Antibacterial Properties of PMMA/ZnO(NanoAg) Coatings for Dental Implant Abutments
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.1.1. Synthesis of Zinc Oxide Nanoparticles
2.1.2. Synthesis of Zinc Oxide-Silver Nanoparticles
2.1.3. Preparation of Antimicrobial PMMA Films on Titanium Alloy Substrates
2.2. Methods
2.2.1. Synthesis Methods for Nanoparticles
Synthesis of Zinc Oxide (ZnO) Nanoparticles
Synthesis of Zinc Oxide-Silver (ZnO-Ag) Nanoparticles
2.2.2. Synthesis Methods for Film Preparation
Preparation of Polymethyl Methacrylate (PMMA) Films on Ti6Al4V Substrate
Preparation of PMMA Films Containing ZnO and ZnO-Ag Nanoparticles on Ti6Al4V Substrate
2.3. Characterization Techniques
2.3.1. X-Ray Diffraction
2.3.2. Fourier Transform Infrared Spectroscopy
2.3.3. Scanning Electron Microscopy
2.3.4. Infrared Microscopy
2.3.5. Antimicrobial Assay—Biofilm Development
2.3.6. In Vitro Cell-Based Assays—Biocompatibility and Oxidative Stress Production Assessment
3. Results
3.1. Powder-Type Samples Results—ZnO and ZnO-Ag
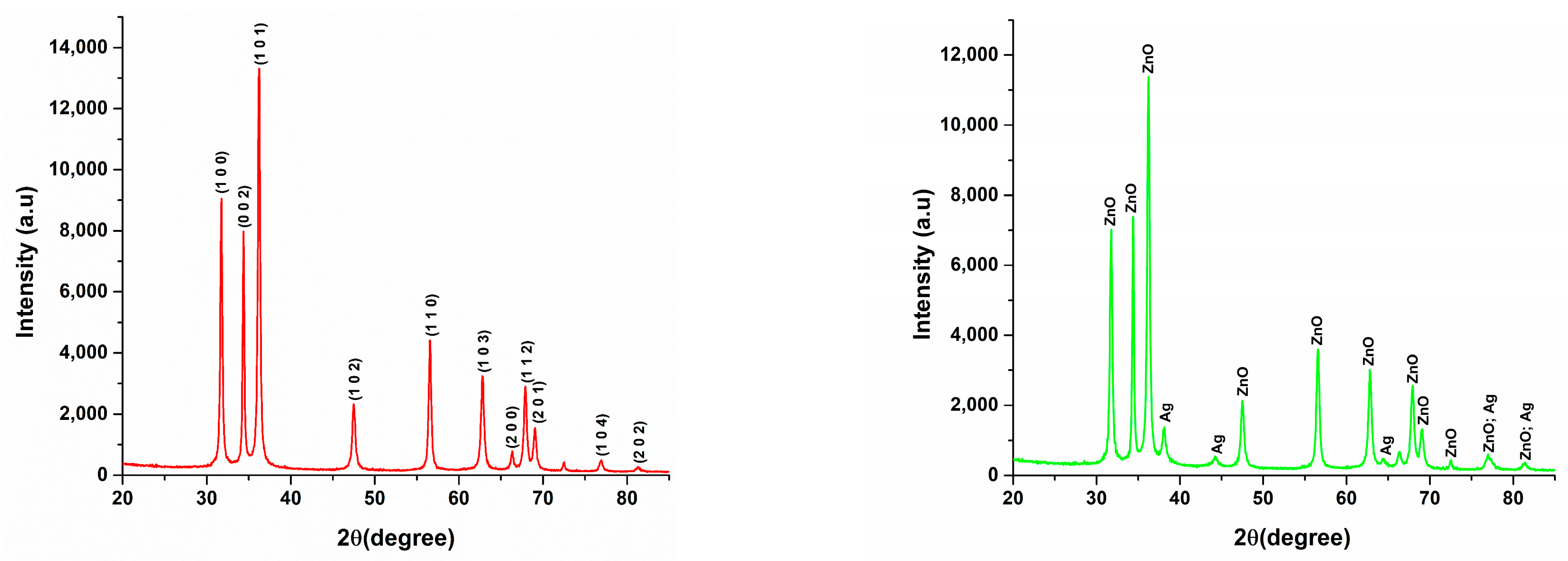
3.1.1. X-Ray Diffraction (XRD)
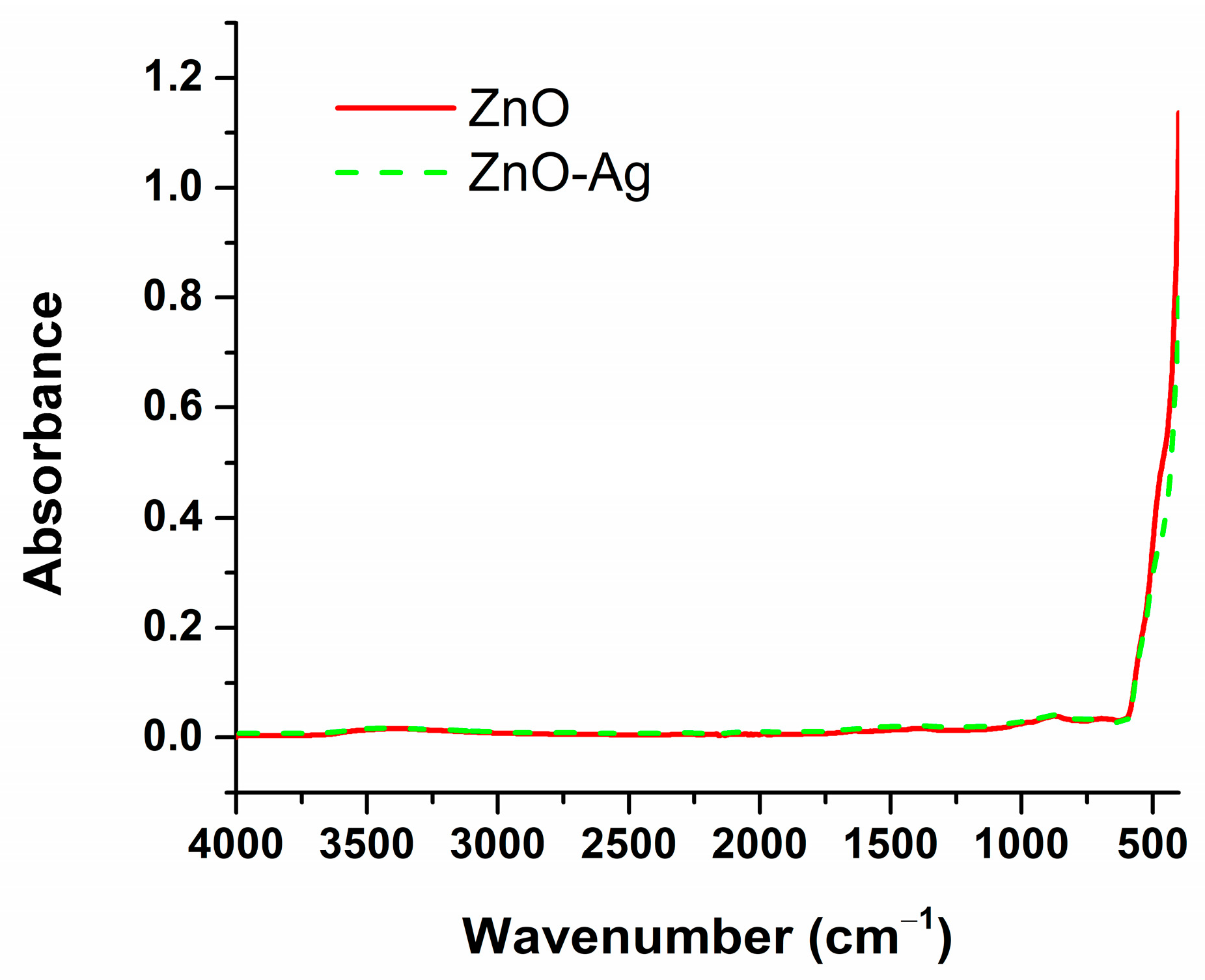
3.1.2. Fourier Transform Infrared Spectroscopy (FT-IR)
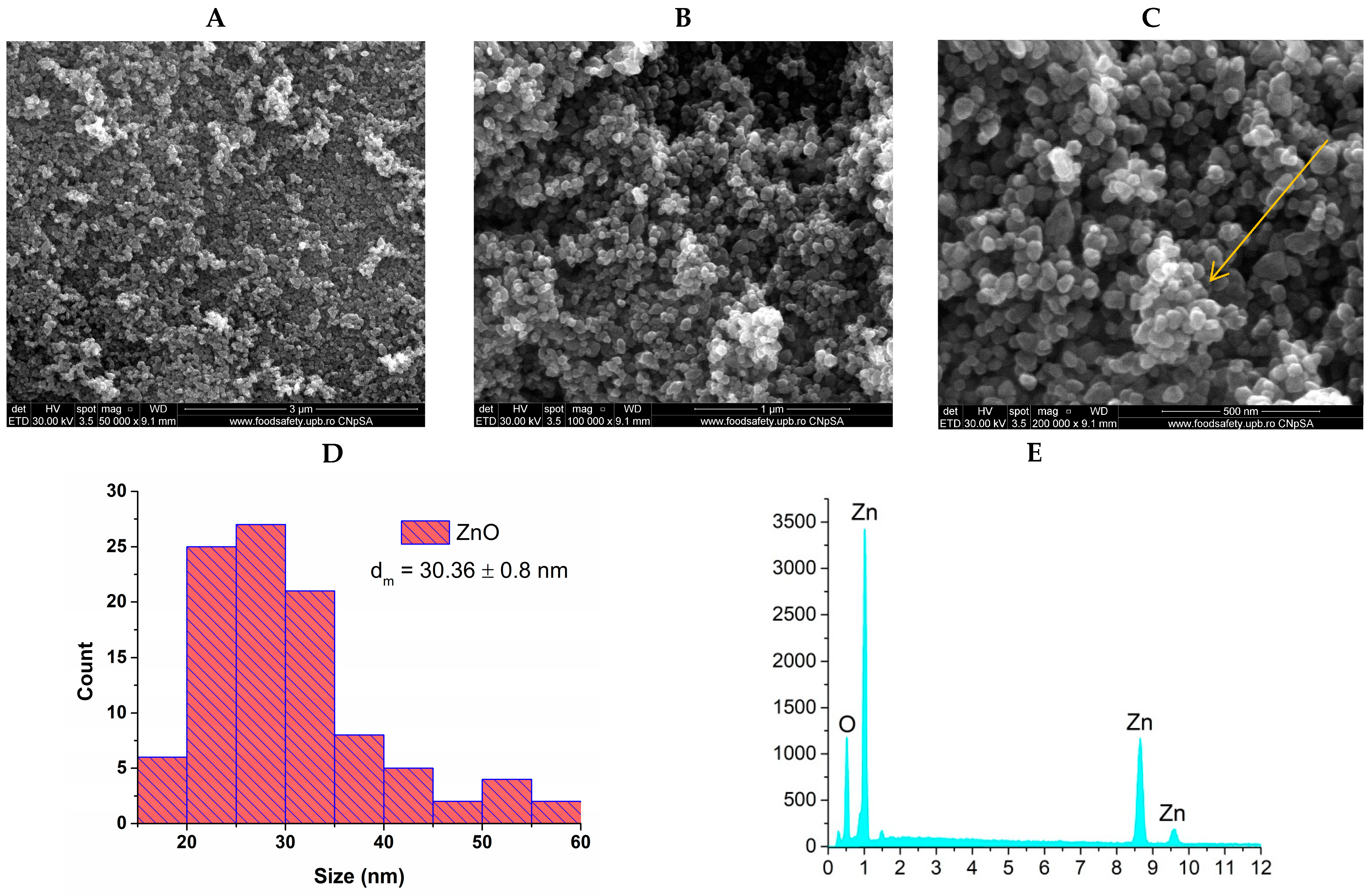
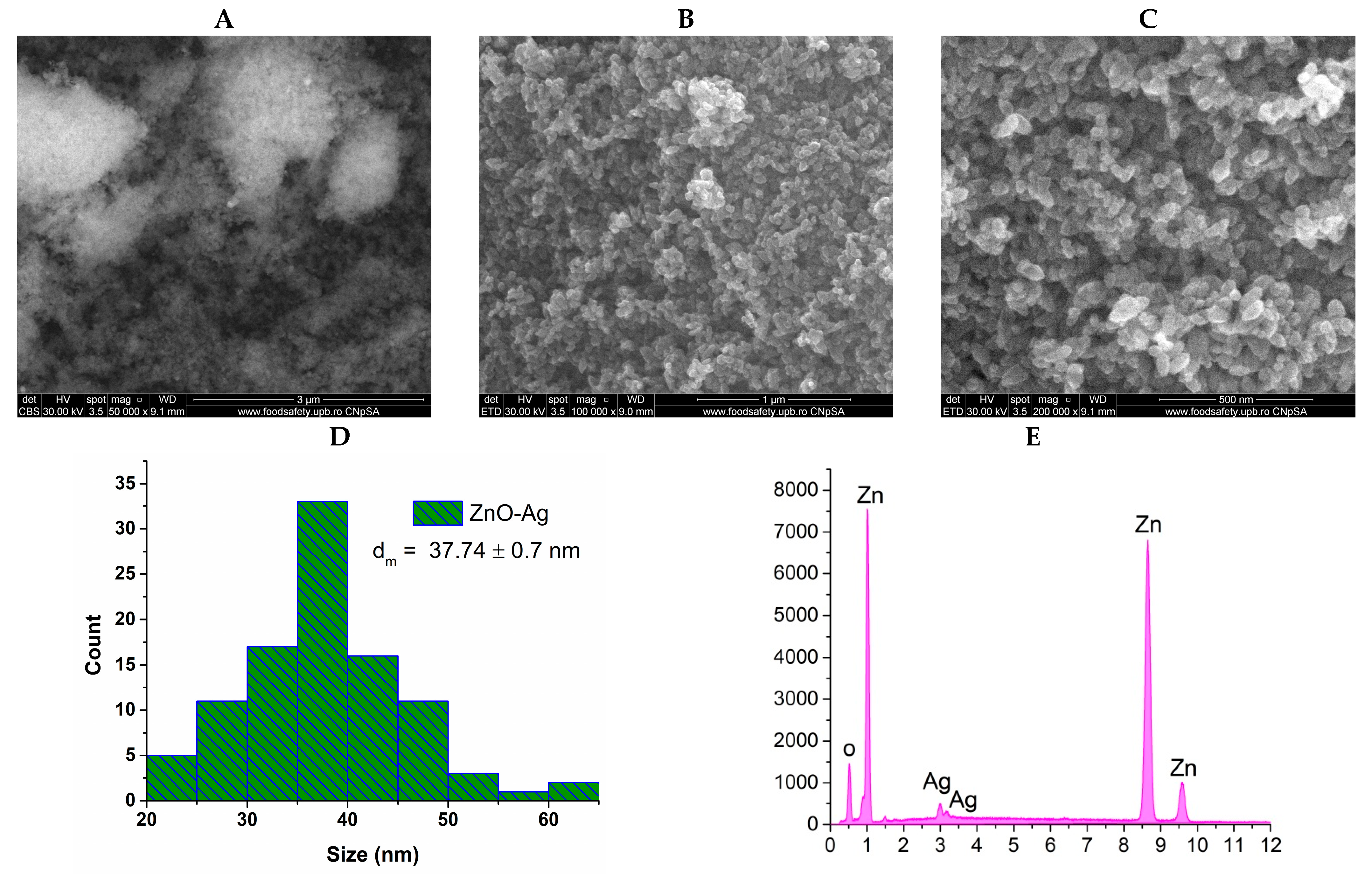
3.1.3. Scanning Electron Microscopy (SEM)
3.2. Coating-Type Samples Results—PMMA, PMMA ZnO, PMMA ZnO-Ag
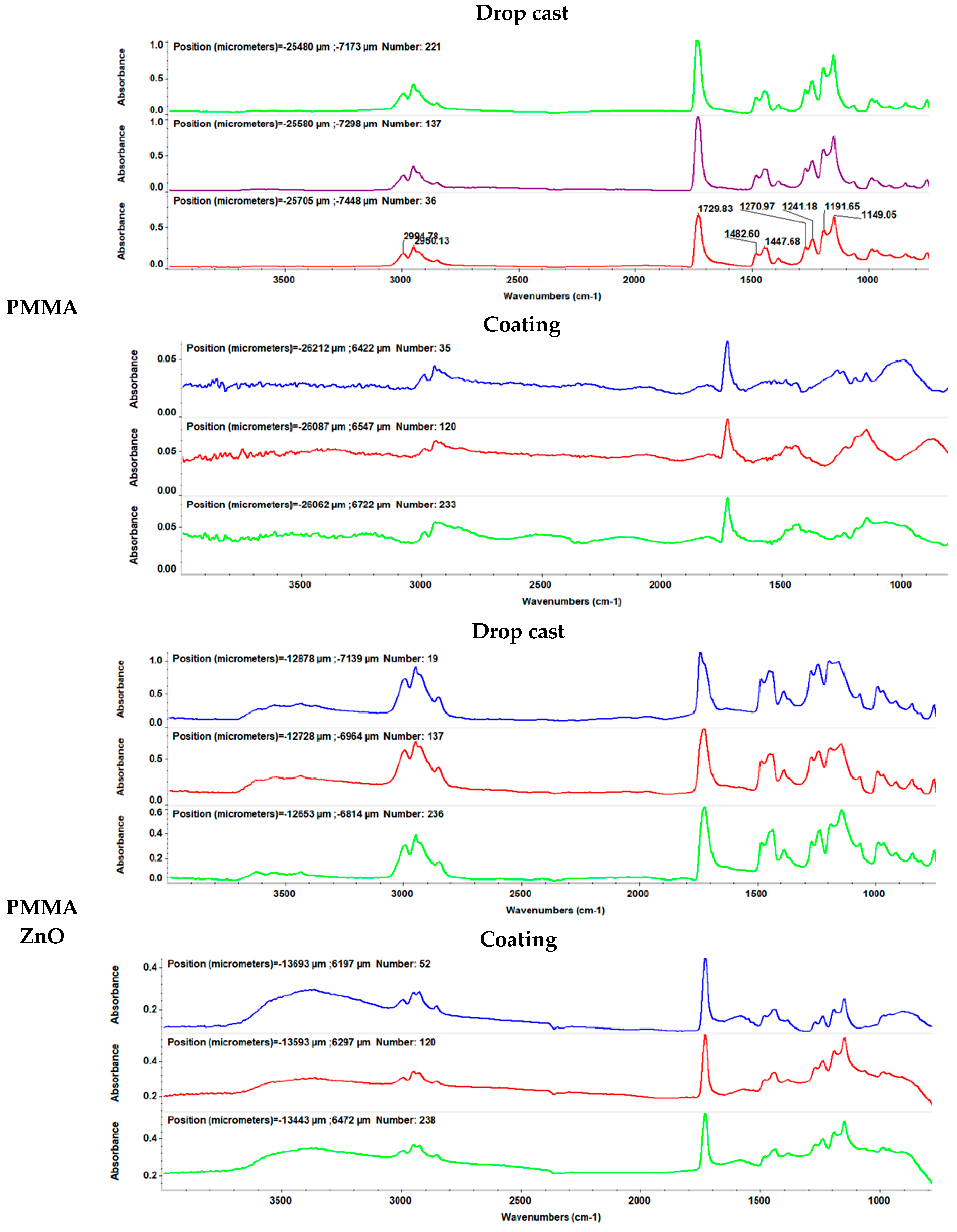
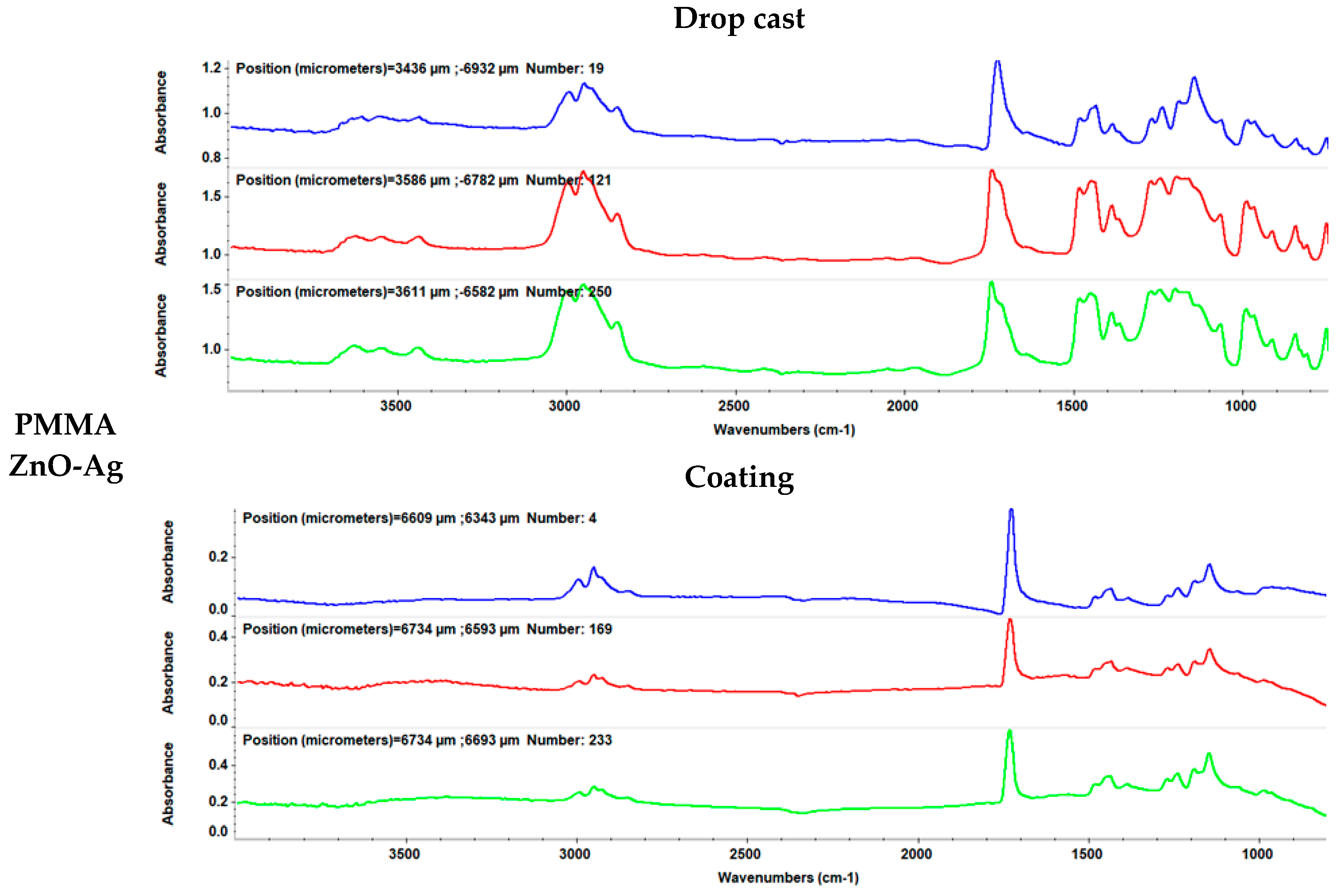
3.2.1. Infrared Microscopy (IRM)
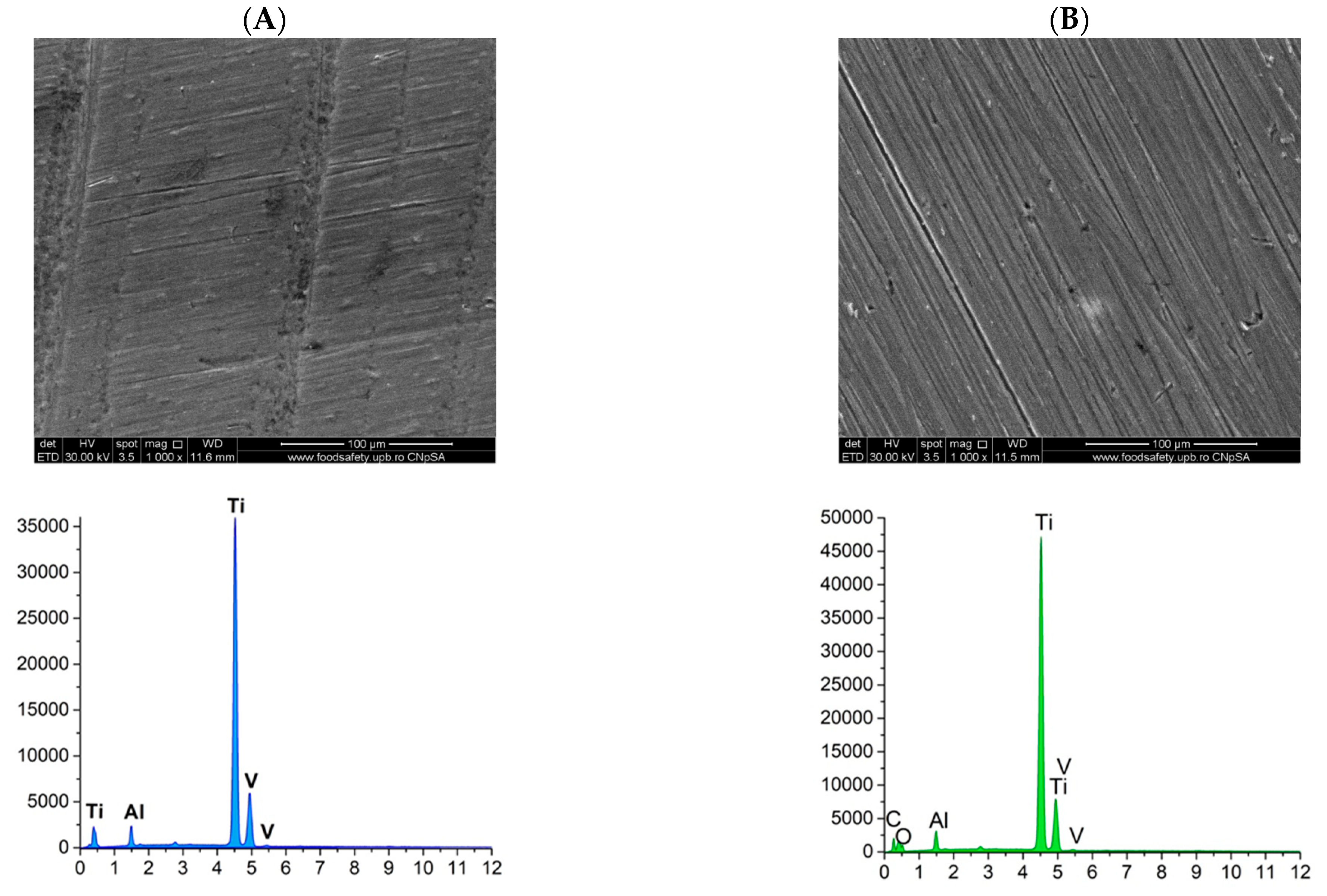
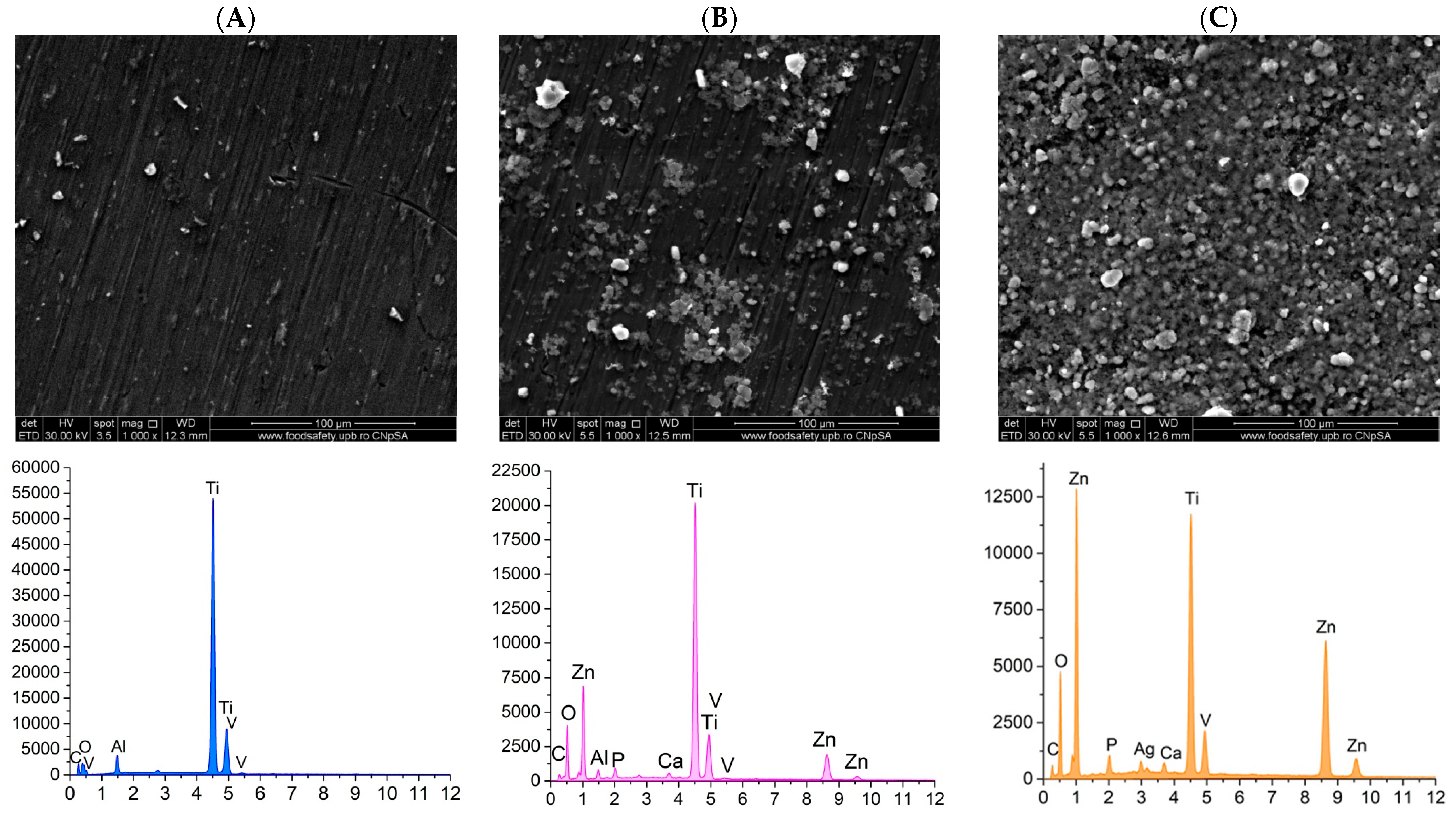
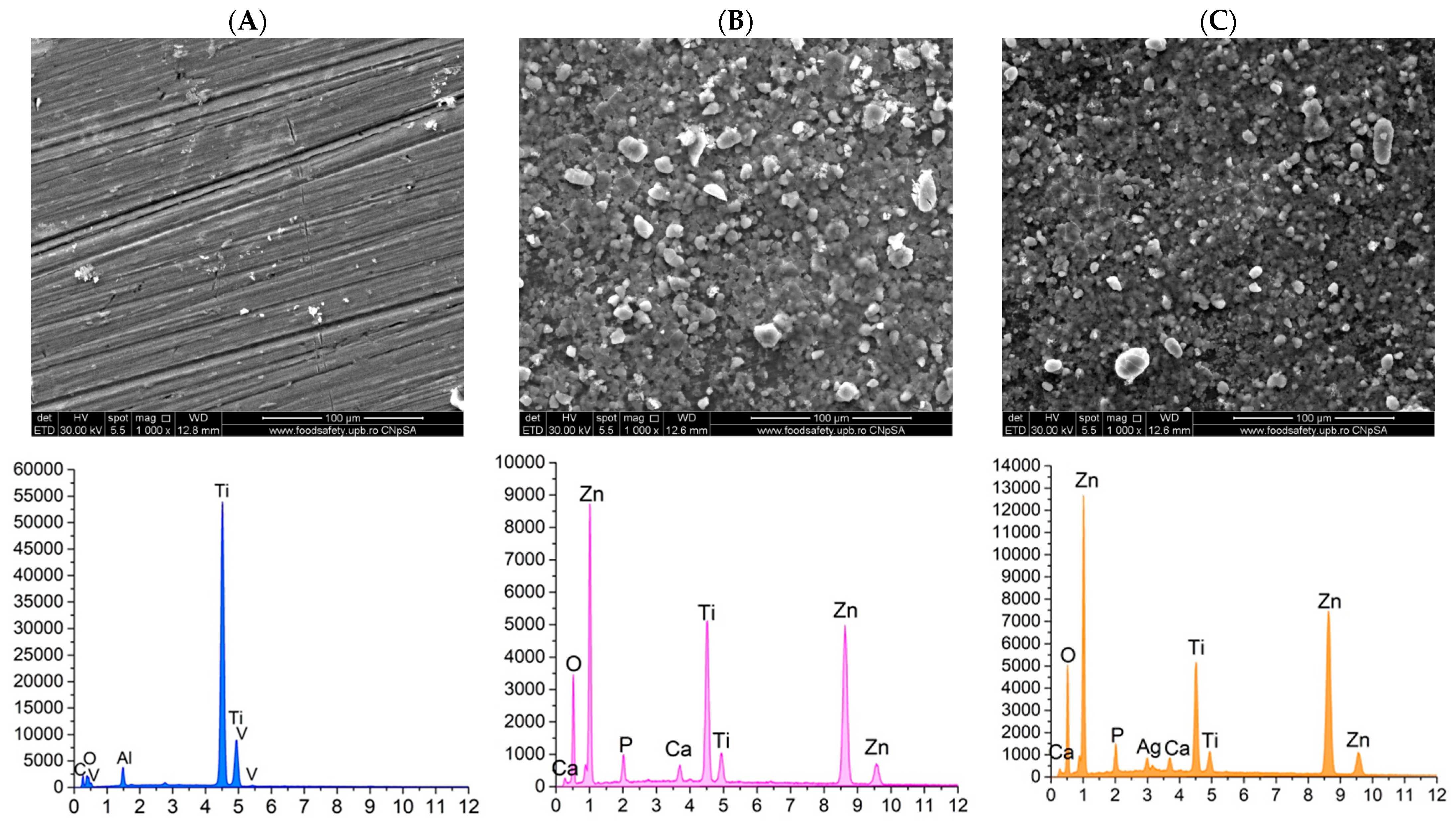
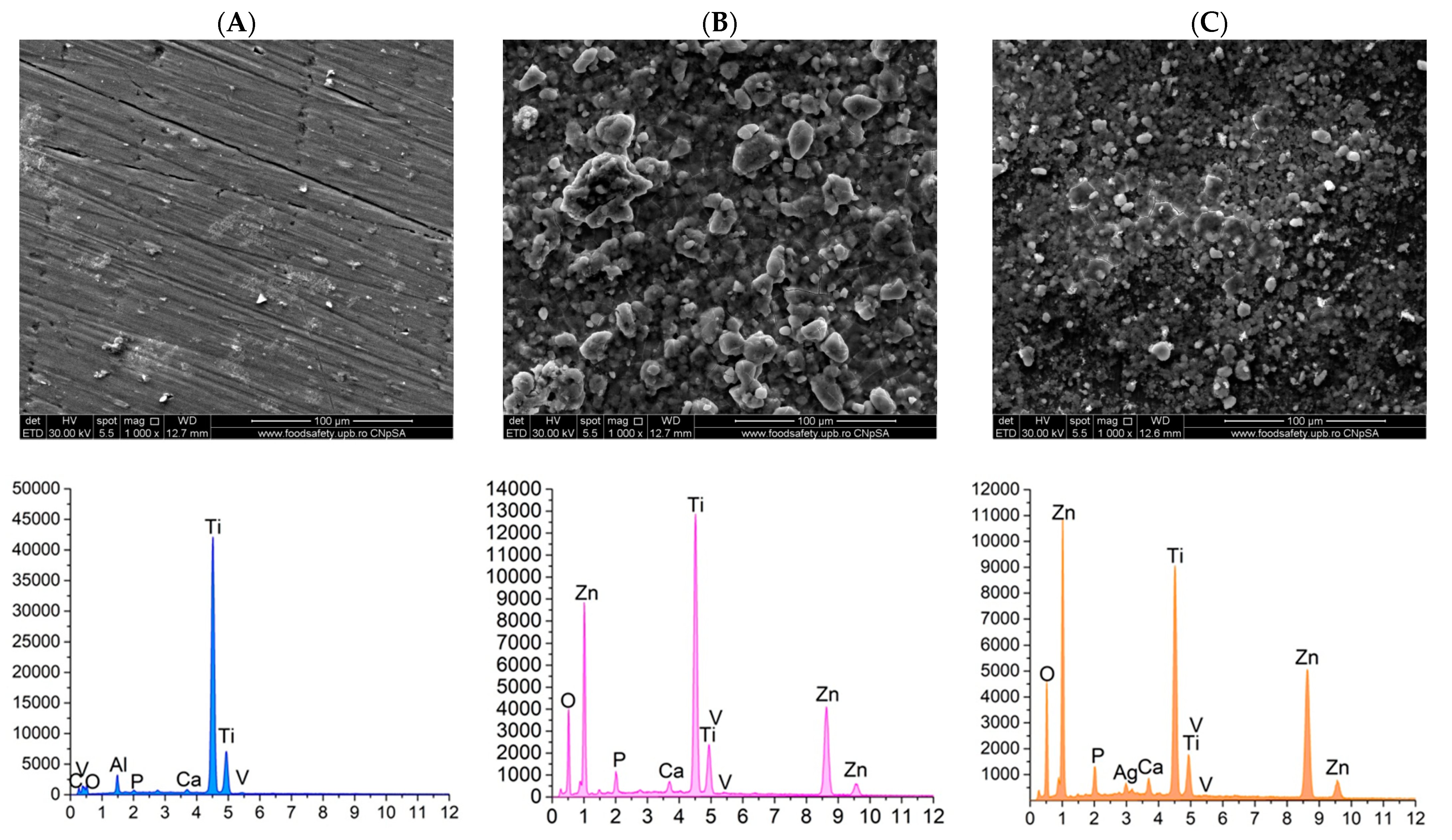
3.2.2. Scanning Electron Microscopy (SEM) and Energy Dispersive X-Ray Spectroscopy (EDS)
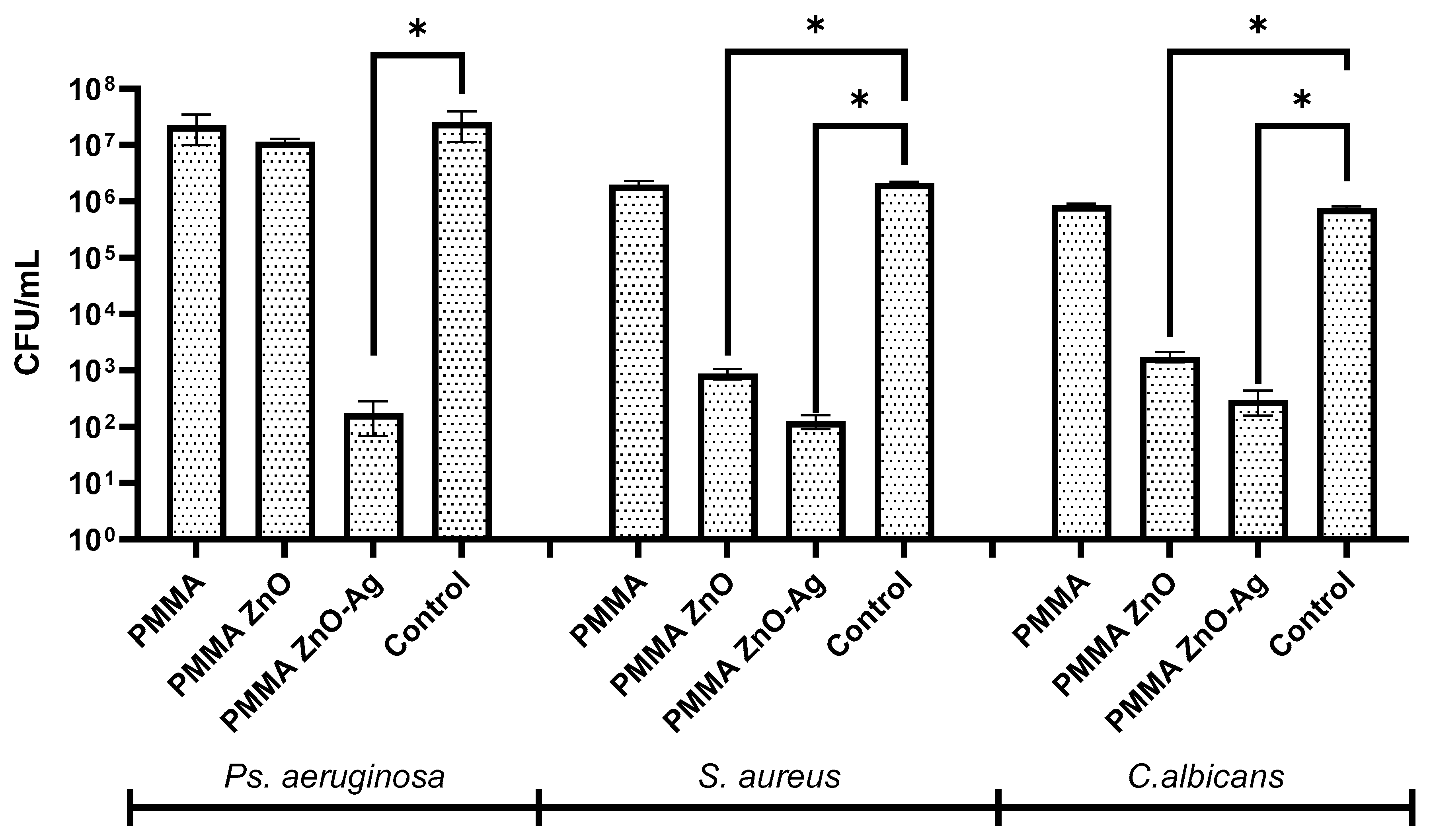
3.2.3. Biofilm Development
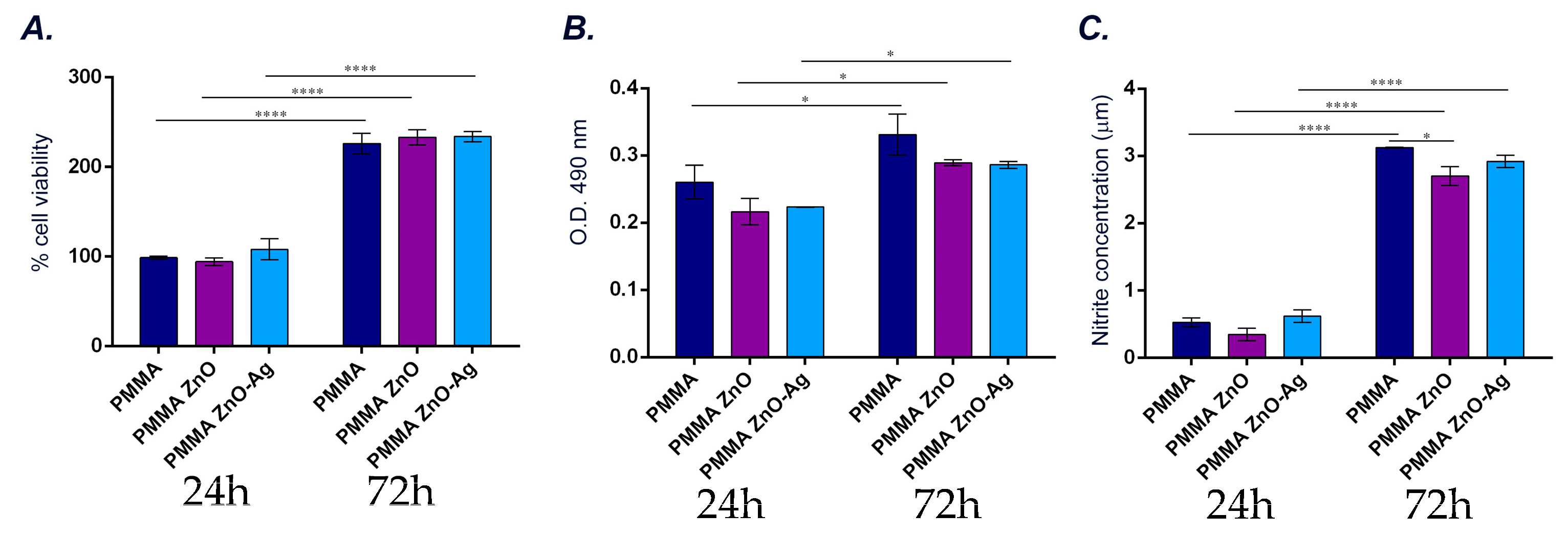
3.2.4. In Vitro Evaluation of Materials’ Impact on Human Fibroblasts’ Health
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rupp, F.; Liang, L.; Geis-Gerstorfer, J.; Scheideler, L.; Hüttig, F. Surface characteristics of dental implants: A review. Dent. Mater. 2018, 34, 40–57. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, W.J. Titanium Alloys for Dental Implants: A Review. Prosthesis 2020, 2, 100–116. [Google Scholar] [CrossRef]
- Halim, F.C.; Pesce, P.; De Angelis, N.; Benedicenti, S.; Menini, M. Comparison of the Clinical Outcomes of Titanium and Zirconia Implant Abutments: A Systematic Review of Systematic Reviews. J. Clin. Med. 2022, 11, 5052. [Google Scholar] [CrossRef] [PubMed]
- Benakatti, V.; Sajjanar, J.A.; Acharya, A.R. Dental implant abutments and their selection—A review. J. Evol. Med. Dent. Sci. 2021, 10, 3053–3059. [Google Scholar] [CrossRef]
