Stress Behaviour of an Immature Maxillary Central Incisor: A 3D Finite Element Analysis
Abstract
1. Introduction
2. Materials and Methods
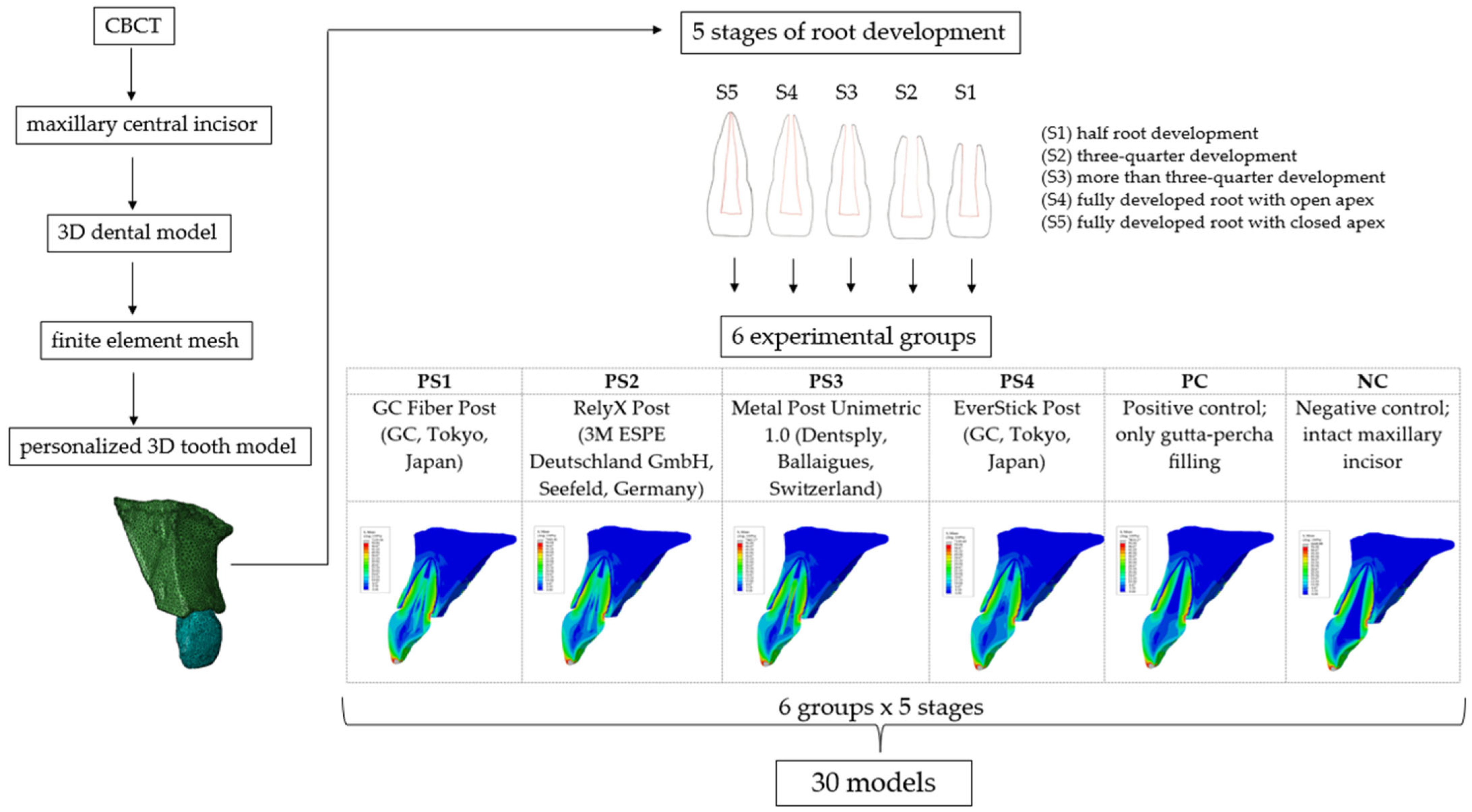
2.1. Study Design
2.2. Model Generation
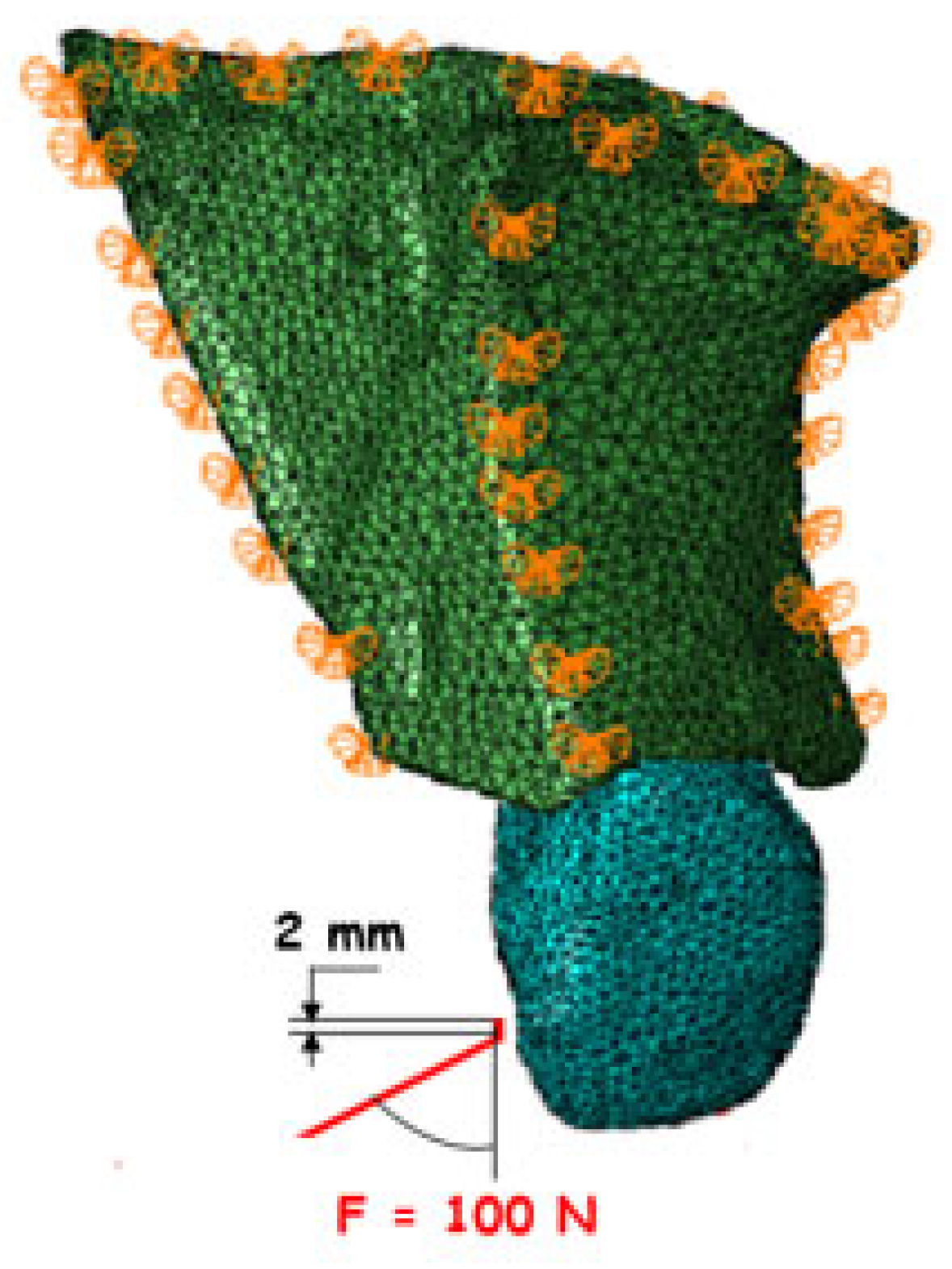
2.3. Loading and Boundary Conditions
2.4. Statistical Analysis
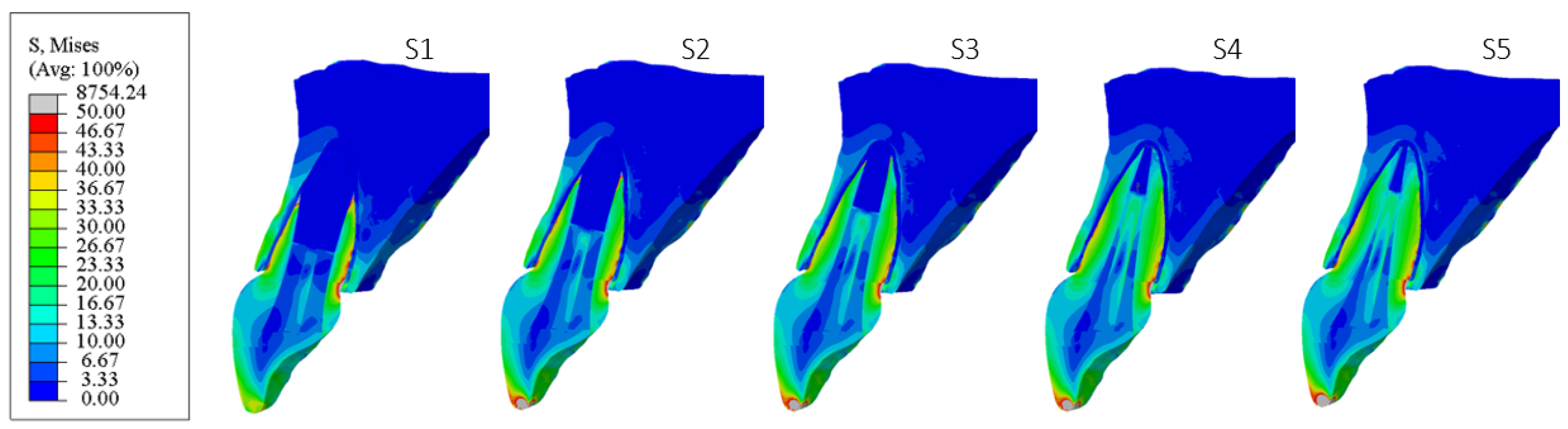
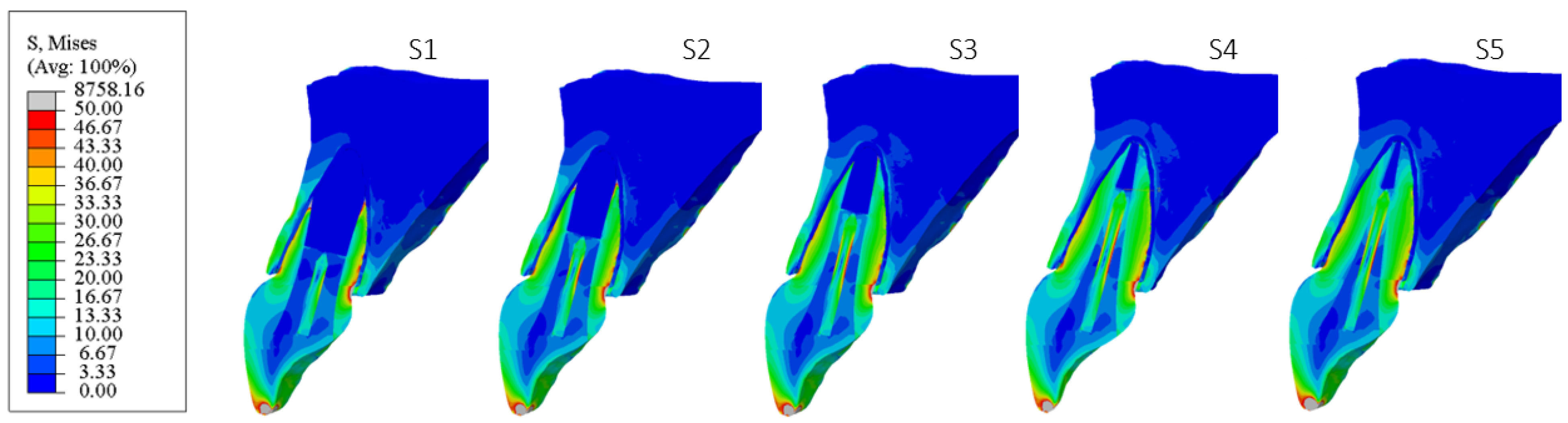
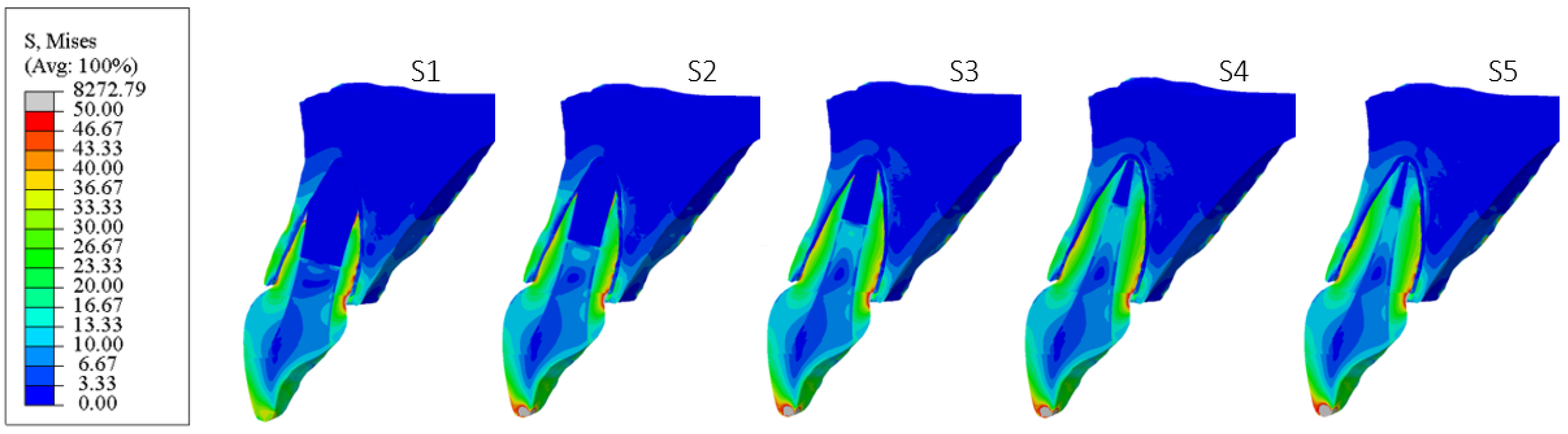
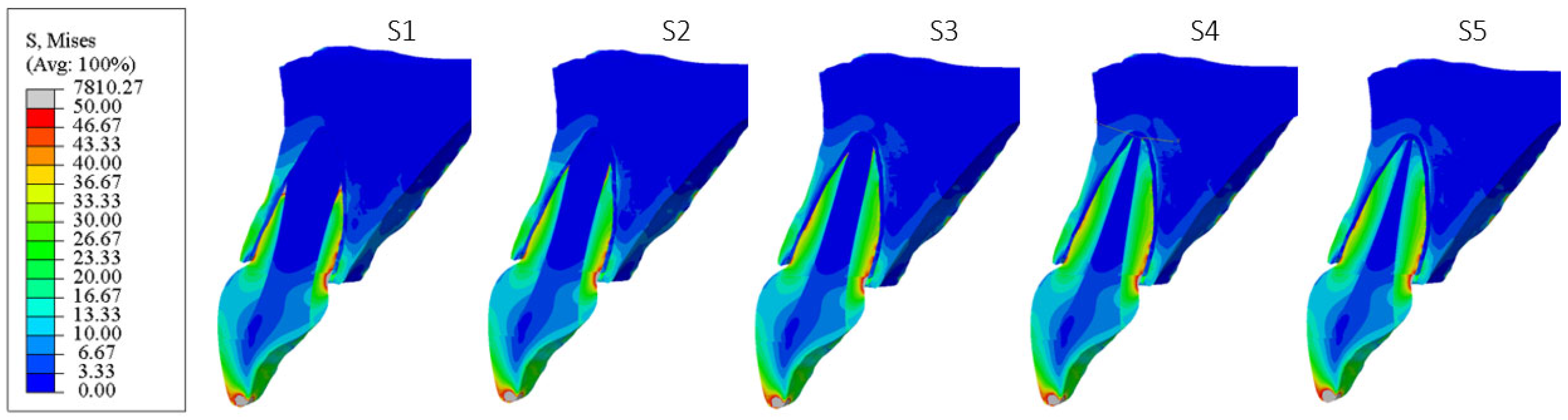
3. Results
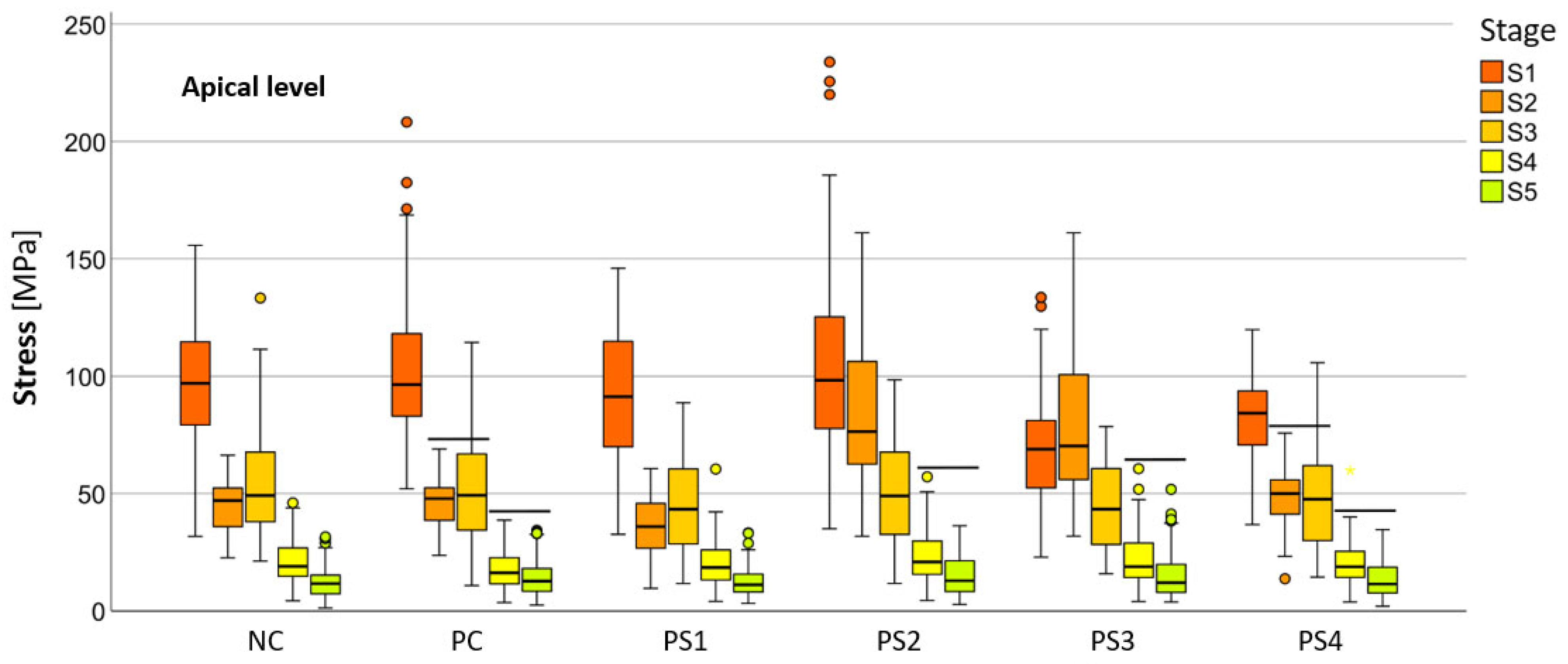
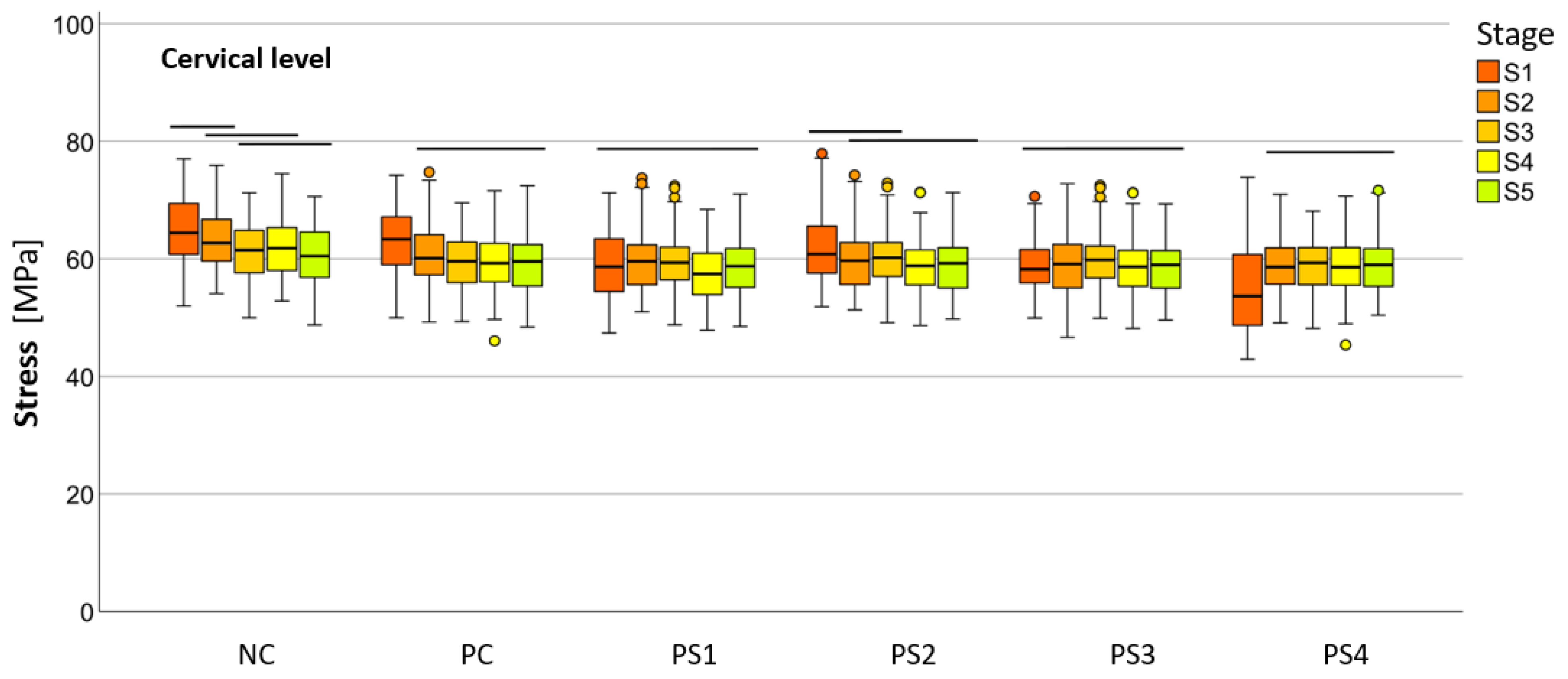
Descriptive Statistics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ANOVA | Analysis of variance |
| CBCT | Cone beam computed tomography |
| FEA | Finite element analysis |
| FEM | Finite element method |
| FRC | Fiber-reinforced composite |
| GFP | Glass fiber post |
| HMN | Hencky–von Mises |
| IMI | Immature maxillary incisor |
| NC | Negative control group—intact maxillary incisor |
| PC | Positive control group with only the gutta-percha filling |
| PS1 | Post system with GC Fiber Post |
| PS2 | Post system with RelyX Post |
| PS3 | Post system with metal post Unimetric |
| PS4 | Post system with GC everStick Post |
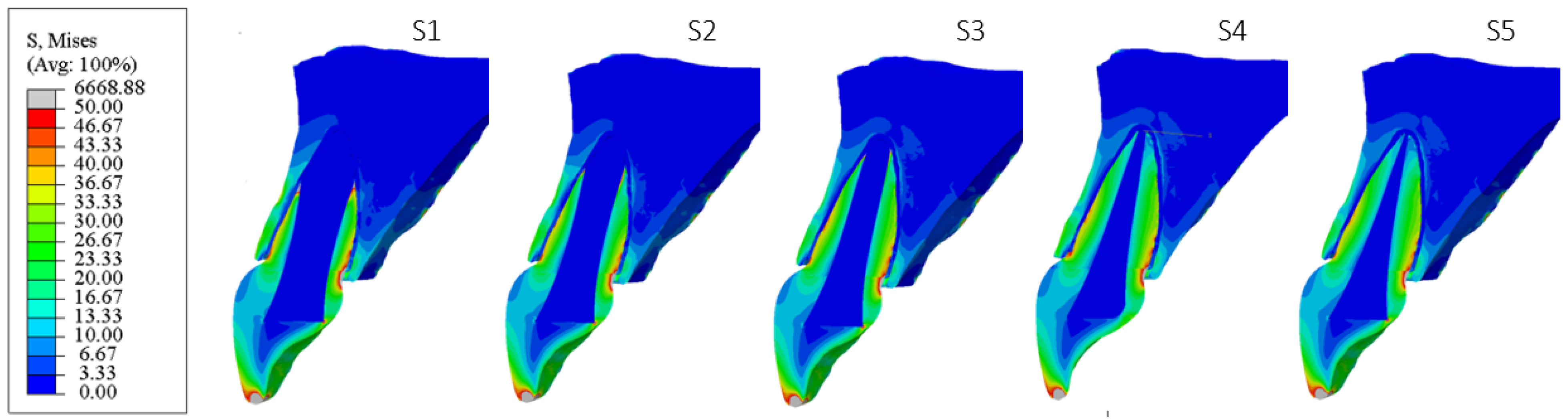
| S1 | Stage with half of the root development |
| S2 | Stage with three quarters of root development |
| S3 | Stage with more than three quarters of root development |
| S4 | Stage with fully developed root with open apex |
| S5 | Stage with fully developed root with closed apex |
References
- Mayya, A.; Bhandary, S.; Kolakemar, A.; George, A.M. Management of necrotic immature permanent maxillary incisors using a modified technique of revascularisation. BMJ Case Rep. 2021, 17, e240203. [Google Scholar] [CrossRef] [PubMed]
- Jadhav, K.; Vaidya, M.J.; Hegde, V.; Kawle, S. Management of non-vital immature teeth: A review. IOSR J. Dent. Med. Sci. 2021, 20, 35–40. [Google Scholar] [CrossRef]
- Cadenaro, M.; Josic, U.; Maravić, T.; Mazzitelli, C.; Marchesi, G.; Mancuso, E.; Breschi, L.; Mazzoni, A. Progress in dental adhesive materials. J. Dent. Res. 2023, 102, 254–262. [Google Scholar] [CrossRef] [PubMed]
- Mannocci, F.; Bitter, K.; Sauro, S.; Ferrari, P.; Austin, R.; Bhuva, B. Present status and future directions: The restoration of root filled teeth. Int. Endod. J. 2022, 55, 1059–1084. [Google Scholar] [CrossRef]
