Three-Dimensional Printing Resin-Based Dental Provisional Crowns and Bridges: Recent Progress in Properties, Applications, and Perspectives
Abstract
1. Introduction
2. Three-Dimensional Printing Technology and Materials
2.1. Types of 3D Printing Technologies
2.1.1. SLA
2.1.2. DLP
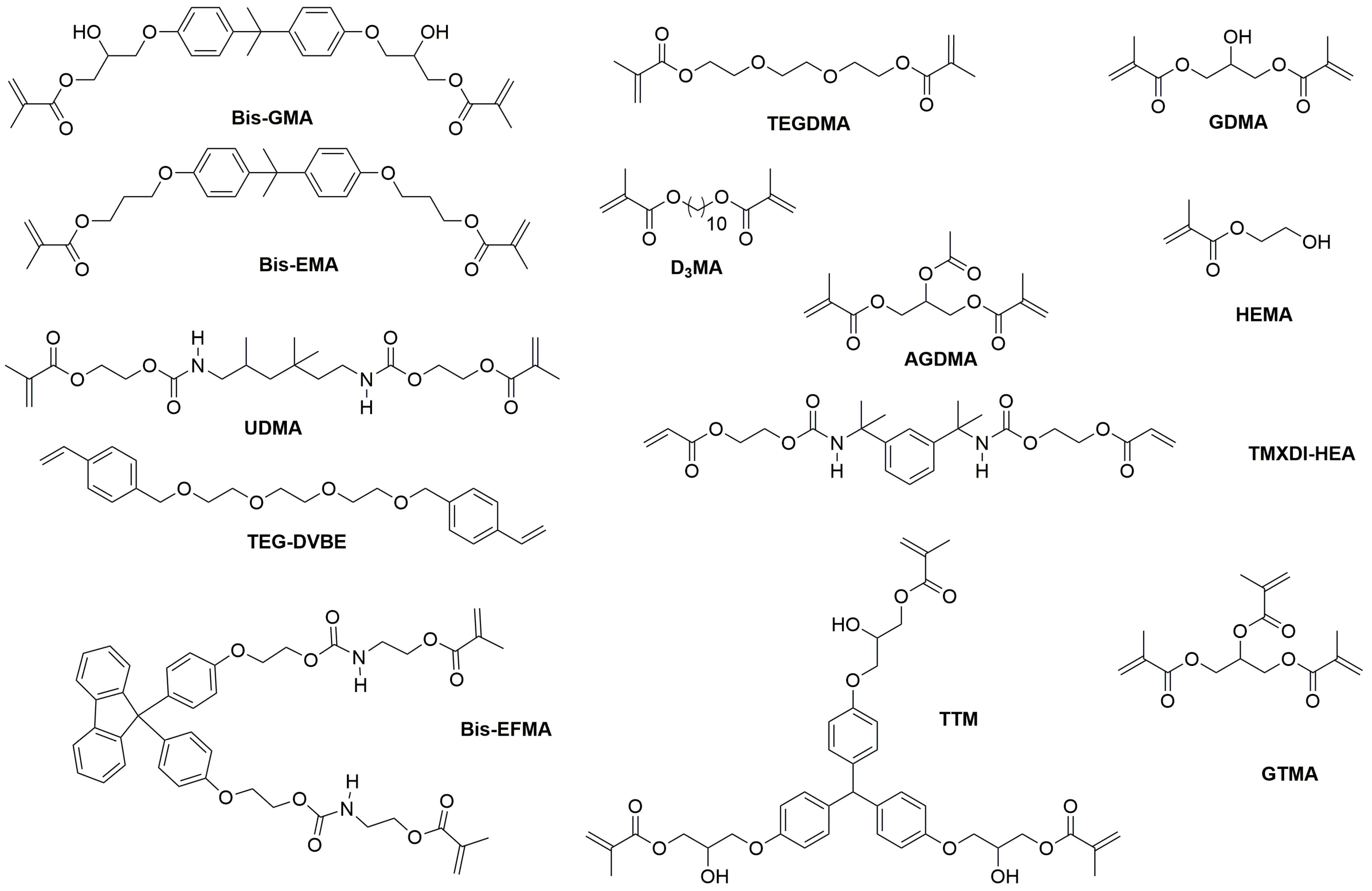
2.2. Composition of Printable Provisional Resins
3. Properties and Performance
3.1. Mechanical Properties
3.1.1. Flexural Strength
3.1.2. Elastic Modulus
3.1.3. Fracture Strength
3.1.4. Microhardness
3.1.5. Wear Resistance and Frictional Properties
3.2. Mechanical Property Enhancement
3.2.1. Filler
3.2.2. Printing Parameters
3.2.3. Cleaning Methods
3.2.4. Post-Polymerization
3.2.5. Aging Treatment
3.3. Physical Properties
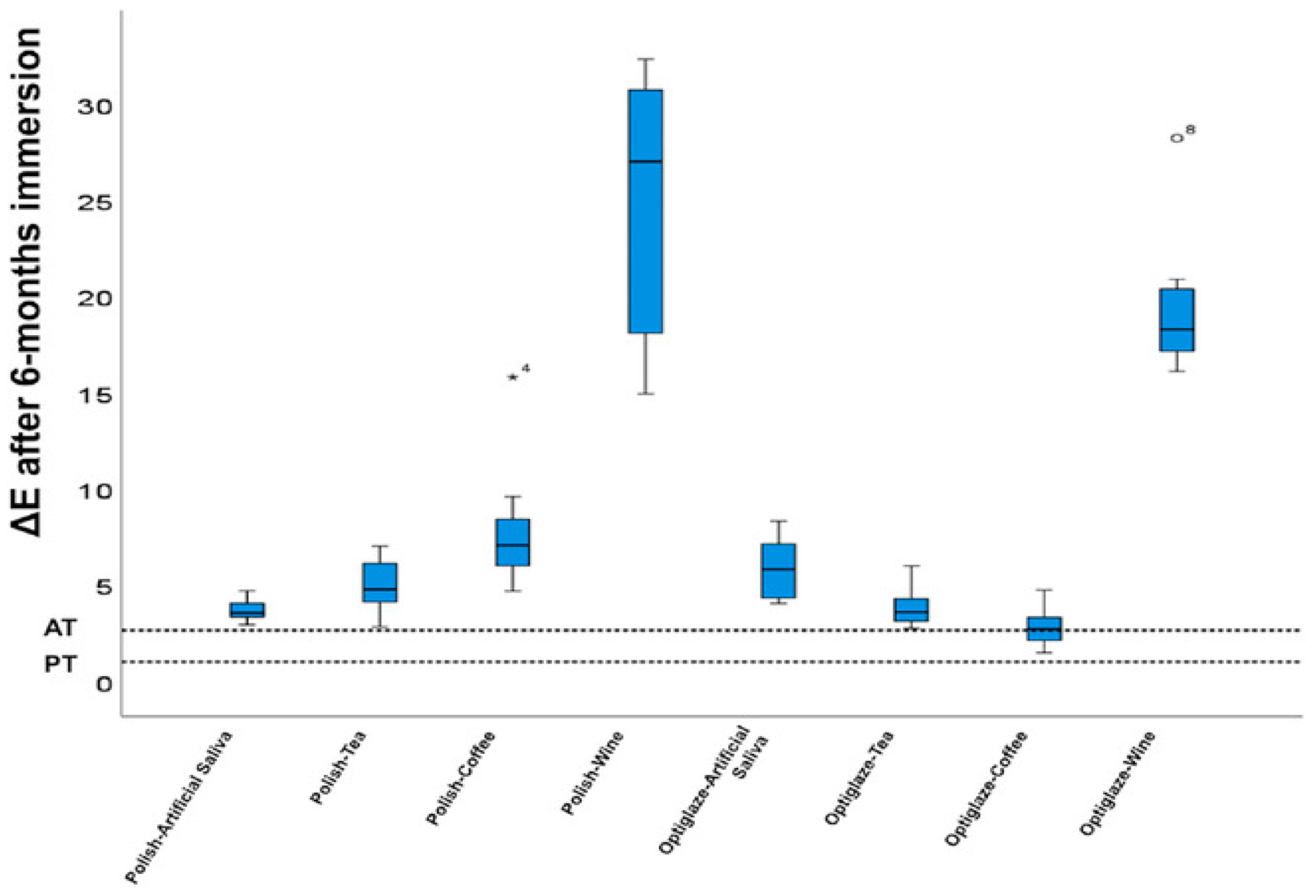
3.3.1. Color Stability
3.3.2. Water Sorption and Solubility
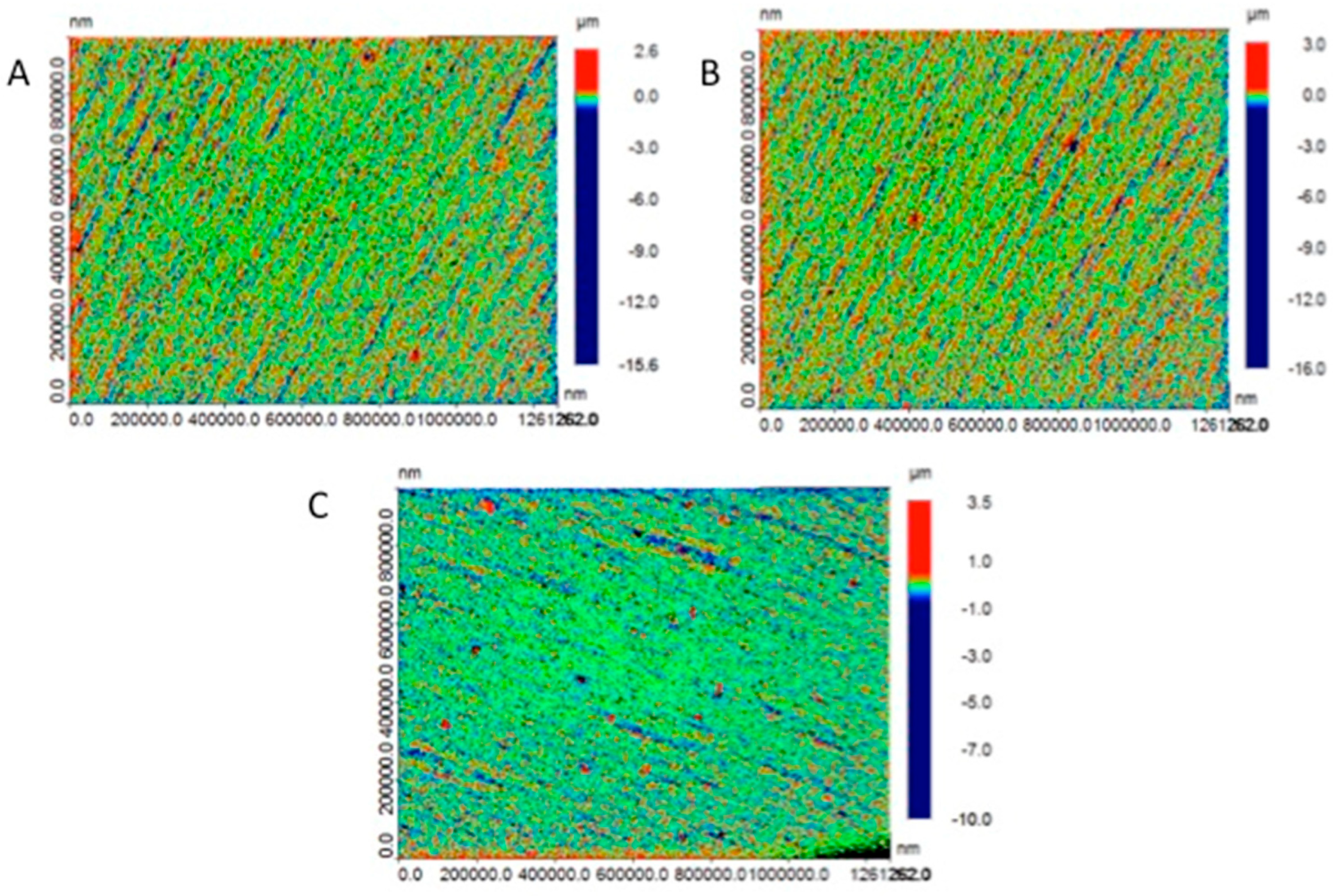
3.3.3. Surface Roughness
| Author and Year | Evaluated Materials | Specimen Fabrication Technique | 3D Printing Parameters | Key Results |
|---|---|---|---|---|
| Aldahian et al. (2021) [86] | -Conventional: PMMA -CAD/CAM: PMMA blocks -3D Printing: Dimethacrylates | -Conventional: Auto-polymerizing resin poured into molds -CAD/CAM: Milled from PMMA blocks using a wet milling machine -3D Printing: SLA | -Layer thickness: 50 μm -Wavelength: 405 nm -Curing time per layer: 2.40 s -3D-printed specimens soaked in 99% isopropyl alcohol for 60 s | -Highest surface roughness observed in 3D-printed specimens (5.61 ± 0.33 μm). -Lowest surface roughness observed in CAD/CAM specimens (3.28 ± 0.34 μm). |
| Wadhwani et al. (2022) [150] | NextDent C&B temporary tooth-colored resin (SprintRay for DLP and FormLabs for SLA) | 3D printing using SLA and DLP technologies | -Specific values of layer thickness not provided -Cleaning with 99.9% ethyl alcohol, clipping support structures, and light curing according to manufacturer’s guidelines | Both SLA and DLP samples showed surface roughness within acceptable ranges. Polishing significantly reduced roughness depth (p < 0.05). SLA samples had slightly lower roughness than DLP. |
| Rafat Sasany et al. (2024) [146] | -VarseoSmile Crown Plus-Crowntec: Similar to VS but with pyrogenic silica -NextDent C&B MFH -GC Temp PRINT | DLP | -Layer thickness (μm): 25, 50, 100 -Build angle: 30 degrees -Post-print cleaning with alcohol -Specimens were polished with silicon carbide papers (500–4000 grit) and stored in the dark | -Surface roughness (Ra) increased significantly with 100 μm layer thickness (p ≤ 0.001). -At 25 μm layer thickness, Ra values were within the 0.2 μm threshold for all materials. |
| Shin et al. (2020) [147] | -Polycarbonate block: Polycarbonate, nanosilica filler, glass fiber, alkoxysilane -PMMA: High cross-linked PMMA resin -Dispersed–Filled Composite: Composite resin material (BisGMA, TEGDMA) with 77 wt% silica, zirconia, and barium glass nanoparticles -NextDent C&B -Denture Teeth A2 resin | -CAD/CAM blocks: Milled using a precision cutting machine -3D printing resins: DLP and SLA | -Layer thickness: 100 µm -Printers: DLP (NextDent ND5100) and SLA (Form 3) -Settings: 405 nm UV LED light and 250 mW laser power -Washed using 90% isopropyl alcohol -Post-curing conducted in UV post-curing equipment | -3D printing resins showed smoother surfaces compared to CAD/CAM blocks, which had rough surfaces with traces of bur passes. |
