A 3D-Printed Crown Integrated with 3D-Printed Orthodontic Brackets: A Novel One-Unit Printing Technique
Abstract
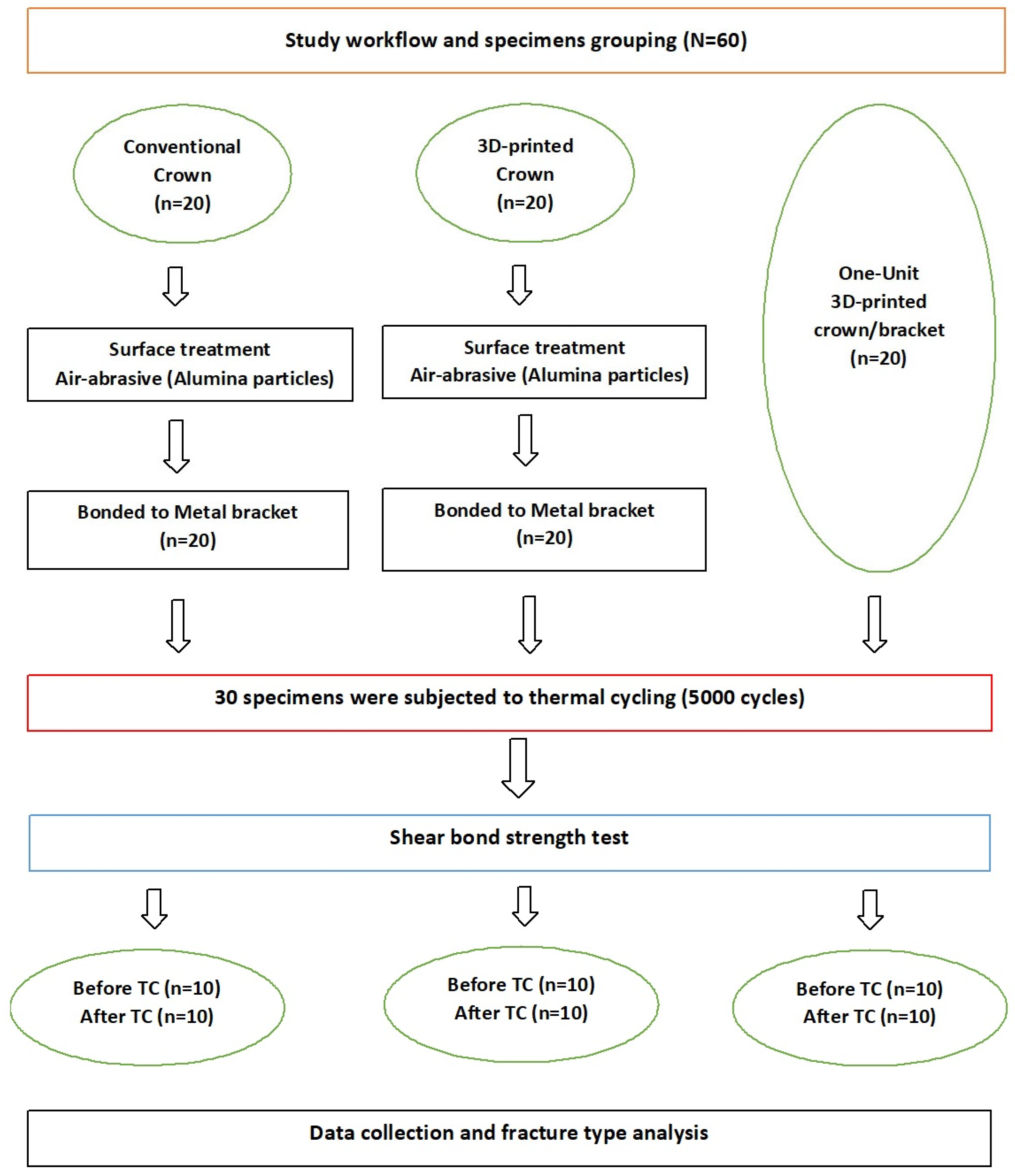
1. Introduction
2. Materials and Methods
2.1. Sample Size and Specimen Grouping
2.2. Conventional Specimen Fabrication
2.3. Three Dimensional-Printed Teeth Fabrication
2.4. Bonding Procedures for the Bonded Groups
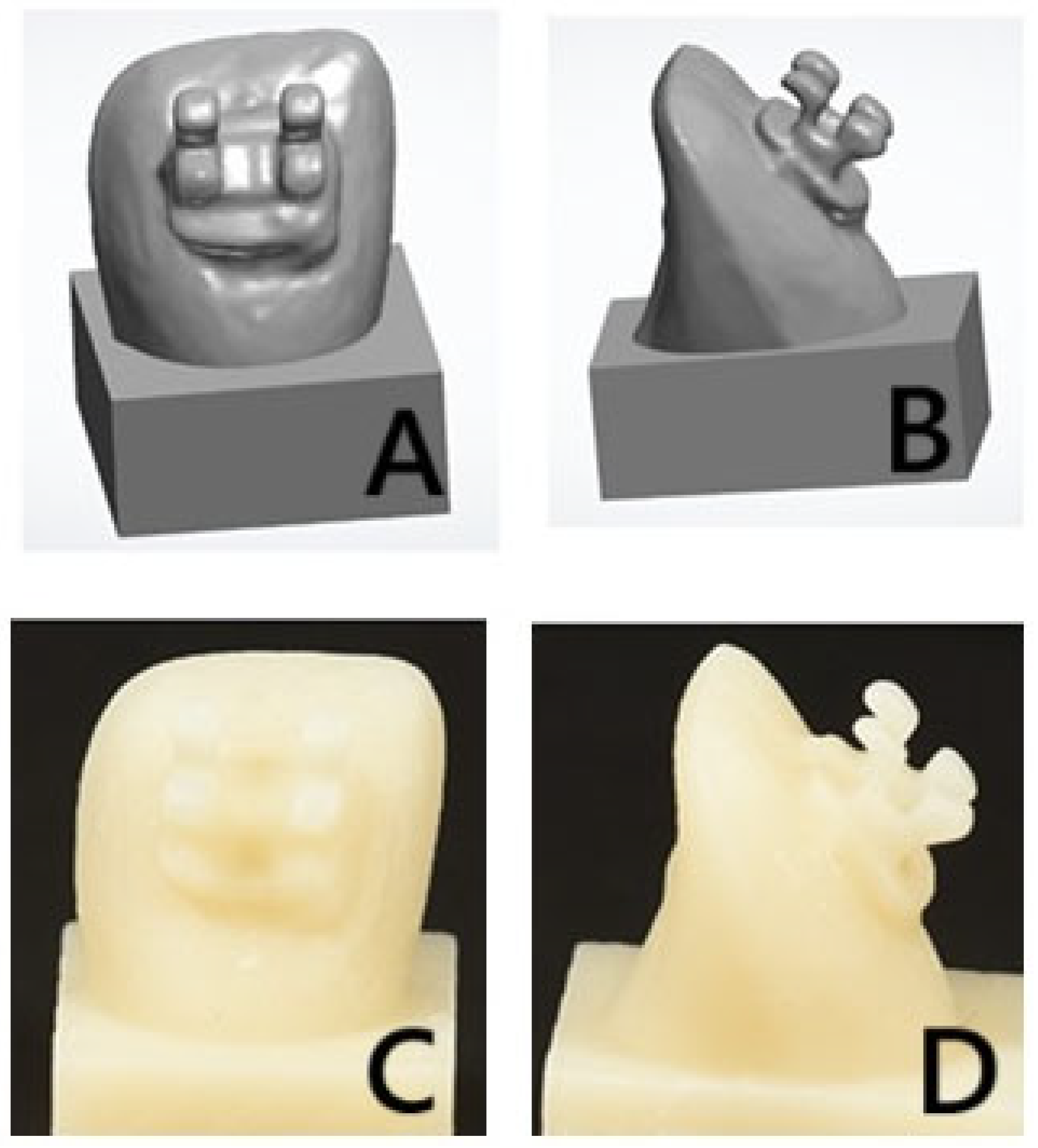
2.5. Three Dimensional-Printed One-Unit Group Preparation
2.6. Specimen Storage and Thermal Aging
2.7. Testing Procedures
2.8. Mode of Failure Analysis
2.9. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Al Jabbari, Y.S.; Al Taweel, S.M.; Al Rifaiy, M.; Alqahtani, M.Q.; Koutsoukis, T.; Zinelis, S. Effects of surface treatment and artificial aging on the shear bond strength of orthodontic brackets bonded to four different provisional restorations. Angle Orthod. 2014, 84, 649–655. [Google Scholar] [CrossRef] [PubMed]
- Goymen, M.; Topcuoglu, T.; Topcuoglu, S.; Akin, H. Effect of different temporary crown materials and surface roughening methods on the shear bond strengths of orthodontic brackets. Photomed. Laser Surg. 2015, 33, 55–60. [Google Scholar] [CrossRef]
- Soon, H.I.; Gill, D.S.; Jones, S.P. A study to investigate the bond strengths of orthodontic brackets bonded to prosthetic acrylic teeth. J. Orthod. 2015, 42, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Blakey, R.; Mah, J. Effects of surface conditioning on the shear bond strength of orthodontic brackets bonded to temporary polycarbonate crowns. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 72–78. [Google Scholar] [CrossRef]
- Rambhia, S.; Heshmati, R.; Dhuru, V.; Iacopino, A. Shear bond strength of orthodontic brackets bonded to provisional crown materials utilizing two different adhesives. Angle Orthod. 2009, 79, 784–789. [Google Scholar] [CrossRef]
- Shillinburg, H.T.; Hobo, S.; Whitsett, L.D.; Jacobi, R.; Brackett, S. Fundamentals of Fixed Prosthodontics, 3rd ed.; Quintessence Books: Chicago, IL, USA, 1997; pp. 225–226. [Google Scholar]
- Reynolds, I. A review of direct orthodontic bonding. Br. J. Orthodont. 1975, 2, 171–178. [Google Scholar] [CrossRef]
