Evaluation of Microhardness and Compressive Strength of Mineral Trioxide Aggregate Modified by Addition of Short Glass Fibers and Shredded Polyglycolic Acid Sutures
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Microhardness and Compressive Strength
3.2. SEM Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Modaresi, J.; Mokhtari, F.; Khodarahmi, E. In vitro comparison of the marginal adaptation of cold ceramic sealer with the single-cone obturation technique versus AH-26 sealer with the lateral compaction technique in single-canal teeth. BMC Oral Health 2025, 25, 69. [Google Scholar]
- Pedano, M.S.; Li, X.; Yoshihara, K.; Landuyt, K.V.; Van Meerbeek, B. Cytotoxicity and Bioactivity of Dental Pulp-Capping Agents towards Human Tooth-Pulp Cells: A Systematic Review of In-Vitro Studies and Meta-Analysis of Randomized and Controlled Clinical Trials. Materials 2020, 13, 2670. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Xiao, Y.; Song, W.; Ye, L.; Yang, C.; Xing, Y.; Yuan, Z. Clinical application of calcium silicate-based bioceramics in endodontics. J. Transl. Med. 2023, 21, 853. [Google Scholar] [PubMed]
- von Arx, T.; Jensen, S.S.; Janner, S.F.M.; Hänni, S.; Bornstein, M.M. A 10-year Follow-up Study of 119 Teeth Treated with Apical Surgery and Root-end Filling with Mineral Trioxide Aggregate. J. Endod. 2019, 45, 394–401. [Google Scholar]
- Kayahan, M.B.; Nekoofar, M.H.; McCann, A.; Sunay, H.; Kaptan, R.F.; Meraji, N.; Dummer, P.M. Effect of acid etching procedures on the compressive strength of 4 calcium silicate-based endodontic cements. J. Endod. 2013, 39, 1646–1648. [Google Scholar]
- Pushpalatha, C.; Dhareshwar, V.; Sowmya, S.V.; Augustine, D.; Vinothkumar, T.S.; Renugalakshmi, A.; Shaiban, A.; Kakti, A.; Bhandi, S.H.; Dubey, A.; et al. Modified Mineral Trioxide Aggregate-A Versatile Dental Material: An Insight on Applications and Newer Advancements. Front. Bioeng. Biotechnol. 2022, 10, 941826. [Google Scholar]
- Formosa, L.M.; Mallia, B.; Camilleri, J. A quantitative method for determining the antiwashout characteristics of cement-based dental materials including mineral trioxide aggregate. Int. Endod. J. 2013, 46, 179–186. [Google Scholar]
- Eskandarinezhad, M.; Ghodrati, M.; Pournaghi Azar, F.; Jafari, F.; Samadi Pakchin, P.; Abdollahi, A.A.; Sadrhaghighi, A.H.; Rezvan, F. Effect of Incorporating Hydroxyapatite and Zinc Oxide Nanoparticles on the Compressive Strength of White Mineral Trioxide Aggregate. J. Dent. 2020, 21, 300–306. [Google Scholar]
- Kucukyildiz, E.N.; Dayi, B.; Altin, S.; Yigit, O. In vitro comparison of physical, chemical, and mechanical properties of graphene nanoplatelet added Angelus mineral trioxide aggregate to pure Angelus mineral trioxide aggregate and calcium hydroxide. Microsc. Res. Tech. 2021, 84, 929–942. [Google Scholar]
- Nagas, E.; Cehreli, Z.C.; Uyanik, O.; Vallittu, P.K.; Lassila, L.V. Reinforcing Effect of Glass Fiber-incorporated ProRoot MTA and Biodentine as Intraorifice Barriers. J. Endod. 2016, 42, 1673–1676. [Google Scholar]