3.3.4. Marginal Adaptation and Internal Fit
| Author and Year | Evaluated Materials | Shape and Dimension of Tested Resin Samples | Key Results |
|---|---|---|---|
| Wadhwani et al., 2022 [150] | -NextDent C&B temporary tooth-colored resin | 3-unit fixed partial denture (FPD) | -SLA technology demonstrated better marginal adaptation compared to DLP; the study suggests SLA might be more precise for dental provisional restorations |
| Pekka Ahlholm et al., 2024 [157] | -Resin: G-aenial Universal Injectable (GC) -Flowable Composite: everX Flow (GC) | 12 different restorations: -11 inlays/onlays -1 crown Approximate dimensions: 3.5–7.7 mm width, 6–10 mm height, 1.6–4.2 mm depth | -Internal gaps in the 3D-printed mold group were 6% to 51% smaller than in the milled group -The accuracy was more favorable for most restoration types, except for crown preparations -3D-printed mold restorations showed better fit in complex shapes and long margins |
| Saurabh Chaturvedi et al. (2020) [159] | -Protemp™ 4 (3M ESPE, Seefeld, Germany) -Formlabs Dental SG Resin (Formlabs Inc., USA) -Ceramill TEMP (Amann Girrbach, Maeder, Austria) | Provisional crowns for maxillary first premolar with three finish-line designs: -Chamfer -Rounded shoulder -Rounded shoulder with bevel | -3D-printed crowns showed minimal marginal gap -Best overall internal fit compared to molding and milling methods |
| Nawal Alharbi et al. (2018) [158] | Temporis™ (Hybrid composite resin material) | Maxillary central incisor crown models | -3D-printed restorations showed significantly lower marginal and internal gaps compared to milled restorations |
| Tahayeri et al. (2018) [15] | 1. NextDent C&B (3D-printed resin)—Vertex Dental 2. Integrity®—Dentsply Canada Ltd., Woodbridge, Canada 3. Jet®—Lang Dental Inc., Wheeling, IL, USA | Test bars: 25 mm × 2 mm × 2 mm | Printing accuracy varied as follows: -Length: 0.12–2.4% error -Width: Up to 22% error -Thickness: Up to 20% error -90° orientation and white resin setting were most accurate |
| Peng et al., 2020 [161] | 1. Jet (Lang Dental Inc., Wheeling, IL, USA)—Autopolymerized PMMA resin, APP group 2. ZCAD Temp Fix (Harvest Dental)—CAD/CAM PMMA resin, CAM group 3. NextDent C&B MFH (3D Systems)—3D-printed methacrylic oligomers, 3DP group | Interim dental crowns on a mandibular first molar resin die | 1. Digitally fabricated crowns (CAM and 3DP) had significantly better internal fit and smaller marginal discrepancy compared to manually constructed crowns 2. No significant difference between CAD/CAM and 3D-printed crowns 3. Gap distance ranged from 0.13 mm to 0.55 mm 4. Cement space volume ranged from 24.09 to 33.67 mm3 |
| Wan-Sun Lee et al., 2017 [162] | 1. Vipi block (VIPI, Pirassununga, Brazil)—Milling block 2. VeroGlaze MED620 (Stratasys, Minnetonka, MN, USA)—3D Printing Resin 3. ZMD-1000B (Dentis, Daegu, Korea)—3D Printing Resin | Interim dental crowns for upper first molar | -Mean discrepancy: CAD/CAM milling: 171.6 (97.4) μm 3D printing (Stratasys): 149.1 (65.9) μm 3D printing (Dentis): 91.1 (36.4) μm -3D printing showed statistically better fit than milling |
3.3.5. The Effect of pH on the Durability of 3D-Printed Resins