- Al-Thobity, A.M. Titanium base abutments in implant prosthodontics: A literature review. Eur. J. Dent. 2022, 16, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Chantler, J.G.M.; Evans, C.D.J.; Zitzmann, N.U.; Derksen, W. Clinical performance of single implant prostheses restored using titanium base abutments: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2023, 34 (Suppl. S26), 64–85. [Google Scholar] [CrossRef] [PubMed]
- Dhesi, G.S.; Sidhu, S.; Al-Haj Husain, N.; Özcan, M. Evaluation of Adhesion Protocol for Titanium Base Abutments to Different Ceramic and Hybrid Materials. Eur. J. Prosthodont. Restor. Dent. 2021, 29, 22–34. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Gulati, K.; Li, Z.; Di, P.; Liu, Y. Dental Implant Nano-Engineering: Advances, Limitations and Future Directions. Nanomaterials 2021, 11, 2489. [Google Scholar] [CrossRef]
- Kurup, A.; Dhatrak, P.; Khasnis, N. Surface modification techniques of titanium and titanium alloys for biomedical dental applications: A review. Mater. Today Proc. 2021, 39, 84–90. [Google Scholar] [CrossRef]
- Canullo, L.; Menini, M.; Santori, G.; Rakic, M.; Sculean, A.; Pesce, P. Titanium abutment surface modifications and peri-implant tissue behavior: A systematic review and meta-analysis. Clin. Oral Investig. 2020, 24, 1113–1124. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Wang, M.; Jiang, T.; Zhou, Y.; Wang, Y. Roles of a new drug-delivery healing abutment in the prevention and treatment of peri-implant infections: A preliminary study. RSC Adv. 2018, 8, 38836–38843. [Google Scholar] [CrossRef] [PubMed]
- Wada, M.; Mameno, T.; Otsuki, M.; Kani, M.; Tsujioka, Y.; Ikebe, K. Prevalence and risk indicators for peri-implant diseases: A literature review. Jpn. Dent. Sci. Rev. 2021, 57, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Wychowański, P.; Nowak, M.; Miskiewicz, A.; Morawiec, T.; Woliński, J.; Kucharski, Z.; Passarelli, P.C.; Bodnarenko, A.; Lopez, M.A. The Effectiveness of a Bioactive Healing Abutment as a Local Drug Delivery System to Impact Peri-Implant Mucositis: A Prospective Case Series Study. Pharmaceutics 2023, 15, 138. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.M.S.; Suresh, G.; Dumpala, R.; Bradagunta, R.S. In Vitro Degradation Studies on Mg-Zn-CeO2 Composites for Biodegradable Implant Applications. Biointerface Res. Appl. Chem. 2024, 14, 86. [Google Scholar] [CrossRef]
- Iwańczyk, B.; Wychowański, P.; Minkiewicz-Zochniak, A.; Strom, K.; Jarzynka, S.; Olędzka, G. Bioactive Healing Abutment as a Potential Tool for the Treatment of Peri-Implant Disease—In Vitro Study. Appl. Sci. 2020, 10, 5376. [Google Scholar] [CrossRef]
- Lasserre, J.F.; Brecx, M.C.; Toma, S. Oral Microbes, Biofilms and Their Role in Periodontal and Peri-Implant Diseases. Materials 2018, 11, 1802. [Google Scholar] [CrossRef]
