P.J. FGF signaling pathways in endochondral and intramembranous bone development and human genetic disease. Genes Dev. 2002, 16, 1446–1465. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Shi, W.; Cao, X. Multiplicity of BMP signaling in skeletal development. Ann. NY Acad. Sci. 2007, 1116, 29–49. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, V.; Moore, T.L.; Ma, Y.L.; Helvering, L.M.; Frolik, C.A.; Valasek, K.M.; Ducy, P.; Geiser, A.G. Parathyroid hormone bone anabolic action requires Cbfa1/Runx2-dependent signaling. Mol. Endocrinol. 2003, 17, 423–435. [Google Scholar] [CrossRef] [PubMed]
- Teitelbaum, S.L.; Ross, F.P. Genetic regulation of osteoclast development and function. Nat. Rev. Genet. 2003, 4, 638–649. [Google Scholar] [CrossRef] [PubMed]
- Lacey, D.L.; Timms, E.; Tan, H.L.; Kelley, M.J.; Dunstan, C.R.; Burgess, T.; Elliott, R.; Colombero, A.; Elliott, G.; Scully, S.; et al. Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell 1998, 93, 165–176. [Google Scholar]
- Melcher, A.H. On the repair potential of periodontal tissues. J. Periodontol. 1976, 47, 256–260. [Google Scholar] [CrossRef] [PubMed]
- Majzoub, Z.; Berengo, M.; Giardino, R.; Aldini, N.N.; Cordioli, G. Role of intramarrow penetration in osseous repair: A pilot study in the rabbit calvaria. J. Periodontol. 1999, 70, 1501–1510. [Google Scholar] [CrossRef] [PubMed]
- Crea, A.; Deli, G.; Littarru, C.; Lajolo, C.; Orgeas, G.V.; Tatakis, D.N. Intrabony defects, open-flap debridement, and decortication: A randomized clinical trial. J. Periodontol. 2014, 85, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, V.M. Selection of bone grafts for revision total hip arthroplasty. Clin. Orthop. Relat. Res. 2000, 381, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Hiatt, W.H.; Schallhorn, R.G.; Aaronian, A.J. The induction of new bone and cementum formation. Iv. Microscopic examination of the periodontium following human bone and marrow allograft, autograft and nongraft periodontal regenerative procedures. J. Periodontol. 1978, 49, 495–512. [Google Scholar]
- Hiatt, W.H.; Schallho, R. Intraoral transplants of cancellous bone and marrow in periodontal lesions. J. Periodontol. 1973, 44, 194–208. [Google Scholar] [CrossRef] [PubMed]
- Urist, M.R. Bone transplants and implants. In Fundamental and Clinical Bone Physiology; Urist, M.R., Ed.; JB Lippincott: Philadelphia, PA, USA, 1980; pp. 331–368. [Google Scholar]
- Goldberg, V.M.; Stevenson, S. Natural history of autografts and allografts. Clin. Orthop. Relat. Res. 1987, 23, 7–16. [Google Scholar]
- Cornell, C.N. Osteoconductive materials and their role as substitutes for autogenous bone grafts. Orthop. Clin. North Am. 1999, 30, 591–598. [Google Scholar] [CrossRef] [PubMed]
- Mastrogiacomo, M.; Scaglione, S.; Martinetti, R.; Dolcini, L.; Beltrame, F.; Cancedda, R.; Quarto, R. Role of scaffold internal structure on in vivo bone formation in macroporous calcium phosphate bioceramics. Biomaterials 2006, 27, 3230–3237. [Google Scholar] [CrossRef] [PubMed]
- Boyne, P.J. Bone induction and the use of HTR polymer as a vehicle for osseous inductor materials. Compendium 1988, 10, S337–S341. [Google Scholar] [PubMed]
- Ewers, R.T.B.; Ghali, G.; Jensen, O. A new biologic classification of bone augmentation. In The Osteoperiosteal Flap: A Simplified Approach to Alveolar Bone Reconstruction; Quintessence Publishing: Chicago, IL, USA, 2010. [Google Scholar]
- Ito, T.; Kohno, T.; Kojima, T. Free vascularized fibular graft. J. Trauma 1984, 24, 756–760. [Google Scholar] [CrossRef] [PubMed]
- Malizos, K.N.; Zalavras, C.G.; Soucacos, P.N.; Beris, A.E.; Urbaniak, J.R. Free vascularized fibular grafts for reconstruction of skeletal defects. J. Am. Acad. Orthop. Surg. 2004, 12, 360–369. [Google Scholar] [PubMed]
- Kramer, F.J.; Dempf, R.; Bremer, B. Efficacy of dental implants placed into fibula-free flaps for orofacial reconstruction. Clin. Oral Implant. Res. 2005, 16, 80–88. [Google Scholar] [CrossRef]
- Raoul, G.; Ruhin, B.; Briki, S.; Lauwers, L.; Haurou Patou, G.; Capet, J.P.; Maes, J.M.; Ferri, J. Microsurgical reconstruction of the jaw with fibular grafts and implants. J. Craniofac. Surg. 2009, 20, 2105–2117. [Google Scholar] [CrossRef] [PubMed]
- Jensen, O.T.; Kuhlke, K.L. Maxillary full-arch alveolar split osteotomy with island osteoperiosteal flaps and sinus grafting using bone morphogenetic protein-2 and retrofitting for immediate loading with a provisional: Surgical and prosthetic procedures and case report. Int. J. Oral Maxillofac. Implant. 2013, 28, e260–e271. [Google Scholar] [CrossRef]
- Kilic, E.; Alkan, A.; Ulu, M.; Zortuk, M.; Gumus, H.O. Vertical ridge augmentation using sandwich osteotomy: 2 case reports. Gen. Dent. 2013, 61, e22–e25. [Google Scholar] [PubMed]
- Scipioni, A.; Bruschi, G.B.; Calesini, G. The edentulous ridge expansion technique: A five-year study. Int. J. Periodontics Restor. Dent. 1994, 14, 451–459. [Google Scholar]
- Duncan, J.M.; Westwood, R.M. Ridge widening for the thin maxilla: A clinical report. Int. J. Oral Maxillofac. Implant. 1997, 12, 224–227. [Google Scholar]
- Yoshioka, I.; Tanaka, T.; Khanal, A.; Habu, M.; Kito, S.; Kodama, M.; Oda, M.; Wakasugi-Sato, N.; Matsumoto-Takeda, S.; Seta, Y.; et al. Correlation of mandibular bone quality with neurosensory disturbance after sagittal split ramus osteotomy. Br. J. Oral Maxillofac. Surg. 2011, 49, 552–556. [Google Scholar]
- Jensen, O.T.; Cockrell, R.; Kuhike, L.; Reed, C. Anterior maxillary alveolar distraction osteogenesis: A prospective 5-year clinical study. Int. J. Oral Maxillofac. Implant. 2002, 17, 52–68. [Google Scholar]
- Rachmiel, A.; Srouji, S.; Peled, M. Alveolar ridge augmentation by distraction osteogenesis. Int. J. Oral Maxillofac. Surg. 2001, 30, 510–517. [Google Scholar] [CrossRef] [PubMed]
- McAllister, B.S. Histologic and radiographic evidence of vertical ridge augmentation utilizing distraction osteogenesis: 10 consecutively placed distractors. J. Periodontol. 2001, 72, 1767–1779. [Google Scholar] [CrossRef] [PubMed]
- Klug, C.N.; Millesi-Schobel, G.A.; Millesi, W.; Watzinger, F.; Ewers, R. Preprosthetic vertical distraction osteogenesis of the mandible using an l-shaped osteotomy and titanium membranes for guided bone regeneration. J. Oral Maxillofac. Surg. 2001, 59, 1302–1308; discussion 1309–1310. [Google Scholar] [CrossRef] [PubMed]
- Simion, M.; Fontana, F.; Rasperini, G.; Maiorana, C. Vertical ridge augmentation by expanded-polytetrafluoroethylene membrane and a combination of intraoral autogenous bone graft and deproteinized anorganic bovine bone (bio oss). Clin. Oral Implant. Res. 2007, 18, 620–629. [Google Scholar] [CrossRef]
- Enislidis, G.; Fock, N.; Ewers, R. Distraction osteogenesis with subperiosteal devices in edentulous mandibles. Br. J. Oral Maxillofac. Surg. 2005, 43, 399–403. [Google Scholar] [CrossRef] [PubMed]
- Kunkel, M.; Wahlmann, U.; Reichert, T.E.; Wegener, J.; Wagner, W. Reconstruction of mandibular defects following tumor ablation by vertical distraction osteogenesis using intraosseous distraction devices. Clin. Oral Implant. Res. 2005, 16, 89–97. [Google Scholar] [CrossRef]
- Chiapasco, M.; Romeo, E.; Casentini, P.; Rimondini, L. Alveolar distraction osteogenesis vs. Vertical guided bone regeneration for the correction of vertically deficient edentulous ridges: A 1–3-year prospective study on humans. Clin. Oral Implant. Res. 2004, 15, 82–95. [Google Scholar]
- Chiapasco, M.; Consolo, U.; Bianchi, A.; Ronchi, P. Alveolar distraction osteogenesis for the correction of vertically deficient edentulous ridges: A multicenter prospective study on humans. Int. J. Oral Maxillofac. Implant. 2004, 19, 399–407. [Google Scholar]
- Oda, T.; Sawaki, Y.; Ueda, M. Experimental alveolar ridge augmentation by distraction osteogenesis using a simple device that permits secondary implant placement. Int. J. Oral Maxillofac. Implant. 2000, 15, 95–102. [Google Scholar]
- Block, M.S.; Akin, R.; Chang, A.; Gottsegen, G.B.; Gardiner, D. Skeletal and dental movements after anterior maxillary advancement using implant-supported distraction osteogenesis in dogs. J. Oral Maxillofac. Surg. 1997, 55, 1433–1439; discussion 1439–1440. [Google Scholar] [CrossRef] [PubMed]
- Block, M.S.; Almerico, B.; Crawford, C.; Gardiner, D.; Chang, A. Bone response to functioning implants in dog mandibular alveolar ridges augmented with distraction osteogenesis. Int. J. Oral Maxillofac. Implant. 1998, 13, 342–351. [Google Scholar]
- Ilizarov, G.A. Basic principles of transosseous compression and distraction osteosynthesis. Ortop. Travmatol. Protez. 1971, 32, 7–15. [Google Scholar] [PubMed]
- Ilizarov, G.A. The tension-stress effect on the genesis and growth of tissues: Part II. The influence of the rate and frequency of distraction. Clin. Orthop. Relat. Res. 1989, 239, 263–285. [Google Scholar]
- Davies, J.; Turner, S.; Sandy, J.R. Distraction osteogenesis—A review. Br. Dent. J. 1998, 185, 462–467. [Google Scholar] [CrossRef] [PubMed]
- Maffuli, N.; Fixsen, J.A. Distraction osteogenesis in congenital limb length discrepancy: A review. J. R. Coll. Surg. Edinb. 1996, 41, 258–264. [Google Scholar] [PubMed]
- Hidding, J.; Lazar, F.; Zoller, J.E. Initial outcome of vertical distraction osteogenesis of the atrophic alveolar ridge. Mund Kiefer Gesichtschirurgie MKG 1999, 3, S79–S83. [Google Scholar] [CrossRef]
- Chiapasco, M.; Romeo, E.; Vogel, G. Vertical distraction osteogenesis of edentulous ridges for improvement of oral implant positioning: A clinical report of preliminary results. Int. J. Oral Maxillofac. Implant. 2001, 16, 43–51. [Google Scholar]
- Urbani, G.; Lombardo, G.; Santi, E.; Consolo, U. Distraction osteogenesis to achieve mandibular vertical bone regeneration: A case report. Int. J. Periodontics Restor. Dent. 1999, 19, 321–331. [Google Scholar]
- McAllister, B.S.; Gaffaney, T.E. Distraction osteogenesis for vertical bone augmentation prior to oral implant reconstruction. Periodontology 2000 2003, 33, 54–66. [Google Scholar] [CrossRef] [PubMed]
- Chin, M.; Toth, B.A. Distraction osteogenesis in maxillofacial surgery using internal devices: Review of five cases. J. Oral Maxillofac. Surg. 1996, 54, 45–53; discussion 54. [Google Scholar] [CrossRef] [PubMed]