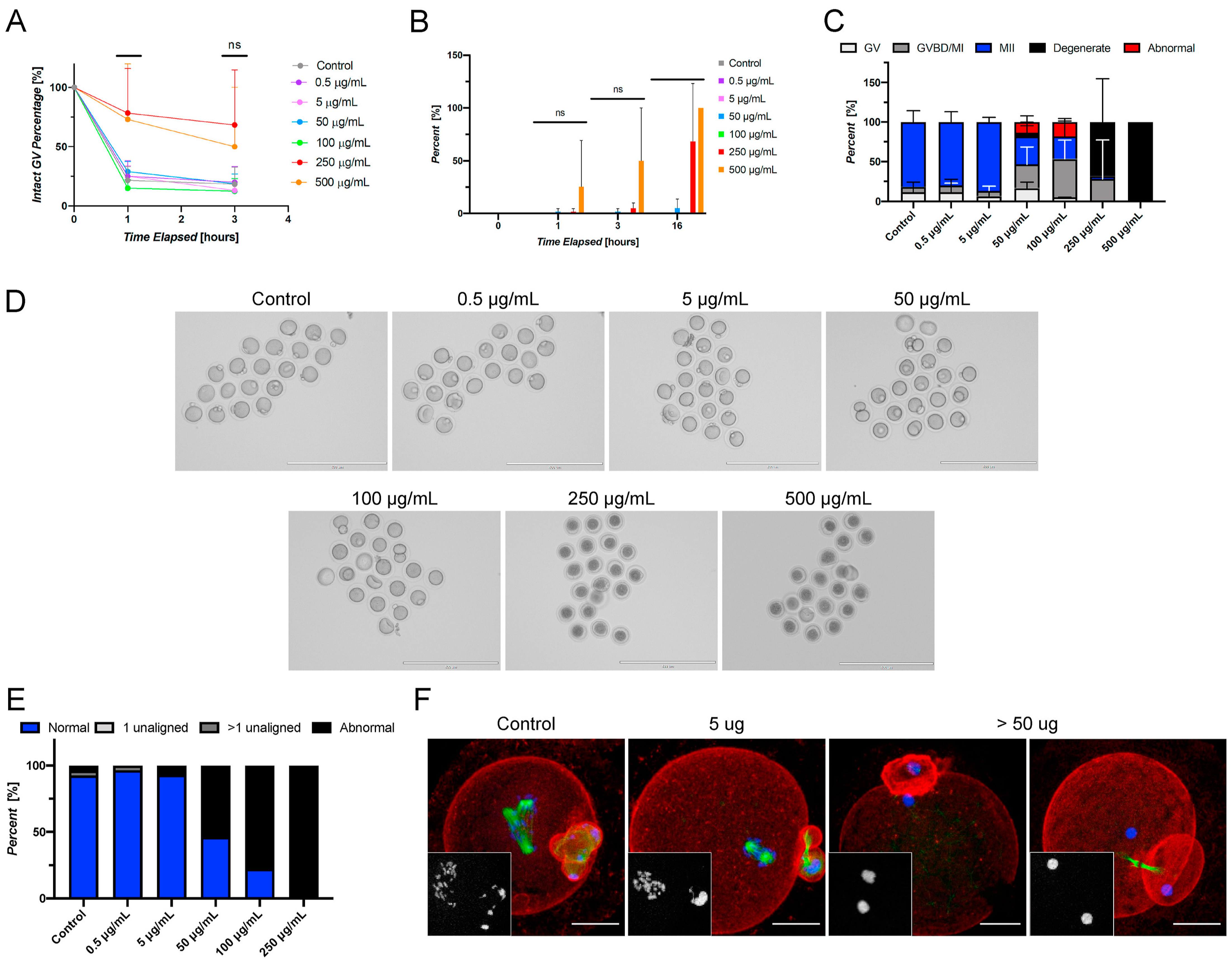
3.4. Biocompatibility
3.5. Antibacterial Property
4. Clinical Applications
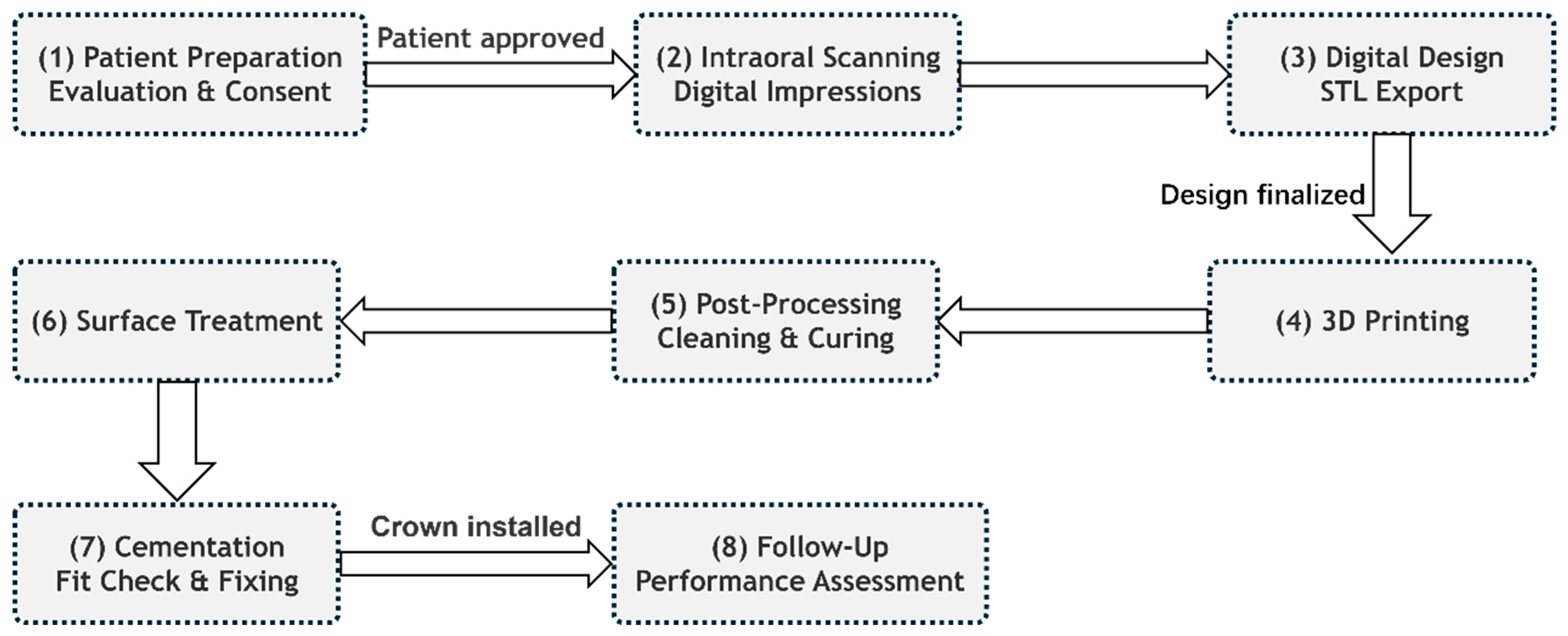
4.1. Clinical Workflow
4.2. Clinical Studies and Evidence
4.3. Limitations and Clinical Challenges
5. Conclusions and Future Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Espinar, C.; Della Bona, A.; Perez, M.M.; Tejada-Casado, M.; Pulgar, R. The influence of printing angle on color and translucency of 3D printed resins for dental restorations. Dent. Mater. 2023, 39, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Song, S.-Y.; Shin, Y.-H.; Lee, J.-Y.; Shin, S.-W. Color stability of provisional restorative materials with different fabrication methods. J. Adv. Prosthodont. 2020, 12, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Abdulmohsen, B.; Parker, S.; Braden, M.; Patel, M.P. A study to investigate and compare the physicomechanical properties of experimental and commercial temporary crown and bridge materials. Dent. Mater. 2016, 32, 200–210. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.; Wismeijer, D. Effects of build direction on the mechanical properties of 3D-printed complete coverage interim dental restorations. J. Prosthet. Dent. 2016, 115, 760–767. [Google Scholar] [CrossRef]
- Gupta, G.; Gupta, T. Evaluation of the effect of various beverages and food material on the color stability of provisional materials—An in vitro study. J. Conserv. Dent. JCD 2011, 14, 287–292. [Google Scholar] [CrossRef]
- Atria, P.J.; Lagos, I.; Sampaio, C.S. In vitro evaluation of surface roughness, color stability, and color masking of provisional restoration materials for veneers and crowns. Int. J. Comput. Dent. 2020, 23, 343–350. [Google Scholar]
- Andjela, L.; Abdurahmanovich, V.M.; Vladimirovna, S.N.; Mikhailovna, G.I.; Yurievich, D.D.; Alekseevna, M.Y. A review on Vat Photopolymerization 3D-printing processes for dental application. Dent. Mater. 2022, 38, e284–e296. [Google Scholar] [CrossRef]
- Xia, J.; Li, Y.; Cai, D.; Shi, X.; Zhao, S.; Jiang, Q.; Yang, X. Direct resin composite restoration of maxillary central incisors using a 3D-printed template: Two clinical cases. BMC Oral Health 2018, 18, 158. [Google Scholar] [CrossRef]
- Moraru, E.; Besnea, D.; Dontu, O.; Gheorghe, G.I.; Constantin, V. Applications of Additive Technologies in Realization of Customized Dental Prostheses; Springer International Publishing: Cham, Switzerland, 2019; pp. 8–17. [Google Scholar]
- Della Bona, A.; Cantelli, V.; Britto, V.T.; Collares, K.F.; Stansbury, J.W. 3D printing restorative materials using a stereolithographic technique: A systematic review. Dent. Mater. 2021, 37, 336–350. [Google Scholar] [CrossRef]
- Yang, J.; Liang, X.; Liu, F.; Biao, Y.; He, J. Comparing Properties of Urethane Dimethacrylate (UDMA) Based 3D Printing Resin Using N-Acryloylmorpholine (ACMO) and Triethylene Glycol Dimethacrylate (TEGDMA) Separately as Diluents. J. Macromol. Sci. Part B 2024, 1–17. [Google Scholar] [CrossRef]
- Carlotti, M.; Mattoli, V. Functional Materials for Two-Photon Polymerization in Microfabrication. Small 2019, 15, 1902687. [Google Scholar] [CrossRef] [PubMed]
- Thomé, T.; Erhardt, M.C.G.; Leme, A.A.; Al Bakri, I.; Bedran-Russo, A.K.; Bertassoni, L.E. Emerging Polymers in Dentistry. In Advanced Polymers in Medicine; Puoci, F., Ed.; Springer International Publishing: Cham, Switzerland, 2015; pp. 265–296. [Google Scholar]