- de Andrade, G.; Saavedra, G.; Augusto, M.; Alfonzo, G.; Brandão, H.; Tribst, J.; Dal Piva, A. Post-endodontic restorative treatments and their mechanical behavior: A narrative review. Dent. Rev. 2023, 3, 100067. [Google Scholar] [CrossRef]
- Yang, A.; Lamichhane, A.; Xu, C. Remaining coronal dentin and risk of fiber-reinforced composite post-core restoration failure: A meta-analysis. Int. J. Prosthodont. 2015, 28, 258–264. [Google Scholar] [CrossRef]
- Alshabib, A.; Althaqafi, K.A.; AlMoharib, H.S.; Mirah, M.; AlFawaz, Y.F.; Algamaiah, H. Dental fiber-post systems: An in-depth review of their evolution, current practice, and future directions. Bioengineering 2023, 10, 551. [Google Scholar] [CrossRef]
- Suni, A.O.; Lassila, L.V.J.; Tuokko, J.K.; Garoushi, S.; Vallittu, P.K. Adhesion of individually formed fiber post adhesively luted with flowable short fiber composite. Biomater. Investig. Dent. 2023, 10, 2209593. [Google Scholar] [CrossRef]
- Dikbas, I.; Tanalp, J. An overview of clinical studies on fiber post systems. Sci. World J. 2013, 2013, 171380. [Google Scholar] [CrossRef]
- Parčina, I.; Baraba, A. Esthetic intracanal posts. Acta Stomatol. Croat. 2016, 50, 143–150. [Google Scholar] [CrossRef]
- de Morais, D.C.; Butler, S.; Santos, M.J.M.C. Current insights on fiber posts: A narrative review of laboratory and clinical studies. Dent. J. 2023, 11, 236. [Google Scholar] [CrossRef] [PubMed]
- Bonchev, A.; Radeva, E.; Tsvetanova, N. Fiber reinforced composite posts-A review of literature. Int. J. Sci. Res. 2017, 6, 1887–1893. [Google Scholar] [CrossRef]
- Amizic, I.P.; Baraba, A.; Ionescu, A.C.; Brambilla, E.; Van Ende, A.; Miletic, I. Bond strength of individually formed and prefabricated fiber-reinforced composite posts. J. Adhes. Dent. 2019, 21, 557–565. [Google Scholar] [CrossRef]
- de Carvalho, M.A.; Lazari, P.C.; Gresnigt, M.; Del Bel Cury, A.A.; Magne, P. Current options concerning the endodontically-treated teeth restoration with the adhesive approach. Braz. Oral. Res. 2018, 32, e74. [Google Scholar] [CrossRef]
- Nair, K.R.; Geetha, P.; Veedu, R.; George, E.; Joseph, M. Management of an oblique crown fracture of an anterior tooth with a missed coronal segment: A case report. Conserv. Dent. Endod. J. 2019, 4, 21–24. [Google Scholar] [CrossRef]
- Cvek, M. Prognosis of luxated non-vital maxillary incisors treated with calcium hydroxide and filled with gutta-percha. A retrospective clinical study. Endod. Dent. Traumatol. 1992, 8, 45–55. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Farik, B.; Munksgaard, E.C. Long-term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dent. Traumatol. 2002, 18, 134–137. [Google Scholar] [CrossRef]
