Comparison of Surface Strains of Polymeric Frameworks for Fixed Implant-Supported Prostheses: A Digital Image Correlation Study
Abstract
1. Introduction
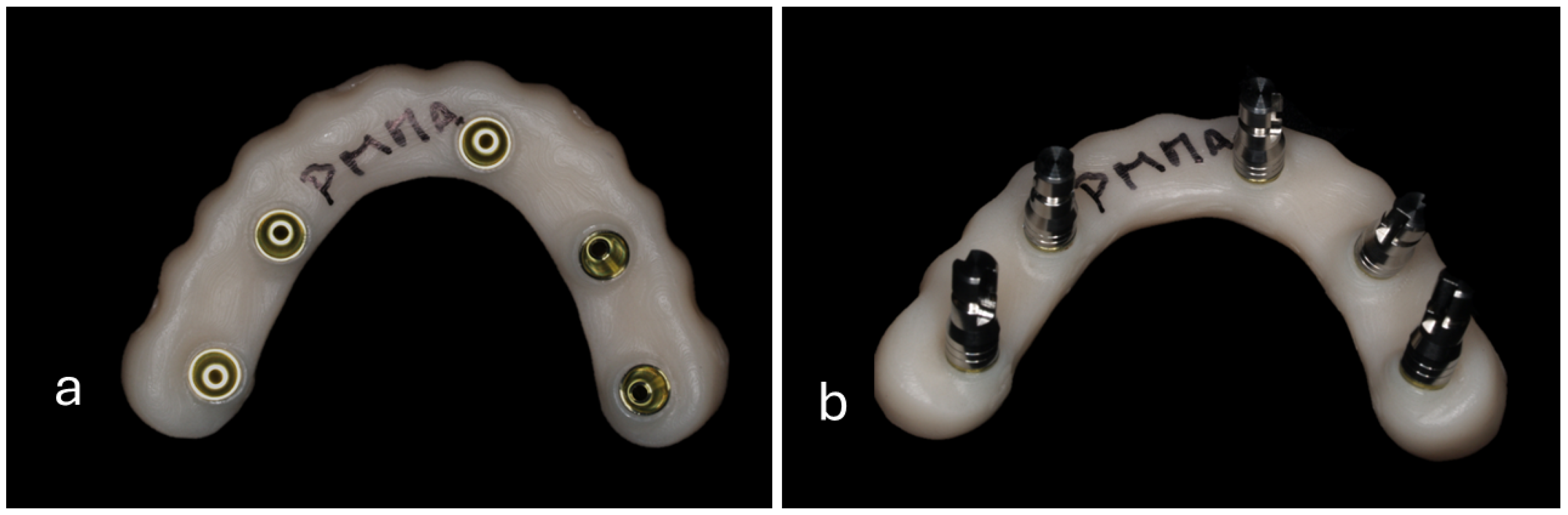
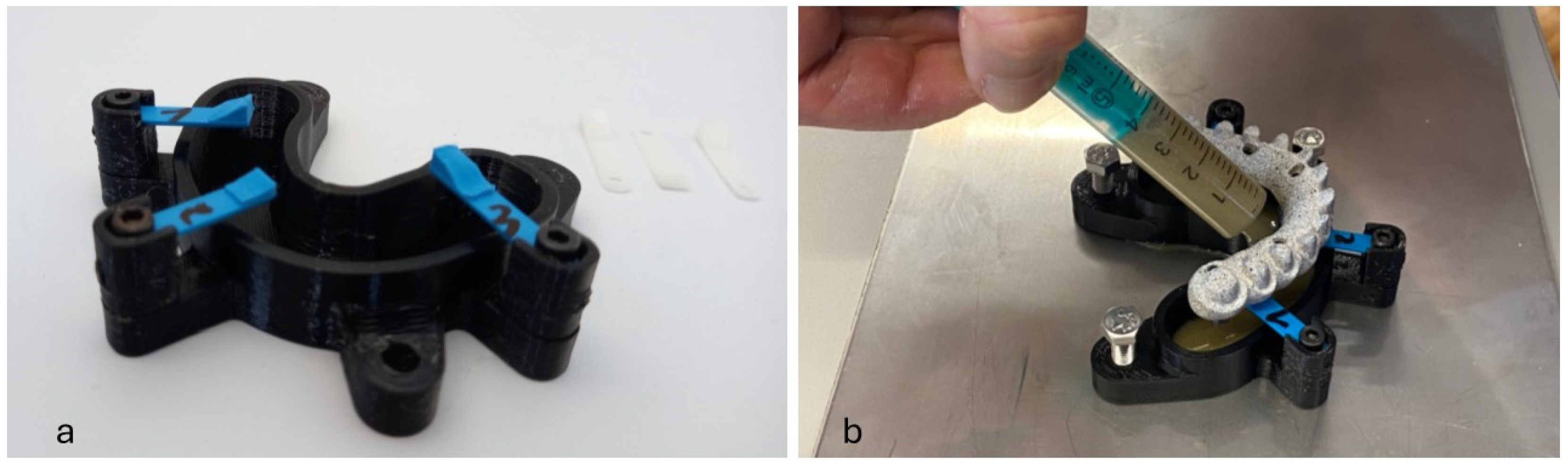
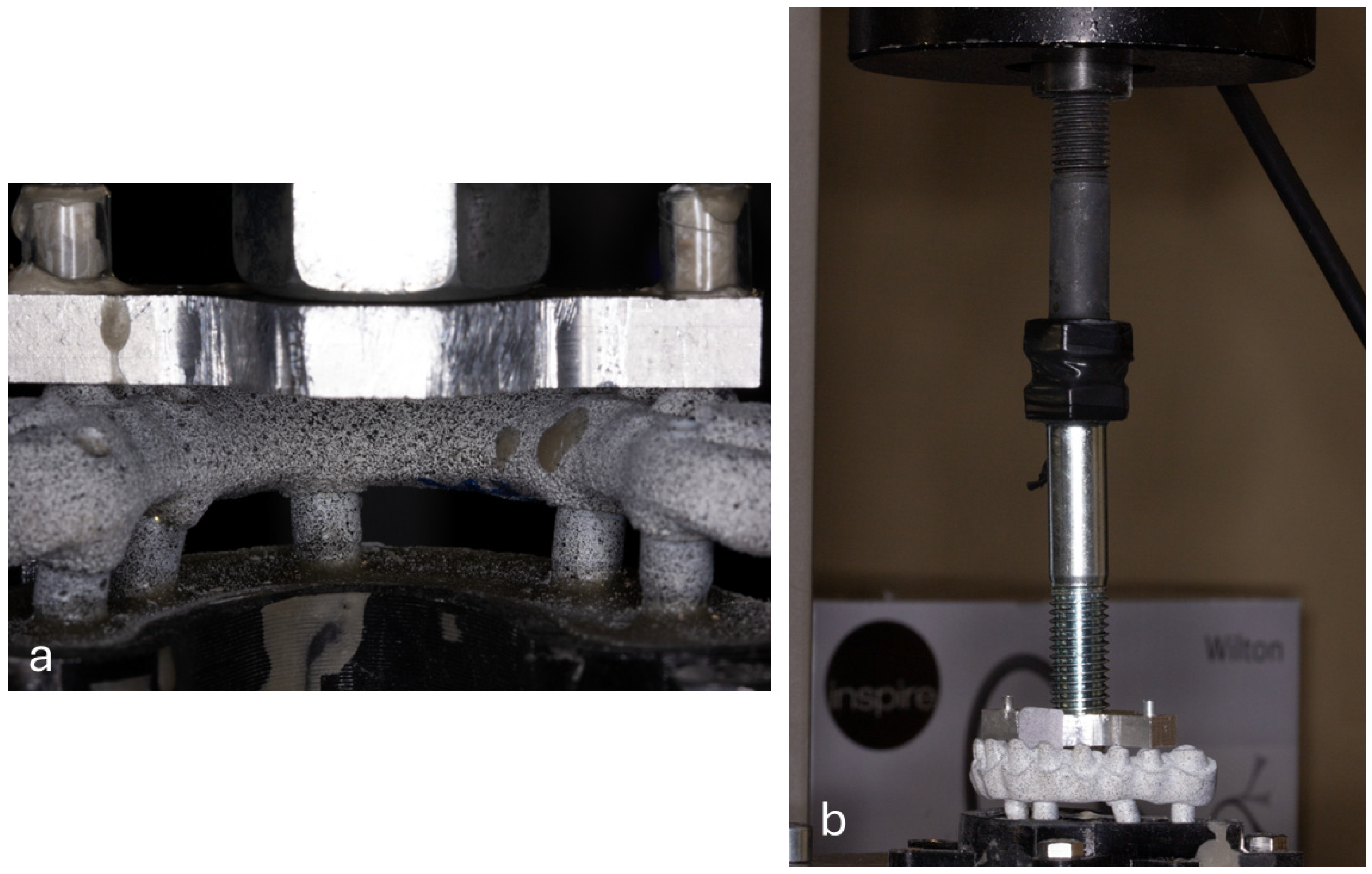
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Berniyanti, T.; Palupi, R.; Alkadasi, B.A.; Sari, K.P.; Putri, R.I.; Salma, N.; Prasita, S.; Regita, A.S. Oral Health-Related Quality of Life (OHRQoL) Analysis in Partially Edentulous Patients with and without Denture Therapy. Clin. Cosmet. Investig. Dent. 2023, 15, 89–98. [Google Scholar] [CrossRef] [PubMed]
- García-Minguillán, G.; Preciado, A.; Romeo, M.; Río, J.D.; Lynch, C.D.; Castillo-Oyagüe, R. Differences in self-perceived OHRQoL between fully dentate subjects and edentulous patients depending on their prosthesis type, socio-demographic profile, and clinical features. J. Dent. 2021, 114, 103756. [Google Scholar] [CrossRef] [PubMed]
- Garg, P.; Klineberg, I. Benefits of Contemporary Rehabilitation of Edentulism: A Statement. Int. J. Prosthodont. 2022, 35, 575–580. [Google Scholar] [CrossRef]
- Feng, Y.; Xiao, L.; Fu, L.L.; Gosau, M.; Vollkommer, T.; Speth, U.; Smeets, R.; Rutkowski, R.; Friedrich, R.E.; Yan, M. Global, Regional and National Burden of Edentulism and Periodontal Diseases from 1990 to 2021: Analysis of Risk Factors and Prediction of Trends in 2050. In Vivo 2025, 39, 1148–1161. [Google Scholar] [CrossRef]
