Flexural Strength, Fatigue Behavior, and Microhardness of Three-Dimensional (3D)-Printed Resin Material for Indirect Restorations: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Protocol
2.2. Literature Search
2.3. Eligibility Criteria
2.4. Criteria for Article Selection
2.5. Selection, Management and Data Collection
2.6. Assessment of Risk of Bias and Methodological Quality
2.7. Analysis and Synthesis of Data
3. Results
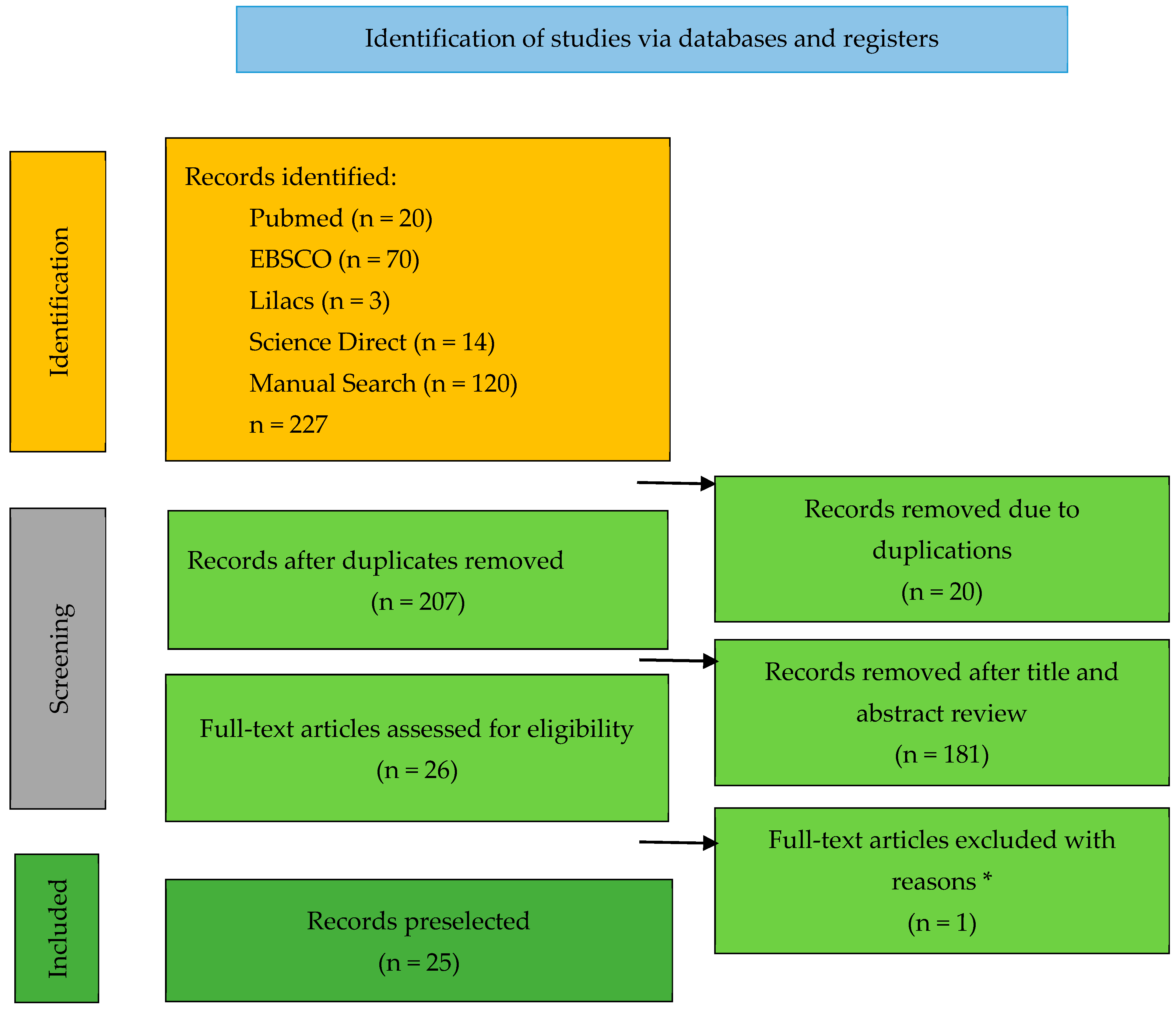
3.1. Search and Selection
3.2. Assessment of Risk of Bias and Methodological Quality
4. Discussion
5. Conclusions
- -
- In general, 3D-printed resins showed lower flexural strength, fatigue behavior, and microhardness compared to other types of resin used for the fabrication of temporary and permanent restorations.
- -
- The technology used, type of 3D printer, polymerization time, and post-processing processes are factors that significantly affect the flexural strength, fatigue behavior, and microhardness of 3D-printed resins.
- -
- It has been shown that the main application of 3D-printed resins in prosthodontics is the manufacturing of dental crowns and bridges. Therefore, this technology would also have other applications in other fields of dentistry, such as implantology and orthodontics. It also can be applied in biomedicine within the manufacture of prothesis and orthoses.
- -
- Finally, it should be considered based on the existing evidence that additive technology has promising future prospects for temporary and definitive dental restorations; so, further studies on this technology and materials should be conducted.