- Banu Raza, F.; Vijayaraghavalu, S.; Kandasamy, R.; Krishnaswami, V.; Kumar, V.A. Microbiome and the inflammatory pathway in peri-implant health and disease with an updated review on treatment strategies. J. Oral Biol. Craniofacial Res. 2023, 13, 84–91. [Google Scholar] [CrossRef]
- Li, Y.; Stewart, C.A.; Finer, Y. Advanced Antimicrobial and Anti-Infective Strategies to Manage Peri-Implant Infection: A Narrative Review. Dent. J. 2024, 12, 125. [Google Scholar] [CrossRef]
- Blank, E.; Grischke, J.; Winkel, A.; Eberhard, J.; Kommerein, N.; Doll, K.; Yang, I.; Stiesch, M. Evaluation of biofilm colonization on multi-part dental implants in a rat model. BMC Oral Health 2021, 21, 313. [Google Scholar] [CrossRef] [PubMed]
- Fragkioudakis, I.; Tseleki, G.; Doufexi, A.E.; Sakellari, D. Current Concepts on the Pathogenesis of Peri-implantitis: A Narrative Review. Eur. J. Dent. 2021, 15, 379–387. [Google Scholar] [CrossRef] [PubMed]
- de Avila, E.D.; van Oirschot, B.A.; van den Beucken, J. Biomaterial-based possibilities for managing peri-implantitis. J. Periodontal Res. 2020, 55, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Kunrath, M.F.; Gerhardt, M.d.N. Trans-mucosal platforms for dental implants: Strategies to induce muco-integration and shield peri-implant diseases. Dent. Mater. 2023, 39, 846–859. [Google Scholar] [CrossRef] [PubMed]
- Luke Yeo, I.-S. Dental Implants: Enhancing Biological Response Through Surface Modifications. Dent. Clin. N. Am. 2022, 66, 627–642. [Google Scholar] [CrossRef]
- Dong, H.; Liu, H.; Zhou, N.; Li, Q.; Yang, G.; Chen, L.; Mou, Y. Surface Modified Techniques and Emerging Functional Coating of Dental Implants. Coatings 2020, 10, 1012. [Google Scholar] [CrossRef]
- Kligman, S.; Ren, Z.; Chung, C.-H.; Perillo, M.A.; Chang, Y.-C.; Koo, H.; Zheng, Z.; Li, C. The Impact of Dental Implant Surface Modifications on Osseointegration and Biofilm Formation. J. Clin. Med. 2021, 10, 1641. [Google Scholar] [CrossRef] [PubMed]
- Pokrowiecki, R.; Szałaj, U.; Fudala, D.; Zaręba, T.; Wojnarowicz, J.; Łojkowski, W.; Tyski, S.; Dowgierd, K.; Mielczarek, A. Dental Implant Healing Screws as Temporary Oral Drug Delivery Systems for Decrease of Infections in the Area of the Head and Neck. Int. J. Nanomed. 2022, 17, 1679–1693. [Google Scholar] [CrossRef]
- Song, W.; Ge, S. Application of Antimicrobial Nanoparticles in Dentistry. Molecules 2019, 24, 1033. [Google Scholar] [CrossRef] [PubMed]
- Guerrero Correa, M.; Martínez, F.B.; Vidal, C.P.; Streitt, C.; Escrig, J.; de Dicastillo, C.L. Antimicrobial metal-based nanoparticles: A review on their synthesis, types and antimicrobial action. Beilstein J. Nanotechnol. 2020, 11, 1450–1469. [Google Scholar] [CrossRef] [PubMed]