- Al-Jundi, S.H. Type of treatment, prognosis, and estimation of time spent to manage dental trauma in late presentation cases at a dental teaching hospital: A longitudinal and retrospective study. Dent. Traumatol. 2004, 20, 1–5. [Google Scholar] [CrossRef]
- Rodd, H.; Noble, F. Psychosocial impacts relating to dental injuries in childhood: The bigger picture. Dent. J. 2019, 7, 23. [Google Scholar] [CrossRef]
- Shivakumar, S.; Kudagi, V.S.; Talwade, P. Applications of finite element analysis in dentistry: A review. J. Int. Oral. Health 2021, 13, 415–422. [Google Scholar] [CrossRef]
- Trivedi, S. Finite element analysis: A boon to dentistry. J. Oral Biol. Craniofacial Res. 2014, 4, 200–203. [Google Scholar] [CrossRef] [PubMed]
- Soares, C.J.; Rodrigues, M.P.; Faria-E-Silva, A.L.; Santos-Filho, P.C.F.; Veríssimo, C.; Kim, H.C.; Versluis, A. How biomechanics can affect the endodontic treated teeth and their restorative procedures? Braz. Oral. Res. 2018, 32, e76. [Google Scholar] [CrossRef] [PubMed]
- Hassouneh, L.; Matoug-Elwerfelli, M.; Al-Omari, T.; Setzer, F.C.; Nagendrababu, V. Assessment of biomechanical behavior of immature non-vital incisors with various treatment modalities by means of three-dimensional quasi–static finite element analysis. Sci. Rep. 2023, 13, 17491. [Google Scholar] [CrossRef]
- Santos Filho, P.C.F.; Soares, P.V.; Reis, B.R.; Veríssimo, C.; Soares, C.J. Effects of threaded post placement on strain and stress distribution of endodontically treated teeth. Braz. Oral. Res. 2013, 27, 305–310. [Google Scholar] [CrossRef]
- Ferrari, M.; Sorrentino, R.; Zarone, F.; Apicella, D.; Aversa, R.; Apicella, A. Non-linear viscoelastic finite element analysis of the effect of the length of glass fiber posts on the biomechanical behaviour of directly restored incisors and surrounding alveolar bone. Dent. Mater. J. 2008, 27, 485–498. [Google Scholar] [CrossRef][Green Version]
- Eram, A.; Zuber, M.; Keni, L.G.; Kalburgi, S.; Naik, R.; Bhandary, S.; Amin, S.; Badruddin, I.A. Finite element analysis of immature teeth filled with MTA, Biodentine and Bioaggregate. Comput. Methods Programs Biomed. 2020, 190, 105356. [Google Scholar] [CrossRef]
- Nokar, S.; Bahrami, M.; Mostafavi, A.S. Comparative evaluation of the effect of different post and core materials on stress distribution in radicular dentin by three-dimensional finite element analysis. J. Dent. 2018, 15, 69–78. [Google Scholar] [PubMed Central]