Funding
Conflicts of Interest
References
- Prause, E.; Malgaj, T.; Kocjan, A.; Beuer, F.; Hey, J.; Jevnikar, P.; Schmidt, F. Mechanical properties of 3D-printed and milled composite resins for definitive restorations: An in vitro comparison of initial strength and fatigue behavior. J. Esthet. Restor. Dent. 2024, 36, 391–401. [Google Scholar] [CrossRef] [PubMed]
- Kessler, A.; Hickel, R.; Reymus, M. 3D Printing in Dentistry—State of the Art. Oper. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Hwangbo, N.-K.; Nam, N.-E.; Choi, J.-H.; Kim, J.-E. Effects of the Washing Time and Washing Solution on the Biocompatibility and Mechanical Properties of 3D Printed Dental Resin Materials. Polymers 2021, 13, 4410. [Google Scholar] [CrossRef] [PubMed]
- Daher, R.; Ardu, S.; di Bella, E.; Krejci, I.; Duc, O. Efficiency of 3D-printed composite resin restorations compared with subtractive materials: Evaluation of fatigue behavior, cost, and time of production. J. Prosthet. Dent. 2022, 131, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Ligon, S.C.; Liska, R.; Stampfl, J.; Gurr, M.; Mülhaupt, R. Polymers for 3D Printing and Customized Additive Manufacturing. Chem. Rev. 2017, 117, 10212–10290. [Google Scholar] [CrossRef]
- Sandmair, M.N.; Kleber, C.; Ströbele, D.A.; von See, C. AFM Analysis of a Three-Point Flexure Tested, 3D Printing Definitive Restoration Material for Dentistry. J. Funct. Biomater. 2023, 14, 152. [Google Scholar] [CrossRef] [PubMed]
- Flury, S.; Diebold, E.; Peutzfeldt, A.; Lussi, A. Effect of artificial toothbrushing and water storage on the surface roughness and micromechanical properties of tooth-colored CAD-CAM materials. J. Prosthet. Dent. 2017, 117, 767–774. [Google Scholar] [CrossRef]
- Graf, T.; Erdelt, K.-J.; Güth, J.-F.; Edelhoff, D.; Schubert, O.; Schweiger, J. Influence of Pre-Treatment and Artificial Aging on the Retention of 3D-Printed Permanent Composite Crowns. Biomedicines 2022, 10, 2186. [Google Scholar] [CrossRef] [PubMed]
- Balestra, D.; Lowther, M.; Goracci, C.; Mandurino, M.; Cortili, S.; Paolone, G.; Louca, C.; Vichi, A. 3D Printed Materials for Permanent Restorations in Indirect Restorative and Prosthetic Dentistry: A Critical Review of the Literature. Materials 2024, 17, 1380. [Google Scholar] [CrossRef] [PubMed]
- Temizci, T.; Bozoğulları, H.N. Effect of thermocycling on the mechanical properties of permanent composite-based CAD-CAM restorative materials produced by additive and subtractive manufacturing techniques. BMC Oral Health 2024, 24, 334. [Google Scholar] [CrossRef]
- Nam, N.-E.; Hwangbo, N.-K.; Kim, J.-E. Effects of surface glazing on the mechanical and biological properties of 3D printed permanent dental resin materials. J. Prosthodont. Res. 2023, 68, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.G.; Yang, K.R.; Lerner, H.; Porrà, T.; Khachatryan, L.G.; Gordienko, I.D.; Admakin, O. 3D-printed short-span hybrid composite implant-supported restorations fabricated through tilting stereolithography: A retrospective clinical study on 85 patients with 1 year of follow-up. J. Dent. 2024, 147, 105095. [Google Scholar] [CrossRef]
- Al-Halabi, M.N.; Bshara, N.; Nassar, J.A.; Comisi, J.C.; Alawa, L. Comparative assessment of novel 3d printed resin crowns versus direct celluloid crowns in restoring pulp treated primary molars. J. Evid. Based Dent. Pract. 2022, 22, 101664. [Google Scholar] [CrossRef] [PubMed]
- Nabil, M.S.; Mahanna, F.F.; Said, M.M. Evaluation of masticatory performance and patient satisfaction for conventional and 3D-printed implant overdentures: A randomized crossover study. BMC Oral Health 2024, 24, 672. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Atria, P.J.; Bordin, D.; Marti, F.; Nayak, V.V.; Conejo, J.; Jalkh, E.B.; Witek, L.; Sampaio, C.S. 3D-printed resins for provisional dental restorations: Comparison of mechanical and biological properties. J. Esthet. Restor. Dent. 2022, 34, 804–815. [Google Scholar] [CrossRef]
- ISO 6872:2024; Dentistry—Ceramic Materials. ISO: Geneva, Switzerland, 2024.
- Park, S.-M.; Park, J.-M.; Kim, S.-K.; Heo, S.-J.; Koak, J.-Y. Flexural Strength of 3D-Printing Resin Materials for Provisional Fixed Dental Prostheses. Materials 2020, 13, 3970. [Google Scholar] [CrossRef] [PubMed]
- Aati, S.; Akram, Z.; Ngo, H.; Fawzy, A.S. Development of 3D printed resin reinforced with modified ZrO2 nanoparticles for long-term provisional dental restorations. Dent. Mater. 2021, 37, e360–e374. [Google Scholar] [CrossRef] [PubMed]
- Bayarsaikhan, E.; Gu, H.; Hwangbo, N.-K.; Lim, J.-H.; Shim, J.-S.; Lee, K.-W.; Kim, J.-E. Influence of different postcuring parameters on mechanical properties and biocompatibility of 3D printed crown and bridge resin for temporary restorations. J. Mech. Behav. Biomed. Mater. 2022, 128, 105127. [Google Scholar] [CrossRef]
- ISO 10477; Dentistry—Polymer-Based Crown and Veneering Materials. ISO: Geneva, Switzerland, 2020.
- Karaoğlanoğlu, S.; Aydın, N.; Oktay, E.; Ersöz, B. Comparison of the Surface Properties of 3D-printed Permanent Restorative Resins and Resin-based CAD/CAM Blocks. Oper. Dent. 2023, 48, 588–598. [Google Scholar] [CrossRef] [PubMed]
- Simoneti, D.M.; Pereira-Cenci, T.; dos Santos, M.B.F. Comparison of material properties and biofilm formation in interim single crowns obtained by 3D printing and conventional methods. J. Prosthet. Dent. 2022, 127, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Bora, P.V.; Ahmed, A.S.; Alford, A.; Pitttman, K.; Thomas, V.; Lawson, N.C. Characterization of materials used for 3D printing dental crowns and hybrid prostheses. J. Esthet. Restor. Dent. 2024, 36, 220–230. [Google Scholar] [CrossRef] [PubMed]
- ISO 4049; Dentistry—Polymer-Based Restorative Materials. ISO: Geneva, Switzerland, 2019.
