In Vivo Wear Analysis of Leucite-Reinforced Ceramic Inlays/Onlays After 14 Years
Abstract
1. Introduction
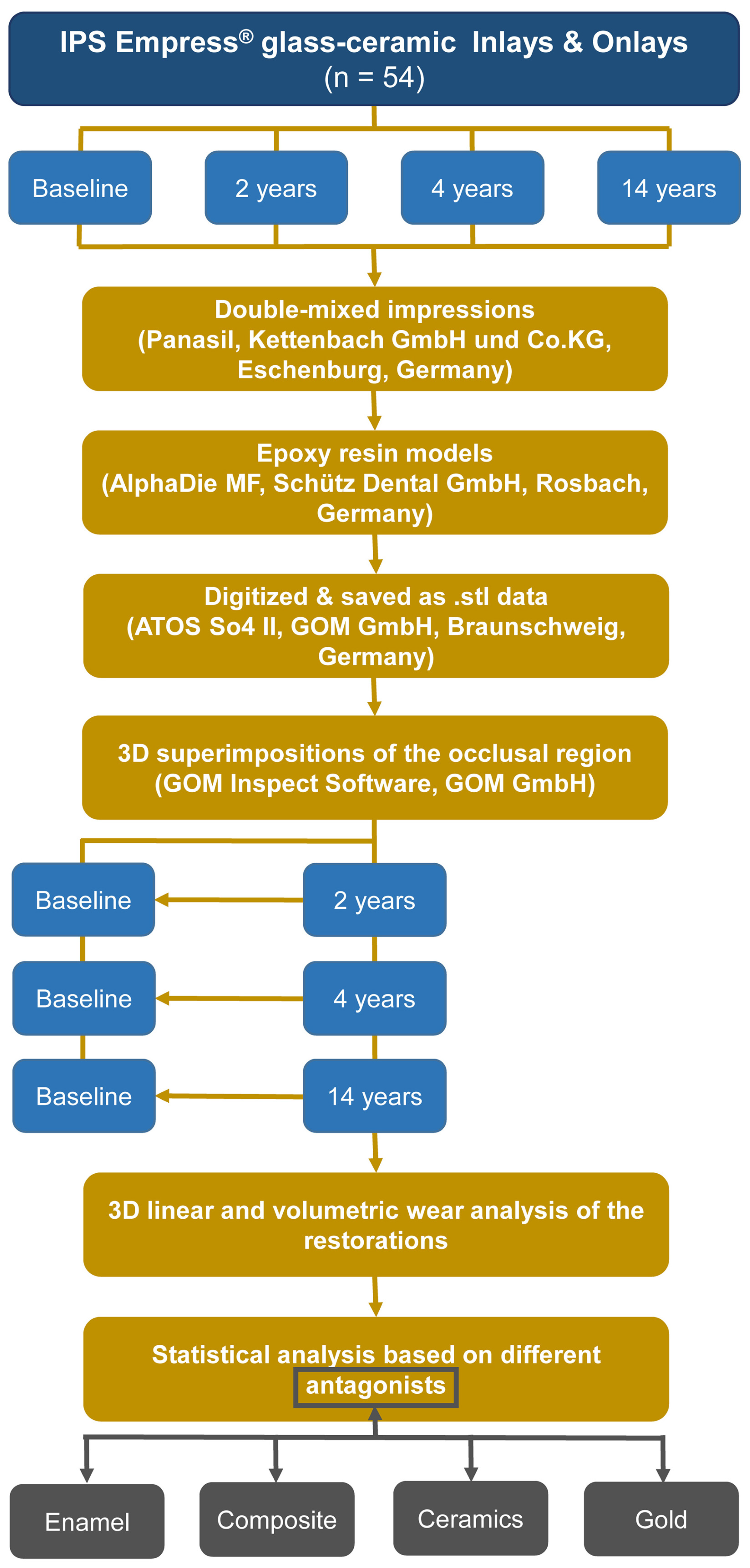
2. Materials and Methods
2.1. Study Design
2.2. Subject Recruitment and Intervention
2.3. Three-Dimensional Data Acquisition and Volumetric Measurements
2.4. Statistical Data Analysis
3. Results
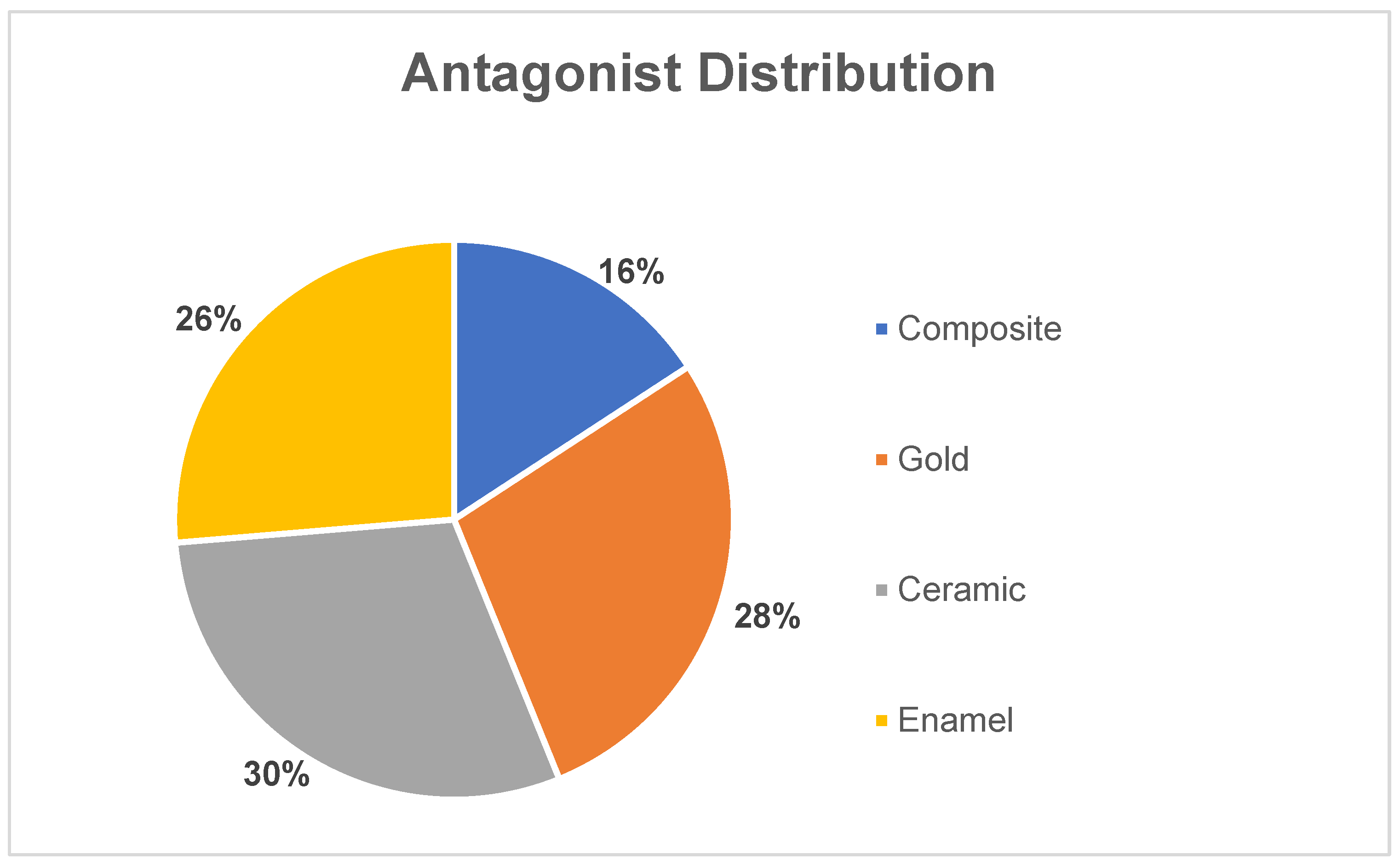
3.1. Study Population
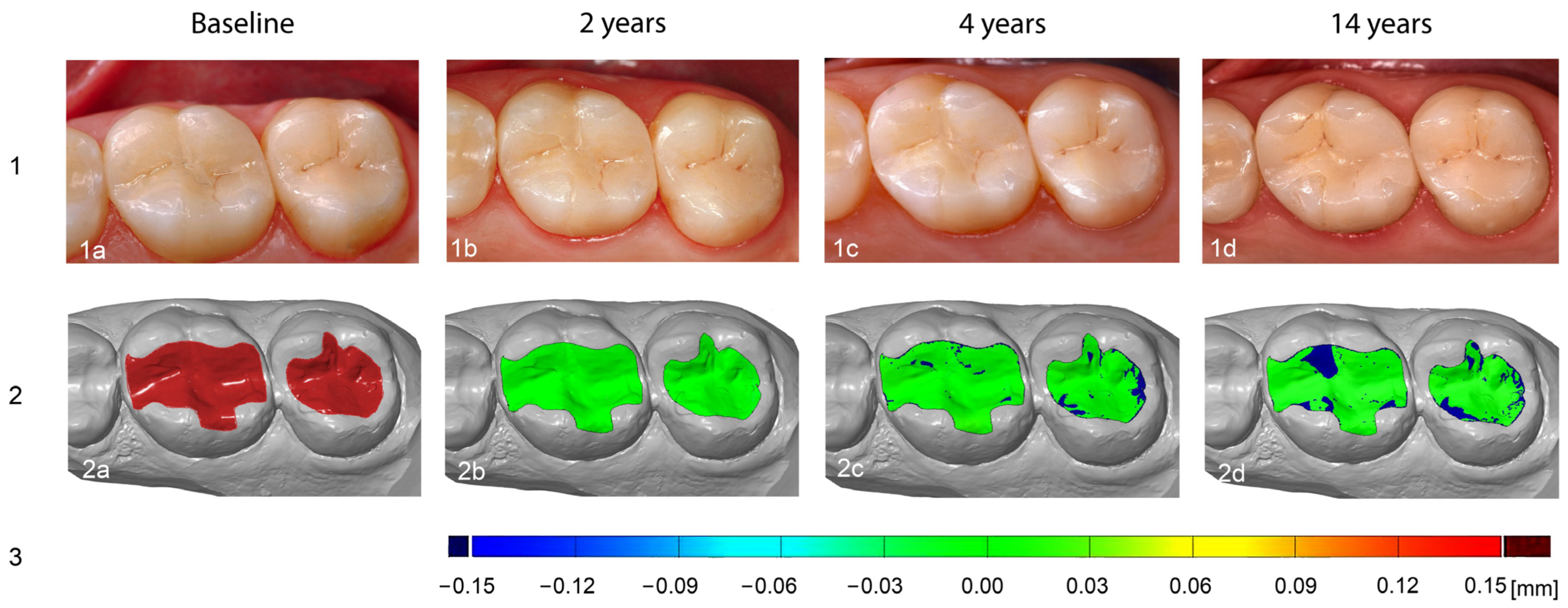
3.2. Substance Loss Analysis Methodology
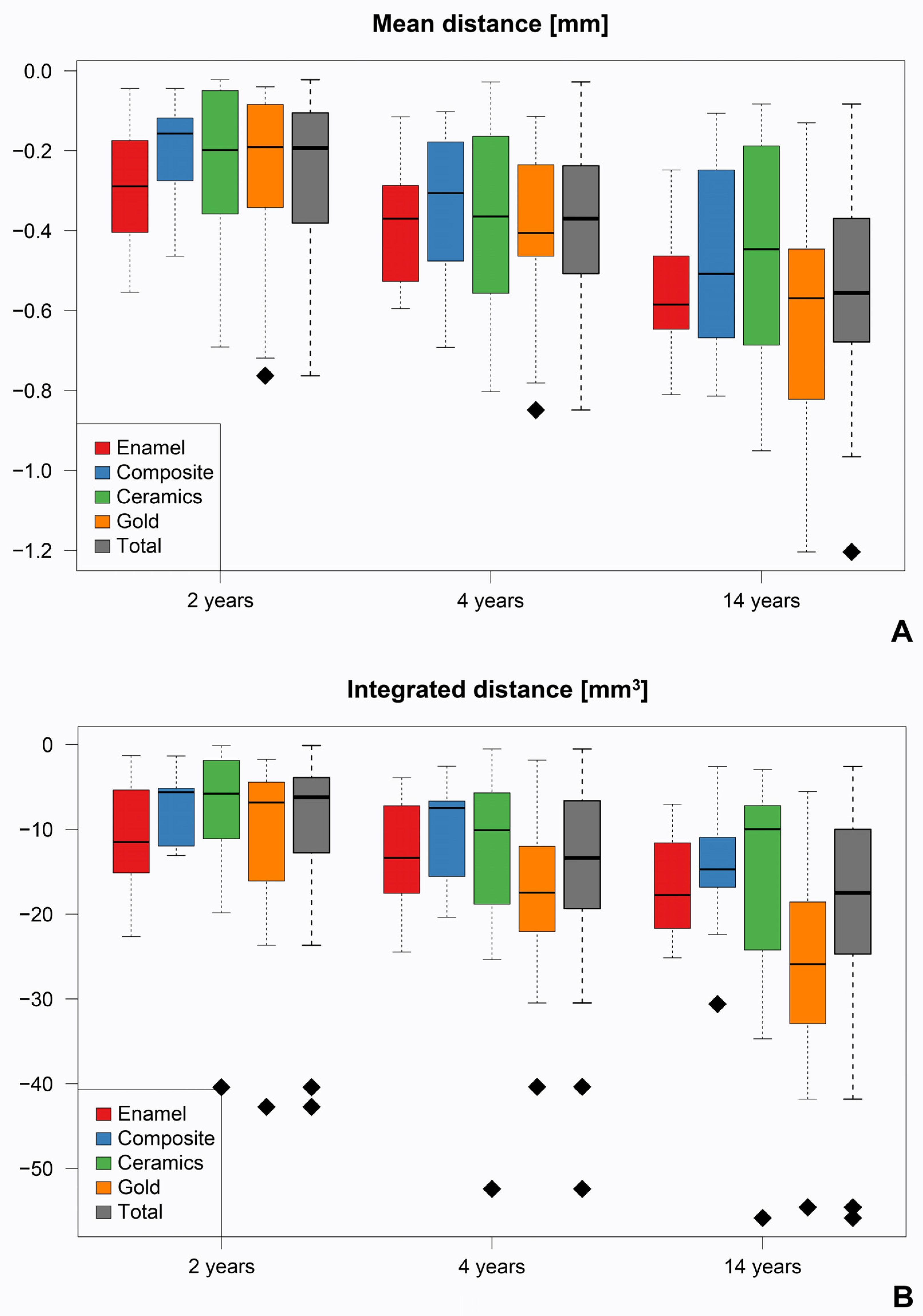
3.3. Average Surface Loss
3.4. Volume Decrease
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| 3D | three-dimensional |
| EN | European norm |
| MOD | Mesial–occlusal–distal |
| ROI | region of interest |
| CONSORT | Consolidated Standards of Reporting Trials |
References
- Meyer, A., Jr.; Cardoso, L.C.; Araujo, E.; Baratieri, L.N. Ceramic inlays and onlays: Clinical procedures for predictable results. J. Esthet. Restor. Dent. 2003, 15, 338–351; discussion 352. [Google Scholar] [CrossRef] [PubMed]
- Hopp, C.D.; Land, M.F. Considerations for ceramic inlays in posterior teeth: A review. Clin. Cosmet. Investig. Dent. 2013, 5, 21–32. [Google Scholar] [CrossRef] [PubMed]
- Al-Fouzan, A.F.; Tashkandi, E.A. Volumetric measurements of removed tooth structure associated with various preparation designs. Int. J. Prosthodont. 2013, 26, 545–548. [Google Scholar] [CrossRef] [PubMed]
- Collares, K.; Corrêa, M.B.; Laske, M.; Kramer, E.; Reiss, B.; Moraes, R.R.; Huysmans, M.C.; Opdam, N.J. A practice-based research network on the survival of ceramic inlay/onlay restorations. Dent. Mater. 2016, 32, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Forna, N.C.; Uleanu, R.; Lungu, I.; Dimofte, A.-R. Dental ceramics: Advantages and benefits. Practice 2024, 4, 7. [Google Scholar]