- Sofi-Mahmudi, A.; Shamsoddin, E.; Khademioore, S.; Khazaei, Y.; Vahdati, A.; Tovani-Palone, M.R. Global, regional, and national survey on burden and Quality of Care Index (QCI) of orofacial clefts: Global burden of disease systematic analysis 1990–2019. PLoS ONE 2025, 20, e0317267. [Google Scholar] [CrossRef]
- Nilsson, S.; Stenport, V.F.; Nilsson, M.; Göthberg, C. A retrospective clinical study of fixed tooth- and implant-supported prostheses in titanium and cobalt-chromium-ceramic: 5-9-year follow-up. Clin. Oral Investig. 2022, 26, 6097–6103. [Google Scholar] [CrossRef] [PubMed]
- Teigen, K.; Jokstad, A. Dental implant suprastructures using cobalt-chromium alloy compared with gold alloy framework veneered with ceramic or acrylic resin: A retrospective cohort study up to 18 years. Clin. Oral Implants Res. 2012, 23, 853–860. [Google Scholar] [CrossRef] [PubMed]
- Vahnström, M.; Johansson, P.H.; Svanborg, P.; Stenport, V.F. Comparison of porcelain veneer fracture in implant-supported fixed full-arch prostheses with a framework of either titanium, cobalt-chromium, or zirconia: An in vitro study. Clin. Exp. Dent. Res. 2022, 8, 544–551. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; Sinada, N.; Ntovas, P.; Barmak, A.B.; Chochlidakis, K. Zirconia full-arch implant prostheses: Survival, complications, and prosthetic space dimensions with 115 edentulous jaws. J. Prosthodont. 2025, 34, 271–280. [Google Scholar] [CrossRef]
- Grosgogeat, B.; Vaicelyte, A.; Gauthier, R.; Janssen, C.; Le Borgne, M. Toxicological Risks of the Cobalt-Chromium Alloys in Dentistry: A Systematic Review. Materials 2022, 15, 5801. [Google Scholar] [CrossRef]