- Abad-Coronel, C.; Chimbo, D.V.; Lupú, B.; Pacurucu, M.; Fárez, M.V.; Fajardo, J.I. Comparative Analysis of the Structural Weights of Fixed Prostheses of Zirconium Dioxide, Metal Ceramic, PMMA and 3DPP Printing Resin—Mechanical Implications. Dent. J. 2023, 11, 249. [Google Scholar] [CrossRef] [PubMed]
- Abad-Coronel, C.; Bravo, M.; Tello, S.; Cornejo, E.; Paredes, Y.; Paltan, C.A.; Fajardo, J.I. Fracture Resistance Comparative Analysis of Milled-Derived vs. 3D-Printed CAD/CAM Materials for Single-Unit Restorations. Polymers 2023, 15, 3773. [Google Scholar] [CrossRef]
- Chung, S.; Jiang, E.-S.; Lim, B.-S.; Kim, S.-H.; Chang, J. Multi-peak Light-emitting Diode Curing Units and Polymerization of 3D-printed Crown and Bridge Resin. Oper. Dent. 2024, 49, 98–109. [Google Scholar] [CrossRef] [PubMed]
- Sahin, Z.; Ozer, N.E.; Yιkιcι, C.; Kιlιçarslan, M.A. Mechanical Characteristics of Composite Resins Produced by Additive and Subtractive Manufacturing. Eur. J. Prosthodont. Restor. Dent. 2023, 31, 278–285. [Google Scholar] [PubMed]
- Abdulkareem, M.A.; Al-Shamma, A.M.W. Marginal Adaptation and Fracture Resistance of 3D Printed and CAD/CAM Milled Definitive Resin Matrix Ceramic Crowns. Int. J. Comput. Dent. 2023, 27, 355–363. [Google Scholar]
- Schönhoff, L.M.; Mayinger, F.; Eichberger, M.; Reznikova, E.; Stawarczyk, B. 3D printing of dental restorations: Mechanical properties of thermoplastic polymer materials. J. Mech. Behav. Biomed. Mater. 2021, 119, 104544. [Google Scholar] [CrossRef] [PubMed]
- Soto-Montero, J.; de Castro, E.F.; Romano, B.D.C.; Nima, G.; Shimokawa, C.A.; Giannini, M. Color alterations, flexural strength, and microhardness of 3D printed resins for fixed provisional restoration using diferentes post-curing times. Dent. Mater. 2022, 38, 1271–1282. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, A.K.C.; de Freitas, R.F.C.P.; de Carvalho, I.H.G.; de Miranda, L.M.; da Silva, N.R.; de Fátima Dantas de Almeida, L.; Zhang, Y.; da Fonte Porto Carreiro, A.; de Assunção e Souza, R.O. Flexural strength, surface roughness, micro-CT analysis, and microbiological adhesion of a 3D-printed temporary crown material. Clin. Oral Investig. 2023, 27, 2207–2220. [Google Scholar] [CrossRef]
- Alageel, O.; Alhijji, S.; Alsadon, O.; Alsarani, M.; Gomawi, A.A.; Alhotan, A. Trueness, Flexural Strength, and Surface Properties of Various Three-Dimensional (3D) Printed Interim Restorative Materials after Accelerated Aging. Polymers 2023, 15, 3040. [Google Scholar] [CrossRef] [PubMed]
- Scotti, C.K.; Velo, M.M.d.A.C.; Rizzante, F.A.P.; Nascimento, T.R.d.L.; Mondelli, R.F.L.; Bombonatti, J.F.S. Physical and surface properties of a 3D-printed composite resin for a digital workflow. J. Prosthet. Dent. 2020, 124, 614.e1–614.e5. [Google Scholar] [CrossRef]
- Grzebieluch, W.; Kowalewski, P.; Grygier, D.; Rutkowska-Gorczyca, M.; Kozakiewicz, M.; Jurczyszyn, K. Printable and Machinable Dental Restorative Composites for CAD/CAM Application—Comparison of Mechanical Properties, Fractographic, Texture and Fractal Dimension Analysis. Materials 2021, 14, 4919. [Google Scholar] [CrossRef]
- Alshamrani, A.A.; Raju, R.; Ellakwa, A. Effect of Printing Layer Thickness and Postprinting Conditions on the Flexural Strength and Hardness of a 3D-Printed Resin. BioMed Res. Int. 2022, 2022, 8353137. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Morillo, J.A.; Att, W.; Özcan, M. Chemical Composition, Knoop Hardness, Surface Roughness, and Adhesion Aspects of Additively Manufactured Dental Interim Materials. J. Prosthodont. 2021, 30, 698–705. [Google Scholar] [CrossRef] [PubMed]
- Alageel, O.; Alsadon, O.; Almansour, H.; Alshehri, A.; Alhabbad, F.; Alsarani, M. Assessment of effect of accelerated aging on interim fixed dental materials using digital technologies. J. Adv. Prosthodont. 2022, 14, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Scherer, M.; Husain, N.A.; Barmak, A.B.; Kois, J.C.; Özcan, M.; Revilla-León, M. Influence of the layer thickness on the flexural strength of aged and nonaged additively manufactured interim dental material. J. Prosthodont. 2023, 32, 68–73. [Google Scholar] [CrossRef]
- Sadek, H.M.A.; El-Banna, A. Biaxial flexural strength of different provisional restorative materials under chemo-mechanical aging: An in vitro study. J. Prosthodont. 2024, 33, 149–156. [Google Scholar] [CrossRef]
- Kang, Y.-J.; Kim, H.; Lee, J.; Park, Y.; Kim, J.-H. Effect of airborne particle abrasion treatment of two types of 3D-printing resin materials for permanent restoration materials on flexural strength. Dent. Mater. 2023, 39, 648–658. [Google Scholar] [CrossRef]