- Contrepois, M.; Soenen, A.; Bartala, M.; Laviole, O. Marginal adaptation of ceramic crowns: A systematic review. J. Prosthet. Dent. 2013, 110, 447–454.e410. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.R.; Benetti, P. Ceramic materials in dentistry: Historical evolution and current practice. Aust. Dent. J. 2011, 56 (Suppl. 1), 84–96. [Google Scholar] [CrossRef] [PubMed]
- Sen, N.; Us, Y.O. Mechanical and optical properties of monolithic CAD-CAM restorative materials. J. Prosthet. Dent. 2018, 119, 593–599. [Google Scholar] [CrossRef] [PubMed]
- Albakry, M.; Guazzato, M.; Swain, M.V. Influence of hot pressing on the microstructure and fracture toughness of two pressable dental glass-ceramics. J. Biomed. Mater. Res. B Appl. Biomater. 2004, 71, 99–107. [Google Scholar] [CrossRef] [PubMed]
- El-Mowafy, O.; Brochu, J.F. Longevity and clinical performance of IPS-Empress ceramic restorations—A literature review. J. Can. Dent. Assoc. 2002, 68, 233–237. [Google Scholar] [PubMed]
- Abdulrahman, S.; Von See Mahm, C.; Talabani, R.; Abdulateef, D. Evaluation of the clinical success of four different types of lithium disilicate ceramic restorations: A retrospective study. BMC Oral Health 2021, 21, 625. [Google Scholar] [CrossRef] [PubMed]
- Manhart, J.; Chen, H.; Hamm, G.; Hickel, R. Buonocore Memorial Lecture. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper. Dent. 2004, 29, 481–508. [Google Scholar] [PubMed]