- Pinho, M.; Manso, M.; Martin, C.; Souza, J.; Almeida, R.; Ferreira, A. Adhesion strength of orthodontic brackets to acrylic surfaces. A systematic review on in vitro studies. Rev. Port. Estomatol. Med. Dent. Cir. Maxilofac. 2017, 58, 65–70. [Google Scholar] [CrossRef][Green Version]
- Krey, K.F.; Darkazanly, N.; Kühnert, R.; Ruge, S. 3D-printed orthodontic brackets—Proof of concept. Int. J. Comput. Dent. 2016, 19, 351–362. [Google Scholar]
- Panayi, N.C. In-house three-dimensional designing and printing customized brackets. J. World Fed. Orthod. 2022, 11, 190–196. [Google Scholar] [CrossRef]
- Polychronis, G.; Papageorgiou, S.N.; Riollo, C.S.; Panayi, N.; Zinelis, S.; Eliades, T. Fracture toughness and hardness of in-office, 3D-printed ceramic brackets. Orthod. Craniofac. Res. 2023, 26, 476–480. [Google Scholar] [CrossRef]
- Hanson, M.S.; Ontiveros, J.C.; English, J.D.; Wirthlin, J.O.; Cozad, B.E.; Harrington, D.A.; Kasper, F.K. Effect of Material and Pad Abrasion on Shear Bond Strength of 3D-Printed Orthodontic Brackets. Orthod. Craniofac. Res. 2023, 26 (Suppl. S1), 171–179. [Google Scholar] [CrossRef] [PubMed]
- Haynie, A.S.; English, J.D.; Paravina, R.D.; Moon, A.; Hanigan, J.; Abu Al Tamn, M.A.; Kasper, F.K. Colour stability of 3D-printed resin orthodontic brackets. J. Orthod. 2021, 48, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Urichianu, M.; Makowka, S.; Covell, D., Jr.; Warunek, S.; Al-Jewair, T. Shear Bond Strength and Bracket Base Morphology of New and Rebonded Orthodontic Ceramic Brackets. Materials 2022, 15, 1865. [Google Scholar] [CrossRef] [PubMed]
- Hodecker, L.D.; Scheurer, M.; Scharf, S.; Roser, C.J.; Fouda, A.M.; Bourauel, C.; Lux, C.J.; Bauer, C.A.J. Influence of Individual Bracket Base Design on the Shear Bond Strength of In-Office 3D Printed Brackets-An In Vitro Study. J. Funct. Biomater. 2023, 14, 289. [Google Scholar] [CrossRef]
- Papageorgiou, S.N.; Polychronis, G.; Panayi, N.; Zinelis, S.; Eliades, T. New aesthetic in-house 3D-printed brackets: Proof of concept and fundamental mechanical properties. Prog. Orthod. 2022, 23, 6. [Google Scholar] [CrossRef]
- Hodecker, L.; Bourauel, C.; Braumann, B.; Kruse, T.; Christ, H.; Scharf, S. Comparative in vitro analysis of the sliding resistance of a modern 3D-printed polymer bracket in combination with different archwire types. Clin. Oral. Investig. 2022, 26, 4049–4057. [Google Scholar] [CrossRef]