- Vaicelyte, A.; Janssen, C.; Le Borgne, M.; Grosgogeat, B. Cobalt–Chromium Dental Alloys: Metal Exposures, Toxicological Risks, CMR Classification, and EURegulatory Framework. Crystals 2020, 10, 1151. [Google Scholar] [CrossRef]
- Alqurashi, H.; Khurshid, Z.; Syed, A.U.Y.; Rashid Habib, S.; Rokaya, D.; Zafar, M.S. Polyetherketoneketone (PEKK): An emerging biomaterial for oral implants and dental prostheses. J. Adv. Res. 2021, 28, 87–95. [Google Scholar] [CrossRef]
- Bemelmanns, P.; Pfeiffer, P. Shock absorption capacities of mouthguards in different types and thicknesses. Int. J. Sports Med. 2001, 22, 149–153. [Google Scholar] [CrossRef]
- Menini, M.; Delucchi, F.; Bagnasco, F.; Baldi, D.; Canullo, L.; Setti, P.; Migliorati, M.; Simetti, E.; Pesce, P. Shock Absorption Capacity of High-Performance Polymers for Dental Implant-Supported Restorations: In Vitro Study. Dent. J. 2024, 12, 111. [Google Scholar] [CrossRef] [PubMed]
- Villefort, R.F.; Diamantino, P.J.S.; Zeidler, S.L.V.V.; Borges, A.L.S.; Silva-Concílio, L.R.; Saavedra, G.D.F.A.; Tribst, J.P.M. Mechanical Response of PEKK and PEEK As Frameworks for Implant-Supported Full-Arch Fixed Dental Prosthesis: 3D Finite Element Analysis. Eur. J. Dent. 2022, 16, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Almjaddr, M.; Saker, J. Effect of Different Cantilever Lengths in Polyether Ether Ketone Prosthetic Framework in All-on-Four Technique on Stress Distribution: A Three-Dimensional (3D) Finite Element Analysis. Cureus 2024, 16, e74544. [Google Scholar] [CrossRef]