- Okamoto, K.; Ino, T.; Iwase, N.; Shimizu, E.; Suzuki, M.; Satoh, G.; Ohkawa, S.; Fujisawa, M. Three-dimensional finite element analysis of stress distribution in composite resin cores with fiber posts of varying diameters. Dent. Mater. J. 2008, 27, 49–55. [Google Scholar] [CrossRef]
- Gurbuz, T.; Sengul, F.; Altun, C. Finite element stress analysis of short-post core and over restorations prepared with different restorative materials. Dent. Mater. J. 2008, 27, 499–507. [Google Scholar] [CrossRef]
- Kumar, P.; Rao, R.N. Three-dimensional finite element analysis of stress distribution in a tooth restored with metal and fiber posts of varying diameters: An in-vitro study. J. Conserv. Dent. 2015, 18, 100–104. [Google Scholar] [CrossRef]
- Jain, P.; Lakshmi, S.; Vigneshwaran, S. Endodontically treated teeth with custom cast post and core and metal ceramic crowns restoration: A case report. Int. J. Appl. Dent. Sci. 2021, 7, 16–19. [Google Scholar] [CrossRef]
- Madfa, A.A.; Al-Hamzi, M.A.; Al-Sanabani, F.A.; Al-Qudaimi, N.H.; Yue, X.G. 3D FEA of cemented glass fiber and cast posts with various dental cements in a maxillary central incisor. Springerplus 2015, 4, 598. [Google Scholar] [CrossRef] [PubMed]
- Oskui, I.Z.; Hashemi, A.; Jafarzadeh, H.; Kato, A. Finite element investigation of human maxillary incisor under traumatic loading: Static vs dynamic analysis. Comput. Methods Programs Biomed. 2018, 155, 121–125. [Google Scholar] [CrossRef] [PubMed]
- Jayasudha, K.; Hemanth, M.; Baswa, R.; Raghuveer, H.P.; Vedavathi, B.; Hegde, C. Traumatic impact loading on human maxillary incisor: A Dynamic finite element analysis. J. Indian Soc. Pedod. Prev. Dent. 2015, 33, 302–306. [Google Scholar] [CrossRef]
- Ruse, N.D. Propagation of erroneous data for the modulus of elasticity of periodontal ligament and gutta percha in FEM/FEA papers: A story of broken links. Dent. Mater. 2008, 24, 1717–1719. [Google Scholar] [CrossRef]
- Ausiello, P.; Dal Piva, A.; Borges, A.; Lanzotti, A.; Zamparini, F.; Epifania, E.; Tribst, J.P.M. Effect of shrinking and no shrinking dentine and enamel replacing materials in posterior restoration: A 3D-FEA study. Appl. Sci. 2021, 11, 11052215. [Google Scholar] [CrossRef]
- Matuda, A.G.N.; Silveira, M.P.M.; de Andrade, G.S.; Piva, A.M.O.D.; Tribst, J.P.M.; Borges, A.L.S.; Testarelli, L.; Mosca, G.; Ausiello, P. Computer aided design modelling and finite element analysis of premolar proximal cavities restored with resin composites. Materials 2021, 14, 2366. [Google Scholar] [CrossRef]