- Eliades, T.; Zinelis, S. Three dimensional printing and inhouse appliance fabrication: Between innovation and stepping into the unknown. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 1–3. [Google Scholar] [CrossRef]
- Bauer, C.A.J.; Scheurer, M.; Bourauel, C.; Kretzer, J.P.; Roser, C.J.; Lux, C.J.; Hodecker, L.D. Precision of slot widths and torque transmission of in-office 3D printed brackets: An in vitro study. J. Orofac. Orthop. 2024, 85, 327–339. [Google Scholar] [CrossRef]
- Möller, M.; Klocke, A.; Sadat-Khonsari, R.; Schlegel, V.; Kahl-Nieke, B. Torque stability of plastic brackets following multiple loading and artificial material aging—An in-vitro comparison. J. Orofac. Orthop. 2009, 70, 385–395. [Google Scholar] [CrossRef]
- Hiroce, M.; Fernandes, D.J.; Elias, C.N.; Miguel, J.A.M. Sliding resistance of polycarbonate self-ligating brackets and stainless steel esthetic archwires. Prog. Orthod. 2012, 13, 148–153. [Google Scholar] [CrossRef]
- Gkantidisa, N.; Zinelisb, S.; Karamolegkouc, M.; Eliades, T.; Topouzelis, N. Comparative assessment of clinical performance of esthetic bracket materials. Angle Orthod. 2012, 82, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Hodecker, L.; Bourauel, C.; Braumann, B.; Kruse, T.; Christ, H.; Scharf, S. Sliding behaviour and surface quality after static air polishing of conventional and modern bracket materials: In vitro analysis. J. Orofac. Orthop. 2021, 84, 110–124. [Google Scholar] [CrossRef] [PubMed]
- Nakano, T.; Nakajima, A.; Watanabe, H.; Osada, A.; Namura, Y.; Yoneyama, T.; Tanaka, E.; Motoyoshi, M. Evaluation of torque moment in esthetic brackets from bendable alloy wires. Angle Orthod. 2021, 91, 656–663. [Google Scholar] [CrossRef]
- Feldner, J.C.; Sarkar, N.K.; Sheridan, J.J.; Lancaster, D.M. In vitro torque-deformation characteristics of orthodontic polycarbonate brackets. Am. J. Orthod. Dentofac. Orthop. 1994, 106, 265–272. [Google Scholar] [CrossRef]
- Çokakoğlu, S.; Karaokutan, I.; Buyuk, S.K. Effects of orientation and postprocessing on the bonding of 3-dimensional printed brackets to printable permanent crown resin. Am. J. Orthod. Dentofac. Orthop. 2025, 167, 362–370. [Google Scholar] [CrossRef]