- Maull, D.J. Review of devices for distraction osteogenesis of the craniofacial complex. Semin. Orthod. 1999, 5, 64–73. [Google Scholar] [CrossRef] [PubMed]
- Uckan, S.; Oguz, Y.; Bayram, B. Comparison of intraosseous and extraosseous alveolar distraction osteogenesis. J. Oral Maxillofac. Surg. 2007, 65, 671–674. [Google Scholar] [CrossRef] [PubMed]
- Chin, M. The role of distraction osteogenesis in oral and maxillofacial surgery. J. Oral Maxillofac. Surg. 1998, 56, 805–806. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Zhang, Y.; Shao, B.; Gao, Y.; Zhang, C.; Cao, Q.; Kong, L. Partially biodegradable distraction implant to replace conventional implants in alveolar bone of insufficient height: A preliminary study in dogs. Clin. Implant Dent. Relat. Res. 2014. [Google Scholar] [CrossRef]
- Polo, W.C.; Cury, P.R.; Sendyk, W.R.; Gromatzky, A. Posterior mandibular alveolar distraction osteogenesis utilizing an extraosseous distractor: A prospective study. J. Periodontol. 2005, 76, 1463–1468. [Google Scholar] [CrossRef] [PubMed]
- Iizuka, T.; Hallermann, W.; Seto, I.; Smolka, W.; Smolka, K.; Bosshardt, D.D. Bi-directional distraction osteogenesis of the alveolar bone using an extraosseous device. Clin. Oral Implant. Res. 2005, 16, 700–707. [Google Scholar] [CrossRef]
- Gaggl, A.; Schultes, G.; Karcher, H. Vertical alveolar ridge distraction with prosthetic treatable distractors: A clinical investigation. Int. J. Oral Maxillofac. Implant. 2000, 15, 701–710. [Google Scholar]
- McCarthy, J.G.; Schreiber, J.; Karp, N.; Thorne, C.H.; Grayson, B.H. Lengthening the human mandible by gradual distraction. Plast. Reconstr. Surg. 1992, 89, 1–8; discussion 9–10. [Google Scholar] [CrossRef] [PubMed]
- Lammens, J.; Liu, Z.; Aerssens, J.; Dequeker, J.; Fabry, G. Distraction bone healing vs. osteotomy healing: A comparative biochemical analysis. J. Bone Miner. Res. 1998, 13, 279–286. [Google Scholar] [CrossRef]
- Verlinden, C.R.; van de Vijfeijken, S.E.; Jansma, E.P.; Becking, A.G.; Swennen, G.R. Complications of mandibular distraction osteogenesis for congenital deformities: A systematic review of the literature and proposal of a new classification for complications. Int. J. Oral Maxillofac. Surg. 2015, 44, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Kempton, S.J.; McCarthy, J.E.; Afifi, A.M. A systematic review of distraction osteogenesis in hand surgery: What are the benefits, complication rates, and duration of treatment? Plast. Reconstr. Surg. 2014, 133, 1120–1130. [Google Scholar] [CrossRef] [PubMed]
- Verlinden, C.R.; van de Vijfeijken, S.E.; Tuinzing, D.B.; Jansma, E.P.; Becking, A.G.; Swennen, G.R. Complications of mandibular distraction osteogenesis for developmental deformities: A systematic review of the literature. Int. J. Oral Maxillofac. Surg. 2015, 44, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Batal, H.S.; Cottrell, D.A. Alveolar distraction osteogenesis for implant site development. Oral Maxillofac. Surg. Clin. North Am. 2004, 16, 91–109. [Google Scholar] [CrossRef] [PubMed]
- Isaksson, S.; Alberius, P. Maxillary alveolar ridge augmentation with onlay bone-grafts and immediate endosseous implants. J. Cranio Maxillo Fac. Surg. 1992, 20, 2–7. [Google Scholar] [CrossRef]
- Barone, A.; Covani, U. Maxillary alveolar ridge reconstruction with nonvascularized autogenous block bone: Clinical results. J. Oral Maxillofac. Surg. 2007, 65, 2039–2046. [Google Scholar] [CrossRef] [PubMed]
- Cordaro, L.; Amade, D.S.; Cordaro, M. Clinical results of alveolar ridge augmentation with mandibular block bone grafts in partially edentulous patients prior to implant placement. Clin. Oral Implant. Res. 2002, 13, 103–111. [Google Scholar] [CrossRef]
- Bahat, O.; Fontanessi, R.V. Implant placement in three-dimensional grafts in the anterior jaw. Int. J. Periodontics Restor. Dent. 2001, 21, 357–365. [Google Scholar]
- Schleier, P.; Wolf, C.; Siebert, H.; Shafer, D.; Freilich, M.; Berndt, A.; Schumann, D. Treatment options in distraction osteogenesis therapy using a new bidirectional distractor system. Int. J. Oral Maxillofac. Implant. 2007, 22, 408–416. [Google Scholar]
- Turker, N.; Basa, S.; Vural, G. Evaluation of osseous regeneration in alveolar distraction osteogenesis with histological and radiological aspects. J. Oral Maxillofac. Surg. 2007, 65, 608–614. [Google Scholar] [CrossRef] [PubMed]
- Tolman, D.E. Reconstructive procedures with endosseous implants in grafted bone: A review of the literature. Int. J. Oral Maxillofac. Implants 1995, 10, 275–294. [Google Scholar] [PubMed]
- Misch, C.M. Comparison of intraoral donor sites for onlay grafting prior to implant placement. Int. J. Oral Maxillofac. Implant. 1997, 12, 767–776. [Google Scholar]
- Proussaefs, P.; Lozada, J.; Kleinman, A.; Rohrer, M.D. The use of ramus autogenous block grafts for vertical alveolar ridge augmentation and implant placement: A pilot study. Int. J. Oral Maxillofac. Implant. 2002, 17, 238–248. [Google Scholar]
- Tamimi, F.; Torres, J.; Gbureck, U.; Lopez-Cabarcos, E.; Bassett, D.C.; Alkhraisat, M.H.; Barralet, J.E. Craniofacial vertical bone augmentation: A comparison between 3D printed monolithic monetite blocks and autologous onlay grafts in the rabbit. Biomaterials 2009, 30, 6318–6326. [Google Scholar] [CrossRef] [PubMed]
- Draenert, F.G.; Huetzen, D.; Neff, A.; Mueller, W.E. Vertical bone augmentation procedures: Basics and techniques in dental implantology. J. Biomed. Mater. Res. Part A 2014, 102, 1605–1613. [Google Scholar] [CrossRef]
- Sailer, H.F. A new method of inserting endosseous implants in totally atrophic maxillae. J. Cranio Maxillo Fac. Surg. 1989, 17, 299–305. [Google Scholar] [CrossRef]
- Keller, E.E.; Tolman, D.E.; Eckert, S. Surgical-prosthodontic reconstruction of advanced maxillary bone compromise with autogenous onlay block bone grafts and osseointegrated endosseous implants: A 12-year study of 32 consecutive patients. Int. J. Oral Maxillofac. Implant. 1999, 14, 197–209. [Google Scholar]
- Breine, U.; Branemark, P.I. Reconstruction of alveolar jaw bone. An experimental and clinical study of immediate and preformed autologous bone grafts in combination with osseointegrated implants. Scand. J. Plast. Reconstr. Surg. 1980, 14, 23–48. [Google Scholar]
- Jensen, O.T.; Greer, R.O., Jr.; Johnson, L.; Kassebaum, D. Vertical guided bone-graft augmentation in a new canine mandibular model. Int. J. Oral Maxillofac. Implant. 1995, 10, 335–344. [Google Scholar]
- Jardini, M.A.; De Marco, A.C.; Lima, L.A. Early healing pattern of autogenous bone grafts with and without e-PTFE membranes: A histomorphometric study in rats. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2005, 100, 666–673. [Google Scholar] [CrossRef] [PubMed]
- Buser, D.; Dula, K.; Hirt, H.P.; Schenk, R.K. Lateral ridge augmentation using autografts and barrier membranes: A clinical study with 40 partially edentulous patients. J. Oral Maxillofac. Surg. 1996, 54, 420–432; discussion 432–433. [Google Scholar] [CrossRef] [PubMed]
- Ronda, M.; Rebaudi, A.; Torelli, L.; Stacchi, C. Expanded vs. Dense polytetrafluoroethylene membranes in vertical ridge augmentation around dental implants: A prospective randomized controlled clinical trial. Clin. Oral Implant. Res. 2014, 25, 859–866. [Google Scholar]
- Handelsman, M.; Celletti, R. Alveolar ridge augmentation using membranes. Oral Maxillofac. Surg. Clin. North Am. 2004, 16, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Urban, I.A.; Lozada, J.L.; Jovanovic, S.A.; Nagursky, H.; Nagy, K. Vertical ridge augmentation with titanium-reinforced, dense-PTFE membranes and a combination of particulated autogenous bone and anorganic bovine bone-derived mineral: A prospective case series in 19 patients. Int. J. Oral Maxillofac. Implant. 2014, 29, 185–193. [Google Scholar] [CrossRef]
- Pikos, M.A. Block autografts for localized ridge augmentation: Part I. The posterior maxilla. Implant Dent. 1999, 8, 279–285. [Google Scholar] [CrossRef]
- Pikos, M.A. Block autografts for localized ridge augmentation: Part II. The posterior mandible. Implant Dent. 2000, 9, 67–75. [Google Scholar] [CrossRef]
- Levin, L.; Nitzan, D.; Schwartz-Arad, D. Success of dental implants placed in intraoral block bone grafts. J. Periodontol. 2007, 78, 18–21. [Google Scholar] [CrossRef] [PubMed]
- Stubinger, S.; Nuss, K.; Landes, C.; von Rechenberg, B.; Sader, R. Harvesting of intraoral autogenous block grafts from the chin and ramus region: Preliminary results with a variable square pulse Er:YAG laser. Lasers Surg. Med. 2008, 40, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Pourabbas, R.; Nezafati, S. Clinical results of localized alveolar ridge augmentation with bone grafts harvested from symphysis in comparison with ramus. J. Dent. Res. Dent. Clin. Dent. Prospect. 2007, 1, 7–12. [Google Scholar]
- Verhoeven, J.W.; Cune, M.S.; Terlou, M.; Zoon, M.A.; de Putter, C. The combined use of endosteal implants and iliac crest onlay grafts in the severely atrophic mandible: A longitudinal study. Int. J. Oral Maxillofac. Surg. 1997, 26, 351–357. [Google Scholar] [CrossRef] [PubMed]
- Proussaefs, P.; Lozada, J. The use of intraorally harvested autogenous block grafts for vertical alveolar ridge augmentation: A human study. Int. J. Periodontics Restor. Dent. 2005, 25, 351–363. [Google Scholar]
- Felice, P.; Checchi, V.; Pistilli, R.; Scarano, A.; Pellegrino, G.; Esposito, M. Bone augmentation vs. 5-mm dental implants in posterior atrophic jaws. Four-month post-loading results from a randomised controlled clinical trial. Eur. J. Oral Implantol. 2009, 2, 267–281. [Google Scholar]
- Felice, P.; Cannizzaro, G.; Checchi, V.; Marchetti, C.; Pellegrino, G.; Censi, P.; Esposito, M. Vertical bone augmentation vs. 7-mm-long implants in posterior atrophic mandibles. Results of a randomised controlled clinical trial of up to 4 months after loading. Eur. J. Oral Implantol. 2009, 2, 7–20. [Google Scholar]
- Felice, P.; Marchetti, C.; Iezzi, G.; Piattelli, A.; Worthington, H.; Pellegrino, G.; Esposito, M. Vertical ridge augmentation of the atrophic posterior mandible with interpositional bloc grafts: Bone from the iliac crest vs. Bovine anorganic bone. Clinical and histological results up to one year after loading from a randomized-controlled clinical trial. Clin. Oral Implant. Res. 2009, 20, 1386–1393. [Google Scholar]