- Yip, K.H.; Smales, R.J.; Kaidonis, J.A. Differential wear of teeth and restorative materials: Clinical implications. Int. J. Prosthodont. 2004, 17, 350–356. [Google Scholar] [PubMed]
- Sripetchdanond, J.; Leevailoj, C. Wear of human enamel opposing monolithic zirconia, glass ceramic, and composite resin: An in vitro study. J. Prosthet. Dent. 2014, 112, 1141–1150. [Google Scholar] [CrossRef] [PubMed]
- Lambrechts, P.; Braem, M.; Vuylsteke-Wauters, M.; Vanherle, G. Quantitative in vivo wear of human enamel. J. Dent. Res. 1989, 68, 1752–1754. [Google Scholar] [CrossRef] [PubMed]
- Dupriez, N.D.; von Koeckritz, A.K.; Kunzelmann, K.H. A comparative study of sliding wear of nonmetallic dental restorative materials with emphasis on micromechanical wear mechanisms. J. Biomed. Mater. Res. B Appl. Biomater. 2015, 103, 925–934. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho Ramos, N.; Augusto, M.G.; Alves, L.M.M.; Kleverlaan, C.J.; Dal Piva, A.M.d.O. Wear of dental ceramics. Braz. Dent. Sci. 2023, 26, e3638. [Google Scholar] [CrossRef]
- Osiewicz, M.A.; Werner, A.; Roeters, F.J.M.; Kleverlaan, C.J. Wear of direct resin composites and teeth: Considerations for oral rehabilitation. Eur. J. Oral Sci. 2019, 127, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Schlueter, N.; Amaechi, B.T.; Bartlett, D.; Buzalaf, M.A.R.; Carvalho, T.S.; Ganss, C.; Hara, A.T.; Huysmans, M.; Lussi, A.; Moazzez, R.; et al. Terminology of Erosive Tooth Wear: Consensus Report of a Workshop Organized by the ORCA and the Cariology Research Group of the IADR. Caries Res. 2020, 54, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Lobbezoo, F.; Ahlberg, J.; Raphael, K.G.; Wetselaar, P.; Glaros, A.G.; Kato, T.; Santiago, V.; Winocur, E.; De Laat, A.; De Leeuw, R.; et al. International consensus on the assessment of bruxism: Report of a work in progress. J. Oral Rehabil. 2018, 45, 837–844. [Google Scholar] [CrossRef] [PubMed]