- Elsayed, S.; Ahmed, Y.; El-Anwar, M.I.; Elddamony, E.; Ashraf, R. Influence of different polymeric materials of implant and attachment on stress distribution in implant-supported overdentures: A three-dimensional finite element study. BMC Oral Health 2025, 25, 166. [Google Scholar] [CrossRef]
- Kilic, S.; Caglar, I. An Investigation of Stress Distribution Between Two Different Implant Concept in Implant-Supported Maxillary Prostheses with Different Framework Materials: A Finite Element Study. Int. J. Prosthodont. 2024, 1–22. [Google Scholar] [CrossRef]
- Ogawa, T.; Dhaliwal, S.; Naert, I.; Mine, A.; Kronstrom, M.; Sasaki, K.; Duyck, J. Impact of implant number, distribution and prosthesis material on loading on implants supporting fixed prostheses. J. Oral Rehabil. 2010, 37, 525–531. [Google Scholar] [CrossRef]
- Reddy, K.U.K.; Seth, A.; Vuppuluri, A.; Verma, P.C.; Narala, S.K.R.; Babu, P.J.; Saravanan, P. Exploring the bio-mechanical behavior of PEEK and CFR-PEEK materials for dental implant applications using finite element analysis. J. Prosthodont. Res. 2025, 69, 41–48. [Google Scholar] [CrossRef]
- Sahin Hazir, D.; Sozen Yanik, I.; Guncu, M.B.; Canay, R.S. Biomechanical behavior of titanium, cobalt-chromium, zirconia, and PEEK frameworks in implant-supported prostheses: A dynamic finite element analysis. BMC Oral Health 2025, 25, 97. [Google Scholar] [CrossRef] [PubMed]
- LLC, M.t. MatWeb: Online Materials Information Resource. Available online: http://www.matweb.com (accessed on 28 February 2025).