- Felice, P.; Pistilli, R.; Lizio, G.; Pellegrino, G.; Nisii, A.; Marchetti, C. Inlay vs. onlay iliac bone grafting in atrophic posterior mandible: A prospective controlled clinical trial for the comparison of two techniques. Clin. Implant Dent. Relat. Res. 2009, 11, e69–e82. [Google Scholar]
- Lin, K.Y.; Bartlett, S.P.; Yaremchuk, M.J.; Fallon, M.; Grossman, R.F.; Whitaker, L.A. The effect of rigid fixation on the survival of onlay bone grafts: An experimental study. Plast. Reconstr. Surg. 1990, 86, 449–456. [Google Scholar] [CrossRef] [PubMed]
- De Carvalho, P.S.; Vasconcellos, L.W.; Pi, J. Influence of bed preparation on the incorporation of autogenous bone grafts: A study in dogs. Int. J. Oral Maxillofac. Implant. 2000, 15, 565–570. [Google Scholar]
- Jensen, J.; Reiche-Fischel, O.; Sindet-Pedersen, S. Autogenous mandibular bone grafts for malar augmentation. J. Oral Maxillofac. Surg. 1995, 53, 88–90. [Google Scholar] [CrossRef] [PubMed]
- Valentini, P.; Abensur, D. Maxillary sinus floor elevation for implant placement with demineralized freeze-dried bone and bovine bone (bio-oss): A clinical study of 20 patients. Int. J. Periodontics Restor. Dent. 1997, 17, 232–241. [Google Scholar]
- Urbani, G.; Lombardo, G.; Santi, E.; Tarnow, D. Localized ridge augmentation with chin grafts and resorbable pins: Case reports. Int. J. Periodontics Restor. Dent. 1998, 18, 363–375. [Google Scholar]
- Whittaker, J.M.; James, R.A.; Lozada, J.; Cordova, C.; GaRey, D.J. Histological response and clinical evaluation of heterograft and allograft materials in the elevation of the maxillary sinus for the preparation of endosteal dental implant sites. Simultaneous sinus elevation and root form implantation: An eight-month autopsy report. J. Oral Implantol. 1989, 15, 141–144. [Google Scholar]
- Albrektsson, T. Repair of bone grafts. A vital microscopic and histological investigation in the rabbit. Scand. J. Plast. Reconstr. Surg. 1980, 14, 1–12. [Google Scholar] [CrossRef]
- Lyford, R.H.; Mills, M.P.; Knapp, C.I.; Scheyer, E.T.; Mellonig, J.T. Clinical evaluation of freeze-dried block allografts for alveolar ridge augmentation: A case series. Int. J. Periodontics Restor. Dent. 2003, 23, 417–425. [Google Scholar]
- Leonetti, J.A.; Koup, R. Localized maxillary ridge augmentation with a block allograft for dental implant placement: Case reports. Implant Dent. 2003, 12, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Keith, J.D., Jr. Localized ridge augmentation with a block allograft followed by secondary implant placement: A case report. Int. J. Periodontics Restor. Dent. 2004, 24, 11–17. [Google Scholar]
- Dahlin, C.; Linde, A.; Gottlow, J.; Nyman, S. Healing of bone defects by guided tissue regeneration. Plast. Reconstr. Surg. 1988, 81, 672–676. [Google Scholar] [CrossRef] [PubMed]
- Buser, D.; Dula, K.; Hess, D.; Hirt, H.P.; Belser, U.C. Localized ridge augmentation with autografts and barrier membranes. Periodontology 2000 1999, 19, 151–163. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, S.; Deshmukh, J.; Deshpande, S.; Khatri, R.; Deshpande, S. Vertical and horizontal ridge augmentation in anterior maxilla using autograft, xenograft and titanium mesh with simultaneous placement of endosseous implants. J. Indian Soc. Periodontol. 2014, 18, 661–665. [Google Scholar] [CrossRef] [PubMed]
- Simion, M.; Jovanovic, S.A.; Tinti, C.; Benfenati, S.P. Long-term evaluation of osseointegrated implants inserted at the time or after vertical ridge augmentation. A retrospective study on 123 implants with 1–5 year follow-up. Clin. Oral Implant. Res. 2001, 12, 35–45. [Google Scholar]
- Simion, M.; Jovanovic, S.A.; Trisi, P.; Scarano, A.; Piattelli, A. Vertical ridge augmentation around dental implants using a membrane technique and autogenous bone or allografts in humans. Int. J. Periodontics Restor. Dent. 1998, 18, 8–23. [Google Scholar]
- Bhola, M.; Kinaia, B.M.; Chahine, K. Guided bone regeneration using an allograft material: Review and case presentations. Pract. Proced. Aesthet. Dent. PPAD 2008, 20, 551–557. [Google Scholar]
- Chiapasco, M.; Zaniboni, M. Clinical outcomes of GBR procedures to correct peri-implant dehiscences and fenestrations: A systematic review. Clin. Oral Implant. Res. 2009, 20, 113–123. [Google Scholar] [CrossRef]
- Clarizio, L.F. Successful implant restoration without the use of membrane barriers. J. Oral Maxillofac. Surg. 1999, 57, 1117–1121. [Google Scholar] [CrossRef] [PubMed]
- Ten Bruggenkate, C.M.; Kraaijenhagen, H.A.; van der Kwast, W.A.; Krekeler, G.; Oosterbeek, H.S. Autogenous maxillary bone grafts in conjunction with placement of I.T.I. Endosseous implants. A preliminary report. Int. J. Oral Maxillofac. Surg. 1992, 21, 81–84. [Google Scholar] [CrossRef]
- Malmquist, J.P. Successful implant restoration with the use of barrier membranes. J. Oral Maxillofac. Surg. 1999, 57, 1114–1116. [Google Scholar] [CrossRef] [PubMed]
- Jovanovic, S.A.; Spiekermann, H.; Richter, E.J. Bone regeneration around titanium dental implants in dehisced defect sites: A clinical study. Int. J. Oral Maxillofac. Implant. 1992, 7, 233–245. [Google Scholar]
- Schenk, R.K.; Buser, D.; Hardwick, W.R.; Dahlin, C. Healing pattern of bone regeneration in membrane-protected defects: A histologic study in the canine mandible. Int. J. Oral Maxillofac. Implant. 1994, 9, 13–29. [Google Scholar]
- Mellonig, J.T.; Nevins, M. Guided bone regeneration of bone defects associated with implants: An evidence-based outcome assessment. Int. J. Periodontics Restor. Dent. 1995, 15, 168–185. [Google Scholar]
- Hurzeler, M.B.; Kohal, R.J.; Naghshbandi, J.; Mota, L.F.; Conradt, J.; Hutmacher, D.; Caffesse, R.G. Evaluation of a new bioresorbable barrier to facilitate guided bone regeneration around exposed implant threads. An experimental study in the monkey. Int. J. Oral Maxillofac. Surg. 1998, 27, 315–320. [Google Scholar] [CrossRef]
- Canullo, L.; Trisi, P.; Simion, M. Vertical ridge augmentation around implants using e-PTFE titanium-reinforced membrane and deproteinized bovine bone mineral (bio-oss): A case report. Int. J. Periodontics Restor. Dent. 2006, 26, 355–361. [Google Scholar]
- Parma-Benfenati, S.; Tinti, C.; Albrektsson, T.; Johansson, C. Histologic evaluation of guided vertical ridge augmentation around implants in humans. Int. J. Periodontics Restor. Dent. 1999, 19, 424–437. [Google Scholar]
- Tinti, C.; Parma-Benfenati, S. Vertical ridge augmentation: Surgical protocol and retrospective evaluation of 48 consecutively inserted implants. Int. J. Periodontics Restor. Dent. 1998, 18, 434–443. [Google Scholar]
- Tinti, C.; Parma-Benfenati, S.; Manfrini, F. Spacemaking metal structures for nonresorbable membranes in guided bone regeneration around implants. Two case reports. Int. J. Periodontics Restor. Dent. 1997, 17, 53–61. [Google Scholar]
- Simion, M.; Trisi, P.; Piattelli, A. Vertical ridge augmentation using a membrane technique associated with osseointegrated implants. Int. J. Periodontics Restor. Dent. 1994, 14, 496–511. [Google Scholar]
- Torres, J.; Tamimi, F.; Alkhraisat, M.H.; Manchon, A.; Linares, R.; Prados-Frutos, J.C.; Hernandez, G.; Lopez Cabarcos, E. Platelet-rich plasma may prevent titanium-mesh exposure in alveolar ridge augmentation with anorganic bovine bone. J. Clin. Periodontol. 2010, 37, 943–951. [Google Scholar] [CrossRef] [PubMed]
- Tinti, C.; Parma-Benfenati, S.; Polizzi, G. Vertical ridge augmentation: What is the limit? Int. J. Periodontics Restor. Dent. 1996, 16, 220–229. [Google Scholar]
- Enislidis, G.; Fock, N.; Millesi-Schobel, G.; Klug, C.; Wittwer, G.; Yerit, K.; Ewers, R. Analysis of complications following alveolar distraction osteogenesis and implant placement in the partially edentulous mandible. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2005, 100, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Raghoebar, G.M.; Liem, R.S.; Vissink, A. Vertical distraction of the severely resorbed edentulous mandible: A clinical, histological and electron microscopic study of 10 treated cases. Clin. Oral Implant. Res. 2002, 13, 558–565. [Google Scholar] [CrossRef]
- Rakhmatia, Y.D.; Ayukawa, Y.; Furuhashi, A.; Koyano, K. Current barrier membranes: Titanium mesh and other membranes for guided bone regeneration in dental applications. J. Prosthodont. Res. 2013, 57, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Kent, J.N. Reconstruction of the alveolar ridge with hydroxyapatite. Dent. Clin. North Am. 1986, 30, 231–257. [Google Scholar] [PubMed]
- Kent, J.N.; Quinn, J.H.; Zide, M.F.; Finger, I.M.; Jarcho, M.; Rothstein, S.S. Correction of alveolar ridge deficiencies with nonresorbable hydroxylapatite. J. Am. Dent. Assoc. 1982, 105, 993–1001. [Google Scholar] [CrossRef] [PubMed]
- Kent, J.N.; Quinn, J.H.; Zide, M.F.; Guerra, L.R.; Boyne, P.J. Alveolar ridge augmentation using nonresorbable hydroxylapatite with or without autogenous cancellous bone. J. Oral Maxillofac. Surg. 1983, 41, 629–642. [Google Scholar] [CrossRef] [PubMed]
- Smiler, D.; Soltan, M.; Lee, J.W. A histomorphogenic analysis of bone grafts augmented with adult stem cells. Implant Dent. 2007, 16, 42–53. [Google Scholar] [CrossRef] [PubMed]
- Rothstein, S.S.; Paris, D.A.; Zacek, M.P. Use of hydroxylapatite for the augmentation of deficient alveolar ridges. J. Oral Maxillofac. Surg. 1984, 42, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Hasson, O. Augmentation of deficient lateral alveolar ridge using the subperiosteal tunneling dissection approach. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 103, e14–e19. [Google Scholar] [CrossRef] [PubMed]
- Mehlisch, D.R.; Taylor, T.D.; Leibold, D.G.; Hiatt, R.; Waite, D.E.; Waite, P.D.; Laskin, D.M.; Smith, S.T. Collagen/hydroxylapatite implant for augmenting deficient alveolar ridges: Twelve-month clinical data. J. Oral Maxillofac. Surg. 1988, 46, 839–843. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.W.; Meyers, J.F.; Robinson, R.R. Hydroxyapatite augmentation of the anterior portion of the maxilla with a modified transpositional flap technique. Oral Surg. Oral Med. Oral Pathol. 1991, 72, 395–399. [Google Scholar] [CrossRef] [PubMed]