- Khorsandi, D.; Fahimipour, A.; Abasian, P.; Saber, S.S.; Seyedi, M.; Ghanavati, S.; Ahmad, A.; De Stephanis, A.A.; Taghavinezhaddilami, F.; Leonova, A.; et al. 3D and 4D printing in dentistry and maxillofacial surgery: Printing techniques, materials, and applications. Acta Biomater. 2021, 122, 26–49. [Google Scholar] [CrossRef] [PubMed]
- Tahayeri, A.; Morgan, M.; Fugolin, A.P.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.S.; Ferracane, J.L.; Bertassoni, L.E. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef]
- Piedra-Cascón, W.; Krishnamurthy, V.R.; Att, W.; Revilla-León, M. 3D printing parameters, supporting structures, slicing, and post-processing procedures of vat-polymerization additive manufacturing technologies: A narrative review. J. Dent. 2021, 109, 103630. [Google Scholar] [CrossRef]
- Jain, S.; Sayed, M.E.; Shetty, M.; Alqahtani, S.M.; Al Wadei, M.H.D.; Gupta, S.G.; Othman, A.A.A.; Alshehri, A.H.; Alqarni, H.; Mobarki, A.H.; et al. Physical and Mechanical Properties of 3D-Printed Provisional Crowns and Fixed Dental Prosthesis Resins Compared to CAD/CAM Milled and Conventional Provisional Resins: A Systematic Review and Meta-Analysis. Polymers 2022, 14, 2691. [Google Scholar] [CrossRef]
- Dimitrova, M.; Vlahova, A.; Kalachev, Y.; Zlatev, S.; Kazakova, R.; Capodiferro, S. Recent Advances in 3D Printing of Polymers for Application in Prosthodontics. Polymers 2023, 15, 4525. [Google Scholar] [CrossRef]
- Stansbury, J.W.; Idacavage, M.J. 3D printing with polymers: Challenges among expanding options and opportunities. Dent. Mater. 2016, 32, 54–64. [Google Scholar] [CrossRef]
- Bakhtiari, H.; Aamir, M.; Tolouei-Rad, M. Effect of 3D Printing Parameters on the Fatigue Properties of Parts Manufactured by Fused Filament Fabrication: A Review. Appl. Sci. 2023, 13, 904. [Google Scholar] [CrossRef]
- de Souza, F.A.; Blois, M.C.; Collares, K.; dos Santos, M.B.F. 3D-printed and conventional provisional single crown fabrication on anterior implants: A randomized clinical trial. Dent. Mater. 2024, 40, 340–347. [Google Scholar] [CrossRef]
- He, Y.; Wu, Y.; Fu, J.-z.; Gao, Q.; Qiu, J.-j. Developments of 3D Printing Microfluidics and Applications in Chemistry and Biology: A Review. Electroanalysis 2016, 28, 1658–1678. [Google Scholar] [CrossRef]
- Dehurtevent, M.; Robberecht, L.; Hornez, J.-C.; Thuault, A.; Deveaux, E.; Béhin, P. Stereolithography: A new method for processing dental ceramics by additive computer-aided manufacturing. Dent. Mater. 2017, 33, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Jiang, M.; Zhou, Z.; Gou, J.; Hui, D. 3D printing of polymer matrix composites: A review and prospective. Compos. Part B: Eng. 2017, 110, 442–458. [Google Scholar] [CrossRef]
- Kessler, A.; Hickel, R.; Reymus, M. 3D Printing in Dentistry—State of the Art. Oper. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Puebla, K.; Arcaute, K.; Quintana, R.; Wicker, R.B. Effects of environmental conditions, aging, and build orientations on the mechanical properties of ASTM type I specimens manufactured via stereolithography. Rapid Prototyp. J. 2012, 18, 374–388. [Google Scholar] [CrossRef]