- Dinçtürk B, A.; Garoushi, S.; Alp C, K.; Pk, V.; Mb, Ü.; Lassila, L. Fracture resistance of endocrowns made from different CAD/CAM materials after prolonged fatigue aging. Clin. Oral Investig. 2025, 29, 149. [Google Scholar] [CrossRef]
- Breitman, L.S.; Alsahafi, T.; Kofford, B.; Felton, D.A.; Prasad, S. Flexural strength and mode of failure of interim implant-supported fixed dental prostheses following different conversion techniques and structural reinforcement. J. Prosthet. Dent. 2025, 133, 543.e1–543.e8. [Google Scholar] [CrossRef] [PubMed]
- Bijelic-Donova, J.; Bath, A.K.; Rocca, G.T.; Bella, E.D.; Saratti, C.M. Can Fiber-reinforced Composites Increase the Fracture Resistance of Direct Composite Restorations in Structurally Compromised Teeth? A Systematic Review and Meta-analysis of Laboratory Studies. Oper. Dent. 2025, 50, E1–E29. [Google Scholar] [CrossRef] [PubMed]
- Lahoud, L.; Boulos, P.; Kahale, D.; Gheno, E.; Benedicenti, S.; Calasans-Maia, M.D.; Bassano, M.B.; Signore, A.; Dawalibi, A.; Nasr, E. Fracture load comparison of a new Fiber-Reinforced Composite and Zirconia in All-on-Four Prosthesis: An In Vitro Study. Int. J. Prosthodont. 2024, 1–21. [Google Scholar] [CrossRef]
- Garoushi, S.; Barlas, D.; Vallittu, P.K.; Uctasli, M.B.; Lassila, L. Fracture behavior of short fiber-reinforced CAD/CAM inlay restorations after cyclic fatigue aging. Odontology 2024, 112, 138–147. [Google Scholar] [CrossRef]
- Corbani, K.; Hardan, L.; Eid, R.; Skienhe, H.; Alharbi, N.; Ozcan, M.; Salameh, Z. Fracture Resistance of Three-unit Fixed Dental Prostheses Fabricated with Milled and 3D Printed Composite-based Materials. J. Contemp. Dent. Pract. 2021, 22, 985–990. [Google Scholar] [PubMed]
- Cahyanto, A.; Martins, M.V.S.; Bianchi, O.; Sudhakaran, D.P.; Sililkas, N.; Echeverrigaray, S.G.; Rosa, V. Graphene oxide increases PMMA’s resistance to fatigue and strength degradation. Dent. Mater. 2023, 39, 763–769. [Google Scholar] [CrossRef]
- Facenda, J.C.; Borba, M.; Benetti, P.; Borges, A.L.S.; Dutra, M.D.Z.; Corazza, P.H. Fatigue resistance of polymeric restorative materials: Effect of supporting substrate. Gen. Dent. 2023, 71, 24–29. [Google Scholar]
- Magne, P.; Milani, T. Short-fiber Reinforced MOD Restorations of Molars with Severely Undermined Cusps. J. Adhes. Dent. 2023, 25, 99–106. [Google Scholar] [CrossRef]
- Alarcon, J.V.; Engelmeier, R.L.; Powers, J.M.; Triolo, P.T. Wear testing of composite, gold, porcelain, and enamel opposing a removable cobalt-chromium partial denture alloy. J. Prosthodont. 2009, 18, 421–426. [Google Scholar] [CrossRef] [PubMed]
- Domagała, I.; Przystupa, K.; Firlej, M.; Pieniak, D.; Gil, L.; Borucka, A.; Naworol, I.; Biedziak, B.; Levkiv, M. Analysis of the Statistical Comparability of the Hardness and Wear of Polymeric Materials for Orthodontic Applications. Materials 2021, 14, 2925. [Google Scholar] [CrossRef]
- Harrison, A.; Huggett, R.; Handley, R.W. A correlation between abrasion resistance and other properties of some acrylic resins used in dentistry. J. Biomed. Mater. Res. 1979, 13, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Sayed, M.E.; Shetty, M.; Alqahtani, S.M.; Al Wadei, M.H.D.; Gupta, S.G.; Othman, A.A.A.; Alshehri, A.H.; Alqarni, H.; Mobarki, A.H.; et al. Physical and Mechanical Properties of 3D-Printed Provisional Crowns and Fixed Dental Prosthesis Resins Compared to CAD/CAM Milled and Conventional Provisional Resins: A Systematic Review and Meta-Analysis. Polymers 2022, 14, 2691. [Google Scholar] [CrossRef] [PubMed]