- Marshall, S.G. The combined use of endosseous dental implants and collagen/hydroxylapatite augmentation procedures for reconstruction/augmentation of the edentulous and atrophic mandible: A preliminary report. Oral Surg. Oral Med. Oral Pathol. 1989, 68, 517–525; discussion 525–526. [Google Scholar] [CrossRef] [PubMed]
- Kfir, E.; Kfir, V.; Eliav, E.; Kaluski, E. Minimally invasive guided bone regeneration. J. Oral Implantol. 2007, 33, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Mazzocco, C.; Buda, S.; De Paoli, S. The tunnel technique: A different approach to block grafting procedures. Int. J. Periodontics Restor. Dent. 2008, 28, 45–53. [Google Scholar]
- Li, J.; Xuan, F.; Choi, B.H.; Jeong, S.M. Minimally invasive ridge augmentation using xenogenous bone blocks in an atrophied posterior mandible: A clinical and histological study. Implant Dent. 2013, 22, 112–116. [Google Scholar] [CrossRef] [PubMed]
- Vanassche, B.J.; Stoelinga, P.J.; de Koomen, H.A.; Blijdorp, P.A.; Schoenaers, J.H. Reconstruction of the severely resorbed mandible with interposed bone grafts and hydroxylapatite. A 2–3 year follow-up. Int. J. Oral Maxillofac. Surg. 1988, 17, 157–160. [Google Scholar] [CrossRef]
- Block, M.S. Horizontal ridge augmentation using particulate bone. Atlas Oral Maxillofac. Surg. Clin. North Am. 2006, 14, 27–38. [Google Scholar] [CrossRef] [PubMed]
- Block, M.S.; Degen, M. Horizontal ridge augmentation using human mineralized particulate bone: Preliminary results. J. Oral Maxillofac. Surg. 2004, 62, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Kuemmerle, J.M.; Oberle, A.; Oechslin, C.; Bohner, M.; Frei, C.; Boecken, I.; von Rechenberg, B. Assessment of the suitability of a new brushite calcium phosphate cement for cranioplasty—An experimental study in sheep. J. Cranio Maxillofac. Surg. 2005, 33, 37–44. [Google Scholar] [CrossRef]
- Frayssinet, P.; Gineste, L.; Conte, P.; Fages, J.; Rouquet, N. Short-term implantation effects of a DCPD-based calcium phosphate cement. Biomaterials 1998, 19, 971–977. [Google Scholar] [CrossRef] [PubMed]
- Apelt, D.; Theiss, F.; El-Warrak, A.O.; Zlinszky, K.; Bettschart-Wolfisberger, R.; Bohner, M.; Matter, S.; Auer, J.A.; von Rechenberg, B. In vivo behavior of three different injectable hydraulic calcium phosphate cements. Biomaterials 2004, 25, 1439–1451. [Google Scholar] [CrossRef] [PubMed]
- Flautre, B.; Lemaitre, J.; Maynou, C.; Van Landuyt, P.; Hardouin, P. Influence of polymeric additives on the biological properties of brushite cements: An experimental study in rabbit. J. Biomed. Mater. Res. Part A 2003, 66A, 214–223. [Google Scholar] [CrossRef]
- Flautre, B.; Maynou, C.; Lemaitre, J.; van Landuyt, P.; Hardouin, P. Bone colonization of beta-TCP granules incorporated in brushite cements. J. Biomed. Mater. Res. 2002, 63, 413–417. [Google Scholar] [CrossRef] [PubMed]
- Flautre, B.; Delecourt, C.; Blary, M.C.; van Landuyt, P.; Lemaitre, J.; Hardouin, P. Volume effect on biological properties of a calcium phosphate hydraulic cement: Experimental study in sheep. Bone 1999, 25, 35S–39S. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.X.; About, I.; Stephan, G.; Van Landuyt, P.; Dejou, J.; Fiocchi, M.; Lemaitre, J.; Proust, J.P. Histological and biomechanical studies of two bone colonizable cements in rabbits. Bone 1999, 25, 41S–45S. [Google Scholar] [CrossRef] [PubMed]
- Penel, G.; Leroy, N.; Van Landuyt, P.; Flautre, B.; Hardouin, P.; Lemaitre, J.; Leroy, G. Raman microspectrometry studies of brushite cement: In vivo evolution in a sheep model. Bone 1999, 25, 81S–84S. [Google Scholar] [CrossRef] [PubMed]
- Ohura, K.; Bohner, M.; Hardouin, P.; Lemaitre, J.; Pasquier, G.; Flautre, B. Resorption of, and bone formation from, new beta-tricalcium phosphate-monocalcium phosphate cements: An in vivo study. J. Biomed. Mater. Res. 1996, 30, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Munting, E.; Mirtchi, A.A.; Lemaitre, J. Bone repair of defects filled with phosphoclacic hydraulic cemet—An in vitro study. J. Mater. Sci. Mater. Med. 1993, 4, 337–344. [Google Scholar] [CrossRef]
- Hallman, M.; Thor, A. Bone substitutes and growth factors as an alternative/complement to autogenous bone for grafting in implant dentistry. Periodontology 2000 2008, 47, 172–192. [Google Scholar] [CrossRef] [PubMed]
- Botticelli, D.; Berglundh, T.; Buser, D.; Lindhe, J. The jumping distance revisited: An experimental study in the dog. Clin. Oral Implant. Res. 2003, 14, 35–42. [Google Scholar] [CrossRef]
- Wilson, T.G., Jr.; Schenk, R.; Buser, D.; Cochran, D. Implants placed in immediate extraction sites: A report of histologic and histometric analyses of human biopsies. Int. J. Oral Maxillofac. Implant. 1998, 13, 333–341. [Google Scholar]
- Yukna, R.A. Clinical comparison of hydroxyapatite-coated titanium dental implants placed in fresh extraction sockets and healed sites. J. Periodontol. 1991, 62, 468–472. [Google Scholar] [CrossRef] [PubMed]
- Cypher, T.J.; Grossman, J.P. Biological principles of bone graft healing. J. Foot Ankle Surg. 1996, 35, 413–417. [Google Scholar] [CrossRef] [PubMed]
- Younger, E.M.; Chapman, M.W. Morbidity at bone graft donor sites. J. Orthop. Trauma 1989, 3, 192–195. [Google Scholar] [CrossRef] [PubMed]
- Dodd, C.A.; Fergusson, C.M.; Freedman, L.; Houghton, G.R.; Thomas, D. Allograft vs. autograft bone in scoliosis surgery. J. Bone Joint Surg. Br. 1988, 70, 431–434. [Google Scholar]
- Summers, B.N.; Eisenstein, S.M. Donor site pain from the ilium. A complication of lumbar spine fusion. J. Bone Joint Surg. Br. 1989, 71, 677–680. [Google Scholar]
- Arrington, E.D.; Smith, W.J.; Chambers, H.G.; Bucknell, A.L.; Davino, N.A. Complications of iliac crest bone graft harvesting. Clin. Orthop. Relat. Res. 1996, 300–309. [Google Scholar] [CrossRef]
- Sandhu, H.S.; Grewal, H.S.; Parvataneni, H. Bone grafting for spinal fusion. Orthop. Clin. N. Am. 1999, 30, 685–698. [Google Scholar] [CrossRef]
- Khoury, F. Augmentation of the sinus floor with mandibular bone block and simultaneous implantation: A 6-year clinical investigation. Int. J. Oral Maxillofac. Implant. 1999, 14, 557–564. [Google Scholar]
- Nkenke, E.; Weisbach, V.; Winckler, E.; Kessler, P.; Schultze-Mosgau, S.; Wiltfang, J.; Neukam, F.W. Morbidity of harvesting of bone grafts from the iliac crest for preprosthetic augmentation procedures: A prospective study. Int. J. Oral Maxillofac. Surg. 2004, 33, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Wilk, R.M. Bony reconstruction of the jaws. In Peterson’s Principles of Oral and Maxillofacial Surgery, 2nd ed.; Miloro, M., Ed.; B C Decker Inc.: Hamilton, ON, Canada, 2004; pp. 785–787. [Google Scholar]
- Rocchietta, I.; Simion, M.; Hoffmann, M.; Trisciuoglio, D.; Benigni, M.; Dahlin, C. Vertical bone augmentation with an autogenous block or particles in combination with guided bone regeneration: A clinical and histological preliminary study in humans. Clin. Implan. Dent. Relat. Res. 2015, in press. [Google Scholar]
- Merli, M.; Migani, M.; Esposito, M. Vertical ridge augmentation with autogenous bone grafts: Resorbable barriers supported by ostheosynthesis plates vs. titanium-reinforced barriers. A preliminary report of a blinded, randomized controlled clinical trial. Int. J. Oral Maxillofac. Implant. 2007, 22, 373–382. [Google Scholar]
- Boyce, T.; Edwards, J.; Scarborough, N. Allograft bone. The influence of processing on safety and performance. Orthop. Clin. North Am. 1999, 30, 571–581. [Google Scholar] [CrossRef]
- Tomford, W.W. Transmission of disease through transplantation of musculoskeletal allografts. J. Bone Joint Surg. Am. 1995, 77, 1742–1754. [Google Scholar] [PubMed]
- Centers for Disease Control and Prevention (CDC). Update: Allograft-associated bacterial infections—United States, 2002. MMWR Morb. Mortal. Wkly. Rep 2002, 51, 207–210. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Septic arthritis following anterior cruciate ligament reconstruction using tendon allografts—Florida and Louisiana, 2000. MMWR Morb. Mortal. Wkly. Rep. 2001, 50, 1081–1083. [Google Scholar]
- Oxlund, H.; Andersen, N.B.; Ortoft, G.; Orskov, H.; Andreassen, T.T. Growth hormone and mild exercise in combination markedly enhance cortical bone formation and strength in old rats. Endocrinology 1998, 139, 1899–1904. [Google Scholar] [PubMed]
- Bolander, M.E.; Balian, G. The use of demineralized bone matrix in the repair of segmental defects. Augmentation with extracted matrix proteins and a comparison with autologous grafts. J. Bone Joint Surg. Am. 1986, 68, 1264–1274. [Google Scholar]
- Araujo, P.P.; Oliveira, K.P.; Montenegro, S.C.; Carreiro, A.F.; Silva, J.S.; Germano, A.R. Block allograft for reconstruction of alveolar bone ridge in implantology: A systematic review. Implant Dent. 2013, 22, 304–308. [Google Scholar] [CrossRef] [PubMed]
- Sterio, T.W.; Katancik, J.A.; Blanchard, S.B.; Xenoudi, P.; Mealey, B.L. A prospective, multicenter study of bovine pericardium membrane with cancellous particulate allograft for localized alveolar ridge augmentation. Int. J. Periodontics Restor. Dent. 2013, 33, 499–507. [Google Scholar] [CrossRef]
- Cochran, D.L.; Douglas, H.B. Augmentation of osseous tissue around nonsubmerged endosseous dental implants. Int. J. Periodontics Restor. Dent. 1993, 13, 506–519. [Google Scholar]
- Guerrero, J.S.; Al-Jandan, B.A. Allograft for maxillary sinus floor augmentation: A retrospective study of 90 cases. Implant Dent. 2012, 21, 136–140. [Google Scholar] [CrossRef] [PubMed]
- Avila, G.; Neiva, R.; Misch, C.E.; Galindo-Moreno, P.; Benavides, E.; Rudek, I.; Wang, H.L. Clinical and histologic outcomes after the use of a novel allograft for maxillary sinus augmentation: A case series. Implant Dent. 2010, 19, 330–341. [Google Scholar] [CrossRef] [PubMed]
- Sohn, D.S.; Lee, J.K.; An, K.M.; Shin, H.I. Histomorphometric evaluation of mineralized cancellous allograft in the maxillary sinus augmentation: A 4 case report. Implant Dent. 2009, 18, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Smukler, H.; Landi, L.; Setayesh, R. Histomorphometric evaluation of extraction sockets and deficient alveolar ridges treated with allograft and barrier membrane: A pilot study. Int. J. Oral Maxillofac. Implant. 1999, 14, 407–416. [Google Scholar]