- Abusrewil, S.; Scott, J.A.; Alqahtani, S.S.; Butcher, M.C.; Tiba, M.; Kumar, C.; Mulvihill, D.M.; Ramage, G.; McLean, W. The Effect of Chitosan Incorporation on Physico-Mechanical and Biological Characteristics of a Calcium Silicate Filling Material. Dent. J. 2024, 12, 100. [Google Scholar] [CrossRef] [PubMed]
- Parirokh, M.; Torabinejad, M. Mineral trioxide aggregate: A comprehensive literature review—Part I: Chemical, physical, and antibacterial properties. J. Endod. 2010, 36, 16–27. [Google Scholar] [PubMed]
- Mariyam, M.; Sunarintyas, S.; Nuryono, N. Improving mechanical, biological, and adhesive properties of synthesized mineral trioxide aggregate by adding chitosan. Inorg. Chem. Commun. 2023, 149, 110446. [Google Scholar]
- Camilleri, J. Mineral trioxide aggregate: Present and future developments. Endod. Top. 2015, 32, 31–46. [Google Scholar]
- Kogan, P.; He, J.; Glickman, G.N.; Watanabe, I. The effects of various additives on setting properties of MTA. J. Endod. 2006, 32, 569–572. [Google Scholar]
- Hernandez-Delgadillo, R.; Del Angel-Mosqueda, C.; Solís-Soto, J.M.; Munguia-Moreno, S.; Pineda-Aguilar, N.; Sánchez-Nájera, R.I.; Chellam, S.; Cabral-Romero, C. Antimicrobial and antibiofilm activities of MTA supplemented with bismuth lipophilic nanoparticles. Dent. Mater. J. 2017, 36, 503–510. [Google Scholar]
- Tien, N.; Lee, J.J.; Lee, A.K.; Lin, Y.H.; Chen, J.X.; Kuo, T.Y.; Shie, M.Y. Additive Manufacturing of Caffeic Acid-Inspired Mineral Trioxide Aggregate/Poly-ε-Caprolactone Scaffold for Regulating Vascular Induction and Osteogenic Regeneration of Dental Pulp Stem Cells. Cells 2021, 10, 2911. [Google Scholar] [CrossRef]
- Magazzini, L.; Grilli, S.; Fenni, S.E.; Donetti, A.; Cavallo, D.; Monticelli, O. The Blending of Poly(glycolic acid) with Polycaprolactone and Poly(l-lactide): Promising Combinations. Polymers 2021, 13, 2780. [Google Scholar] [CrossRef]
- Safwat, E.M.; Khater, A.G.A.; Abd-Elsatar, A.G.; Khater, G.A. Glass fiber-reinforced composites in dentistry. Bull. Natl. Res. Cent. 2021, 45, 190. [Google Scholar]
- Żuk-Grajewska, E.; Saunders, W.P.; Chadwick, R.G. Fracture resistance of human roots filled with mineral trioxide aggregate mixed with phosphate-buffered saline, with and without calcium hydroxide pre-medication. Int. Endod. J. 2021, 54, 439–453. [Google Scholar]
- Tavakoli, M.; Araghi, S.; Fathi, A.; Jalalian, S. Comparison of coronal sealing of flowable composite, resin-modified glass ionomer, and mineral trioxide aggregate in endodontically treated teeth: An in-vitro study. Dent. Res. J. 2024, 21, 13. [Google Scholar]
- Mehta, S.; Ramugade, M.; Abrar, S.; Sapkale, K.; Giuliani, V.; Burbano Balseca, M.J. Evaluation of coronal microleakage of intra-orifice barrier materials in endodontically treated teeth: A systematic review. J. Conserv. Dent. 2022, 25, 588–595. [Google Scholar]
- Nagas, E.; Uyanik, O.; Altundasar, E.; Durmaz, V.; Cehreli, Z.C.; Vallittu, P.K.; Lassila, L.V. Effect of different intraorifice barriers on the fracture resistance of roots obturated with Resilon or gutta-percha. J. Endod. 2010, 36, 1061–1063. [Google Scholar] [PubMed]
- ISO 9917-1:2007; Dentistry: Water-Based Cements. Part 1: Powder/Liquid Acid-Base Cements, 2nd ed. ISO: Geneva, Switzerland, 2007; p. 23.