- Rosli, N.A.; Teow, Y.H.; Mahmoudi, E. Current approaches for the exploration of antimicrobial activities of nanoparticles. Sci. Technol. Adv. Mater. 2021, 22, 885–907. [Google Scholar] [CrossRef] [PubMed]
- Bapat, R.A.; Joshi, C.P.; Bapat, P.; Chaubal, T.V.; Pandurangappa, R.; Jnanendrappa, N.; Gorain, B.; Khurana, S.; Kesharwani, P. The use of nanoparticles as biomaterials in dentistry. Drug Discov. Today 2019, 24, 85–98. [Google Scholar] [CrossRef]
- Choe, S.; Ma, T.; Jones, D.; Shiau, H.J.; Saito, H. Peri-implant mucosal tissue attachment: Narrative review. Dent. Rev. 2024, 4, 100141. [Google Scholar] [CrossRef]
- Díez-Pascual, A.M. PMMA-Based Nanocomposites for Odontology Applications: A State-of-the-Art. Int. J. Mol. Sci. 2022, 23, 10288. [Google Scholar] [CrossRef] [PubMed]
- Pituru, S.M.; Greabu, M.; Totan, A.; Imre, M.; Pantea, M.; Spinu, T.; Tancu, A.M.C.; Popoviciu, N.O.; Stanescu, I.-I.; Ionescu, E. A Review on the Biocompatibility of PMMA-Based Dental Materials for Interim Prosthetic Restorations with a Glimpse into Their Modern Manufacturing Techniques. Materials 2020, 13, 2894. [Google Scholar] [CrossRef] [PubMed]
- Zafar, M.S. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers 2020, 12, 2299. [Google Scholar] [CrossRef]
- Smeets, R.; Henningsen, A.; Jung, O.; Heiland, M.; Hammächer, C.; Stein, J.M. Definition, etiology, prevention and treatment of peri-implantitis—A review. Head. Face Med. 2014, 10, 34. [Google Scholar] [CrossRef] [PubMed]
- Renvert, S.; Persson, G.R.; Pirih, F.Q.; Camargo, P.M. Peri-implant health, peri-implant mucositis, and peri-implantitis: Case definitions and diagnostic considerations. J. Clin. Periodontol. 2018, 45 (Suppl. S20), S278–S285. [Google Scholar] [CrossRef] [PubMed]
- Kaur, H.; Thakur, A. Applications of poly(methyl methacrylate) polymer in dentistry: A review. Mater. Today Proc. 2022, 50, 1619–1625. [Google Scholar] [CrossRef]
- Dhage, S.B.; Sah, P.M.; Lakkakula, J.; Raut, R.W.; Malghe, Y.S.; Roy, A.; Verma, D.; Kaur, K. ZnO-CuO Nanocomposite Synthesized by Co-precipitation: Characterization and Antibacterial Properties. Biointerface Res. Appl. Chem. 2024, 14, 59. [Google Scholar] [CrossRef]
- Ghosh, T.; Das, A.B.; Jena, B.; Pradhan, C. Antimicrobial effect of silver zinc oxide (Ag-ZnO) nanocomposite particles. Front. Life Sci. 2015, 8, 47–54. [Google Scholar] [CrossRef]
- Lallo da Silva, B.; Abuçafy, M.P.; Berbel Manaia, E.; Oshiro Junior, J.A.; Chiari-Andréo, B.G.; Pietro, R.C.L.R.; Chiavacci, L.A. Relationship Between Structure And Antimicrobial Activity Of Zinc Oxide Nanoparticles: An Overview. Int. J. Nanomed. 2019, 14, 9395–9410. [Google Scholar] [CrossRef]
- Abass Sofi, M.; Sunitha, S.; Ashaq Sofi, M.; Khadheer Pasha, S.K.; Choi, D. An overview of antimicrobial and anticancer potential of silver nanoparticles. J. King Saud. Univ.-Sci. 2022, 34, 101791. [Google Scholar] [CrossRef]