- Punia, U.; Kaushik, A.; Garg, R.K.; Chhabra, D.; Sharma, A. 3D printable biomaterials for dental restoration: A systematic review. Mater. Today Proc. 2022, 63, 566–572. [Google Scholar] [CrossRef]
- Schweiger, J.; Edelhoff, D.; Güth, J.-F. 3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing. J. Clin. Med. 2021, 10, 2010. [Google Scholar] [CrossRef] [PubMed]
- Alexander, A.E.; Wake, N.; Chepelev, L.; Brantner, P.; Ryan, J.; Wang, K.C. A guideline for 3D printing terminology in biomedical research utilizing ISO/ASTM standards. 3D Print. Med. 2021, 7, 8. [Google Scholar] [CrossRef] [PubMed]
- Finnes, T. High Definition 3D Printing—Comparing SLA and FDM Printing Technologies. J. Undergrad. Res. 2015, 13, 10–26. [Google Scholar]
- Chung, P.; Heller, J.A.; Etemadi, M.; Ottoson, P.E.; Liu, J.A.; Rand, L.; Roy, S. Rapid and low-cost prototyping of medical devices using 3D printed molds for liquid injection molding. J. Vis. Exp. 2014, e51745. [Google Scholar] [CrossRef]
- Revilla-León, M.; Meyers, M.J.; Zandinejad, A.; Özcan, M. A review on chemical composition, mechanical properties, and manufacturing work flow of additively manufactured current polymers for interim dental restorations. J. Esthet. Restor. Dent. 2019, 31, 51–57. [Google Scholar] [CrossRef]
- Zhao, M.; Geng, Y.; Fan, S.; Yao, X.; Zhu, M.; Zhang, Y. 3D-printed strong hybrid materials with low shrinkage for dental restoration. Compos. Sci. Technol. 2021, 213, 108902. [Google Scholar] [CrossRef]
- Abad-Coronel, C.; Carrera, E.; Córdova, N.M.; Fajardo, J.I.; Aliaga, P. Comparative Analysis of Fracture Resistance between CAD/CAM Materials for Interim Fixed Prosthesis. Materials 2021, 14, 7791. [Google Scholar] [CrossRef]
- Abad-Coronel, C.; Córdova, J.; Merchán, A.; Larriva, J.; Bravo, A.; Bernal, B.; Paltán, C.A.; Fajardo, J.I. Comparative Analysis of the Fracture Resistance of a Polymeric Material for 3D Printing and a Milled Polymethylmethacrylate Material as Interim Material for Fixed Partial Dentures: New Material Updated. Designs 2023, 7, 118. [Google Scholar] [CrossRef]
- Barcena, A.J.R.; Ravi, P.; Kundu, S.; Tappa, K. Emerging Biomedical and Clinical Applications of 3D-Printed Poly(Lactic Acid)-Based Devices and Delivery Systems. Bioengineering 2024, 11, 705. [Google Scholar] [CrossRef] [PubMed]
| PUBMED | |
| P | (Crowns [MeSH Terms] OR Crowns [Title] OR Restorations [Title] OR Restorative [Title] OR Indirect Restorations [Title/Abstract] OR Fixed Dental Prostheses [Title/Abstract] OR Plural Fixed Prostheses [Title/Abstract] OR Single fixed prosthesis [Title/Abstract] OR Single Unit [Title/Abstract]) |
| I | (3D-Printed [Title/Abstract] OR Three Dimensional Printed [Title/Abstract] OR 3-D Printing [MeSH Terms] OR 3-D Printing [Title/Abstract] OR Additive [Title/Abstract]) AND (Polymeric Material [Title/Abstract] OR Resin [Title] OR Composite Resins [MeSH Terms] OR Composite Resins [Title/Abstract] OR Restoration Material [Title]) |
| C | 1 2 and 3 |
| O | (Flexural Strength [MeSH Terms] OR Flexural Strength [Title/Abstract] OR Fatigue Behavior [Title/Abstract] OR Microhardness [Title/Abstract] OR Fracture Strength [Title/Abstract] OR Fracture Resistance [Title/Abstract] OR Mechanical Properties [Title/Abstract] OR Flexure [Title]) |
| EBSCO | |
| P | (TI Crowns) OR (TI Indirect Restorations) OR (TI Fixed Dental Prostheses) OR (TI Plural Fixed Prostheses) OR (TI Restorations) OR (TI Restorative) |
| I | (TI 3D Printed) OR (TI Three Dimensional Printed) OR (TI 3D Printing) OR (TI Aditive) OR (TI Polymeric Material) OR (TI Resin) OR (TI Composite Resins) |
| C | 1 2 and 3 |
| O | (TI Flexural Strength) OR (TI Fatigue Behavior) OR (TI Microhardness) OR (TI Fracture Strength) OR (TI Fracture Resistance) OR (TI Mechanical Properties) |
| LILLACS | |
| P | (ti:(“Crowns”)) OR (ti:(“Plural Fixed Prostheses”)) OR (ti:(“Indirect Restorations”)) OR (ti:(“Fixed Dental Prostheses”)) AND (“Restorations”) |
| I | (TI “3D Printed”) OR (“TI Three Dimensional Printed”) OR (TI “3D Printing”) OR (TI “Aditive”) OR (TI “Polymeric Material”) OR (TI “Resin”) OR (TI “Composite Resins”) |
| C | 1 2 and 3 |
| O | (TI:(“Flexural Strength”)) OR (TI:(“Fatigue Behavior”)) OR (TI:(“Microhardness”)) OR (TI:(“Fracture Strength”)) OR (TI:(“Fracture Resistance”)) AND (TI:(“Mechanical Properties”)) |
| SCIENCE DIRECT | |
| P | Title, abstract, keywords: “Crowns” OR “Indirect Restorations” |
| I | Title, abstract, keywords: “3D Printed” OR “Three Dimensional Printed” OR “Resin” OR “Composite Resins” |
| C | 1 2 and 3 |