- Mackert, J.; El-Shewy, M.; Pannu, D.; Schoenbaum, T. Prosthetic complications and survival rates of metal-acrylic implant fixed complete dental prostheses: A retrospective study up to 10 years. J. Prosthet. Dent. 2024, 132, 766–771. [Google Scholar] [CrossRef]
- Palaniappan, S.; Celis, J.P.; Van Meerbeek, B.; Peumans, M.; Lambrechts, P. Correlating in vitro scratch test with in vivo contact free occlusal area wear of contemporary dental composites. Dent. Mater. 2013, 29, 259–268. [Google Scholar] [CrossRef]
- Almuhayya, S.; Alshahrani, R.; Alsania, R.; Albassam, A.; Alnemari, H.; Babaier, R. Biofilm Formation on Three High-Performance Polymeric CAD/CAM Composites: An In Vitro Study. Polymers 2025, 17, 676. [Google Scholar] [CrossRef]
- Khoury, P.; Kharouf, N.; Etienne, O.; Dillenseger, J.P.; Haikel, Y.; El-Damanhoury, H.M.; Irani, D.; Ozcan, M.; Salameh, Z. Physicochemical Properties and Bacterial Adhesion of Conventional and 3D Printed Complete Denture PMMA Materials: An. J. Contemp. Dent. Pract. 2024, 25, 1001–1008. [Google Scholar] [CrossRef]
- Shamieh, S.; Ribeiro, A.A.; Sulaiman, T.; Swift, E.J.; Vasconcellos, A.B. Biofilm attachment and mineralizing potential of contemporary restorative materials. Am. J. Dent. 2024, 37, 279–287. [Google Scholar]
- ISO 14801; Dentistry—Implants—Dynamic Loading Test for Endosseous Dental Implants. ISO: Geneva, Switzerland, 2016.
- Schimmel, M.; Araujo, M.; Abou-Ayash, S.; Buser, R.; Ebenezer, S.; Fonseca, M.; Heitz-Mayfield, L.J.; Holtzman, L.P.; Kamnoedboon, P.; Levine, R.; et al. Group 4 ITI Consensus Report: Patient benefits following implant treatment in partially and fully edentulous patients. Clin. Oral Implants Res. 2023, 34 (Suppl. S26), 257–265. [Google Scholar] [CrossRef]
- Srinivasan, M.; Kamnoedboon, P.; Angst, L.; Müller, F. Oral function in completely edentulous patients rehabilitated with implant-supported dental prostheses: A systematic review and meta-analysis. Clin. Oral Implants Res. 2023, 34 (Suppl. S26), 196–239. [Google Scholar] [CrossRef]
- Messias, A.; Karasan, D.; Nicolau, P.; Pjetursson, B.E.; Guerra, F. Rehabilitation of full-arch edentulism with fixed or removable dentures retained by root-form dental implants: A systematic review of outcomes and outcome measures used in clinical research in the last 10 years. J. Clin. Periodontol. 2023, 50, 38–54. [Google Scholar] [CrossRef] [PubMed]
- Schwitalla, A.D.; Spintig, T.; Kallage, I.; Müller, W.D. Flexural behavior of PEEK materials for dental application. Dent. Mater. 2015, 31, 1377–1384. [Google Scholar] [CrossRef]
- Yerliyurt, K.; Taşdelen, T.B.; Eğri, Ö.; Eğri, S. Flexural Properties of Heat-Polymerized PMMA Denture Base Resins Reinforced with Fibers with Different Characteristics. Polymers 2023, 15, 3211. [Google Scholar] [CrossRef]
- Bioloren. TRILOR®: The Solution for a Metal Free Dentistry. Available online: https://bioloren.com/english/trilor-fiber-disks-and-blocks (accessed on 28 February 2025).