- Alsaud, B.A.; Hajjaj, M.S.; Masoud, A.I.; Abou Neel, E.A.; Abuelenain, D.A.; Linjawi, A. Bonding of Clear Aligner Composite Attachments to Ceramic Materials: An In Vitro Study. Materials 2022, 15, 4145. [Google Scholar] [CrossRef] [PubMed]
- Arslan, S.; Kilinc, H. Evaluation of the effects of different composite materials and surface roughening techniques in bonding attachments of clear aligner on monolithic zirconia. Orthod. Craniofac. Res. 2023, 26, 546–551. [Google Scholar] [CrossRef]
- Fausto da Veiga Jardim, A.; Curado de Freitas, J.; Estrela, C. Surface wear and adhesive failure of resin attachments used in clear aligner orthodontic treatment. J. Orofac. Orthop. 2023, 85, 52–62. [Google Scholar] [CrossRef]
- Shahin, S.Y.; Abu Showmi, T.H.; Alzaghran, S.H.; Albaqawi, H.; Alrashoudi, L.; Gad, M.M. Bond strength of orthodontic brackets to temporary crowns: In vitro effects of surface treatment. Int. J. Dent. 2021, 2021, 9999933. [Google Scholar] [CrossRef]
- Kedia, N.B.; Bangar, B.; Rao, S.J.; Swarup, S.; Singh, D.; Chikhalia, D.K. Bond Strength of Orthodontic Brackets to Temporary Crowns: In vitro Effects of Surface Treatment. J. Pharm. Bioallied. Sci. 2023, 15 (Suppl. S2), S1013–S1015. [Google Scholar] [CrossRef]
- Carreira, M.; Antunes, P.V.; Ramalho, A.; Paula, A.B.; Carrilho, E. Thermocycling effect on mechanical and tribological characterization of two indirect dental restorative materials. J. Braz. Soc. Mech. Sci. Eng. 2017, 39, 1–17. [Google Scholar] [CrossRef]
- Borzangy, S. Impact of surface treatment methods on bond strength of orthodontic brackets to indirect composite provisional restorations. J. Cont. Dent. Pract. 2019, 20, 1412–1416. [Google Scholar] [CrossRef]
- Goracci, C.; Juloski, J.; D’Amico, C.; Balestra, D.; Volpe, A.; Juloski, J.; Vichi, A. Clinically Relevant Properties of 3D Printable Materials for Intraoral Use in Orthodontics: A Critical Review of the Literature. Materials 2023, 16, 2166. [Google Scholar] [CrossRef]