| O | Title, abstract, keywords: “Flexural Strength” OR “ Microhardness” OR “Fatigue Behavior” |
| Demographics Characteristics | Printer Parameters | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ID Study | Year | SS | ST&ISO | Property | PT&M | RT&B | LT (μm) | CG (°) | PCT | Control |
| [16] | 2022 | 30 | 1.2 mm thick and 14 mm diameter disc ISO 6872:2024 [17] | Biaxial FS | SLA Formlabs, Somerville, MA, USA DLP NextDent 5100; 3D Systems, Soesterberg, NL | 1. Crowntec (CT) 2. Permanent bridge resin (PB) 3. Formlabs (FL) 4. NextDent (ND) | 50 | NA | FL: 20 min CT: 6 min PB: 6 min ND: 30 min | NA |
| [18] | 2020 | 15 | Three-unit plural fixed prosthesis | FS | DLP NextDent 5100; Soesterberg, NL SLA Formlabs, Somerville, MA, USA, FDM FlashForge | 1. DLP: PMMA (D-150 NextDent) 2. SLA: Form2 Formlabs 3. FDM: Polylactic acid (Creator pro, FlashForte) | SLA and DLP: 100 FDM: 200 | 30° | DLP: 120 min SLA: 60 min, FDM did not undergo post-curing | Self-curing (CV) as negative control: PMMA Jet Tooth (ShadeTM Powder, Lang Dental Co., Wheeling, IL, USA). Subtractive method (SM) as positive control: PMMA (ViPi, VIPI Co., Sao Paulo, Brazil) |
| [19] | 2021 | 15 | Discs of 15 mm diameter and 1 mm thickness | FS and MH | DLP Kulzer, Australia | C&B NextDent 3D resin reinforced with ZrO2 nanoparticles at 1, 2, 3, 4 and 5% | 50 | NA | 20 min | C&B NextDent 3D resin without reinforcement |
| [20] | 2022 | FS: 25 MH: 5 | FS: Bar with dimensions of 2 mm × 2 mm × 25 mm ISO: 10477 [21] MH: Discs with a diameter of 10 mm and a thickness of 3 mm | FS and MH | DLP NextDent 5100; Soesterberg, NL | C&B NextDent 3D resin. | 50 | NA | 5, 15, and 30 min with LC 3D Print Box (LC), Form Cure (FC), Cure M (CM) and Veltz 3D (VE) 20 s, 40 s, and 60 s with Valo (VA) | Specimens of the group that were not subjected to post-curing |
| [22] | 2023 | 96 | 12 × 8 × 2 mm blocks | MH | SLA Asiga MAX UV, Australia | Permanent 3D resins: Crowntec (Saremco Dental AG) (CT) Permanent Crown (Formlabs) (CP) | 50 | NA | 6 and 20 min | CAD/CAM blocks based on Cerasmart (CS) resin and Grandio Blocs (GB) |
| [23] | 2022 | MH: 5 FS: 10 | FS: 4 × 2 × 10 mm bars MH: 10 × 2 mm diameter discs CF: individual crowns | FS, MH and CF | SLA and SLS | SLA 3D-printed resin SLS 3D-printed resin | NA | NA | SLA: 30 min SLS: 0 min | Acrylic resin (RA) and bisacrylic resin (BIS) |
| [24] | 2024 | 14 | FS: 2 mm × 2 mm × 25 mm bars MH: 4 × 4 × 6 mm blocks ISO: 4049 [25] | FS and MH | DLP Pro 55, SprintRay, LA, CA | C&B 3D-printed resin MFH (C&B) Ceramic Crown (CC) SprintRay OnX (OnX) SprintRay OnX Tough (OnXT) | 100 | NA | NA | Light-curing composite resin Filtek Supreme Ultra (FS), Lava Ultimate milled composite resin (LU) and IPS e.max CAD milled ceramic (e.max) |
| [26] | 2023 | 8 | 4-unit plural fixed prosthesis | FS | DLP Pro 95, SprintRay, Los Angeles, CA, USA | 3DPP (Sprintray) | NA | NA | NA | Zirconium dioxide (ZR O2) (KATANA, Zirconia STML), Porcelain fused to metal (PFM) and PMMA (Telio CAD, Ivoclar Vivadent) |
| [1] | 2024 | FS: 30 CF: 20 | 14 mm Disc with a diameter of 15 mm and a height of 1.5 mm ISO: 6872 | Biaxial FS and CF | DLP Varseo XS, Bego | VarseoSmile Crown Plus (3D) | 50 | NA | NA | Nanohybrid composite resin (NHC group) (Grandio, VOCO) and polymer-infiltrated ceramic (PICN group) (Enamic, Vita Zahnfabrik) |
| [27] | 2023 | 20 | Unitary fixed prothesis | FS | DLP Pro 95, SprintRay, Los Angeles, CA, USA | 3DPPa (SprintRay) 3DPPb (SprintRay) | 50 | NA | 9 min | Milled PMMA (Ivoclar Vivadent) |
| [28] | 2024 | MH: 792 FS: 180 | MH: Discs FS: Bar-shaped specimens | FS and MH | NA | NextDent C&B MFH | NA | NA | Fast and Standard modes with VALO (V1 and V2) and BluePhase (B1 and B2) cured units and Conventional post curing (PC group) | NA |
| [29] | 2023 | 6 | NA | FS MH | NA | Varseo Smile Crown plus-(VSC) Saremco Print Crowntec (SPC) Formlabs 3B Permanent crown (FLP) | NA | NA | NA | Vita Enamic -VE, Cerasmart -CE, Lava Ultimate-LU |
| [30] | 2023 | 10 | NA | FS | NA | 3D-printed VarseoSmile Crown Plus (VSC) | NA | NA | NA | Milled Vita Enamic (VE), milled Cerasmart 270 (CS) |
| [31] | 2021 | Total: 368 | MD: 10 × 10 × 4 mm bars RF: 2 × 3 × 15 mm bars | FS and MH | fused filament fabrication (FFF) | Polyphenylenesulfone (PPSU): PPSU1-3D = PPSU Radel PPSU2-3D = Ultrason P 3010 NAT | NA | NA | NA | Polyetheretherketone semi-crystalline (PEEK- CG) milled and PPSU obtained by extrusion (PPSU1- EX) |
| [32] | 2022 | RF: 12 MD: 10 | RF: 2 × 2 × 2 mm bars ISO: 4049 MD: 5 × 5 × 5 mm blocks | FS and MH | DLP Photon, Anycubic Technology Co., Shenzhen, China | Cosmos Temp3D (COS), SmartPrint BioTemp (SM) Resilab3D Temp (RES) and Prizma3D BioProv (PRI) | 50 | 0° | 5 min 10 min 15 min 20 min | NA |