- Tushar; Rani, P.; Ananya; Kumar, S.; Prakash, J.; Jayaprakash, M.B. Evaluation of Impact Strength and Flexural Strength of Polyether Ether Ketone vs. Computer-Aided Design/Computer-Aided Manufacturing Polymethyl Methacrylate Denture Base Materials: An In-Vitro Study. Cureus 2023, 15, e47929. [Google Scholar] [CrossRef] [PubMed]
- Valenti, C.; Federici, M.I.; Coniglio, M.; Betti, P.; Pancrazi, G.P.; Tulli, O.; Masciotti, F.; Nanussi, A.; Pagano, S. Mechanical and biological properties of polymer materials for oral appliances produced with additive 3D printing and subtractive CAD-CAM techniques compared to conventional methods: A systematic review and meta-analysis. Clin. Oral Investig. 2024, 28, 396. [Google Scholar] [CrossRef] [PubMed]
- Alghazzawi, T.F. Relation of Crown Failure Load to Flexural Strength for Three Contemporary Dental Polymers. Polymers 2023, 15, 4312. [Google Scholar] [CrossRef]
- Ruschel, G.H.; Gomes, É.; Silva-Sousa, Y.T.; Pinelli, R.G.P.; Sousa-Neto, M.D.; Pereira, G.K.R.; Spazzin, A.O. Mechanical properties and superficial characterization of a milled CAD-CAM glass fiber post. J. Mech. Behav. Biomed. Mater. 2018, 82, 187–192. [Google Scholar] [CrossRef]
- ISO 4049:2019; Dentistry—Polymer-Based Restorative Materials. ISO: Geneva, Switzerland, 2019.
- Muhsin, S.A.; Mohammed, E.K.; Bander, K. Finite Element Analysis: Connector Designs and Pontic Stress Distribution of Fixed Partial Denture Implant-Supported Metal Framework. J. Long Term Eff. Med. Implants 2024, 34, 33–47. [Google Scholar] [CrossRef]
- Huang, L.S.; Huang, Y.C.; Yuan, C.; Ding, S.J.; Yan, M. Biomechanical evaluation of bridge span with three implant abutment designs and two connectors for tooth-implant supported prosthesis: A finite element analysis. J. Dent. Sci. 2023, 18, 248–263. [Google Scholar] [CrossRef]
- Luft, R.L.; da Rosa, L.S.; Machado, P.S.; Valandro, L.F.; Sarkis-Onofre, R.; Pereira, G.K.R.; Bacchi, A. Influence of connector cross-sectional geometry on the load-bearing capacity under fatigue of implant-supported zirconia fixed partial prosthesis. J. Prosthet. Dent. 2022, 128, e1331–e1335. [Google Scholar] [CrossRef] [PubMed]
- Alshiddi, I.F.; Habib, S.R.; Zafar, M.S.; Bajunaid, S.; Labban, N.; Alsarhan, M. Fracture Load of CAD/CAM Fabricated Cantilever Implant-Supported Zirconia Framework: An In Vitro Study. Molecules 2021, 26, 2259. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Fehmer, V.; Sailer, I. EAO Position Paper: Material Selection for Implant-Supported Restorations. Int. J. Prosthodont. 2022, 35, 7–16. [Google Scholar] [CrossRef] [PubMed]


| Group | Load (N) | Displacement Mean ± SD (µm) | Ɛ1 Mean ± SD (µƐ) | Ɛ2 Mean ± SD (µƐ) | ƐVM Mean ± SD (µƐ) |
|---|---|---|---|---|---|
| G1-PEEK | 50 | 96.36 ± 34.72 | 693.55 ± 134.34 | −610.07 ± 92.27 | 858.64 ± 53.47 |