- Froum, S.; Cho, S.C.; Rosenberg, E.; Rohrer, M.; Tarnow, D. Histological comparison of healing extraction sockets implanted with bioactive glass or demineralized freeze-dried bone allograft: A pilot study. J. Periodontol. 2002, 73, 94–102. [Google Scholar] [CrossRef] [PubMed]
- Wood, R.A.; Mealey, B.L. Histologic comparison of healing after tooth extraction with ridge preservation using mineralized vs. demineralized freeze-dried bone allograft. J. Periodontol. 2012, 83, 329–336. [Google Scholar]
- Beck, T.M.; Mealey, B.L. Histologic analysis of healing after tooth extraction with ridge preservation using mineralized human bone allograft. J. Periodontol. 2010, 81, 1765–1772. [Google Scholar] [CrossRef] [PubMed]
- Eskow, A.J.; Mealey, B.L. Evaluation of healing following tooth extraction with ridge preservation using cortical vs. cancellous freeze-dried bone allograft. J. Periodontol. 2014, 85, 514–524. [Google Scholar]
- Borg, T.D.; Mealey, B.L. Histologic healing following tooth extraction with ridge preservation using mineralized freeze dried bone allograft alone vs. a combined mineralized-demineralized freeze dried bone allograft. A randomized controlled clinical trial. J. Periodontol. 2014, 86, 1–13. [Google Scholar]
- Al Ruhaimi, K.A. Bone graft substitutes: A comparative qualitative histologic review of current osteoconductive grafting materials. Int. J. Oral Maxillofac. Implant. 2001, 16, 105–114. [Google Scholar]
- Dias, R.R.; Sehn, F.P.; de Santana Santos, T.; Silva, E.R.; Chaushu, G.; Xavier, S.P. Corticocancellous fresh-frozen allograft bone blocks for augmenting atrophied posterior mandibles in humans. Clin. Oral Implant. Res. 2014. [Google Scholar] [CrossRef]
- Macedo, L.G.; Mazzucchelli-Cosmo, L.A.; Macedo, N.L.; Monteiro, A.S.; Sendyk, W.R. Fresh-frozen human bone allograft in vertical ridge augmentation: Clinical and tomographic evaluation of bone formation and resorption. Cell Tissue Bank. 2012, 13, 577–586. [Google Scholar] [CrossRef] [PubMed]
- Contar, C.M.; Sarot, J.R.; da Costa, M.B.; Bordini, J.; de Lima, A.A.; Alanis, L.R.; Trevilatto, P.C.; Machado, M.A. Fresh-frozen bone allografts in maxillary ridge augmentation: Histologic analysis. J. Oral Implantol. 2011, 37, 223–231. [Google Scholar] [CrossRef] [PubMed]
- Contar, C.M.; Sarot, J.R.; Bordini, J., Jr.; Galvao, G.H.; Nicolau, G.V.; Machado, M.A. Maxillary ridge augmentation with fresh-frozen bone allografts. J. Oral Maxillofac. Surg. 2009, 67, 1280–1285. [Google Scholar] [CrossRef] [PubMed]
- Shetty, V.; Han, T.J. Alloplastic materials in reconstructive periodontal surgery. Dent. Clin. North Am. 1991, 35, 521–530. [Google Scholar] [PubMed]
- Shah, M.; Lobo Gajiwala, A.; Shah, S.; Dave, D. Comparative study of indigenously prepared and imported, demineralized, freeze-dried, irradiated bone allograft in the treatment of periodontal infrabony defects. Cell Tissue Bank. 2014. [Google Scholar] [CrossRef]
- Gurinsky, B.S.; Mills, M.P.; Mellonig, J.T. Clinical evaluation of demineralized freeze-dried bone allograft and enamel matrix derivative vs. enamel matrix derivative alone for the treatment of periodontal osseous defects in humans. J. Periodontol. 2004, 75, 1309–1318. [Google Scholar]
- Turner, D.W.; Mellonig, J.T. Antigenicity of freeze-dried bone allograft in periodontal osseous defects. J. Period. Res. 1981, 16, 89–99. [Google Scholar] [CrossRef]
- Pearson, G.E.; Freeman, E. The composite graft: Autogenous cancellous bone and marrow combined with freeze-dried bone allograft in the treatment of periodontal osseous defects. Ont. Dent. 1980, 57, 10–13. [Google Scholar] [PubMed]
- Markou, N.; Pepelassi, E.; Vavouraki, H.; Stamatakis, H.C.; Nikolopoulos, G.; Vrotsos, I.; Tsiklakis, K. Treatment of periodontal endosseous defects with platelet-rich plasma alone or in combination with demineralized freeze-dried bone allograft: A comparative clinical trial. J. Periodontol. 2009, 80, 1911–1919. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.; Bhattacharya, H.S.; Srikanth, G.; Singh, A. Comparative evaluation of decalcified freeze dried bone allograft with and without local doxycycline in non-contained human periodontal infrabony defects. J. Indian Soc. Periodontol. 2013, 17, 490–494. [Google Scholar] [CrossRef] [PubMed]
- Blaggana, V.; Gill, A.S.; Blaggana, A. A clinical and radiological evaluation of the relative efficacy of demineralized freeze-dried bone allograft vs. anorganic bovine bone xenograft in the treatment of human infrabony periodontal defects: A 6 months follow-up study. J. Indian Soc. Periodontol. 2014, 18, 601–607. [Google Scholar]
- Mazor, Z.; Mamidwar, S.; Ricci, J.L.; Tovar, N.M. Bone repair in periodontal defect using a composite of allograft and calcium sulfate (dentogen) and a calcium sulfate barrier. J. Oral Implantol. 2011, 37, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Kukreja, B.J.; Dodwad, V.; Kukreja, P.; Ahuja, S.; Mehra, P. A comparative evaluation of platelet-rich plasma in combination with demineralized freeze-dried bone allograft and DFDBA alone in the treatment of periodontal intrabony defects: A clinicoradiographic study. J. Indian Soc. Periodontol. 2014, 18, 618–623. [Google Scholar] [CrossRef] [PubMed]
- Friedlaender, G.E.; Strong, D.M.; Sell, K.W. Studies on the antigenicity of bone. I. Freeze-dried and deep-frozen bone allografts in rabbits. J. Bone Joint Surg. Am. 1976, 58, 854–858. [Google Scholar]
- Mellonig, J.T. Freeze-dried bone allografts in periodontal reconstructive surgery. Dent. Clin. North Am. 1991, 35, 505–520. [Google Scholar] [PubMed]
- Quattlebaum, J.B.; Mellonig, J.T.; Hensel, N.F. Antigenicity of freeze-dried cortical bone allograft in human periodontal osseous defects. J. Periodontol. 1988, 59, 394–397. [Google Scholar] [CrossRef] [PubMed]
- Committee on Research, Science. Tissue banking of bone allografts used in periodontal regeneration. J. Periodontol. 2001, 72, 834–838. [Google Scholar]
- Mellonig, J.T. Human histologic evaluation of a bovine-derived bone xenograft in the treatment of periodontal osseous defects. Int. J. Periodontics Restor. Dent. 2000, 20, 19–29. [Google Scholar]
- Wallace, S.; Gellin, R. Clinical evaluation of freeze-dried cancellous block allografts for ridge augmentation and implant placement in the maxilla. Implant Dent. 2010, 19, 272–279. [Google Scholar] [CrossRef] [PubMed]
- Jacotti, M.; Wang, H.L.; Fu, J.H.; Zamboni, G.; Bernardello, F. Ridge augmentation with mineralized block allografts: Clinical and histological evaluation of 8 cases treated with the 3-dimensional block technique. Implant Dent. 2012, 21, 444–448. [Google Scholar] [CrossRef] [PubMed]
- Russell, J.; Scarborough, N.; Chesmel, K. Re: Ability of commercial demineralized freeze-dried bone allograft to induce new bone formation (1996, 67, 918–26). J. Periodontol. 1997, 68, 804–806. [Google Scholar] [CrossRef] [PubMed]
- Hopp, S.G.; Dahners, L.E.; Gilbert, J.A. A study of the mechanical strength of long bone defects treated with various bone autograft substitutes: An experimental investigation in the rabbit. J. Orthop. Res. 1989, 7, 579–584. [Google Scholar] [CrossRef] [PubMed]
- Urist, M.R.; Chang, J.J.; Lietze, A.; Huo, Y.K.; Brownell, A.G.; DeLange, R.J. Preparation and bioassay of bone morphogenetic protein and polypeptide fragments. Methods Enzymol. 1987, 146, 294–312. [Google Scholar] [PubMed]
- Urist, M.R.; Iwata, H.; Strates, B.S. Bone morphogenetic protein and proteinase in the guinea pig. Clin. Orthop. Relat. Res. 1972, 85, 275–290. [Google Scholar] [CrossRef] [PubMed]
- Mellonig, J.T.; Bowers, G.M.; Cotton, W.R. Comparison of bone graft materials. Part II. New bone formation with autografts and allografts: A histological evaluation. J. Periodontol. 1981, 52, 297–302. [Google Scholar]
- Urist, M.R.; Huo, Y.K.; Brownell, A.G.; Hohl, W.M.; Buyske, J.; Lietze, A.; Tempst, P.; Hunkapiller, M.; DeLange, R.J. Purification of bovine bone morphogenetic protein by hydroxyapatite chromatography. Proc. Natl. Acad. Sci. USA 1984, 81, 371–375. [Google Scholar] [CrossRef] [PubMed]
- Sampath, T.K.; Muthukumaran, N.; Reddi, A.H. Isolation of osteogenin, an extracellular matrix-associated, bone-inductive protein, by heparin affinity chromatography. Proc. Natl. Acad. Sci. USA 1987, 84, 7109–7113. [Google Scholar] [CrossRef] [PubMed]
- Shigeyama, Y.; D’Errico, J.A.; Stone, R.; Somerman, M.J. Commercially-prepared allograft material has biological activity in vitro. J. Periodontol. 1995, 66, 478–487. [Google Scholar] [CrossRef] [PubMed]
- Hauschka, P.V.; Chen, T.L.; Mavrakos, A.E. Polypeptide growth factors in bone matrix. Ciba Found. Symp. 1988, 136, 207–225. [Google Scholar] [PubMed]
- Jergesen, H.E.; Chua, J.; Kao, R.T.; Kaban, L.B. Age effects on bone induction by demineralized bone powder. Clin. Orthop. Relat. Res. 1991, 253–259. [Google Scholar]
- Syftestad, G.T.; Urist, M.R. Bone aging. Clin. Orthop. Relat. Res. 1982, 162, 288–297. [Google Scholar] [PubMed]
- Dodson, S.A.; Bernard, G.W.; Kenney, E.B.; Carranza, F.A. In vitro comparison of aged and young osteogenic and hemopoietic bone marrow stem cells and their derivative colonies. J. Periodontol. 1996, 67, 184–196. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Degidi, M.; Iezzi, G.; Pecora, G.; Piattelli, M.; Orsini, G.; Caputi, S.; Perrotti, V.; Mangano, C.; Piattelli, A. Maxillary sinus augmentation with different biomaterials: A comparative histologic and histomorphometric study in man. Implant Dent. 2006, 15, 197–207. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Piattelli, A.; Perrotti, V.; Manzon, L.; Iezzi, G. Maxillary sinus augmentation in humans using cortical porcine bone: A histological and histomorphometrical evaluation after 4 and 6 months. Clin. Implant Dent. Relat. Res. 2011, 13, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Becker, W.; Urist, M.R.; Tucker, L.M.; Becker, B.E.; Ochsenbein, C. Human demineralized freeze-dried bone: Inadequate induced bone formation in athymic mice. A preliminary report. J. Periodontol. 1995, 66, 822–828. [Google Scholar] [CrossRef]
- Senn, N. Senn on the healing of aseptic bone cavities by implantation of antiseptic decalcified bone. Ann. Surg. 1889, 10, 352–368. [Google Scholar] [CrossRef] [PubMed]