- Dahl, B.L.; Carlsson, G.E.; Ekfeldt, A. Occlusal wear of teeth and restorative materials. A review of classification, etiology, mechanisms of wear, and some aspects of restorative procedures. Acta Odontol. Scand. 1993, 51, 299–311. [Google Scholar] [CrossRef] [PubMed]
- Maier, E.; Grottschreiber, C.; Knepper, I.; Opdam, N.; Petschelt, A.; Loomans, B.; Lohbauer, U. Evaluation of wear behavior of dental restorative materials against zirconia in vitro. Dent. Mater. 2022, 38, 778–788. [Google Scholar] [CrossRef] [PubMed]
- Someya, T.; Kasahara, M.; Takemoto, S.; Hattori, M. The Wear Behavior of Glass-Ceramic CAD/CAM Blocks against Bovine Enamel. Materials 2023, 16, 6839. [Google Scholar] [CrossRef] [PubMed]
- Holst, S.; Karl, M.; Wichmann, M.; Matta, R.E. A technique for in vitro fit assessment of multi-unit screw-retained implant restorations: Application of a triple-scan protocol. J. Dent. Biomech. 2012, 3, 1758736012452181. [Google Scholar] [CrossRef] [PubMed]
- Jeon, J.H.; Kim, H.Y.; Kim, J.H.; Kim, W.C. Accuracy of 3D white light scanning of abutment teeth impressions: Evaluation of trueness and precision. J. Adv. Prosthodont. 2014, 6, 468–473. [Google Scholar] [CrossRef] [PubMed]
- Jeon, J.H.; Choi, B.Y.; Kim, C.M.; Kim, J.H.; Kim, H.Y.; Kim, W.C. Three-dimensional evaluation of the repeatability of scanned conventional impressions of prepared teeth generated with white- and blue-light scanners. J. Prosthet. Dent. 2015, 114, 549–553. [Google Scholar] [CrossRef] [PubMed]