| [33] | 2023 | 30 | 8 × 2 × 2 mm bars ISO: 6872:2024 | FS | DLP Miicraft Ultra 125 | Temp 3D-printed resin (PRINT) | 65 | 90° | 7 min | Acrylic resin Dencor (AR), Filtek Z350XT Composite Resin (CR), VIPI Milled PMMA Resin (CAD) and Bisacril Protemp 4 (BIS) |
| [34] | 2023 | 16 | 2 × 2 × 25 mm bars ISO: 10477 | MH | DLP NextDent 5100; Soesterberg, NL Asiga MAX Nova 3D Master, Australia | 1. NextDent 3D-printed resin 2. Asiga DentaTooth 3. JamgHe | 50 | 1. 0° 2. 90° | NA | NA |
| [35] | 2020 | MD: 8 RF: 10 | diameter and 2 mm height discs | FS and MH | SLA NextDent 5100; Soesterberg, NL | Crown & Bridge 3D-printed resin, MFH (Next Dent) (PR) | NA | NA | NA | Bisaccharide resin ProTemp Plus (3M ESPE) (BA) and Filtek Z350XT Conventional Composite Resin (3M ESPE) (Z350) |
| [36] | 2021 | 10 | 15 × 4 × 1.5 mm bars | FS and MH | Sonic Mini 4K Phrozen, Hsinchu City, Taiwan | VarseoSmile Crown plus ® 3D-printed resin (Bego)(VSC) | 50 | 1. 90° 2. 45° | 2 times of 45 min | Grandio pads (VOCO) (GR), Brilliant Crios® (Coltene/Whaledent AG Altstatten)—(CR), Enamic® (Vita Zahnfabrik)—(EN) |
| [37] | 2022 | 210 | 25 × 2 × 2 mm bars | FS and MH | DLP Everes zero, SISMA, Italy | A2 EVERES TEMPORARY printed resin, SISMA, Italy | 25, 50, 100 | 90° | LC: 5 and 15 min HC: 5 and 15 min | NA |
| [38] | 2021 | 20 | Discs of 10 mm diameter and 2 mm thickness | MH | 1. Vat-polymerization 3D printer Rapidshape D30; Rapidshape, Heimsheim, Germany. 2. Vat-polymerization printer Envisiontec VIDA; Dearborn, MI, USA | Printed Resin: 1. AM-1 (FreePrint temp; Detax) 2. AM-2 (E-Dent 400 C&B MFH; Envisiontec) 3. AM-3 (NextDent C&B MFH; 3D Systems), 4. AM-4 (Med620 VEROGlaze; Stratasys). | 50 | 90° | 1: 6 min 2: 15 min 3: 30 min 4: NA | Conventional Materials: CNV-1 (Protemp 4; 3M ESPE) CNV-2 (Anaxdent new outline dentin; Anaxdent), |
| [39] | 2022 | 20 | Rectangular samples (2 × 2 × 25 mm). ISO: 10477 | FS and MH | DLP NextDent 5100; Soesterberg, NL | Photopolymer (Crown & Bridge NextDent®; 3D Systems, Soesterberg, Countries Low) | 50 | 0° | 30 min | Self-healing provisional material (Bosworth Trim Plus; Bosworth, Skokie, IL, USA) and prefabricated resin blocks (Ceramill temp; Amann Girrbach AG, Koblach, Austria) |
| [40] | 2023 | 20 | 25 × 2 × 2 mm bars | FS | Asiga MAX UV, Australia | Temporary resin (Nexdent C&B MFH) | 10, 25, 75, 100, 125 and 150 | NA | 30 min | Control group 50 um |
| [41] | 2023 | 15 | Discs 10 × 2 mm | FS | 3D Printer EPAX, Morrisville, NC, USA | MFH (NextDent C&B) | NA | NA | 30 min | conventional (Protemp 4, Tuff-Temp, Tempron), CAD-CAM milling (VITA CAD-Temp, breCAM.multiCOM) |
| [42] | 2023 | 196 samples | 25 × 2 × 2 mm ISO: 10477 | FS | 1. DLP Pro 95, SprintRay, Los Angeles, CA, USA 2. SLA Form 3, Formlabs, Somerville, MA, USA | 3D printing resins 1. UDMAC 2. BEMAC | NA | NA | UDMA: 20 min BEMA: 30 min | NA |
| Conventional Method | |||||
| Material | Brand | FS (MPa) | DS | FS (N) | DS |
| Bisacryl resin | Protemp [35] | 27.9 | ±6.10 | ||
| UDM resin | Tuff Temp [41] | 48.95 | ±87.64 | ||
| PMMA | Tempron [41] | 61.43 | ±7.29 | ||
| Acrylic resin | Dencor, Brazil [23] | 69.2 | ±8.8 | ||
| Bisacryl resin | Yprov Bisacryl [23] | 75.0 | ±8.2 | ||
| PMMA | Bosworth [39] | 76.0 | ±12 | ||
| Composite | Z350 Filtek (3M) [33] | 84.0 | ±18.54 | ||
| Acrylic resin | Dencor, Brazil [33] | 89.6 | ±9.38 | ||
| Composite | Z350 Filtek (3M) [35] | 105.1 | ±9.80 | ||
| Bisacryl resin | Protemp 4 [41] | 113.06 | ±14.45 | ||
| Bisacryl resin | Protemp [33] | 118.23 | ±16.26 | ||
| Composite | Z350 Filtek 3M [24] | 156.9 | ±14.8 | ||
| PMMA | Lang dental [18] | 543 N | |||
| Polylactic acid | Pla ColorFabb [18] | 1323 N | |||
| Milled Method | |||||
| Material | Brand | FS (MPa) | DS | FS (N) | DS |
| PMMA | VITA CAD-Temp [41] | 62.48 | ±5.90 | ||
| PMMA | breCAM.multiCOM [41] | 77.88 | ±10.25 | ||
| PMMA | Amann [39] | 94 | ±19 | ||
| PMMA | VIPI [33] | 94.63 | ±9.89 | ||
| Resin | Cerasmart 270 [22] | 109.5 | ±1.9 | ||
| Resin | Enamic VITA [36] | 118.96 | |||
| Resin | Enamic VITA [1] | 140.3 | ±12.9 | ||
| Resin | Brilliant blocs [36] | 170.29 | |||
| Resin | Lava ultimate (3M) [24] | 183.6 | ±17.5 | ||
| Resin | Grandio blocs [36] | 186.02 | |||
| Resin | Grandio blocs [22] | 203.9 | ±3.6 | ||
| Resin | Grandio blocs [1] | 237.3 | ±31.6 | ||
| Ceramic | E.max Ips [24] | 299.3 | ±26.0 | ||
| Resin | Vita Enamic [30] | 727.8 N | |||
| Resin | Cerasmart 270 [30] | 1213.8 N | |||