- Richert, R.; Robinson, P.; Viguie, G.; Farges, J.C.; Ducret, M. Multi-fiber-reinforced composites for the coronoradicular reconstruction of premolar teeth: A finite element analysis. BioMed Res. Int. 2018, 2018, 4302607. [Google Scholar] [CrossRef]
- Kedia, S.; Narayana, I.; Shetty, R.V.; Shukla, E.; Kalasaiah, D. Stress distribution in teeth restored with different posts using single or multi-post technique: A three-dimensional finite element analysis. Cons. Dent. Endod. J. 2022, 7, 1–6. [Google Scholar] [CrossRef]
- Aggarwal, S.; Garg, V. Finite element analysis of stress concentration in three popular brands of fiber posts systems used for maxillary central incisor teeth. J. Conserv. Dent. 2011, 14, 293–296. [Google Scholar] [CrossRef]
- Diana, H.H.; Oliveira, J.S.; Ferro, M.C.L.; Silva-Sousa, Y.T.C.; Gomes, É.A. Stress distribution in roots restored with fiber posts and an experimental dentin post: 3D-FEA. Braz. Dent. J. 2016, 27, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Bučević Sojčić, P.; Leder Horina, J.; Jurčević Lulić, T.; Bočkaj, N.; Jurić, H. Measurement of the dentin wall thickness of the maxillary central incisor in relation to the stage of root development: A pilot study. Acta Stomatol. Croat. 2023, 57, 206–215. [Google Scholar] [CrossRef] [PubMed]
- 3M RelyX Fiber Post 3D Glass Fiber Post: Technical Data Sheet. Available online: https://multimedia.3m.com/mws/media/1146520O/3m-relyx-fiber-post-3d-glass-fiber-post-technical-data-sheet.pdf (accessed on 28 February 2024).
- GC Fiber Post—IFU. Available online: https://www.gc.dental/america/sites/america.gc.dental/files/products/downloads/gcfiberpost/ifu/gc-fiber-post-ifu.pdf (accessed on 28 February 2024).
- Dentsply Maillefer Product Catalogue. Available online: https://domdent.hu/wp-content/uploads/2023/10/DENTSPLY_MAILLEFER_2014_Product_Catalogue_Single_Page_HR_0714_EN.pdf (accessed on 28 February 2024).
- Agrawal, R.; Narang, S.; Ahmed, H.; Prasad, S.; Reddy, S.; Aila, S. Influence of occlusal bite forces on teeth with altered periodontal support: A three-dimensional finite element stress analysis. J. Pharm. Bioallied Sci. 2021, 13, S688–S691. [Google Scholar] [CrossRef] [PubMed]
- Nikam, D.; Milani, A.S. Physiological response of a natural central incisor tooth to various loading conditions: A 3D finite element study. Recent Prog. Mater. 2023, 5, 017. [Google Scholar] [CrossRef]