- Theocharopoulos, A.; Chen, X.; Hill, R.; Cattell, M.J. Reduced wear of enamel with novel fine and nano-scale leucite glass-ceramics. J. Dent. 2013, 41, 561–568. [Google Scholar] [CrossRef] [PubMed]
- Cherian, J.; Jayakumar, R.; James, J.; Thomas, V.; Sramadathil, S.; Sasi, A.K. A comparative evaluation of enamel wear against different surface finished ceramics: An in vitro study. Cureus 2023, 15, e44689. [Google Scholar] [CrossRef] [PubMed]
- Elmaria, A.; Goldstein, G.; Vijayaraghavan, T.; Legeros, R.Z.; Hittelman, E.L. An evaluation of wear when enamel is opposed by various ceramic materials and gold. J. Prosthet. Dent. 2006, 96, 345–353. [Google Scholar] [CrossRef] [PubMed]
- Etman, M. Wear properties of dental ceramics. In Non-Metallic Biomaterials for Tooth Repair and Replacement; Elsevier: Amsterdam, The Netherlands, 2013; pp. 161–193. [Google Scholar]
- Heintze, S.D.; Cavalleri, A.; Forjanic, M.; Zellweger, G.; Rousson, V. Wear of ceramic and antagonist--a systematic evaluation of influencing factors in vitro. Dent. Mater. 2008, 24, 433–449. [Google Scholar] [CrossRef] [PubMed]
- Needleman, I.; Worthington, H.; Moher, D.; Schulz, K.; Altman, D.G. Improving the completeness and transparency of reports of randomized trials in oral health: The CONSORT statement. Am. J. Dent. 2008, 21, 7. [Google Scholar] [PubMed]
- Frankenberger, R.; Taschner, M.; Garcia-Godoy, F.; Petschelt, A.; Krämer, N. Leucite-reinforced glass ceramic inlays and onlays after 12 years. J. Adhes. Dent. 2008, 10, 393–398. [Google Scholar] [PubMed]
- Krämer, N.; Kunzelmann, K.-H.; Taschner, M.; Mehl, A.; Garcia-Godoy, F.; Frankenberger, R. Antagonist enamel wears more than ceramic inlays. J. Dent. Res. 2006, 85, 1097–1100. [Google Scholar] [CrossRef] [PubMed]