- Kahraman, O.; Turunc, E.; Dogen, A.; Binzet, R. Synthesis of Graphene Quantum Dot Zinc Oxide Nanocomposites: Assessment of their Antioxidant and Antimicrobial Activity. Biointerface Res. Appl. Chem. 2024, 14, 9. [Google Scholar] [CrossRef]
- Kumar, N.; Sharma, R.; Aggarwal, N.K.; Singh, A.P. Utilization of Parthenium hysterophorus for the Synthesis of Lignin-ZnO Nanocomposites Aimed at Boosting Antibacterial and Antioxidant Activity. Lett. Appl. NanoBioSci. 2024, 13, 171. [Google Scholar] [CrossRef]
- Hosny, N.M.; Eissa, A.S.; Awadalla, A.A.; Barakat, L.A.A. Synthesis, Anti-oxidant and Cytotoxicity Activity of ZnO Nanoparticles Wrapped with Citrus aurantium. Lett. Appl. NanoBioSci. 2024, 13, 177. [Google Scholar] [CrossRef]
- Rayyif, S.M.I.; Mohammed, H.B.; Curuțiu, C.; Bîrcă, A.C.; Grumezescu, A.M.; Vasile, B.Ș.; Dițu, L.M.; Lazăr, V.; Chifiriuc, M.C.; Mihăescu, G.; et al. ZnO Nanoparticles-Modified Dressings to Inhibit Wound Pathogens. Materials 2021, 14, 3084. [Google Scholar] [CrossRef]
- Bîrcă, A.C.; Gherasim, O.; Niculescu, A.-G.; Grumezescu, A.M.; Vasile, B.Ș.; Mihaiescu, D.E.; Neacșu, I.A.; Andronescu, E.; Trușcă, R.; Holban, A.M.; et al. Infection-Free and Enhanced Wound Healing Potential of Alginate Gels Incorporating Silver and Tannylated Calcium Peroxide Nanoparticles. Int. J. Mol. Sci. 2024, 25, 5196. [Google Scholar] [CrossRef] [PubMed]
- Spirescu, V.A.; Șuhan, R.; Niculescu, A.-G.; Grumezescu, V.; Negut, I.; Holban, A.M.; Oprea, O.-C.; Bîrcă, A.C.; Vasile, B.Ș.; Grumezescu, A.M.; et al. Biofilm-Resistant Nanocoatings Based on ZnO Nanoparticles and Linalool. Nanomaterials 2021, 11, 2564. [Google Scholar] [CrossRef] [PubMed]
- Constantinescu, S.; Niculescu, A.-G.; Hudiță, A.; Grumezescu, V.; Rădulescu, D.; Bîrcă, A.C.; Irimiciuc, S.A.; Gherasim, O.; Holban, A.M.; Gălățeanu, B.; et al. Silver/Graphene Oxide Nanostructured Coatings for Modulating the Microbial Susceptibility of Fixation Devices Used in Knee Surgery. Int. J. Mol. Sci. 2024, 25, 246. [Google Scholar] [CrossRef] [PubMed]
- Florea, D.A.; Grumezescu, V.; Bîrcă, A.C.; Vasile, B.Ș.; Mușat, M.; Chircov, C.; Stan, M.S.; Grumezescu, A.M.; Andronescu, E.; Chifiriuc, M.C. Design, Characterization, and Antibacterial Performance of MAPLE-Deposited Coatings of Magnesium Phosphate-Containing Silver Nanoparticles in Biocompatible Concentrations. Int. J. Mol. Sci. 2022, 23, 7910. [Google Scholar] [CrossRef]
- Droepenu, E.K.; Wee, B.S.; Chin, S.F.; Kok, K.Y.; Maligan, M.F. Zinc oxide nanoparticles synthesis methods and its effect on morphology: A review. Biointerface Res. Appl. Chem. 2022, 12, 4261–4292. [Google Scholar]
- Nguyen, T.D.; Pham, N.M.; Thai, N.T.T.; Nguyen, H.T.T.; Hoang, Y.H.; Ha, A.C. Characterization and Applications of Silver Nanoparticles Photosynthesized from Durio Zibethinus Peel Extract. Biointerface Res. Appl. Chem. 2024, 14, 116. [Google Scholar] [CrossRef]