- Dorado, S.; Arias, A.; Jimenez-Octavio, J.R. Biomechanical modelling for tooth survival studies: Mechanical properties, loads and boundary conditions—A narrative review. Materials 2022, 15, 7852. [Google Scholar] [CrossRef]
- Verri, F.R.; Okumura, M.H.T.; Lemos, C.A.A.; Almeida, D.A.F.; de Souza Batista, V.E.; Cruz, R.S.; Oliveira, H.F.F.; Pellizzer, E.P. Three-dimensional finite element analysis of glass fiber and cast metal posts with different alloys for reconstruction of teeth without ferrule. J. Med. Eng. Technol. 2017, 41, 644–651. [Google Scholar] [CrossRef]
- Manaktala, M.; Taneja, S.; Bhalla, V.K. Stress distribution in endodontically treated external cervical resorption lesions restored with MTA and biodentine—A finite element analysis. J. Oral Biol. Craniofacial Res. 2024, 14, 415–422. [Google Scholar] [CrossRef]
- Peroz, I.; Blankenstein, F.; Lange, K.P.; Naumann, M. Restoring endodontically treated teeth with posts and cores-A review. Quintessence Int. 2005, 36, 737–746. [Google Scholar] [PubMed]
- Kalra, D.; Sukhija, D.; Rassawet, R.R.; Rani, D. A review on post and core. Sch. J. Dent. Sci. 2020, 07, 51–56. [Google Scholar] [CrossRef]
- Aurélio, I.L.; Fraga, S.; Rippe, M.P.; Valandro, L.F. Are posts necessary for the restoration of root filled teeth with limited tissue loss? A structured review of laboratory and clinical studies. Int. Endod. J. 2016, 49, 827–835. [Google Scholar] [CrossRef]
- Josic, U.; Radovic, I.; Juloski, J.; Beloica, M.; Popovic, M.; Alil, A.; Mandic, J.C. Can fiber-post placement reinforce structurally compromised roots? J. Adhes. Dent. 2020, 22, 409–414. [Google Scholar] [CrossRef] [PubMed]
- Fehrenbach, J.; de Soares, J.L.S.; do Nascimento Foly, J.C.S.; Miotti, L.L.; Münchow, E.A. Mechanical performance of endocrown restorations in anterior teeth: A systematic review and network meta-analysis. Dent. Mater. 2025, 41, 28–41. [Google Scholar] [CrossRef] [PubMed]
- Shetty, P.P.; Meshramkar, R.; Patil, K.N.; Nadiger, R.K. A finite element analysis for a comparative evaluation of stress with two commonly used esthetic posts. Eur. J. Dent. 2013, 7, 419–422. [Google Scholar] [CrossRef] [PubMed]
- Vikhe, D.M. Restoration of Endodontically Treated Teeth. In Clinical Concepts and Practical Management Techniques in Dentistry; Moolla, I., Ed.; IntechOpen: London, UK, 2021; Available online: https://www.intechopen.com/chapters/76852 (accessed on 21 February 2025).