| PMMA | Telio CAD [26] | 2104.73 N | |||
| 3D-Printed Method | |||||
| Material | Brand | FS (MPa) | DS | FS (N) | DS |
| Resin | Cosmos Temp 3D [32] | 19.5 | ±2.7 | ||
| Resin | Smart Print Bio Temp [32] | 21.9 | ±2.1 | ||
| Resin | Prizma 3D [32] | 33.7 | ±4.3 | ||
| Resin | Resilab 3D Temp [32] | 34.2 | ±3.7 | ||
| Resin | Cosmos Temp 3D [33] | 49.7 | ±7.55 | ||
| PMMA | C&B NextDent [35] | 67.15 | ±11.70 | ||
| Resin | OnXT (SprintRay) [24] | 78 | ±8.6 | ||
| Resin | Eves temporary [37] | 80.8 | |||
| Resin | Varseo Smile Crown Plus [1] | 83.5 | ±18.5 | ||
| PMMA | C&B NextDent [19] | 94.14 | |||
| PMMA | C&B NextDent [24] | 97.1 | ±4.6 | ||
| PMMA | C&B NextDent [41] | 100.87 | ±11.14 | ||
| Resin | Veltz 3D [20] | 110 | |||
| PMMA | C&B NextDent [39] | 114 | ±8 | ||
| Resin | Ceramic Crown (Sprint Ray) [24] | 117.4 | ±11.6 | ||
| Resin | Varseo Smile Crown Plus [36] | 119.85 | |||
| Resin | PrintBox [20] | 120 | |||
| Resin | Permanent Crown, Formlabs [42] | 128 | ±22.4 | ||
| Resin | Form Cure [20] | 130 | |||
| Resin | OnX (Sprint Ray) [24] | 131 | ±11.6 | ||
| Resin | Cure M [20] | 139 | |||
| Resin | Tera Harz TC-80DP, Graphy [42] | 143.6 | ±13.1 | ||
| PMMA | C&B NextDent [16] | 153.51 | |||
| Resin | Crowntec [16] | 187.73 | |||
| Resin | Permanent bridge [16] | 208.03 | |||
| Resin | Formlabs [16] | 249.09 | |||
| PMMA | C&B NextDent [40] | 296.6 | ±11.97 | ||
| Resin | PA2201; Stratasys Direct Manufacturing | 452.4 | ±35.8 | ||
| Resin | Formlabs [23] | 513.3 | ±29.7 | ||
| Resin | Sprint Ray [26] | 1000.88 | |||
| Resin | Nano ceramic hybrid (Sprint Ray) [27] | 1029.92 | ±166.4 | ||
| Resin | Varseo Smile Crown Plus [30] | 1181.5 | |||
| PMMA | C&B NextDent [18] | 1189 | |||
| Resin | Hybrid material (SprintRay) [27] | 1231 | ±380.1 | ||
| PMMA | Formlabs [18] | 1323 | |||
| PMMA | Ivoclar [27] | 1427 | ±36.9 | ||
| PSSU | Radel R-5000 NT | 83 * | |||
| PSSU | PPSU Radel | 78.8 * | |||
| PSSU | Ultrason P 3010 NAT | 158.1 * | |||
| PEEK | PEEK Juvora | 139.1 * | |||
| Conventional Method | |||
| Material | Brand | MH (Kgf/mm2) | DS |
| Acrylic resin | Dencor [23] | 14.2 | ±2.6 |
| PMMA | Bosworth [39] | 19.1 | |
| Bisacryl | Protemp [35] | 22.1 | ±3.10 |
| Composite | Z350 Filtek 3M [35] | 61.7 | ±5.70 |
| Composite | Z350 Filtek 3M [24] | 91.5 | ±10.4 |
| Bisacryl | Protemp [38] | 4.92 * | ±0.36 |
| Acrylic resin | Next outline Anaxdent | 13.35 * | ±5.84 |
| Milled Method | |||
| Material | Brand | MH (Kgf/mm2) | DS |
| PMMA | Amann [39] | 24.3 | |
| Resin | Brilliant crios [36] | 75.4 | |
| Resin | Lava ultimate 3M [24] | 114.8 | ±28.1 |
| Resin | Grandio blocs [36] | 140.43 | |
| Resin | Enamic [36] | 273.42 | |
| Ceramic | E.max IPS [24] | 574 | ±29.0 |
| 3D-Printed Method | |||
| Material | Brand | MH (Kgf/mm2) | DS |
| Resin | Cosmos Temp 3D [32] | 4.58 | ±0.59 |
| Resin | Resilab 3D TEMP [32] | 7.46 | ±0.60 |
| Resin | Smart Print Bio [32] | 8.37 | ±0.93 |
| Resin | Formlabs [23] | 8.4 | ±0.2 |
| Resin | JamgHe temporary resin, Nova 3D Master [34] | 10 | |
| Resin | Prizma 3D [32] | 10.22 | ±0.68 |
| Resin | PA2201; Stratasys Direct Manufacturing [23] | 10.3 | ±1.0 |
| PMMA | C&B Next Dent [24] | 14.1 | ±0.6 |
| Resin | Everes temporary [37] | 14.33 | |
| PMMA | C&B Next Dent [20] | 16 | |
| PMMA | C&B Next Dent [19] | 17.39 | |
| Resin | OnXT [24] | 17.6 | ±0.8 |
| Resin | DentaTooth, Asiga [34] | 23.4 | |
| PMMA | C&B Next Dent [34] | 24.5 | |
| PMMA | C&B Next Dent [39] | 25.2 | |
| Resin | Varseo smile crown [36] | 25.8 | |
| Resin | OnX [24] | 29.3 | ±2.1 |
| Resin | Crowntec [22] | 30 | ±1.3 |
| PMMA | C&B Next Dent [35] | 35 | ±2.50 |
| Resin | Varseo smile crown, Saremco Print Crowntec, Formalbs Permanent Crown [29] | 35.11 | ±4.46 |
| Resin | Permanent crown [22] | 37.4 | ±1.3 |
| Resin | Ceramic Crown [24] | 42.5 | ±5.6 |
| Resin | Vita Enamic, Cerasmart, Lava Ultimate [29] | 253.5 | ±21.5 |
| PMMA | C&B Next Dent [38] | 9.91 * | ±3.71 |
| Resin | Free Print Temp [38] | 12.55 * | ±2.93 |
| Resin | E Dent 400 C&B MFH [38] | 13.03 * | ±3.29 |
| Resin | VeroGlaze MED620 [38] | 13.45 * | ±2.93 |
| PSSU | Radel R-5000 NT | 111 ** | |
| PSSU | PPSU Radel | 113 ** | |
| PSSU | Ultrason P 3010 NAT | 121 ** | |
| PEEK | PEEK Juvora | 207 ** | |
| Milled Method | |||
| Material | Brand | CF (MPa) | DS |
| Resin | Enamic [1] | 73.5 | ±9.9 |
| Resin | Grandio blocs [1] | 141.3 | ±3.8 |
| 3D-Printed Method | |||
| Material | Brand | CF (MPa) | DS |
| Resin | Varseo smile crown [1] | 37.4 | ±23.8 |
| Number | Author | Year | Study | Criteria QUINN and Points | Total (%) | Bias Risk | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | ||||||