- Moradpoor, H.; Safaei, M.; Mozaffari, H.R.; Sharifi, R.; Imani, M.M.; Golshah, A.; Bashardoust, N. An overview of recent progress in dental applications of zinc oxide nanoparticles. RSC Adv. 2021, 11, 21189–21206. [Google Scholar] [CrossRef] [PubMed]
- Duman, H.; Eker, F.; Akdaşçi, E.; Witkowska, A.M.; Bechelany, M.; Karav, S. Silver Nanoparticles: A Comprehensive Review of Synthesis Methods and Chemical and Physical Properties. Nanomaterials 2024, 14, 1527. [Google Scholar] [CrossRef] [PubMed]
- Cierech, M.; Wojnarowicz, J.; Kolenda, A.; Krawczyk-Balska, A.; Prochwicz, E.; Woźniak, B.; Łojkowski, W.; Mierzwińska-Nastalska, E. Zinc Oxide Nanoparticles Cytotoxicity and Release from Newly Formed PMMA–ZnO Nanocomposites Designed for Denture Bases. Nanomaterials 2019, 9, 1318. [Google Scholar] [CrossRef] [PubMed]
- Pushpalatha, C.; Suresh, J.; Gayathri, V.S.; Sowmya, S.V.; Augustine, D.; Alamoudi, A.; Zidane, B.; Mohammad Albar, N.H.; Patil, S. Zinc Oxide Nanoparticles: A Review on Its Applications in Dentistry. Front. Bioeng. Biotechnol. 2022, 10, 917990. [Google Scholar] [CrossRef] [PubMed]
- Harb, S.V.; Trentin, A.; Uvida, M.C.; Magnani, M.; Pulcinelli, S.H.; Santilli, C.V.; Hammer, P. A comparative study on PMMA-TiO2 and PMMA-ZrO2 protective coatings. Prog. Org. Coat. 2020, 140, 105477. [Google Scholar] [CrossRef]
- Juan Carlos, F.-A.; Rene, G.-C.; Germán, V.-S.; Laura Susana, A.-T. Antimicrobial Poly (methyl methacrylate) with Silver Nanoparticles for Dentistry: A Systematic Review. Appl. Sci. 2020, 10, 4007. [Google Scholar] [CrossRef]
- Chawraba, K.; Damiri, F.; Toufaily, J.; Lalevee, J.; Hamieh, T. TiO2 Supported in Polymethyl methacrylate (PMMA) Properties, Preparation, and Photocatalytic Activity for the Degradation of Synthetic Dyes. Lett. Appl. NanoBioSci. 2024, 13, 13. [Google Scholar] [CrossRef]
- Nisticò, R.; Scalarone, D.; Magnacca, G. Sol-gel chemistry, templating and spin-coating deposition: A combined approach to control in a simple way the porosity of inorganic thin films/coatings. Microporous Mesoporous Mater. 2017, 248, 18–29. [Google Scholar] [CrossRef]
- Lukong, V.T.; Ukoba, K.; Jen, T.-C. Review of self-cleaning TiO2 thin films deposited with spin coating. Int. J. Adv. Manuf. Technol. 2022, 122, 3525–3546. [Google Scholar] [CrossRef]
- Butt, M.A. Thin-Film Coating Methods: A Successful Marriage of High-Quality and Cost-Effectiveness—A Brief Exploration. Coatings 2022, 12, 1115. [Google Scholar] [CrossRef]
- Yin, Y. Advances and perspectives of spin coating techniques. Appl. Comput. Eng. 2023, 7, 291–301. [Google Scholar] [CrossRef]