- Thaller, S.R.; Hoyt, J.; Borjeson, K.; Dart, A.; Tesluk, H. Reconstruction of calvarial defects with anorganic bovine bone mineral (bio-oss) in a rabbit model. J. Craniofac. Surg. 1993, 4, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Wallace, S.S.; Froum, S.J.; Tarnow, D.P. Histologic evaluation of a sinus elevation procedure: A clinical report. Int. J. Periodontics Restor. Dent. 1996, 16, 46–51. [Google Scholar]
- McAllister, B.S.; Margolin, M.D.; Cogan, A.G.; Buck, D.; Hollinger, J.O.; Lynch, S.E. Eighteen-month radiographic and histologic evaluation of sinus grafting with anorganic bovine bone in the chimpanzee. Int. J. Oral Maxillofac. Implant. 1999, 14, 361–368. [Google Scholar]
- Jarcho, M. Calcium phosphate ceramics as hard tissue prosthetics. Clin. Orthop. Relat. Res. 1981, 157, 259–278. [Google Scholar] [PubMed]
- Melcher, A.H.; Dent, H.D. The use of heterogenous anorganic bone as an implant material in oral procedures. Oral Surg. Oral Med. Oral Pathol. 1962, 15, 996–1000. [Google Scholar] [CrossRef] [PubMed]
- Emmings, F.G. Chemically modified osseous material for the restoration of bone defects. J. Periodontol. 1974, 45, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Sogal, A.; Tofe, A.J. Risk assessment of bovine spongiform encephalopathy transmission through bone graft material derived from bovine bone used for dental applications. J. Periodontol. 1999, 70, 1053–1063. [Google Scholar] [CrossRef] [PubMed]
- Wenz, B.; Oesch, B.; Horst, M. Analysis of the risk of transmitting bovine spongiform encephalopathy through bone grafts derived from bovine bone. Biomaterials 2001, 22, 1599–1606. [Google Scholar] [CrossRef] [PubMed]
- Zitzmann, N.U.; Naef, R.; Scharer, P. Resorbable vs. nonresorbable membranes in combination with bio-oss for guided bone regeneration. Int. J. Oral Maxillofac. Implants 1997, 12, 844–852. [Google Scholar]
- Yildirim, M.; Spiekermann, H.; Biesterfeld, S.; Edelhoff, D. Maxillary sinus augmentation using xenogenic bone substitute material bio-oss in combination with venous blood. A histologic and histomorphometric study in humans. Clin. Oral Implant. Res. 2000, 11, 217–229. [Google Scholar] [CrossRef]
- Thoma, D.S.; Jones, A.; Yamashita, M.; Edmunds, R.; Nevins, M.; Cochran, D.L. Ridge augmentation using recombinant bone morphogenetic protein-2 techniques: An experimental study in the canine. J. Periodontol. 2010, 81, 1829–1838. [Google Scholar] [CrossRef] [PubMed]
- Guillemin, G.; Patat, J.L.; Fournie, J.; Chetail, M. The use of coral as a bone graft substitute. J. Biomed. Mater. Res. 1987, 21, 557–567. [Google Scholar] [CrossRef] [PubMed]
- Yukna, R.A. Clinical evaluation of coralline calcium carbonate as a bone replacement graft material in human periodontal osseous defects. J. Periodontol. 1994, 65, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Piattelli, A.; Podda, G.; Scarano, A. Clinical and histological results in alveolar ridge enlargement using coralline calcium carbonate. Biomaterials 1997, 18, 623–627. [Google Scholar] [CrossRef] [PubMed]
- Gao, T.J.; Tuominen, T.K.; Lindholm, T.S.; Kommonen, B.; Lindholm, T.C. Morphological and biomechanical difference in healing in segmental tibial defects implanted with biocoral or tricalcium phosphate cylinders. Biomaterials 1997, 18, 219–223. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.K.; Choi, E.J.; Cho, K.S.; Chai, J.K.; Wikesjo, U.M. Periodontal repair in intrabony defects treated with a calcium carbonate implant and guided tissue regeneration. J. Periodontol. 1996, 67, 1301–1306. [Google Scholar] [CrossRef] [PubMed]
- Mora, F.; Ouhayoun, J.P. Clinical evaluation of natural coral and porous hydroxyapatite implants in periodontal bone lesions: Results of a 1-year follow-up. J. Clin. Periodontol. 1995, 22, 877–884. [Google Scholar] [CrossRef] [PubMed]
- Hench, L.L. Bioactive materials: The potential for tissue regeneration. J. Biomed. Mater. Res. 1998, 41, 511–518. [Google Scholar] [CrossRef] [PubMed]
- AlGhamdi, A.S.; Shibly, O.; Ciancio, S.G. Osseous grafting part II: Xenografts and alloplasts for periodontal regeneration—A literature review. J. Int. Acad. Periodontol. 2010, 12, 39–44. [Google Scholar] [PubMed]
- Teng, F.; Zhang, Q.; Wu, M.; Rachana, S.; Ou, G. Clinical use of ridge-splitting combined with ridge expansion osteotomy, sandwich bone augmentation, and simultaneous implantation. Br. J. Oral Maxillofac. Surg. 2014, 52, 703–708. [Google Scholar] [CrossRef] [PubMed]
- Saffar, J.L.; Colombier, M.L.; Detienville, R. Bone formation in tricalcium phosphate-filled periodontal intrabony lesions. Histological observations in humans. J. Periodontol. 1990, 61, 209–216. [Google Scholar] [CrossRef]
- Schepers, E.; de Clercq, M.; Ducheyne, P.; Kempeneers, R. Bioactive glass particulate material as a filler for bone lesions. J. Oral Rehabil. 1991, 18, 439–452. [Google Scholar] [CrossRef] [PubMed]
- Hislop, W.S.; Finlay, P.M.; Moos, K.F. A preliminary study into the uses of anorganic bone in oral and maxillofacial surgery. Br. J. Oral Maxillofac. Surg. 1993, 31, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Pallesen, L.; Schou, S.; Aaboe, M.; Hjorting-Hansen, E.; Nattestad, A.; Melsen, F. Influence of particle size of autogenous bone grafts on the early stages of bone regeneration: A histologic and stereologic study in rabbit calvarium. Int. J. Oral Maxillofac. Implant. 2002, 17, 498–506. [Google Scholar]
- Tamimi, F.; Sheikh, Z.; Barralet, J. Dicalcium phosphate cements: Brushite and monetite. Acta Biomater. 2012, 8, 474–487. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto-Uoshima, M.; Ishikawa, I.; Kinoshita, A.; Weng, H.T.; Oda, S. Clinical and histologic observation of replacement of biphasic calcium phosphate by bone tissue in monkeys. Int. J. Periodontics Restor. Dent. 1995, 15, 205–213. [Google Scholar]
- Strub, J.R.; Gaberthuel, T.W.; Firestone, A.R. Comparison of tricalcium phosphate and frozen allogenic bone implants in man. J. Periodontol. 1979, 50, 624–629. [Google Scholar] [CrossRef] [PubMed]
- Amler, M.H. Osteogenic potential of nonvital tissues and synthetic implant materials. J. Periodontol. 1987, 58, 758–761. [Google Scholar] [CrossRef] [PubMed]
- Baldock, W.T.; Hutchens, L.H., Jr.; McFall, W.T., Jr.; Simpson, D.M. An evaluation of tricalcium phosphate implants in human periodontal osseous defects of two patients. J. Periodontol. 1985, 56, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Shalash, M.A.; Rahman, H.A.; Azim, A.A.; Neemat, A.H.; Hawary, H.E.; Nasry, S.A. Evaluation of horizontal ridge augmentation using beta tricalcium phosphate and demineralized bone matrix: A comparative study. J. Clin. Exp. Dent. 2013, 5, e253–e259. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Zhang, Z.; Zhao, J.; Zhang, X.; Sun, X.; Xia, L.; Chang, Q.; Ye, D.; Jiang, X. Vertical alveolar ridge augmentation with beta-tricalcium phosphate and autologous osteoblasts in canine mandible. Biomaterials 2009, 30, 2489–2498. [Google Scholar] [CrossRef] [PubMed]
- Nyan, M.; Miyahara, T.; Noritake, K.; Hao, J.; Rodriguez, R.; Kasugai, S. Feasibility of alpha tricalcium phosphate for vertical bone augmentation. J. Investig. Clin. Dent. 2014, 5, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Klein, C.P.; Driessen, A.A.; de Groot, K.; van den Hooff, A. Biodegradation behavior of various calcium phosphate materials in bone tissue. J. Biomed. Mater. Res. 1983, 17, 769–784. [Google Scholar] [CrossRef] [PubMed]
- Rabalais, M.L., Jr.; Yukna, R.A.; Mayer, E.T. Evaluation of durapatite ceramic as an alloplastic implant in periodontal osseous defects. I. Initial six-month results. J. Periodontol. 1981, 52, 680–689. [Google Scholar]
- Meffert, R.M.; Thomas, J.R.; Hamilton, K.M.; Brownstein, C.N. Hydroxylapatite as an alloplastic graft in the treatment of human periodontal osseous defects. J. Periodontol. 1985, 56, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Wagner, J.R. Clinical and histological case study using resorbable hydroxylapatite for the repair of osseous defects prior to endosseous implant surgery. J. Oral Implantol. 1989, 15, 186–192. [Google Scholar] [PubMed]
- Ricci, J.L.; Blumenthal, N.C.; Spivak, J.M.; Alexander, H. Evaluation of a low-temperature calcium phosphate particulate implant material: Physical-chemical properties and in vivo bone response. J. Oral Maxillofac. Surg. 1992, 50, 969–978. [Google Scholar] [CrossRef] [PubMed]
- Heughebaert, M.; LeGeros, R.Z.; Gineste, M.; Guilhem, A.; Bonel, G. Physicochemical characterization of deposits associated with ha ceramics implanted in nonosseous sites. J. Biomed. Mater. Res. 1988, 22, 257–268. [Google Scholar] [CrossRef] [PubMed]
- Yamasaki, H. Hetertopic bone formation around porous hydroxyapatite ceramic in the subcutis of dogs. Jpn. J. Oral Biol. 1990, 32, 190–192. [Google Scholar] [CrossRef]
- Sugar, A.W.; Thielens, P.; Stafford, G.D.; Willins, M.J. Augmentation of the atrophic maxillary alveolar ridge with hydroxyapatite granules in a vicryl (polyglactin 910) knitted tube and simultaneous open vestibuloplasty. Br. J. Oral Maxillofac. Surg. 1995, 33, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Frame, J.W. A convenient animal model for testing bone substitute materials. J. Oral Surg. 1980, 38, 176–180. [Google Scholar] [PubMed]
- Small, S.A.; Zinner, I.D.; Panno, F.V.; Shapiro, H.J.; Stein, J.I. Augmenting the maxillary sinus for implants: Report of 27 patients. Int. J. Oral Maxillofac. Implant. 1993, 8, 523–528. [Google Scholar]
- Hurzeler, M.B.; Kirsch, A.; Ackermann, K.L.; Quinones, C.R. Reconstruction of the severely resorbed maxilla with dental implants in the augmented maxillary sinus: A 5-year clinical investigation. Int. J. Oral Maxillofac. Implant. 1996, 11, 466–475. [Google Scholar]
- Frame, J.W. Hydroxyapatite as a biomaterial for alveolar ridge augmentation. Int. J. Oral Maxillofac. Surg. 1987, 16, 642–655. [Google Scholar] [CrossRef] [PubMed]
- Jensen, O.T.; Shulman, L.B.; Block, M.S.; Iacono, V.J. Report of the sinus consensus conference of 1996. Int. J. Oral Maxillofac. Implant. 1998, 13, 11–45. [Google Scholar]
- Figliuzzi, M.; Mangano, F.G.; Fortunato, L.; De Fazio, R.; Macchi, A.; Iezzi, G.; Piattelli, A.; Mangano, C. Vertical ridge augmentation of the atrophic posterior mandible with custom-made, computer-aided design/computer-aided manufacturing porous hydroxyapatite scaffolds. J. Craniofac. Surg. 2013, 24, 856–859. [Google Scholar] [CrossRef] [PubMed]