- Ha, W.N.; Nicholson, T.; Kahler, B.; Walsh, L.J. Mineral Trioxide Aggregate-A Review of Properties and Testing Methodologies. Materials 2017, 10, 1261. [Google Scholar] [CrossRef] [PubMed]
- Walsh, R.M.; Woodmansey, K.F.; Glickman, G.N.; He, J. Evaluation of compressive strength of hydraulic silicate-based root-end filling materials. J. Endod. 2014, 40, 969–972. [Google Scholar]
- Camilleri, J. Evaluation of the physical properties of an endodontic Portland cement incorporating alternative radiopacifiers used as root-end filling material. Int. Endod. J. 2010, 43, 231–240. [Google Scholar]
- Camilleri, J.; Wang, C.; Kandhari, S.; Heran, J.; Shelton, R.M. Methods for testing solubility of hydraulic calcium silicate cements for root-end filling. Sci. Rep. 2022, 12, 7100. [Google Scholar]
- Dardik, H.; Dardik, I.; Laufman, H. Clinical use of polyglycolic acid polymer as a new absorbable synthetic suture. Am. J. Surg. 1971, 121, 656–660. [Google Scholar]
- Deeken, C.R.; Matthews, B.D. Characterization of the Mechanical Strength, Resorption Properties, and Histologic Characteristics of a Fully Absorbable Material (Poly-4-hydroxybutyrate-PHASIX Mesh) in a Porcine Model of Hernia Repair. ISRN Surg. 2013, 2013, 238067. [Google Scholar]
- Niu, L.N.; Jiao, K.; Wang, T.D.; Zhang, W.; Camilleri, J.; Bergeron, B.E.; Feng, H.L.; Mao, J.; Chen, J.H.; Pashley, D.H.; et al. A review of the bioactivity of hydraulic calcium silicate cements. J. Dent. 2014, 42, 517–533. [Google Scholar]
- Singh, N.B. Effect of gluconates on the hydration of cement. Cem. Concr. Res. 1976, 6, 455–460. [Google Scholar]
- Chaudhari, O.A.; Biernacki, J.J.; Northrup, S.H. Effect of carboxylic and hydroxycarboxylic acids on cement hydration: Experimental and molecular modeling study. J. Mater. Sci. 2017, 52, 13719–13735. [Google Scholar]
- Rai, S.; Singh, N.B.; Singh, N.P. Interaction of tartaric acid during hydration of Portland cement. Ind. J. Chem. Technol. 2006, 13, 256–261. [Google Scholar]
- Khan, A.S.; Azam, M.T.; Khan, M.; Mian, S.A.; Ur Rehman, I. An update on glass fiber dental restorative composites: A systematic review. Mater. Sci. Eng. C Mater. Biol. Appl. 2015, 47, 26–39. [Google Scholar]
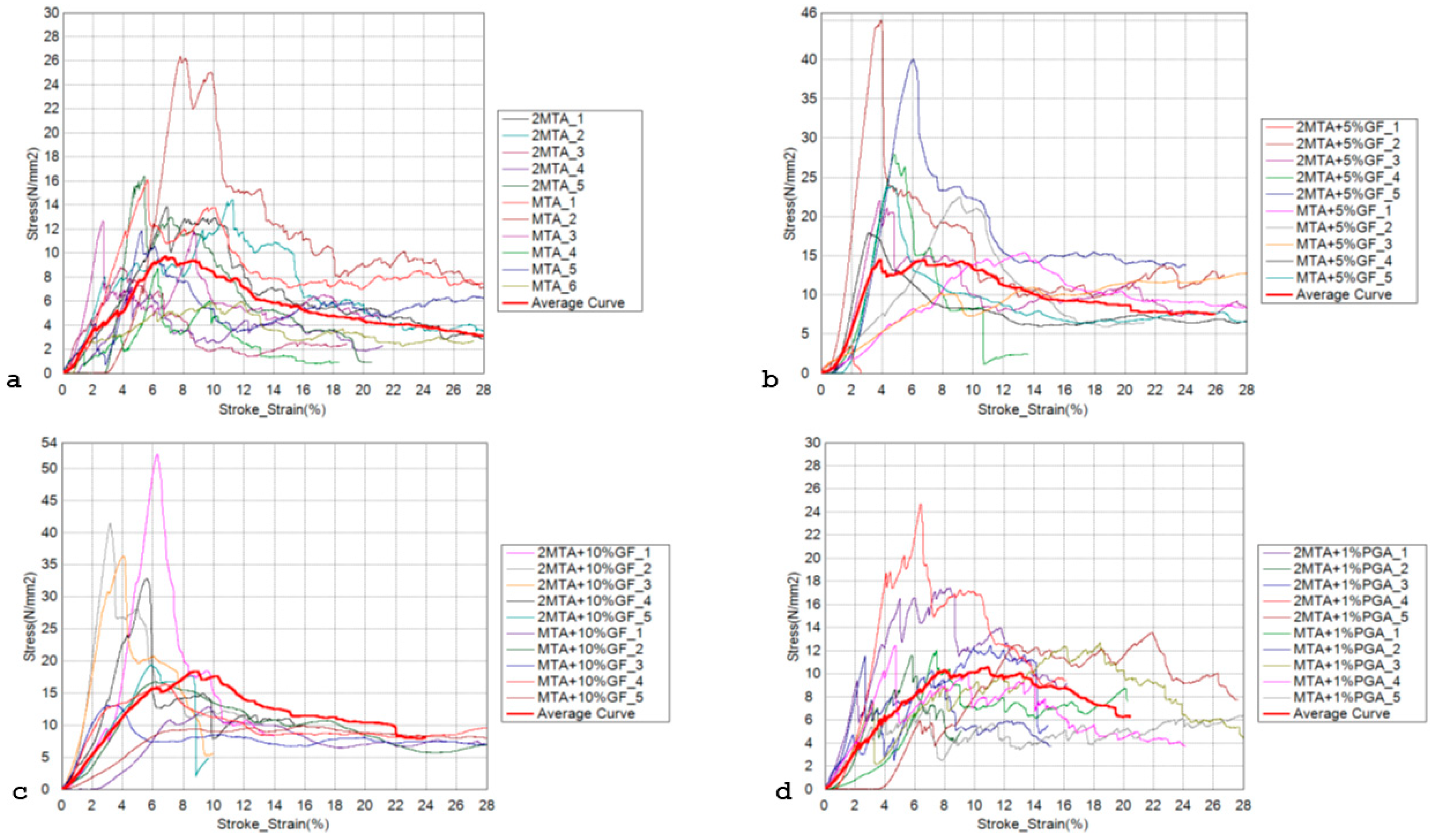

| Compressive Strength [MPa] | Compressive Modulus [MPa] | |||
|---|---|---|---|---|
| Material | MM MTA | Mean | 11.594 a | 279.254 a |
| Standard deviation | 3.731 | 168.343 | ||