- Duan, G.; Zhang, C.; Li, A.; Yang, X.; Lu, L.; Wang, X. Preparation and Characterization of Mesoporous Zirconia Made by Using a Poly (methyl methacrylate) Template. Nanoscale Res. Lett. 2008, 3, 118. [Google Scholar] [CrossRef] [PubMed]
- Stuart, B.W.; Gimeno-Fabra, M.; Segal, J.; Ahmed, I.; Grant, D.M. Degradation and Characterization of Resorbable Phosphate-Based Glass Thin-Film Coatings Applied by Radio-Frequency Magnetron Sputtering. ACS Appl. Mater. Interfaces 2015, 7, 27362–27372. [Google Scholar] [CrossRef] [PubMed]
- Baino, F.; Yamaguchi, S. The Use of Simulated Body Fluid (SBF) for Assessing Materials Bioactivity in the Context of Tissue Engineering: Review and Challenges. Biomimetics 2020, 5, 57. [Google Scholar] [CrossRef] [PubMed]
- Liu, Q.; Liu, E.; Li, J.; Qiu, Y.; Chen, R. Rapid ultrasonic-microwave assisted synthesis of spindle-like Ag/ZnO nanostructures and their enhanced visible-light photocatalytic and antibacterial activities. Catal. Today 2020, 339, 391–402. [Google Scholar] [CrossRef]
- Sudhisha, V.; Saranya, K.; Kalaiyarasan, M.; Rajendran, N. Silver nanoparticles doped poly(3, 4-ethylene dioxythiophene) on titania nanotubes for orthopaedic application. Appl. Surf. Sci. 2023, 610, 155416. [Google Scholar] [CrossRef]
- Raj, I.; Mozetic, M.; Jayachandran, V.; Jose, J.; Thomas, S.; Kalarikkal, N. Fracture resistant, antibiofilm adherent, self-assembled PMMA/ZnO nanoformulations for biomedical applications: Physico-chemical and biological perspectives of nano reinforcement. Nanotechnology 2018, 29, 305704. [Google Scholar] [CrossRef]
- Zaharia, A.; Muşat, V.; Pleşcan Ghisman, V.; Baroiu, N. Antimicrobial hybrid biocompatible materials based on acrylic copolymers modified with (Ag)ZnO/chitosan composite nanoparticles. Eur. Polym. J. 2016, 84, 550–564. [Google Scholar] [CrossRef]
- Cierech, M.; Kolenda, A.; Grudniak, A.M.; Wojnarowicz, J.; Woźniak, B.; Gołaś, M.; Swoboda-Kopeć, E.; Łojkowski, W.; Mierzwińska-Nastalska, E. Significance of polymethylmethacrylate (PMMA) modification by zinc oxide nanoparticles for fungal biofilm formation. Int. J. Pharm. 2016, 510, 323–335. [Google Scholar] [CrossRef] [PubMed]
- Toledano, M.; Vallecillo-Rivas, M.; Aguilera, F.S.; Osorio, M.T.; Osorio, E.; Osorio, R. Polymeric zinc-doped nanoparticles for high performance in restorative dentistry. J. Dent. 2021, 107, 103616. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Kim, Y.-J.; Yang, Y.-J.; Lee, J.-H.; Lee, H.-H. Development of antibacterial dual-cure dental resin composites via tetrapod-shaped zinc oxide incorporation. Dent. Mater. 2024, 40, 1762–1772. [Google Scholar] [CrossRef]
- Garibay-Alvarado, J.A.; Garcia-Zamarron, D.J.; Silva-Holguín, P.N.; Donohue-Cornejo, A.; Cuevas-González, J.C.; Espinosa-Cristóbal, L.F.; Ruíz-Baltazar, Á.D.; Reyes-López, S.Y. Polymer-Based Hydroxyapatite–Silver Composite Resin with Enhanced Antibacterial Activity for Dental Applications. Polymers 2024, 16, 2017. [Google Scholar] [CrossRef] [PubMed]