- Petrovic, V.; Zivkovic, P.; Petrovic, D.; Stefanovic, V. Craniofacial bone tissue engineering. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 114, e1–e9. [Google Scholar] [CrossRef] [PubMed]
- Hall, E.E.; Meffert, R.M.; Hermann, J.S.; Mellonig, J.T.; Cochran, D.L. Comparison of bioactive glass to demineralized freeze-dried bone allograft in the treatment of intrabony defects around implants in the canine mandible. J. Periodontol. 1999, 70, 526–535. [Google Scholar] [CrossRef] [PubMed]
- Schepers, E.J.; Ducheyne, P.; Barbier, L.; Schepers, S. Bioactive glass particles of narrow size range: A new material for the repair of bone defects. Implant Dent. 1993, 2, 151–156. [Google Scholar] [CrossRef] [PubMed]
- MacNeill, S.R.; Cobb, C.M.; Rapley, J.W.; Glaros, A.G.; Spencer, P. In vivo comparison of synthetic osseous graft materials. A preliminary study. J. Clin. Periodontol. 1999, 26, 239–245. [Google Scholar] [CrossRef]
- Wilson, J.; Clark, A.E.; Hall, M.; Hench, L.L. Tissue response to bioglass endosseous ridge maintenance implants. J. Oral Implantol. 1993, 19, 295–302. [Google Scholar] [PubMed]
- Stanley, H.R.; Hall, M.B.; Clark, A.E.; King, C.J., 3rd; Hench, L.L.; Berte, J.J. Using 45s5 bioglass cones as endosseous ridge maintenance implants to prevent alveolar ridge resorption: A 5-year evaluation. Int. J. Oral Maxillofac. Implant. 1997, 12, 95–105. [Google Scholar]
- Ong, M.M.; Eber, R.M.; Korsnes, M.I.; MacNeil, R.L.; Glickman, G.N.; Shyr, Y.; Wang, H.L. Evaluation of a bioactive glass alloplast in treating periodontal intrabony defects. J. Periodontol. 1998, 69, 1346–1354. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.A.; Chen, A.Y.; Yu, Z.E.; Huang, Z.J.; Wao, Y.M. Alveolar ridge augmentation with bioactive glass ceramics: A histological study. J. Oral Rehabil. 1989, 16, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Stavropoulos, A.; Sima, C.; Sima, A.; Nyengaard, J.; Karring, T.; Sculean, A. Histological evaluation of healing after transalveolar maxillary sinus augmentation with bioglass and autogenous bone. Clin. Oral Implant. Res. 2012, 23, 125–131. [Google Scholar] [CrossRef]
- Maria, S.M.; Prukner, C.; Sheikh, Z.; Mueller, F.; Barralet, J.E.; Komarova, S.V. Reproducible quantification of osteoclastic activity: Characterization of a biomimetic calcium phosphate assay. J. Biomed. Mater. Res. B Appl. Biomater. 2013, 102, 903–912. [Google Scholar] [CrossRef] [PubMed]
- Gunn, J.M.; Rekola, J.; Hirvonen, J.; Aho, A.J. Comparison of the osteoconductive properties of three particulate bone fillers in a rabbit model: Allograft, calcium carbonate (biocoral(r)) and S53P4 bioactive glass. Acta Odontol. Scand. 2013, 71, 1238–1242. [Google Scholar] [CrossRef] [PubMed]
- Tamimi, F.; Torres, J.; Lopez-Cabarcos, E.; Bassett, D.C.; Habibovic, P.; Luceron, E.; Barralet, J.E. Minimally invasive maxillofacial vertical bone augmentation using brushite based cements. Biomaterials 2009, 30, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Tamimi, F.; Torres, J.; Bassett, D.; Barralet, J.; Cabarcos, E.L. Resorption of monetite granules in alveolar bone defects in human patients. Biomaterials 2010, 31, 2762–2769. [Google Scholar] [CrossRef] [PubMed]
- Bauer, T.W.; Muschler, G.F. Bone graft materials. An overview of the basic science. Clin. Orthop. Relat. Res. 2000, 371, 10–27. [Google Scholar] [CrossRef]
- Marino, F.T.; Torres, J.; Tresguerres, I.; Jerez, L.B.; Cabarcos, E.L. Vertical bone augmentation with granulated brushite cement set in glycolic acid. J. Biomed. Mater. Res. Part A 2007, 81, 93–102. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Fama, F.G. Buccal dehiscence and sinus lift cases-predictable bone augmentation with synthetic bone material. Implants 2010, 11, 28–31. [Google Scholar]
- Torres, J.; Tamimi, I.; Cabrejos-Azama, J.; Tresguerres, I.; Alkhraisat, M.; López-Cabarcos, E.; Hernández, G.; Tamimi, F. Monetite granules versus particulate autologous bone in bone regeneration. Ann. Anat. Anat. Anz. 2015, 200, 126–133. [Google Scholar] [CrossRef]
- Tamimi, F.M.; Torres, J.; Tresguerres, I.; Clemente, C.; Lopez-Cabarcos, E.; Blanco, L.J. Bone augmentation in rabbit calvariae: Comparative study between bio-oss(r) and a novel beta-TCP/DCPD granulate. J. Clin. Periodontol. 2006, 33, 922–928. [Google Scholar] [CrossRef] [PubMed]
- Bohner, M.; Gbureck, U. Thermal reactions of brushite cements. J. Biomed. Mater. Res. Part B Appl. Biomater. 2008, 84B, 375–385. [Google Scholar] [CrossRef]
- Gbureck, U.; Hozel, T.; Klammert, U.; Wurzler, K.; Muller, F.A.; Barralet, J.E. Resorbable dicalcium phosphate bone substitutes prepared by 3d powder printing. Adv. Funct. Mater. 2007, 17, 3940–3945. [Google Scholar] [CrossRef]
- Tamimi, F.; Le Nihouannen, D.; Eimar, H.; Sheikh, Z.; Komarova, S.; Barralet, J. The effect of autoclaving on the physical and biological properties of dicalcium phosphate dihydrate bioceramics: Brushite vs. Monetite. Acta Biomater. 2012, 8, 3161–3169. [Google Scholar] [CrossRef]
- Idowu, B.; Cama, G.; Deb, S.; di Silvio, L. In vitro osteoinductive potential of porous monetite for bone tissue engineering. J. Tissue Eng. 2014, 5. [Google Scholar] [CrossRef]
- Tamimi, F.; Torres, J.; Kathan, C.; Baca, R.; Clemente, C.; Blanco, L.; Cabarcos, E.L. Bone regeneration in rabbit calvaria with novel monetite granules. J. Biomed. Mater. Res. Part A 2008, 87A, 980–985. [Google Scholar] [CrossRef]
- Rezwan, K.; Chen, Q.; Blaker, J.; Boccaccini, A.R. Biodegradable and bioactive porous polymer/inorganic composite scaffolds for bone tissue engineering. Biomaterials 2006, 27, 3413–3431. [Google Scholar] [CrossRef] [PubMed]
- Sabir, M.I.; Xu, X.; Li, L. A review on biodegradable polymeric materials for bone tissue engineering applications. J. Mater. Sci. 2009, 44, 5713–5724. [Google Scholar] [CrossRef]
- Liu, X.; Ma, P.X. Polymeric scaffolds for bone tissue engineering. Ann. Biomed. Eng. 2004, 32, 477–486. [Google Scholar] [CrossRef] [PubMed]
- Yunos, D.M.; Bretcanu, O.; Boccaccini, A.R. Polymer-bioceramic composites for tissue engineering scaffolds. J. Mater. Sci. 2008, 43, 4433–4442. [Google Scholar] [CrossRef]
- Sheikh, Z.; Geffers, M.; Christel, T.; Barralet, J.E.; Gbureck, U. Chelate setting of alkali ion substituted calcium phosphates. Ceram. Int. 2015, in press. [Google Scholar]
- Paul, W.; Sharma, C.P. Bioceramic scaffold—Bone tissue engineering. In Handbook of Intelligent Scaffold for Tissue Engineering and Regenerative Medicine; Pan Stanford Publishing: Danvers, MA, USA, 2012. [Google Scholar]
- Barinov, S.; Komlev, V. Calcium Phosphate Based Bioceramics for Bone Tissue Engineering; Trans Tech Publications: Zurich, Switzerland, 2008. [Google Scholar]
- Taba, M., Jr.; Jin, Q.; Sugai, J.V.; Giannobile, W.V. Current concepts in periodontal bioengineering. Orthod. Craniofac. Res. 2005, 8, 292–302. [Google Scholar] [CrossRef] [PubMed]
- Howell, T.H.; Fiorellini, J.; Jones, A.; Alder, M.; Nummikoski, P.; Lazaro, M.; Lilly, L.; Cochran, D. A feasibility study evaluating rhBMP-2/absorbable collagen sponge device for local alveolar ridge preservation or augmentation. Int. J. Periodontics Restor. Dent. 1997, 17, 124–139. [Google Scholar]
- Margolin, M.D.; Cogan, A.G.; Taylor, M.; Buck, D.; McAllister, T.N.; Toth, C.; McAllister, B.S. Maxillary sinus augmentation in the non-human primate: A comparative radiographic and histologic study between recombinant human osteogenic protein-1 and natural bone mineral. J. Periodontol. 1998, 69, 911–919. [Google Scholar] [CrossRef] [PubMed]
- Becker, W.; Becker, B.E.; Caffesse, R. A comparison of demineralized freeze-dried bone and autologous bone to induce bone formation in human extraction sockets. J. Periodontol. 1994, 65, 1128–1133. [Google Scholar] [CrossRef] [PubMed]
- Boyne, P.J.; Nath, R.; Nakamura, A. Human recombinant BMP-2 in osseous reconstruction of simulated cleft palate defects. Br. J. Oral Maxillofac. Surg. 1998, 36, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, J.M.; Hwang, K.; Winn, S.R.; Hollinger, J.O. Bone morphogenetic proteins: An update on basic biology and clinical relevance. J. Orthop. Res. 1999, 17, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Urist, M.R. Bone: Formation by autoinduction. Science 1965, 150, 893–899. [Google Scholar] [CrossRef] [PubMed]
- Edmunds, R.K.; Mealey, B.L.; Mills, M.P.; Thoma, D.S.; Schoolfield, J.; Cochran, D.L.; Mellonig, J. Maxillary anterior ridge augmentation with recombinant human bone morphogenetic protein 2. Int. J. Periodontics Restor. Dent. 2014, 34, 551–557. [Google Scholar] [CrossRef]
- Katanec, D.; Granic, M.; Majstorovic, M.; Trampus, Z.; Panduric, D.G. Use of recombinant human bone morphogenetic protein (rhBMP2) in bilateral alveolar ridge augmentation: Case report. Coll. Antropol. 2014, 38, 325–330. [Google Scholar] [PubMed]
- Kim, Y.J.; Lee, J.Y.; Kim, J.E.; Park, J.C.; Shin, S.W.; Cho, K.S. Ridge preservation using demineralized bone matrix gel with recombinant human bone morphogenetic protein-2 after tooth extraction: A randomized controlled clinical trial. J. Oral Maxillofac. Surg. 2014, 72, 1281–1290. [Google Scholar] [CrossRef] [PubMed]
- Sheikh, Z.; Javaid, M.A.; Hamdan, N.; Hashmi, R. Bone regeneration using bone morphogenetic proteins and various biomaterial carriers. Materials 2015, 8, 1778–1816. [Google Scholar] [CrossRef]
- Shweikeh, F.; Hanna, G.; Bloom, L.; Sayegh, E.T.; Liu, J.; Acosta, F.L.; Drazin, D. Assessment of outcome following the use of recombinant human bone morphogenetic protein-2 for spinal fusion in the elderly population. J. Neurosurg. Sci. 2014, in press. [Google Scholar]
- Zhang, H.; Wang, F.; Ding, L.; Zhang, Z.; Sun, D.; Feng, X.; An, J.; Zhu, Y. A meta analysis of lumbar spinal fusion surgery using bone morphogenetic proteins and autologous iliac crest bone graft. PLoS ONE 2014, 9. [Google Scholar] [CrossRef] [PubMed]