- Shannon, T.; Groth, C. Be your own manufacturer: 3D printing intraoral appliances. Semin. Orthod. 2021, 27, 184–188. [Google Scholar] [CrossRef]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Efficacy of clear aligners in controlling orthodontic tooth movement: A systematic review. Angle Orthod. 2015, 85, 881–889. [Google Scholar] [CrossRef]
- Chen, W.; Qian, L.; Qian, Y.; Zhang, Z.; Wen, X. Comparative study of three composite materials in bonding attachments for clear aligners. Orthod. Craniofac. Res. 2021, 24, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Tamer, I.; Oztas, E.; Marsan, G. Orthodontic treatment with clear aligners and the scientific reality behind their marketing: A literature review. Turk. J. Orthod. 2019, 32, 241–246. [Google Scholar] [CrossRef]
- Alajmi, S.; Shaban, A.; Al-Azemi, R. Comparison of Short-Term Oral Impacts Experienced by Patients Treated with Invisalign or Conventional Fixed Orthodontic Appliances. Med. Princ. Pract. 2020, 29, 382–388. [Google Scholar] [CrossRef]
- Shin, S.H.; Lee, K.J.; Kim, S.J.; Yu, H.S.; Kim, K.M.; Hwang, C.J.; Cha, J.Y. Accuracy of bracket position using thermoplastic and 3D-printed indirect bonding trays. Int. J. Comput. Dent. 2021, 24, 133–145. [Google Scholar]
- Fotovat, F.; Shishehian, A.; Alijani, S.; Alafchi, B.; Parchami, P. Comparison of shear bond strength of orthodontic stainless-steel brackets on temporary crowns fabricated by three different methods: An in vitro study. Int. Orthod. 2022, 20, 100641. [Google Scholar] [CrossRef]
- Harikrishnan, S.; Subramanian, A.K. 3D printing in orthodontics: A narrative review. J. Int. Oral Health 2023, 15, 15–27. [Google Scholar]
- Cao, J.; Liu, X.; Cameron, A.; Aarts, J.; Choi, J.J.E. Influence of different post-processing methods on the dimensional accuracy of 3D-printed photopolymers for dental crown applications—A systematic review. J. Mech. Behav. Biomed. Mater. 2024, 150, 106314. [Google Scholar] [CrossRef] [PubMed]
- Farag, E.; Sabet, A.; Ebeid, K.; El Sergany, O. Build angle effect on 3D-printed dental crowns marginal fit using digital lightpr cessing and stereo-lithography technology: An in vitro study. BMC Oral Health 2024, 24, 73. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M. Factors affecting flexural strength of 3D-printed resins: A systematic review. J. Prosthodont. 2023, 32, 96–110. [Google Scholar] [CrossRef]