- Boschetto, F.; Honma, T.; Adachi, T.; Kanamura, N.; Zhu, W.; Yamamoto, T.; Marin, E.; Pezzotti, G. Development and evaluation of osteogenic PMMA bone cement composite incorporating curcumin for bone repairing. Mater. Today Chem. 2023, 27, 101307. [Google Scholar] [CrossRef]
- Ramanathan, S.; Lin, Y.-C.; Thirumurugan, S.; Hu, C.-C.; Duann, Y.-F.; Chung, R.-J. Poly(methyl methacrylate) in Orthopedics: Strategies, Challenges, and Prospects in Bone Tissue Engineering. Polymers 2024, 16, 367. [Google Scholar] [CrossRef] [PubMed]
- Fais, G.; Sidorowicz, A.; Perra, G.; Dessì, D.; Loy, F.; Lai, N.; Follesa, P.; Orrù, R.; Cao, G.; Concas, A. Cytotoxic Effects of ZnO and Ag Nanoparticles Synthesized in Microalgae Extracts on PC12 Cells. Mar. Drugs 2024, 22, 549. [Google Scholar] [CrossRef]
- Dutta, G.; Chinnaiyan, S.K.; Sugumaran, A.; Narayanasamy, D. Sustainable bioactivity enhancement of ZnO-Ag nanoparticles in antimicrobial, antibiofilm, lung cancer, and photocatalytic applications. RSC Adv. 2023, 13, 26663–26682. [Google Scholar] [CrossRef] [PubMed]
- Maheswaran, H.; Djearamane, S.; Tanislaus Antony Dhanapal, A.C.; Wong, L.S. Cytotoxicity of green synthesized zinc oxide nanoparticles using Musa acuminata on Vero cells. Heliyon 2024, 10, e31316. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rehner, A.M.G.; Tudorache, D.-I.; Bîrcă, A.C.; Nicoară, A.I.; Niculescu, A.-G.; Holban, A.M.; Hudiță, A.; Bîclesanu, F.C.; Balaure, P.C.; Pangică, A.M.; et al. Antibacterial Properties of PMMA/ZnO(NanoAg) Coatings for Dental Implant Abutments. Materials 2025, 18, 382. https://doi.org/10.3390/ma18020382
Rehner AMG, Tudorache D-I, Bîrcă AC, Nicoară AI, Niculescu A-G, Holban AM, Hudiță A, Bîclesanu FC, Balaure PC, Pangică AM, et al. Antibacterial Properties of PMMA/ZnO(NanoAg) Coatings for Dental Implant Abutments. Materials. 2025; 18(2):382. https://doi.org/10.3390/ma18020382
Chicago/Turabian StyleRehner (Costache), Ana Maria Gianina, Dana-Ionela Tudorache, Alexandra Cătălina Bîrcă, Adrian Ionuț Nicoară, Adelina-Gabriela Niculescu, Alina Maria Holban, Ariana Hudiță, Florentina Cornelia Bîclesanu, Paul Cătălin Balaure, Anna Maria Pangică, and et al. 2025. "Antibacterial Properties of PMMA/ZnO(NanoAg) Coatings for Dental Implant Abutments" Materials 18, no. 2: 382. https://doi.org/10.3390/ma18020382
APA StyleRehner, A. M. G., Tudorache, D.-I., Bîrcă, A. C., Nicoară, A. I., Niculescu, A.-G., Holban, A. M., Hudiță, A., Bîclesanu, F. C., Balaure, P. C., Pangică, A. M., Grumezescu, A. M., & Croitoru, G.-A. (2025). Antibacterial Properties of PMMA/ZnO(NanoAg) Coatings for Dental Implant Abutments. Materials, 18(2), 382. https://doi.org/10.3390/ma18020382