- Taschner, M.; Frankenberger, R.; Garcia-Godoy, F. IPS Empress inlays luted with a self-adhesive resin cement after 1 year. Am. J. Dent. 2009, 22, 55. [Google Scholar] [PubMed]
- Taschner, M.; Stirnweiss, A.; Frankenberger, R.; Kramer, N.; Galler, K.M.; Maier, E. Fourteen years clinical evaluation of leucite-reinforced ceramic inlays luted using two different adhesion strategies. J. Dent. 2022, 123, 104210. [Google Scholar] [CrossRef] [PubMed]
- Beham, G. IPS Empress: Eine Neue Keramik Techologie; ZWR: Stuttgart, Germany, 1991; Volume 100. [Google Scholar]
- Vlaar, S.T.; van der Zel, J.M. Accuracy of dental digitizers. Int. Dent. J. 2006, 56, 301–309. [Google Scholar] [CrossRef] [PubMed]
- Matta, R.E.; von Wilmowsky, C.; Neuhuber, W.; Lell, M.; Neukam, F.W.; Adler, W.; Wichmann, M.; Bergauer, B. The impact of different cone beam computed tomography and multi-slice computed tomography scan parameters on virtual three-dimensional model accuracy using a highly precise ex vivo evaluation method. J. Craniomaxillofac. Surg. 2016, 44, 632–636. [Google Scholar] [CrossRef] [PubMed]
- Holst, S.; Karl, M.; Wichmann, M.; Matta, R.E. A new triple-scan protocol for 3D fit assessment of dental restorations. Quintessence Int. 2011, 42, 651–657. [Google Scholar] [PubMed]
- Zimmermann, M.; Mehl, A.; Mörmann, W.H.; Reich, S. Intraoral scanning systems—A current overview. Int. J. Comput. Dent. 2015, 18, 101–129. [Google Scholar] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2024; Available online: https://www.R-project.org/ (accessed on 30 May 2024).