- Wu, G.-H.; Hsu, S.-h. Review: Polymeric-Based 3D Printing for Tissue Engineering. J. Med. Biol. Eng. 2015, 35, 285–292. [Google Scholar] [CrossRef]
- Golubovic, Z.; Mitrovic, A.; Mitrovic, N. 3D Printing in Contemporary Dentistry. In Proceedings of the International Conference of Experimental and Numerical Investigations and New Technologies (CNNTech), Zlatibor, Serbia, 5–8 July 2023; pp. 213–232. [Google Scholar]
- Dawood, A.; Marti, B.M.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef]
- Lin, C.-H.; Lin, Y.-M.; Lai, Y.-L.; Lee, S.-Y. Mechanical properties, accuracy, and cytotoxicity of UV-polymerized 3D printing resins composed of Bis-EMA, UDMA, and TEGDMA. J. Prosthet. Dent. 2020, 123, 349–354. [Google Scholar] [CrossRef]
- Molinero-Mourelle, P.; Gomez-Polo, M.; Gomez-Polo, C.; Ortega, R.; del Rio Highsmith, J.; Celemin-Vinuela, A. Preliminary Study on the Assessment of the Marginal Fit of Three-Dimensional Methacrylate Oligomer Phosphine Oxide Provisional Fixed Dental Prostheses Made by Digital Light Processing. Prosthesis 2020, 2, 240–245. [Google Scholar] [CrossRef]
- Osman, R.B.; Alharbi, N.; Wismeijer, D. Build angle: Does it influence the accuracy of 3D-printed dental restorations using digital light-processing technology? Int. J. Prosthodont. 2017, 30, 182–188. [Google Scholar] [CrossRef]
- Lai, J.; Wang, C.; Wang, M. 3D printing in biomedical engineering: Processes, materials, and applications. Appl. Phys. Rev. 2021, 8, 021322. [Google Scholar] [CrossRef]
- Ligon, S.C.; Liska, R.; Stampfl, J.; Gurr, M.; Mülhaupt, R. Polymers for 3D Printing and Customized Additive Manufacturing. Chem. Rev. 2017, 117, 10212–10290. [Google Scholar] [CrossRef] [PubMed]
- Hazeveld, A.; Huddleston Slater, J.J.R.; Ren, Y. Accuracy and reproducibility of dental replica models reconstructed by different rapid prototyping techniques. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Lutz, A.-M.; Hampe, R.; Roos, M.; Lümkemann, N.; Eichberger, M.; Stawarczyk, B. Fracture resistance and 2-body wear of 3-dimensional–printed occlusal devices. J. Prosthet. Dent. 2019, 121, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Sherman, S.L.; Kadioglu, O.; Currier, G.F.; Kierl, J.P.; Li, J. Accuracy of digital light processing printing of 3-dimensional dental models. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 422–428. [Google Scholar] [CrossRef]
- Revilla-León, M.; Meyers, M.J.; Zandinejad, A.; Özcan, M. A review on chemical composition, mechanical properties, and manufacturing work flow of additively manufactured current polymers for interim dental restorations. J. Esthet. Restor. Dent. 2019, 31, 51–57. [Google Scholar] [CrossRef]
- Britto, V.T.; Cantelli, V.; Collares, F.M.; Bertol, C.D.; Della Bona, A. Biomechanical properties of a 3D printing polymer for provisional restorations and artificial teeth. Dent. Mater. 2022, 38, 1956–1962. [Google Scholar] [CrossRef]
- Park, J.-M.; Ahn, J.-S.; Cha, H.-S.; Lee, J.-H. Wear Resistance of 3D Printing Resin Material Opposing Zirconia and Metal Antagonists. Materials 2018, 11, 1043. [Google Scholar] [CrossRef]
- Bergamo, E.T.P.; Campos, T.M.B.; Piza, M.M.T.; Gutierrez, E.; Lopes, A.C.O.; Witek, L.; Coelho, P.G.; Celestrino, M.; de Carvalho, L.F.; Benalcazar, E.B.; et al. Temporary materials used in prosthodontics: The effect of composition, fabrication mode, and aging on mechanical properties. J. Mech. Behav. Biomed. Mater. 2022, 133, 105333. [Google Scholar] [CrossRef]