- Goracci, C.; Ferrari, M. Current perspectives on post systems: A literature review. Aust. Dent. J. 2011, 56, 77–83. [Google Scholar] [CrossRef]
- Machado, J.; Almeida, P.; Fernandes, S.; Marques, A.; Vaz, M. Currently used systems of dental posts for endodontic treatment. Procedia Struct. Integr. 2017, 5, 27–33. [Google Scholar] [CrossRef]
- Anthrayose, P.; Nawal, R.R.; Yadav, S.; Talwar, S.; Yadav, S. Effect of revascularisation and apexification procedures on biomechanical behaviour of immature maxillary central incisor teeth: A three-dimensional finite element analysis study. Clin. Oral. Investig. 2021, 25, 6671–6679. [Google Scholar] [CrossRef]
- Almaroof, A.G.; Thyab, S.A.; Ali, A.H. Bond strength of a new Kevlar fiber-reinforced composite post with semi-interpenetrating polymer network (IPN) matrix. J. Clin. Exp. Dent. 2019, 11, e695–e700. [Google Scholar] [CrossRef]
- Li, J.; Parada, C.; Chai, Y. Cellular and molecular mechanisms of tooth root development. Development 2017, 144, 374–384. [Google Scholar] [CrossRef]
- Badami, V.; Ketineni, H.; Pb, S.; Akarapu, S.; Mittapalli, S.P.; Khan, A. Comparative evaluation of different post materials on stress distribution in endodontically treated teeth using the finite element analysis method: A systematic review. Cureus 2022, 14, e29753. [Google Scholar] [CrossRef]
- Jitumori, R.T.; Bittencourt, B.F.; Reis, A.; Gomes, J.C.; Gomes, G.M. Effect of root canal irrigants on fiber post bonding using self-adhesive composite cements. J. Adhes. Dent. 2019, 21, 537–544. [Google Scholar] [CrossRef]
- Gomes, E.A.; Diana, H.H.; Oliveira, J.S.; Silva-Sousa, Y.T.C.; Faria, A.C.L.; Ribeiro, R.F. Reliability of FEA on the results of mechanical properties of materials. Braz. Dent. J. 2015, 26, 667–670. [Google Scholar] [CrossRef] [PubMed]
- Brkić, H.; Dumančić, J.; Vodanović, M. Biologija i Morfologija Ljudskih Zuba; Naklada Slap: Zagreb, Croatia, 2016; p. 61. [Google Scholar]


| Structure/Material | E, GPa | ν, - | References |
|---|---|---|---|
| Enamel | 41.0 | 0.30 | [33] |
| Dentin | 18.6 | 0.31 | [33] |
| Periodontal ligament (PDL) | 0.00067 | 0.45 | [34] |
| Pulp | 0.00207 | 0.45 | [33] |
| Cortical bone | 13.4 | 0.26 | [33] |
| Trabecular bone | 0.345 | 0.36 | [33] |
| Gutapercha | 0.14 | 0.45 | [35] |
| Glass ionomer cement | 8.0 | 0.25 | [36] |
| Composite filling | 13.45 | 0.17 | [37] |
| Composite cement | 8.3 | 0.28 | [38] |
| PS1 (GC Fiberpost) | 40.0 | 0.25 | [39] |
| PS2 (RelyX post 3M ESPE) | 37.5 | 0.26 | [40,41] |
| PS3 (Metal post Unimetric 1.0 Dentsply) | 110.0 | 0.32 | [38] |
| PS4 (EverStick Post GC) | 15.0 | 0.18 | [39] |
| APICAL LEVEL | ||||||
|---|---|---|---|---|---|---|
| Model | S1 | S2 | S3 | S4 | S5 | |
| PS1 | Mean | 91.78 ± 6.17 | 35.99 ± 2.63 | 44.30 ± 4.07 | 20.12 ± 2.14 | 12.51 ± 1.42 |
| SD | 27.75 | 11.82 | 18.33 | 9.64 | 6.42 | |
| PS2 | Mean | 105.59 ± 8.72 | 85.50 ± 6.84 | 51.11 ± 4.55 | 23.29 ± 2.47 | 15.19 ± 1.95 |
| SD | 39.19 | 30.74 | 20.47 | 11.13 | 8.78 | |
| PS3 | Mean | 69.60 ± 5.03 | 80.84 ± 6.87 | 44.53 ± 4.08 | 21.73 ± 2.53 | 15.17 ± 2.33 |
| SD | 22.61 | 30.87 | 18.37 | 11.40 | 10.50 | |
| PS4 | Mean | 82.83 ± 3.95 | 48.43 ± 2.73 | 47.95 ± 4.71 | 20.24 ± 2.14 | 14.08 ± 1.81 |
| SD | 17.77 | 12.29 | 21.19 | 9.63 | 8.17 | |
| PC | Mean | 103.44 ± 6.68 | 46.10 ± 2.32 | 52.49 ± 4.89 | 17.85 ± 1.88 | 14.40 ± 1.84 |
| SD | 30.05 | 10.45 | 22.01 | 8.46 | 8.28 | |
| NC | Mean | 97.95 ± 5.95 | 44.96 ± 2.39 | 54.28 ± 5.20 | 21.25 ± 1.96 | 12.67 ± 1.63 |
| SD | 26.76 | 10.77 | 23.36 | 8.82 | 7.35 | |
| CERVICAL LEVEL | ||||||
| Model | S1 | S2 | S3 | S4 | S5 | |
| PS1 | Mean | 59.06 ± 1.28 | 59.70 ± 1.11 | 59.35 ± 0.79 | 57.48 ± 1.03 | 58.81 ± 1.08 |
| SD | 5.77 | 5.01 | 4.97 | 4.65 | 4.88 | |
| PS2 | Mean | 61.60 ± 1.25 | 60.12 ± 1.14 | 59.89 ± 1.14 | 58.79 ± 1.02 | 58.98 ± 1.09 |
| SD | 5.63 | 5.16 | 5.14 | 4.59 | 4.91 | |
| PS3 | Mean | 58.77 ± 0.96 | 59.29 ± 1.13 | 59.64 ± 1.11 | 58.62 ± 1.08 | 58.66 ± 0.98 |
| SD | 4.34 | 5.11 | 5.02 | 4.87 | 4.42 | |
| PS4 | Mean | 55.19 ± 1.70 | 58.78 ± 0.93 | 58.84 ± 1.04 | 58.74 ± 1.11 | 58.87 ± 1.02 |
| SD | 7.67 | 4.19 | 4.68 | 5.03 | 4.58 | |
| PC | Mean | 63.00 ± 1.24 | 60.51 ± 1.20 | 59.64 ± 1.08 | 59.44 ± 1.14 | 59.50 ± 1.14 |
| SD | 5.58 | 5.42 | 4.85 | 5.12 | 5.14 | |