- Malament, K.A.; Natto, Z.S.; Thompson, V.; Rekow, D.; Eckert, S.; Weber, H.P. Ten-year survival of pressed, acid-etched e.max lithium disilicate monolithic and bilayered complete-coverage restorations: Performance and outcomes as a function of tooth position and age. J. Prosthet. Dent. 2019, 121, 782–790. [Google Scholar] [CrossRef] [PubMed]
- Dondani, J.R.; Pardeshi, V.; Gangurde, A.; Shaikh, A.; Mahule, A.; Deval, P. Comparative Evaluation of Wear of Natural Enamel Antagonist Against Glazed Monolithic Zirconia Crowns and Polished Monolithic Zirconia Crowns: An In Vivo Study. Int. J. Prosthodont. 2023, 36, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Almejrad, L.; Almansour, A.; Bartlett, D.; Austin, R. CAD/CAM leucite-reinforced glass-ceramic for simulation of attrition in human enamel in vitro. Dent. Mater. 2024, 40, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Murbay, S.; Yeung, S.K.W.; Yip, C.Y.; Pow, E.H.N. Assessing Enamel Wear of Monolithic Ceramics with Micro-CT and Intra-oral Scanner. Int. Dent. J. 2023, 73, 496–502. [Google Scholar] [CrossRef] [PubMed]
- Krejci, I.; Lutz, F. In-vitro test results of the evaluation of dental restoration systems. Correlation with in-vivo results. Schweiz. Monatsschr. Zahnmed. 1990, 100, 1445–1449. [Google Scholar] [PubMed]
- Aladağ, A.; Oğuz, D.; Çömlekoğlu, M.E.; Akan, E. In vivo wear determination of novel CAD/CAM ceramic crowns by using 3D alignment. J. Adv. Prosthodont. 2019, 11, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Ohlmann, B.; Trame, J.P.; Dreyhaupt, J.; Gabbert, O.; Koob, A.; Rammelsberg, P. Wear of posterior metal-free polymer crowns after 2 years. J. Oral Rehabil. 2008, 35, 782–788. [Google Scholar] [CrossRef] [PubMed]
- Hickel, R.; Peschke, A.; Tyas, M.; Mjör, I.; Bayne, S.; Peters, M.; Hiller, K.-A.; Randall, R.; Vanherle, G.; Heintze, S.D. FDI World Dental Federation: Clinical criteria for the evaluation of direct and indirect restorations—Update and clinical examples. Clin. Oral Investig. 2010, 14, 349–366. [Google Scholar] [CrossRef] [PubMed]
- Suputtamongkol, K.; Anusavice, K.J.; Suchatlampong, C.; Sithiamnuai, P.; Tulapornchai, C. Clinical performance and wear characteristics of veneered lithia-disilicate-based ceramic crowns. Dent. Mater. 2008, 24, 667–673. [Google Scholar] [CrossRef] [PubMed]
- Krejci, I.; Lutz, F.; Reimer, M.; Heinzmann, J.L. Wear of ceramic inlays, their enamel antagonists, and luting cements. J. Prosthet. Dent. 1993, 69, 425–430. [Google Scholar] [CrossRef] [PubMed]
- Monasky, G.E.; Taylor, D.F. Studies on the wear of porcelain, enamel, and gold. J. Prosthet. Dent. 1971, 25, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.; Swain, M.; He, L.; Lyons, K. Wear behavior of human enamel against lithium disilicate glass ceramic and type III gold. J. Prosthet. Dent. 2014, 112, 1399–1405. [Google Scholar] [CrossRef] [PubMed]
- Zurek, A.D.; Alfaro, M.F.; Wee, A.G.; Yuan, J.C.; Barao, V.A.; Mathew, M.T.; Sukotjo, C. Wear Characteristics and Volume Loss of CAD/CAM Ceramic Materials. J. Prosthodont. 2019, 28, e510–e518. [Google Scholar] [CrossRef] [PubMed]
- Krejci, I.; Lutz, F.; Reimer, M. Wear of CAD/CAM ceramic inlays: Restorations, opposing cusps, and luting cements. Quintessence Int. 1994, 25, 199–207. [Google Scholar] [PubMed]
- Nawafleh, N.A.; Mack, F.; Evans, J.; Mackay, J.; Hatamleh, M.M. Accuracy and reliability of methods to measure marginal adaptation of crowns and FDPs: A literature review. J. Prosthodont. 2013, 22, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Mendřický, R. Determination of measurement accuracy of optical 3D scanners. MM Sci. J. 2016, 2016, 1565–1572. [Google Scholar] [CrossRef]