- Schulz, A.-C.; Othman, A.; Strobele, D.-A.; Wagner, J.; Mosch, R.; von See, C. Fracture strength test of digitally produced ceramic-filled and unfilled dental resin restorations via 3d printing: An in vitro study. J. Clin. Exp. Dent. 2023, 15, e118–e124. [Google Scholar]
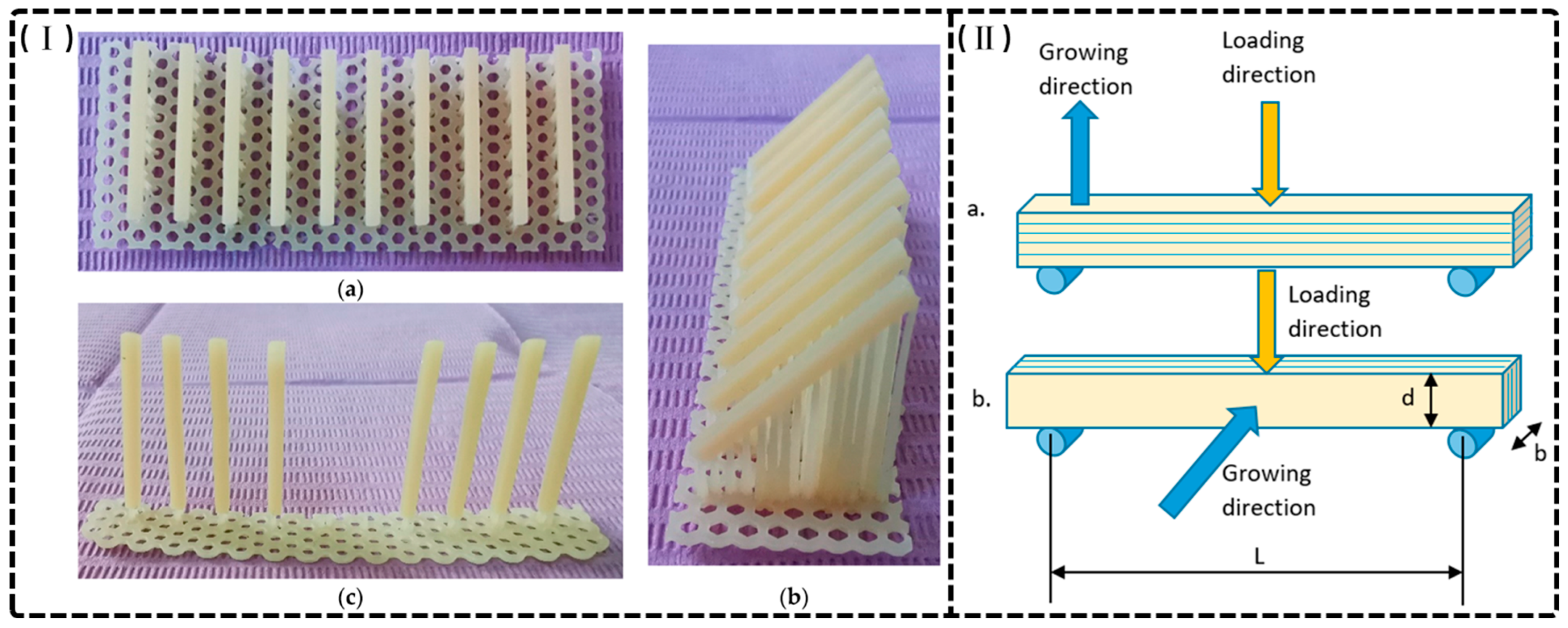
- Derban, P.; Negrea, R.; Rominu, M.; Marsavina, L. Influence of the Printing Angle and Load Direction on Flexure Strength in 3D Printed Materials for Provisional Dental Restorations. Materials 2021, 14, 3376. [Google Scholar] [CrossRef]
- Barragan-Paredes, M.-A.; Mosquera-Victoria, I.; Viveros-Rebolledo, C.A.; Rodriguez-Paz, M.L.; Munoz-Velez, M.F.; Valencia-Llano, C.H. Comparison of the Mechanical Properties of Temporary Abutments Made of Polyetheretherketone and Photopolymeric Resin. Open Dent. J. 2021, 15, 512–519. [Google Scholar] [CrossRef]
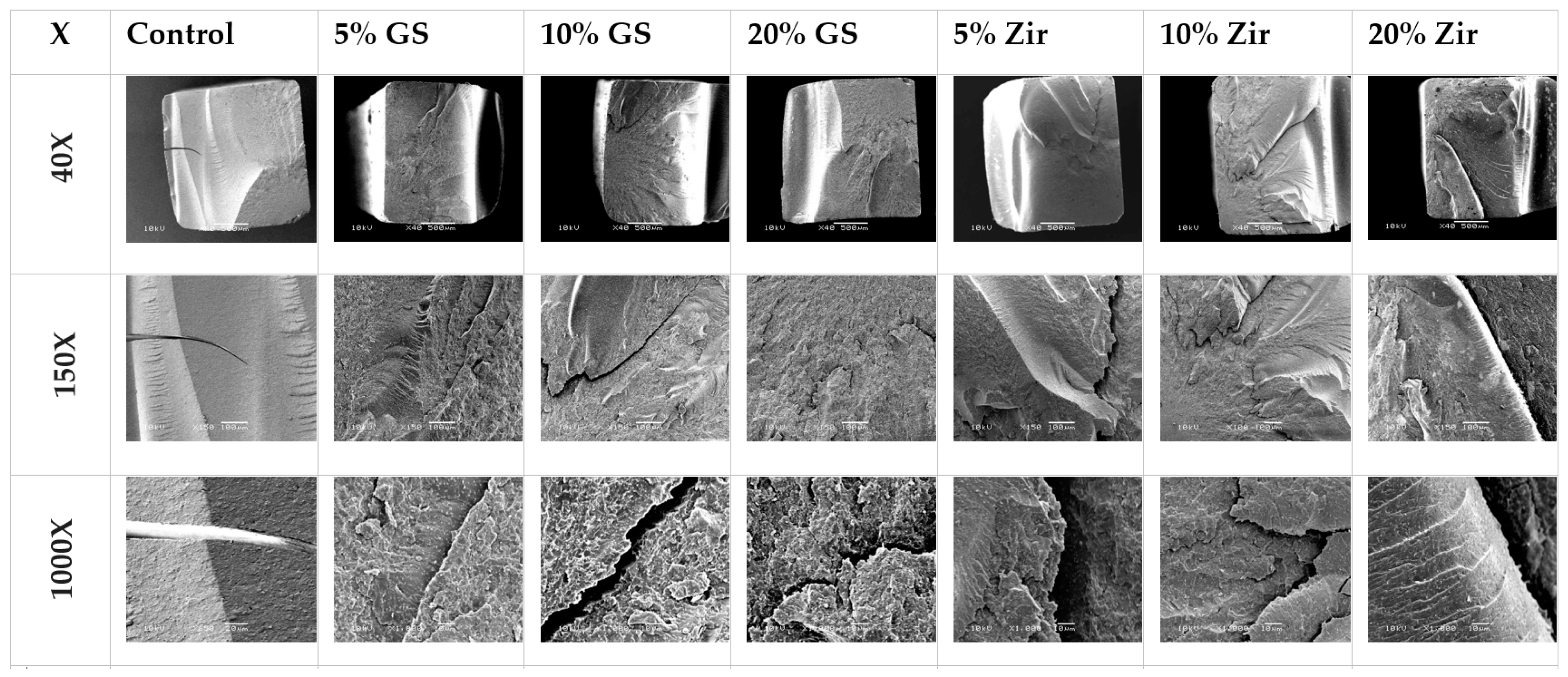
- Alshamrani, A.; Alhotan, A.; Kelly, E.; Ellakwa, A. Mechanical and Biocompatibility Properties of 3D-Printed Dental Resin Reinforced with Glass Silica and Zirconia Nanoparticles: In Vitro Study. Polymers 2023, 15, 2523. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Shou, W.; Makatura, L.; Matusik, W.; Fu, K. 3D printing of polymer composites: Materials, processes, and applications. Matter 2022, 5, 43–76. [Google Scholar] [CrossRef]
- Cho, K.; Rajan, G.; Farrar, P.; Prentice, L.; Prusty, B.G. Dental resin composites: A review on materials to product realizations. Compos. Part B Eng. 2022, 230, 109495. [Google Scholar] [CrossRef]
- Liang, X.; Yu, B.; Ye, L.; Lin, D.; Zhang, W.; Zhong, H.-J.; He, J. Recent Advances in Quaternary Ammonium Monomers for Dental Applications. Materials 2024, 17, 345. [Google Scholar] [CrossRef]
- Henderson, J.Y.; Korioth, T.V.P.; Tantbirojn, D.; Versluis, A. Failure load of milled, 3D-printed, and conventional chairside- dispensed interim 3-unit fixed dental prostheses. J. Prosthet. Dent. 2022, 127, 275.e1–275.e7. [Google Scholar] [CrossRef]
- Dickens, S.H.; Stansbury, J.W.; Choi, K.M.; Floyd, C.J.E. Photopolymerization Kinetics of Methacrylate Dental Resins. Macromolecules 2003, 36, 6043–6053. [Google Scholar] [CrossRef]
- Moszner, N.; Fischer, U.K.; Angermann, J. New Diluents for Dental Composites. Macromol. Mater. Eng. 2016, 301, 750–759. [Google Scholar] [CrossRef]
- Pérez-Mondragón, A.A.; Cuevas-Suárez, C.E.; González-López, J.A.; Trejo-Carbajal, N.; Meléndez-Rodríguez, M.; Herrera-González, A.M. Preparation and evaluation of a BisGMA-free dental composite resin based on a novel trimethacrylate monomer. Dent. Mater. 2020, 36, 542–550. [Google Scholar] [CrossRef]
- He, J.; Kopperud, H.M. Preparation and characterization of Bis-GMA-free dental composites with dimethacrylate monomer derived from 9,9-Bis [4-(2-hydroxyethoxy)phenyl]fluorene. Dent. Mater. 2018, 34, 1003–1013. [Google Scholar] [CrossRef]