| Minimum | 5.927 | 115.069 | ||
| Percentile 25 | 8.737 | 152.237 | ||
| Median | 12.250 | 203.753 | ||
| Percentile 75 | 14.428 | 423.411 | ||
| Maximum | 16.409 | 563.189 | ||
| MM MTA + 5% SGF | Mean | 23.189 b | 249.857 a | |
| Standard deviation | 12.317 | 114.570 | ||
| Minimum | 3.569 | 125.323 | ||
| Percentile 25 | 15.355 | 168.728 | ||
| Median | 22.698 | 245.659 | ||
| Percentile 75 | 27.927 | 280.553 | ||
| Maximum | 45.005 | 474.254 | ||
| MM MTA + 10% SGF | Mean | 25.149 b | 286.228 a | |
| Standard deviation | 14.540 | 137.843 | ||
| Minimum | 9.884 | 117.869 | ||
| Percentile 25 | 13.104 | 165.564 | ||
| Median | 18.039 | 272.778 | ||
| Percentile 75 | 36.803 | 344.381 | ||
| Maximum | 52.197 | 536.189 | ||
| MM MTA + 1% PGA | Mean | 13.547 a | 215.058 a | |
| Standard deviation | 4.639 | 88.883 | ||
| Minimum | 7.085 | 67.123 | ||
| Percentile 25 | 11.602 | 144.983 | ||
| Median | 12.450 | 205.464 | ||
| Percentile 75 | 13.552 | 289.389 | ||
| Maximum | 24.666 | 337.280 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Filipović, J.; Ivanišević, A.; Matijević, J.; Pilipović, A.; Zajc, I.; Miletić, I.; Baraba, A. Evaluation of Microhardness and Compressive Strength of Mineral Trioxide Aggregate Modified by Addition of Short Glass Fibers and Shredded Polyglycolic Acid Sutures. Materials 2025, 18, 1491. https://doi.org/10.3390/ma18071491
Filipović J, Ivanišević A, Matijević J, Pilipović A, Zajc I, Miletić I, Baraba A. Evaluation of Microhardness and Compressive Strength of Mineral Trioxide Aggregate Modified by Addition of Short Glass Fibers and Shredded Polyglycolic Acid Sutures. Materials. 2025; 18(7):1491. https://doi.org/10.3390/ma18071491
Chicago/Turabian StyleFilipović, Josip, Ana Ivanišević, Jurica Matijević, Ana Pilipović, Ivan Zajc, Ivana Miletić, and Anja Baraba. 2025. "Evaluation of Microhardness and Compressive Strength of Mineral Trioxide Aggregate Modified by Addition of Short Glass Fibers and Shredded Polyglycolic Acid Sutures" Materials 18, no. 7: 1491. https://doi.org/10.3390/ma18071491
APA StyleFilipović, J., Ivanišević, A., Matijević, J., Pilipović, A., Zajc, I., Miletić, I., & Baraba, A. (2025). Evaluation of Microhardness and Compressive Strength of Mineral Trioxide Aggregate Modified by Addition of Short Glass Fibers and Shredded Polyglycolic Acid Sutures. Materials, 18(7), 1491. https://doi.org/10.3390/ma18071491