- Bajoghli, F.; Sabouhi, M.; Nosouhian, S.; Davoudi, A.; Behnamnia, Z. Comparing the Accuracy of Three Different Impression Materials in Making Duplicate Dies. J. Int. Oral Health 2015, 7, 12–16. [Google Scholar] [PubMed]
- Gujjarlapudi, M.C.; Reddy, S.V.; Madineni, P.K.; Ealla, K.K.; Nunna, V.N.; Manne, S.D. Comparative evaluation of few physical properties of epoxy resin, resin-modified gypsum and conventional type IV gypsum die materials: An in vitro study. J. Contemp. Dent. Pract. 2012, 13, 48–54. [Google Scholar] [CrossRef] [PubMed]
- Ahlholm, P.; Sipilä, K.; Vallittu, P.; Jakonen, M.; Kotiranta, U. Digital Versus Conventional Impressions in Fixed Prosthodontics: A Review. J. Prosthodont. 2018, 27, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Pinto, R.J.; Casado, S.A.; Chmielewski, K.; Caramês, J.M.; Marques, D.S. Accuracy of different digital acquisition methods in complete arch implant-supported prostheses: An in vitro study. J. Prosthet. Dent. 2024, 132, 172–177. [Google Scholar] [CrossRef] [PubMed]
| Inclusion Criteria |
|---|
|
| Mean Distance [mm] | |||
|---|---|---|---|
| Material comparison | 2 years | 4 years | 14 years |
| Enamel vs. Composite | 0.27 | 0.421 | 0.743 |
| Enamel vs. Ceramic | 0.216 | 0.767 | 0.333 |
| Enamel vs. Gold | 0.412 | 1.000 | 0.709 |
| Composite vs. Ceramic | 0.955 | 0.777 | 0.777 |
| Composite vs. Gold | 0.858 | 0.421 | 0.411 |
| Ceramic vs. Gold | 0.752 | 0.922 | 0.202 |
| Time point comparison | 2 vs. 4 years | 2 vs. 14 years | 4 vs. 14 years |
| Enamel | <0.001 | <0.001 | 0.001 |
| Composite | 0.004 | 0.004 | 0.004 |
| Ceramic | <0.001 | <0.001 | <0.001 |
| Gold | <0.001 | <0.001 | <0.001 |
| Integrated Distance [mm3] | |||
| Material comparison | 2 years | 4 years | 14 years |
| Enamel vs. Composite | 0.194 | 0.411 | 0.421 |
| Enamel vs. Ceramic | 0.163 | 0.626 | 0.358 |
| Enamel vs. Gold | 0.806 | 0.233 | 0.026 |
| Composite vs. Ceramic | 0.978 | 0.760 | 0.760 |
| Composite vs. Gold | 0.482 | 0.108 | 0.025 |
| Ceramic vs. Gold | 0.304 | 0.140 | 0.030 |
| Time point comparison | 2 vs. 4 years | 2 vs. 14 years | 4 vs. 14 years |
| Enamel | 0.002 | <0.001 | 0.004 |
| Composite | 0.004 | 0.004 | 0.020 |
| Ceramic | <0.001 | <0.001 | 0.005 |
| Gold | <0.001 | <0.001 | 0.003 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matta, R.-E.; Berger, L.; Sednyev, O.; Bäuerle, D.; Maier, E.; Adler, W.; Taschner, M. In Vivo Wear Analysis of Leucite-Reinforced Ceramic Inlays/Onlays After 14 Years. Materials 2025, 18, 3446. https://doi.org/10.3390/ma18153446
Matta R-E, Berger L, Sednyev O, Bäuerle D, Maier E, Adler W, Taschner M. In Vivo Wear Analysis of Leucite-Reinforced Ceramic Inlays/Onlays After 14 Years. Materials. 2025; 18(15):3446. https://doi.org/10.3390/ma18153446
Chicago/Turabian StyleMatta, Ragai-Edward, Lara Berger, Oleksandr Sednyev, Dennis Bäuerle, Eva Maier, Werner Adler, and Michael Taschner. 2025. "In Vivo Wear Analysis of Leucite-Reinforced Ceramic Inlays/Onlays After 14 Years" Materials 18, no. 15: 3446. https://doi.org/10.3390/ma18153446
APA StyleMatta, R.-E., Berger, L., Sednyev, O., Bäuerle, D., Maier, E., Adler, W., & Taschner, M. (2025). In Vivo Wear Analysis of Leucite-Reinforced Ceramic Inlays/Onlays After 14 Years. Materials, 18(15), 3446. https://doi.org/10.3390/ma18153446