- Yoshinaga, K.; Yoshihara, K.; Yoshida, Y. Development of new diacrylate monomers as substitutes for Bis-GMA and UDMA. Dent. Mater. 2021, 37, e391–e398. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Mondragón, A.A.; Cuevas-Suárez, C.E.; Suárez Castillo, O.R.; González-López, J.A.; Herrera-González, A.M. Evaluation of biocompatible monomers as substitutes for TEGDMA in resin-based dental composites. Mater. Sci. Eng. C 2018, 93, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Yu, X.; Liu, F.; Deng, F.; He, J. Synthesis of antibacterial dimethacrylate derived from niacin and its application in preparing antibacterial dental resin system. J. Mech. Behav. Biomed. Mater. 2020, 102, 103521. [Google Scholar] [CrossRef]
- Zhang, L.; Ma, Z.; Wang, R.; Zhu, M. Synthesis and Characterization of Methacrylate-Functionalized Betulin Derivatives as Antibacterial Comonomer for Dental Restorative Resins. ACS Biomater. Sci. Eng. 2021, 7, 3132–3140. [Google Scholar] [CrossRef]
- Sun, Y.; Zhou, Z.; Jiang, H.; Duan, Y.; Li, J.; Liu, X.; Hong, L.; Zhao, C. Preparation and evaluation of novel bio-based Bis-GMA-free dental composites with low estrogenic activity. Dent. Mater. 2022, 38, 281–293. [Google Scholar] [CrossRef]
- Zhang, L.; Ma, Z.; Wang, R.; Zuo, W.; Zhu, M. Bis-quaternary ammonium betulin-based dimethacrylate: Synthesis, characterization, and application in dental restorative resins. Mater. Adv. 2023, 4, 2127–2137. [Google Scholar] [CrossRef]
- Lai, H.; Zhang, J.; Xiao, P. Renewable Photopolymers: Transformation of Biomass Resources into Value-Added Products Under Light. ACS Sustain. Chem. Eng. 2023, 11, 16365–16406. [Google Scholar] [CrossRef]
- Folwaczny, M.; Ahantab, R.; Kessler, A.; Ern, C.; Frasheri, I. Cytotoxicity of 3D printed resin materials for temporary restorations on human periodontal ligament (PDL-hTERT) cells. Dent. Mater. 2023, 39, 529–537. [Google Scholar] [CrossRef]
- Pantea, M.; Ciocoiu, R.C.; Greabu, M.; Ripszky Totan, A.; Imre, M.; Țâncu, A.M.C.; Sfeatcu, R.; Spînu, T.C.; Ilinca, R.; Petre, A.E. Compressive and Flexural Strength of 3D-Printed and Conventional Resins Designated for Interim Fixed Dental Prostheses: An In Vitro Comparison. Materials 2022, 15, 3075. [Google Scholar] [CrossRef]
- Alshamrani, A.A.; Raju, R.; Ellakwa, A. Effect of Printing Layer Thickness and Postprinting Conditions on the Flexural Strength and Hardness of a 3D-Printed Resin. Biomed Res. Int. 2022, 2022, 8353137. [Google Scholar] [CrossRef]
- Palavicini, J.; Quin, S.L.; Zakkour, W.; Zakkour, K.; Manafi Varkiani, S.; Xu, X.; Lawson, N.C.; Nejat, A.H. Bond Strength of Reline Materials to 3D-Printed Provisional Crown Resins. Polymers 2023, 15, 3745. [Google Scholar] [CrossRef] [PubMed]
- Kwang, Y.; Ronald, L.E.; Steven, R.A.; Terry, L.; David, G.G.; Fang, Q. In vitro evaluation of the marginal integrity of CAD/CAM interim crowns. J. Prosthet. Dent. 2016, 115, 617–623. [Google Scholar]
- Yao, J.; Li, J.; Wang, Y.; Huang, H. Comparison of the flexural strength and marginal accuracy of traditional and CAD/CAM interim materials before and after thermal cycling. J. Prosthet. Dent. 2014, 112, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Mudhaffer, S.; Haider, J.; Satterthwaite, J.; Silikas, N. Effects of print orientation and artificial aging on the flexural strength and flexural modulus of 3D printed restorative resin materials. J. Prosthet. Dent. 2024, 133, 1345–1357. [Google Scholar] [CrossRef]
- ISO 4049:2019; Dentistry—Polymer-Based Restorative Materials. ISO: Geneva, Switzerland, 2019.