| 100 | 152.21 ± 9.26 | 1032.95 ± 73.67 | −941.95 ± 107.08 | 1392.81 ± 85.82 | |
| 150 | 220.87 ± 3.01 | 1330.36 ± 25.43 | −1297.15 ± 71.11 | 1830.72 ± 76.09 | |
| 200 | 257.69 ± 11.12 | 1580.74 ± 110.04 | −1535.52 ± 174.12 | 2165.73 ± 105.60 | |
| G2-PEKK | 50 | 72.92 ± 5.95 | 616.11 ± 75.85 | −675.71 ± 294.50 | 850.21 ± 190.72 |
| 100 | 92.95 ± 11.98 | 814.88 ± 25.03 | −799.74 ± 295.65 | 1074.91 ± 206.82 | |
| 150 | 114.11 ± 11.06 | 964.35 ± 100.38 | −987.93 ± 334.20 | 1309.28 ± 254.87 | |
| 200 | 134.66 ± 16.91 | 1088.21 ± 159.53 | −1075.86 ± 274.86 | 1483.69 ± 260.75 | |
| G3-PMMA | 50 | 40.95 ± 2.77 | 890.15 ± 134.74 | −874.92 ± 131.57 | 1133.10 ± 62.69 |
| 100 | 59.35 ± 16.39 | 1342.96 ± 328.18 | −1181.44 ± 178.25 | 1622.01 ± 61.56 | |
| 150 | 67.00 ± 8.59 | 1580.66 ± 302.56 | −1524.64 ± 151.81 | 1985.14 ± 215.66 | |
| 200 | 84.77 ± 11.07 | 1873.95 ± 501.22 | −1710.32 ± 117.94 | 2285.96 ± 215.17 | |
| G4-FRC | 50 | 34.22 ± 33.50 | 843.38 ± 191.48 | −545.71 ± 84.29 | 830.09 ± 156.02 |
| 100 | 35.36 ± 22.09 | 908.83 ± 48.88 | −667.63 ± 64.21 | 949.54 ± 52.15 | |
| 150 | 58.66 ± 50.43 | 1117.07 ± 67.94 | −775.20 ± 41.03 | 1156.69 ± 66.47 | |
| 200 | 74.50 ± 51.02 | 1205.39 ± 20.24 | −896.15 ± 104.68 | 1267.83 ± 47.38 |
| Material | Flexural Strength (MPa) | Elastic Modulus (GPa) | Observed Mechanical Behaviour in ISFP Frameworks |
|---|---|---|---|
| PEEK | 165 | 3–4 | High flexibility, increased displacement under load. |
| PEKK | 200 | 5.1 | Slightly stiffer than PEEK but still displays flexibility. |
| PMMA | 50–100 | 2–3 | High strain values, concerns over long-term performance. |
| FRC | 540 | 6–15 | Minimal displacement, rigidity and low strain values |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Messias, A.; Neto, M.A.; Piedade, A.P.; Amaro, A.; Krauser, J.T.; Guerra, F. Comparison of Surface Strains of Polymeric Frameworks for Fixed Implant-Supported Prostheses: A Digital Image Correlation Study. Materials 2025, 18, 1700. https://doi.org/10.3390/ma18081700
Messias A, Neto MA, Piedade AP, Amaro A, Krauser JT, Guerra F. Comparison of Surface Strains of Polymeric Frameworks for Fixed Implant-Supported Prostheses: A Digital Image Correlation Study. Materials. 2025; 18(8):1700. https://doi.org/10.3390/ma18081700
Chicago/Turabian StyleMessias, Ana, Maria Augusta Neto, Ana Paula Piedade, Ana Amaro, Jack T. Krauser, and Fernando Guerra. 2025. "Comparison of Surface Strains of Polymeric Frameworks for Fixed Implant-Supported Prostheses: A Digital Image Correlation Study" Materials 18, no. 8: 1700. https://doi.org/10.3390/ma18081700
APA StyleMessias, A., Neto, M. A., Piedade, A. P., Amaro, A., Krauser, J. T., & Guerra, F. (2025). Comparison of Surface Strains of Polymeric Frameworks for Fixed Implant-Supported Prostheses: A Digital Image Correlation Study. Materials, 18(8), 1700. https://doi.org/10.3390/ma18081700