- de Castro, E.F.; Nima, G.; Rueggeberg, F.A.; Giannini, M. Effect of build orientation in accuracy, flexural modulus, flexural strength, and microhardness of 3D-Printed resins for provisional restorations. J. Mech. Behav. Biomed. Mater. 2022, 136, 105479. [Google Scholar] [CrossRef]
- AlGhamdi, M.A.; Gad, M.M. Impact of Printing Orientation on the Accuracy of Additively Fabricated Denture Base Materials: A Systematic Review. Dent. J. 2024, 12, 230. [Google Scholar] [CrossRef]
- Scherer, M.; Al-Haj Husain, N.; Barmak, A.B.; Kois, J.C.; Özcan, M.; Revilla-León, M. Influence of the layer thickness on the flexural strength of aged and nonaged additively manufactured interim dental material. J. Prosthodont. 2023, 32, 68–73. [Google Scholar] [CrossRef]
- Topsakal, K.G.; Gökmen, S.; Yurdakurban, E.; Duran, G.S.; Gorgoulu, S. The effect of layer thickness on the accuracy of the different in-house clear aligner attachments. Clin. Oral. Investig. 2023, 27, 5331–5341. [Google Scholar] [CrossRef] [PubMed]
- ElShebiny, T.; Matthaios, S.; Menezes, L.M.; Tsolakis, I.A.; Palomo, J.M. Effect of printing technology, layer height, and orientation on assessment of 3D-printed models. J. World Fed. Orthod. 2024, 13, 169–174. [Google Scholar] [CrossRef]
- Soto-Montero, J.; de Castro, E.F.; Romano, B.C.; Nima, G.; Shimokawa, C.A.K.; Giannini, M. Color alterations, flexural strength, and microhardness of 3D printed resins for fixed provisional restoration using different post-curing times. Dent. Mater. 2022, 38, 1271–1282. [Google Scholar] [CrossRef]
- Dizon, J.R.C.; Gache, C.C.L.; Cascolan, H.M.S.; Cancino, L.T.; Advincula, R.C. Post-processing of 3D-printed polymers. Technologies 2021, 9, 61. [Google Scholar] [CrossRef]
- Rueggeberg, F.A.; Margeson, D.H. The effect of oxygen inhibitionon an unfilled/filled composite system. J. Dent. Res. 1990, 69, 1652–1658. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.H.; Lee, S.Y.; Gu, H.; Jin, G.; Kim, J.E. Evaluating oxygen shielding effect using glycerin or vacuum with varying temperature on 3D printed photopolymer in post-polymerization. J. Mech. Behav. Biomed. Mater. 2022, 130, 105170. [Google Scholar] [CrossRef] [PubMed]