- Myllyla, R.M.; Haapasaari, K.M.; Lehenkari, P.; Tuukkanen, J. Bone morphogenetic proteins 4 and 2/7 induce osteogenic differentiation of mouse skin derived fibroblast and dermal papilla cells. Cell Tissue Res. 2014, 355, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.; Ye, Y.; Wang, J.; Zhang, W.; Chen, A.; Guo, F. Bone morphogenetic proteins induce rabbit bone marrow-derived mesenchyme stem cells to differentiate into osteoblasts via BMP signals pathway. Artif. Cells Nanomed. Biotechnol. 2013, 41, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Saito, E.; Saito, A.; Kawanami, M. Favorable healing following space creation in rhBMP-2-induced periodontal regeneration of horizontal circumferential defects in dogs with experimental periodontitis. J. Periodontol. 2003, 74, 1808–1815. [Google Scholar] [CrossRef] [PubMed]
- Wikesjo, U.M.; Xiropaidis, A.V.; Thomson, R.C.; Cook, A.D.; Selvig, K.A.; Hardwick, W.R. Periodontal repair in dogs: rhBMP-2 significantly enhances bone formation under provisions for guided tissue regeneration. J. Clin. Periodontol. 2003, 30, 705–714. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Zhao, M.; Mundy, G.R. Bone morphogenetic proteins. Growth Fact. 2004, 22, 233–241. [Google Scholar] [CrossRef]
- Turgeman, G.; Zilberman, Y.; Zhou, S.; Kelly, P.; Moutsatsos, I.K.; Kharode, Y.P.; Borella, L.E.; Bex, F.J.; Komm, B.S.; Bodine, P.V. Systemically administered rhBMP-2 promotes MSC activity and reverses bone and cartilage loss in osteopenic mice. J. Cell. Biochem. 2002, 86, 461–474. [Google Scholar] [CrossRef] [PubMed]
- Marden, L.J.; Hollinger, J.O.; Chaudhari, A.; Turek, T.; Schaub, R.G.; Ron, E. Recombinant human bone morphogenetic protein-2 is superior to demineralized bone matrix in repairing craniotomy defects in rats. J. Biomed. Mater. Res. 1994, 28, 1127–1138. [Google Scholar] [CrossRef] [PubMed]
- Kirker-Head, C.A.; Gerhart, T.N.; Schelling, S.H.; Hennig, G.E.; Wang, E.; Holtrop, M.E. Long-term healing of bone using recombinant human bone morphogenetic protein 2. Clin. Orthop. Relat. R. 1995, 318, 222–230. [Google Scholar]
- Toriumi, D.M.; Kotler, H.S.; Luxenberg, D.P.; Holtrop, M.E.; Wang, E.A. Mandibular reconstruction with a recombinant bone-inducing factor: Functional, histologic, and biomechanical evaluation. Arch. Otolaryngol. Head Neck Surg. 1991, 117, 1101–1112. [Google Scholar] [CrossRef] [PubMed]
- Agnihotri, S.A.; Mallikarjuna, N.N.; Aminabhavi, T.M. Recent advances on chitosan-based micro-and nanoparticles in drug delivery. J. Control. Release 2004, 100, 5–28. [Google Scholar] [CrossRef] [PubMed]
- Panyam, J.; Labhasetwar, V. Biodegradable nanoparticles for drug and gene delivery to cells and tissue. Adv. Drug Deliv. Rev. 2003, 55, 329–347. [Google Scholar] [CrossRef] [PubMed]
- Farokhzad, O.C.; Langer, R. Impact of nanotechnology on drug delivery. ACS Nano 2009, 3, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Pridgen, E.M.; Alexis, F.; Farokhzad, O.C. Polymeric nanoparticle drug delivery technologies for oral delivery applications. Expert Opin. Drug Deliv. 2015, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Martino, M.M.; Briquez, P.S.; Maruyama, K.; Hubbell, J.A. Extracellular matrix-inspired growth factor delivery systems for bone regeneration. Adv. Drug Deliv. Rev. 2015, in press. [Google Scholar]
- Hu, Y.-L.; Fu, Y.-H.; Tabata, Y.; Gao, J.-Q. Mesenchymal stem cells: A promising targeted-delivery vehicle in cancer gene therapy. J. Control. Release 2010, 147, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Caplan, A.I. Review: Mesenchymal stem cells: Cell-based reconstructive therapy in orthopedics. Tissue Eng. 2005, 11, 1198–1211. [Google Scholar] [CrossRef] [PubMed]
- Bessa, P.C.; Casal, M.; Reis, R. Bone morphogenetic proteins in tissue engineering: The road from laboratory to clinic, part II (bmp delivery). J. Tissue Eng. Regen. Med. 2008, 2, 81–96. [Google Scholar] [CrossRef] [PubMed]
- Kenley, R.; Marden, L.; Turek, T.; Jin, L.; Ron, E.; Hollinger, J. Osseous regeneration in the rat calvarium using novel delivery systems for recombinant human bone morphogenetic protein-2 (rhBMP-). J. Biomed. Mater. Res. 1994, 28, 1139–1147. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Shea, M.; Battle, M.; Kozitza, K.; Ron, E.; Turek, T.; Schaub, R.; Hayes, W. Healing of large segmental defects in rat femurs is aided by rhBMP-2 in PLGA matrix. J. Biomed. Mater. Res. 1994, 28, 1149–1156. [Google Scholar] [CrossRef] [PubMed]
- Schrier, J.A.; Fink, B.F.; Rodgers, J.B.; Vasconez, H.C.; DeLuca, P.P. Effect of a freeze-dried CMC/PLGA microsphere matrix of rhBMP-2 on bone healing. AAPS PharmSciTech 2001, 2, 73–80. [Google Scholar] [CrossRef]
- Becker, W.; Lynch, S.E.; Lekholm, U.; Becker, B.E.; Caffesse, R.; Donath, K.; Sanchez, R. A comparison of ePTFE membranes alone or in combination with platelet-derived growth factors and insulin-like growth factor-I or demineralized freeze-dried bone in promoting bone formation around immediate extraction socket implants. J. Periodontol. 1992, 63, 929–940. [Google Scholar] [CrossRef] [PubMed]
- Simion, M.; Rocchietta, I.; Kim, D.; Nevins, M.; Fiorellini, J. Vertical ridge augmentation by means of deproteinized bovine bone block and recombinant human platelet-derived growth factor-bb: A histologic study in a dog model. Int. J. Periodontics Restor. Dent. 2006, 26, 415–423. [Google Scholar]
- Tsuchiya, N.; Sato, S.; Kigami, R.; Kawano, E.; Takane, M.; Arai, Y.; Ito, K.; Ogiso, B. Effect of a chitosan sponge impregnated with platelet-derived growth factor on bone augmentation beyond the skeletal envelope in rat calvaria. J. Oral Sci. 2014, 56, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Kammerer, P.W.; Palarie, V.; Schiegnitz, E.; Nacu, V.; Draenert, F.G.; Al-Nawas, B. Influence of a collagen membrane and recombinant platelet-derived growth factor on vertical bone augmentation in implant-fixed deproteinized bovine bone—Animal pilot study. Clin. Oral Implants Res. 2013, 24, 1222–1230. [Google Scholar] [PubMed]
- Marx, R.E.; Carlson, E.R.; Eichstaedt, R.M.; Schimmele, S.R.; Strauss, J.E.; Georgeff, K.R. Platelet-rich plasma: Growth factor enhancement for bone grafts. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1998, 85, 638–646. [Google Scholar] [CrossRef] [PubMed]
- Eskan, M.A.; Greenwell, H.; Hill, M.; Morton, D.; Vidal, R.; Shumway, B.; Girouard, M.E. Platelet-rich plasma-assisted guided bone regeneration for ridge augmentation: A randomized, controlled clinical trial. J. Periodontol. 2014, 85, 661–668. [Google Scholar] [CrossRef] [PubMed]
- Khairy, N.M.; Shendy, E.E.; Askar, N.A.; El-Rouby, D.H. Effect of platelet rich plasma on bone regeneration in maxillary sinus augmentation (randomized clinical trial). Int. J. Oral Maxillofac. Surg. 2013, 42, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Cabbar, F.; Guler, N.; Kurkcu, M.; Iseri, U.; Sencift, K. The effect of bovine bone graft with or without platelet-rich plasma on maxillary sinus floor augmentation. J. Oral Maxillofac. Surg. 2011, 69, 2537–2547. [Google Scholar] [CrossRef] [PubMed]
- Annunziata, M.; Oliva, A.; Buonaiuto, C.; Di Feo, A.; Di Pasquale, R.; Passaro, I.; Guida, L. In vitro cell-type specific biological response of human periodontally related cells to platelet-rich plasma. J. Period. Res. 2005, 40, 489–495. [Google Scholar] [CrossRef]
- Hanna, R.; Trejo, P.M.; Weltman, R.L. Treatment of intrabony defects with bovine-derived xenograft alone and in combination with platelet-rich plasma: A randomized clinical trial. J. Periodontol. 2004, 75, 1668–1677. [Google Scholar] [CrossRef] [PubMed]
- Sanchez, A.R.; Sheridan, P.J.; Kupp, L.I. Is platelet-rich plasma the perfect enhancement factor? A current review. Int. J. Oral Maxillofac. Implant. 2003, 18, 93–103. [Google Scholar]
- Wallace, S.S.; Froum, S.J. Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann. Periodontol. Am. Acad. Periodontol. 2003, 8, 328–343. [Google Scholar] [CrossRef]
- Breitbart, A.S.; Grande, D.A.; Mason, J.M.; Barcia, M.; James, T.; Grant, R.T. Gene-enhanced tissue engineering: Applications for bone healing using cultured periosteal cells transduced retrovirally with the BMP-7 gene. Ann. Plast. Surg. 1999, 42, 488–495. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, J.R.; Daluiski, A.; Stevenson, S.; Wu, L.; McAllister, P.; Lee, Y.P.; Kabo, J.M.; Finerman, G.A.; Berk, A.J.; Witte, O.N. The effect of regional gene therapy with bone morphogenetic protein-2-producing bone-marrow cells on the repair of segmental femoral defects in rats. J. Bone Joint Surg. Am. 1999, 81, 905–917. [Google Scholar] [PubMed]
- Malekzadeh, R.; Hollinger, J.O.; Buck, D.; Adams, D.F.; McAllister, B.S. Isolation of human osteoblast-like cells and in vitro amplification for tissue engineering. J. Periodontol. 1998, 69, 1256–1262. [Google Scholar] [CrossRef] [PubMed]
- Freed, L.E.; Marquis, J.C.; Nohria, A.; Emmanual, J.; Mikos, A.G.; Langer, R. Neocartilage formation in vitro and in vivo using cells cultured on synthetic biodegradable polymers. J. Biomed. Mater. Res. 1993, 27, 11–23. [Google Scholar] [CrossRef] [PubMed]
- Ishaug, S.L.; Yaszemski, M.J.; Bizios, R.; Mikos, A.G. Osteoblast function on synthetic biodegradable polymers. J. Biomed. Mater. Res. 1994, 28, 1445–1453. [Google Scholar] [CrossRef] [PubMed]
- Bruder, S.P.; Kraus, K.H.; Goldberg, V.M.; Kadiyala, S. The effect of implants loaded with autologous mesenchymal stem cells on the healing of canine segmental bone defects. J. Bone Joint Surg. Am. 1998, 80, 985–996. [Google Scholar] [PubMed]
- De Kok, I.J.; Drapeau, S.J.; Young, R.; Cooper, L.F. Evaluation of mesenchymal stem cells following implantation in alveolar sockets: A canine safety study. Int. J. Oral Maxillofac. Implant. 2005, 20, 511–518. [Google Scholar]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sheikh, Z.; Sima, C.; Glogauer, M. Bone Replacement Materials and Techniques Used for Achieving Vertical Alveolar Bone Augmentation. Materials 2015, 8, 2953-2993. https://doi.org/10.3390/ma8062953
Sheikh Z, Sima C, Glogauer M. Bone Replacement Materials and Techniques Used for Achieving Vertical Alveolar Bone Augmentation. Materials. 2015; 8(6):2953-2993. https://doi.org/10.3390/ma8062953
Chicago/Turabian StyleSheikh, Zeeshan, Corneliu Sima, and Michael Glogauer. 2015. "Bone Replacement Materials and Techniques Used for Achieving Vertical Alveolar Bone Augmentation" Materials 8, no. 6: 2953-2993. https://doi.org/10.3390/ma8062953
APA StyleSheikh, Z., Sima, C., & Glogauer, M. (2015). Bone Replacement Materials and Techniques Used for Achieving Vertical Alveolar Bone Augmentation. Materials, 8(6), 2953-2993. https://doi.org/10.3390/ma8062953