| 1 | Atria PJ, et al. [16] | 2021 | 2 | 0 | NA | 1 | 2 | NA | NA | 2 | NA | 0 | 2 | 2 | 11 (68.75%) | Medium | |
| 2 | Park SM. et al. [18] | 2020 | in vitro | 2 | 0 | NA | 2 | 2 | NA | NA | 1 | NA | 0 | 2 | 2 | 11 (68.75%) | Medium |
| 3 | Aati S, et al. [19] | 2021 | in vitro | 2 | 0 | NA | 2 | 2 | NA | NA | 1 | NA | 0 | 1 | 2 | 10 (62.5%) | Medium |
| 4 | Bayarsaikhan E. et al. [20] | 2022 | in vitro | 2 | 0 | NA | 2 | 2 | NA | NA | 2 | NA | 0 | 2 | 2 | 12 (75%) | Low |
| 5 | Karaoglandoglu S, et al. [22] | 2023 | in vitro | 2 | 2 | NA | 0 | 2 | NA | NA | 0 | NA | 0 | 1 | 2 | 9 (56.25%) | Medium |
| 6 | Simoneti DM. et al. [23] | 2022 | in vitro | 2 | 0 | NA | 1 | 1 | NA | NA | 0 | NA | 0 | 1 | 2 | 7 (43.75%) | High |
| 7 | Bora PV. et al. [24] | 2024 | in vitro | 2 | 2 | NA | 2 | 2 | NA | NA | 2 | NA | 0 | 2 | 2 | 14 (87.5%) | Low |
| 8 | Abad Coronel C, et al. [26] | 2023 | in vitro | 2 | 0 | NA | 0 | 2 | NA | NA | 2 | NA | 0 | 2 | 2 | 10 (62.5%) | Medium |
| 9 | Prause E. et al. [1] | 2024 | in vitro | 2 | 0 | NA | 2 | 2 | NA | NA | 1 | NA | 0 | 2 | 2 | 11 (68.75%) | Medium |
| 10 | Abad Coronel C, et al. [27] | 2023 | in vitro | 2 | 0 | NA | 1 | 2 | NA | NA | 2 | NA | 0 | 2 | 2 | 11 (68.75%) | Medium |
| 11 | Chung SH, et al. [28] | 2024 | in vitro | 2 | 0 | NA | 2 | 2 | NA | NA | 2 | NA | 0 | 1 | 2 | 11 (68.75%) | Medium |
| 12 | Sahin Z, et al. [29] | 2023 | in vitro | 2 | 0 | NA | 2 | 2 | NA | NA | 2 | NA | 0 | 1 | 2 | 11 (68.75%) | Medium |
| 13 | Abdulkareem MA, et al. [30] | 2023 | in vitro | 2 | 0 | NA | 2 | 2 | NA | NA | 2 | NA | 0 | 1 | 2 | 11 (68.75%) | Medium |
| 14 | Schönhoff LM, et al. [31] | 2021 | in vitro | 2 | 0 | NA | 1 | 1 | NA | NA | 1 | NA | 0 | 2 | 2 | 9 (56.25%) | Medium |
| 15 | Soto-Montero J, et al. [32] | 2022 | in vitro | 2 | 0 | NA | 0 | 2 | NA | NA | 1 | NA | 0 | 2 | 2 | 9 (56.25%) | Medium |
| 16 | Ribeiro AKC, et al. [33] | 2022 | in vitro | 2 | 0 | NA | 1 | 2 | NA | NA | 1 | NA | 0 | 2 | 2 | 10 (62.5%) | Medium |
| 17 | Alageel O, et al. [34] | 2023 | in vitro | 2 | 2 | NA | 1 | 2 | NA | NA | 1 | NA | 0 | 2 | 2 | 12 (75%) | Low |
| 18 | Scotti CK, et al. [35] | 2020 | in vitro | 2 | 0 | NA | 2 | 2 | NA | NA | 2 | NA | 0 | 2 | 2 | 12 (75%) | Low |
| 19 | Grzebieluch W, et al. [36] | 2021 | in vitro | 2 | 0 | NA | 1 | 2 | NA | NA | 2 | NA | 0 | 2 | 2 | 11 (68.75%) | Medium |
| 20 | Alshamrani AA, et al. [37] | 2022 | in vitro | 2 | 0 | NA | 2 | 2 | NA | NA | 2 | NA | 0 | 1 | 2 | 11 (68.75%) | Medium |
| 21 | Revilla-León M, et al. [38] | 2021 | in vitro | 2 | 1 | NA | 1 | 1 | NA | NA | 2 | NA | 0 | 1 | 2 | 10 (62.5%) | Medium |
| 22 | Alageel O, et al. [39] | 2022 | in vitro | 2 | 1 | NA | 1 | 2 | NA | NA | 2 | NA | 0 | 2 | 2 | 12 (75%) | Low |
| 23 | Scherer M, et al. [40] | 2023 | in vitro | 2 | 1 | NA | 1 | 2 | NA | NA | 2 | NA | 0 | 1 | 1 | 10 (62.5%) | Medium |
| 24 | Sadek HMA, et al. [41] | 2023 | in vitro | 2 | 1 | NA | 1 | 2 | NA | NA | 2 | NA | 0 | 2 | 2 | 12 (75%) | Low |
| 25 | Kang YJ, et al. [42] | 2023 | in vitro | 2 | 0 | NA | 1 | 2 | NA | NA | 2 | NA | 0 | 2 | 2 | 11 (68.75%) | Medium |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abad-Coronel, C.; Durán Urdiales, D.; Benalcázar Arias, M.V.; Córdova, A.K.; Medina, M.S.; Bravo Torres, W. Flexural Strength, Fatigue Behavior, and Microhardness of Three-Dimensional (3D)-Printed Resin Material for Indirect Restorations: A Systematic Review. Materials 2025, 18, 556. https://doi.org/10.3390/ma18030556
Abad-Coronel C, Durán Urdiales D, Benalcázar Arias MV, Córdova AK, Medina MS, Bravo Torres W. Flexural Strength, Fatigue Behavior, and Microhardness of Three-Dimensional (3D)-Printed Resin Material for Indirect Restorations: A Systematic Review. Materials. 2025; 18(3):556. https://doi.org/10.3390/ma18030556
Chicago/Turabian StyleAbad-Coronel, Cristian, Daniela Durán Urdiales, María Verónica Benalcázar Arias, Andrea Karina Córdova, María Sol Medina, and Wilson Bravo Torres. 2025. "Flexural Strength, Fatigue Behavior, and Microhardness of Three-Dimensional (3D)-Printed Resin Material for Indirect Restorations: A Systematic Review" Materials 18, no. 3: 556. https://doi.org/10.3390/ma18030556
APA StyleAbad-Coronel, C., Durán Urdiales, D., Benalcázar Arias, M. V., Córdova, A. K., Medina, M. S., & Bravo Torres, W. (2025). Flexural Strength, Fatigue Behavior, and Microhardness of Three-Dimensional (3D)-Printed Resin Material for Indirect Restorations: A Systematic Review. Materials, 18(3), 556. https://doi.org/10.3390/ma18030556