- Mandurino, M.; Cortili, S.; Coccoluto, L.; Greco, K.; Cantatore, G.; Gherlone, E.F.; Vichi, A.; Paolone, G. Mechanical Properties of 3D Printed vs. Subtractively Manufactured Composite Resins for Permanent Restorations: A Systematic Review. Materials 2025, 18, 985. [Google Scholar] [CrossRef]
- Kulkarni, N.B.; Goyal, S.M.; Shah, V.D. 3D Printing Pen: A Novel Adjunct for Indirect Bonding. J. Contemp. Dent. Pract. 2021, 22, 964–968. [Google Scholar]
| CCMBB | 3DPCMBB | 3DPCB-One-Unit | ||
|---|---|---|---|---|
| Thermal stress | Conventional crown and metal-bonded bracket Mean ± SD | 3D-printed crown and metal-bonded bracket Mean ± SD | 3D-printed crown and bracket (one-unit) Mean ± SD | p |
| Before | 5.67 ± 1.02 a | 5.07 ± 0.092 a | 10.14 ± 1.93 | p < 0.001 * |
| After | 3.86 ± 0.99 a | 3.66 ± 1.03 a | 8.67 ± 1.53 | p < 0.001 * |
| p | 0.009 * | 0.013 * | 0.041 * |
| Mode of Failure | Conventional Crown and Bonded Bracket | 3D-Printed Crown and Bonded Bracket | 3D-Printed Crown and Brackets (One-Unit) | |
|---|---|---|---|---|
| No TC | Adhesive (Score 0) | 7 | 8 | All fractures in printed brackets |
| Cohesive (Score 1) | - | - | ||
| Mixed (Score 2) | 3 | 2 | ||
| (Score 3) | ||||
| After TC | Adhesive (Score 0) | 9 | 10 | |
| Cohesive (Score 1) | - | - | ||
| Mixed (Score 2) | 1 | - | ||
| (Score 3) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shahin, S.Y.; Nassar, E.A.; Gad, M.M. A 3D-Printed Crown Integrated with 3D-Printed Orthodontic Brackets: A Novel One-Unit Printing Technique. Materials 2025, 18, 2727. https://doi.org/10.3390/ma18122727
Shahin SY, Nassar EA, Gad MM. A 3D-Printed Crown Integrated with 3D-Printed Orthodontic Brackets: A Novel One-Unit Printing Technique. Materials. 2025; 18(12):2727. https://doi.org/10.3390/ma18122727
Chicago/Turabian StyleShahin, Suliman Y., Essam A. Nassar, and Mohammed M. Gad. 2025. "A 3D-Printed Crown Integrated with 3D-Printed Orthodontic Brackets: A Novel One-Unit Printing Technique" Materials 18, no. 12: 2727. https://doi.org/10.3390/ma18122727
APA StyleShahin, S. Y., Nassar, E. A., & Gad, M. M. (2025). A 3D-Printed Crown Integrated with 3D-Printed Orthodontic Brackets: A Novel One-Unit Printing Technique. Materials, 18(12), 2727. https://doi.org/10.3390/ma18122727