| NC | Mean | 64.88 ± 1.33 | 63.12 ± 1.06 | 61.42 ± 1.13 | 62.07 ± 1.13 | 60.68 ± 1.10 |
| SD | 6.01 | 4.77 | 5.12 | 5.11 | 4.96 | |
| p-VALUE | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| APICAL LEVEL | CERVICAL LEVEL | ||||||||||
| Model | S1 | S2 | S3 | S4 | S5 | S1 | S2 | S3 | S4 | S5 | |
| PS1 | PS2 | 0.025 | 0.000 | 0.299 | 0.330 | 0.325 | 0.075 | 0.995 | 0.983 | 0.543 | 1.000 |
| PS3 | 0.000 | 0.000 | 1.000 | 0.909 | 0.333 | 1.000 | 0.995 | 0.999 | 0.687 | 1.000 | |
| PS4 | 0.337 | 0.001 | 0.874 | 1.000 | 0.842 | 0.001 | 0.848 | 0.986 | 0.586 | 1.000 | |
| PC | 0.094 | 0.019 | 0.125 | 0.697 | 0.706 | 0.000 | 0.906 | 0.999 | 0.120 | 0.94 | |
| NC | 0.735 | 0.055 | 0.029 | 0.979 | 1.000 | 0.000 | 0.000 | 0.091 | 0.000 | 0.141 | |
| PS2 | PS1 | 0.025 | 0.000 | 0.299 | 0.330 | 0.325 | 0.075 | 0.995 | 0.983 | 0.543 | 1.000 |
| PS3 | 0.000 | 0.683 | 0.339 | 0.919 | 1.000 | 0.031 | 0.897 | 0.999 | 1.000 | 0.998 | |
| PS4 | 0.000 | 0.000 | 0.929 | 0.372 | 0.959 | 0.000 | 0.524 | 0.759 | 1.000 | 1.000 | |
| PC | 0.997 | 0.000 | 0.998 | 0.007 | 0.991 | 0.666 | 0.996 | 1.000 | 0.960 | 0.983 | |
| NC | 0.520 | 0.000 | 0.927 | 0.783 | 0.397 | 0.007 | 0.002 | 0.376 | 0.000 | 0.224 | |
| PS3 | PS1 | 0.000 | 0.000 | 1.000 | 0.909 | 0.333 | 1.000 | 0.995 | 0.999 | 0.687 | 1.000 |
| PS2 | 0.000 | 0.683 | 0.339 | 0.919 | 1.000 | 0.031 | 0.897 | 0.999 | 1.000 | 0.998 | |
| PS4 | 0.036 | 0.000 | 0.903 | 0.931 | 0.962 | 0.002 | 0.987 | 0.912 | 1.000 | 1.000 | |
| PC | 0.000 | 0.000 | 0.148 | 0.133 | 0.992 | 0.000 | 0.628 | 1.000 | 0.898 | 0.879 | |
| NC | 0.000 | 0.000 | 0.036 | 1.000 | 0.406 | 0.000 | 0.000 | 0.207 | 0.000 | 0.087 | |
| PS4 | PS1 | 0.337 | 0.001 | 0.874 | 1.000 | 0.842 | 0.001 | 0.848 | 0.986 | 0.586 | 1.000 |
| PS2 | 0.000 | 0.000 | 0.929 | 0.372 | 0.959 | 0.000 | 0.524 | 0.759 | 1.000 | 1.000 | |
| PS3 | 0.036 | 0.000 | 0.903 | 0.931 | 0.962 | 0.002 | 0.987 | 0.912 | 1.000 | 1.000 | |
| PC | 0.000 | 0.977 | 0.736 | 0.651 | 1.000 | 0.000 | 0.234 | 0.911 | 0.946 | 0.962 | |
| NC | 0.010 | 0.884 | 0.383 | 0.987 | 0.894 | 0.000 | 0.000 | 0.014 | 0.000 | 0.169 | |
| PC | PS1 | 0.094 | 0.019 | 0.125 | 0.697 | 0.706 | 0.000 | 0.906 | 0.999 | 0.120 | 0.944 |
| PS2 | 0.997 | 0.000 | 0.998 | 0.007 | 0.991 | 0.666 | 0.996 | 1.000 | 0.960 | 0.983 | |
| PS3 | 0.000 | 0.000 | 0.148 | 0.133 | 0.992 | 0.000 | 0.628 | 1.000 | 0.898 | 0.879 | |
| PS4 | 0.000 | 0.977 | 0.736 | 0.651 | 1.000 | 0.000 | 0.234 | 0.911 | 0.946 | 0.962 | |
| NC | 0.820 | 0.999 | 0.994 | 0.254 | 0.779 | 0.338 | 0.012 | 0.208 | 0.009 | 0.636 | |
| NC | PS1 | 0.735 | 0.055 | 0.029 | 0.979 | 1.000 | 0.000 | 0.000 | 0.091 | 0.000 | 0.141 |
| PS2 | 0.520 | 0.000 | 0.927 | 0.783 | 0.397 | 0.007 | 0.002 | 0.376 | 0.000 | 0.224 | |
| PS3 | 0.000 | 0.000 | 0.036 | 1.000 | 0.406 | 0.000 | 0.000 | 0.207 | 0.000 | 0.087 | |
| PS4 | 0.010 | 0.884 | 0.383 | 0.987 | 0.894 | 0.000 | 0.000 | 0.014 | 0.000 | 0.169 | |
| PC | 0.820 | 0.999 | 0.994 | 0.254 | 0.779 | 0.338 | 0.012 | 0.208 | 0.009 | 0.636 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bučević Sojčić, P.; Leder Horina, J.; Bočkaj, N.; Borojević Renić, T.; Turjanski, D.; Goršeta, K.; Jurčević Lulić, T.; Jurić, H. Stress Behaviour of an Immature Maxillary Central Incisor: A 3D Finite Element Analysis. Materials 2025, 18, 2305. https://doi.org/10.3390/ma18102305
Bučević Sojčić P, Leder Horina J, Bočkaj N, Borojević Renić T, Turjanski D, Goršeta K, Jurčević Lulić T, Jurić H. Stress Behaviour of an Immature Maxillary Central Incisor: A 3D Finite Element Analysis. Materials. 2025; 18(10):2305. https://doi.org/10.3390/ma18102305
Chicago/Turabian StyleBučević Sojčić, Petra, Jasna Leder Horina, Nina Bočkaj, Tea Borojević Renić, Dubravka Turjanski, Kristina Goršeta, Tanja Jurčević Lulić, and Hrvoje Jurić. 2025. "Stress Behaviour of an Immature Maxillary Central Incisor: A 3D Finite Element Analysis" Materials 18, no. 10: 2305. https://doi.org/10.3390/ma18102305
APA StyleBučević Sojčić, P., Leder Horina, J., Bočkaj, N., Borojević Renić, T., Turjanski, D., Goršeta, K., Jurčević Lulić, T., & Jurić, H. (2025). Stress Behaviour of an Immature Maxillary Central Incisor: A 3D Finite Element Analysis. Materials, 18(10), 2305. https://doi.org/10.3390/ma18102305