- Rayyan, M.M.; Aboushelib, M.; Sayed, N.M.; Ibrahim, A.; Jimbo, R. Comparison of interim restorations fabricated by CAD/CAM with those fabricated manually. J. Prosthet. Dent. 2015, 114, 414–419. [Google Scholar] [CrossRef]
- Christensen, G.J. Provisional restorations for fixed prosthodontics. J. Am. Dent. Assoc. 1996, 127, 249–252. [Google Scholar] [CrossRef]
- Martu, I.; Murariu, A.; Baciu, E.R.; Savin, C.N.; Foia, I.; Tatarciuc, M.; Diaconu-Popa, D. An Interdisciplinary Study Regarding the Characteristics of Dental Resins Used for Temporary Bridges. Medicina 2022, 58, 811. [Google Scholar] [CrossRef]
- Park, S.-M.; Park, J.-M.; Kim, S.-K.; Heo, S.-J.; Koak, J.-Y. Flexural Strength of 3D-Printing Resin Materials for Provisional Fixed Dental Prostheses. Materials 2020, 13, 3970. [Google Scholar] [CrossRef]
- Al-Qahtani, A.S.; Tulbah, H.I.; Binhasan, M.; Abbasi, M.S.; Ahmed, N.; Shabib, S.; Farooq, I.; Aldahian, N.; Nisar, S.S.; Tanveer, S.A.; et al. Surface Properties of Polymer Resins Fabricated with Subtractive and Additive Manufacturing Techniques. Polymers 2021, 13, 4077. [Google Scholar] [CrossRef]
- Tasin, S.; Ismatullaev, A. Comparative evaluation of the effect of thermocycling on the mechanical properties of conventionally polymerized, CAD-CAM milled, and 3D-printed interim materials. J. Prosthet. Dent. 2022, 127, 173.e1–173.e8. [Google Scholar] [CrossRef]
- Simoneti, D.M.; Pereira-Cenci, T.; dos Santos, M.B.F. Comparison of material properties and biofilm formation in interim single crowns obtained by 3D printing and conventional methods. J. Prosthet. Dent. 2022, 127, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Ellakany, P.; Fouda, S.M.; Mahrous, A.A.; AlGhamdi, M.A.; Aly, N.M. Influence of CAD/CAM Milling and 3D-Printing Fabrication Methods on the Mechanical Properties of 3-Unit Interim Fixed Dental Prosthesis after Thermo-Mechanical Aging Process. Polymers 2022, 14, 4103. [Google Scholar] [CrossRef] [PubMed]
- Reeponmaha, T.; Angwaravong, O.; Angwarawong, T. Comparison of fracture strength after thermo-mechanical aging between provisional crowns made with CAD/CAM and conventional method. J. Adv. Prosthodont. 2020, 12, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.; Chugh, A.; Kumar, A.; Rathee, M.; Jain, P. Comparative evaluation of fracture resistance of anterior provisional restorations fabricated using conventional and digital techniques—An in vitro study. J. Indian Prosthodont. Soc. 2022, 22, 361–367. [Google Scholar]
- Martín-Ortega, N.; Sallorenzo, A.; Casajús, J.; Cervera, A.; Revilla-León, M.; Gómez-Polo, M. Fracture resistance of additive manufactured and milled implant-supported interim crowns. J. Prosthet. Dent. 2022, 127, 267–274. [Google Scholar] [CrossRef]
- Majed, M.A. Influence of aging process and restoration thickness on the fracture resistance of provisional crowns: A comparative study. Saudi Dent. J. 2023, 35, 939–945. [Google Scholar]
- Abad-Coronel, C.; Bravo, M.; Tello, S.; Cornejo, E.; Paredes, Y.; Paltan, C.A.; Fajardo, J.I. Fracture Resistance Comparative Analysis of Milled-Derived vs. 3D-Printed CAD/CAM Materials for Single-Unit Restorations. Polymers 2023, 15, 3773. [Google Scholar] [CrossRef]
- Revilla-León, M.; Morillo, J.A.; Att, W.; Özcan, M. Chemical Composition, Knoop Hardness, Surface Roughness, and Adhesion Aspects of Additively Manufactured Dental Interim Materials. J. Prosthodont. 2021, 30, 698–705. [Google Scholar] [CrossRef]
- Soto-Montero, J.; de Castro, E.F.; Romano, B.d.C.; Nima, G.; Shimokawa, C.A.K.; Giannini, M. Color alterations, flexural strength, and microhardness of 3D printed resins for fixed provisional restoration using different post-curing times. Dent. Mater. 2022, 38, 1271–1282. [Google Scholar] [CrossRef]
- Bayarsaikhan, E.; Lim, J.-H.; Shin, S.-H.; Park, K.-H.; Park, Y.-B.; Lee, J.-H.; Kim, J.-E. Effects of Postcuring Temperature on the Mechanical Properties and Biocompatibility of Three-Dimensional Printed Dental Resin Material. Polymers 2021, 13, 1180. [Google Scholar] [CrossRef]
- Mayer, J.; Stawarczyk, B.; Vogt, K.; Hickel, R.; Edelhoff, D.; Reymus, M. Influence of cleaning methods after 3D printing on two-body wear and fracture load of resin-based temporary crown and bridge material. Clin. Oral Investig. 2021, 25, 5987–5996. [Google Scholar] [CrossRef] [PubMed]
- Aldahian, N.; Khan, R.; Mustafa, M.; Vohra, F.; Alrahlah, A. Influence of Conventional, CAD-CAM, and 3D Printing Fabrication Techniques on the Marginal Integrity and Surface Roughness and Wear of Interim Crowns. Appl. Sci. 2021, 11, 8964. [Google Scholar] [CrossRef]
- Kessler, A.; Reymus, M.; Hickel, R.; Kunzelmann, K.-H. Three-body wear of 3D printed temporary materials. Dent. Mater. 2019, 35, 1805–1812. [Google Scholar] [CrossRef] [PubMed]
- Digholkar, S.; Madhav, V.N.V.; Palaskar, J. Evaluation of the flexural strength and microhardness of provisional crown and bridge materials fabricated by different methods. J. Indian Prosthodont. Soc. 2016, 16, 328–334. [Google Scholar]
- Reymus, M.; Fabritius, R.; Keßler, A.; Hickel, R.; Edelhoff, D.; Stawarczyk, B. Fracture load of 3D-printed fixed dental prostheses compared with milled and conventionally fabricated ones: The impact of resin material, build direction, post-curing, and artificial aging—An in vitro study. Clin. Oral Investig. 2020, 24, 701–710. [Google Scholar] [CrossRef]
- KeßLer, A.; Hickel, R.; Ilie, N. In vitro investigation of the influence of printing direction on the flexural strength, flexural modulus and fractographic analysis of 3D-printed temporary materials. Dent. Mater. J. 2021, 40, 641–649. [Google Scholar] [CrossRef]
- Lee, E.-H.; Ahn, J.-S.; Lim, Y.-J.; Kwon, H.-B.; Kim, M.-J. Effect of layer thickness and printing orientation on the color stability and stainability of a 3D-printed resin material. J. Prosthet. Dent. 2022, 127, 784.e1–784.e7. [Google Scholar] [CrossRef]
- Scherer, M.; Husain, N.A.-H.; Barmak, A.B.; Kois, J.C.; Oezcan, M.; Revilla-Leon, M. Influence of the layer thickness on the flexural strength of aged and nonaged additively manufactured interim dental material. J. Prosthodont. 2023, 32 (Suppl. S2), 68–73. [Google Scholar] [CrossRef]
- Turksayar, A.A.D.; Donmez, M.B.; Olcay, E.O.; Demirel, M.; Demir, E. Effect of printing orientation on the fracture strength of additively manufactured 3-unit interim fixed dental prostheses after aging. J. Dent. 2022, 124, 104155. [Google Scholar] [CrossRef]
- Unkovskiy, A.; Bui, P.H.-B.; Schille, C.; Geis-Gerstorfer, J.; Huettig, F.; Spintzyk, S. Objects build orientation, positioning, and curing influence dimensional accuracy and flexural properties of stereolithographically printed resin. Dent. Mater. 2018, 34, e324–e333. [Google Scholar] [CrossRef]
- ISO 10993-1:2018; Biological Evaluation of Medical Devices—Part 1: Evaluation and Testing Within a Risk Management Process. ISO: Geneva, Switzerland, 2018.
- Chen, H.; Hou, J.P.; Lee, S.-Y.; Lin, Y.M. Effects of postpolymerization time and temperature on the flexural properties and hardness profile of three-dimensional printed provisional resin. J. Dent. Sci. 2024, 19, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Crispim, A.H.T.; da Silva, S.E.G.; de Gois Moreira, F.G.; da Silva, B.C.D.; de Medeiros, P.J.G.L.; de Assunção e Souza, R.O. Influence of build direction, post-polymerization time, and aging on the fracture resistance and marginal and internal discrepancies of three-dimensional printed provisional crowns. Odontology 2024, 113, 619–633. [Google Scholar] [CrossRef] [PubMed]
- ISO 10477:2020; Dentistry—Polymer-Based Crown and Veneering Materials. ISO: Geneva, Switzerland, 2020.
- Rexhepi, I.; Santilli, M.; D’Addazio, G.; Tafuri, G.; Manciocchi, E.; Caputi, S.; Sinjari, B. Clinical Applications and Mechanical Properties of CAD-CAM Materials in Restorative and Prosthetic Dentistry: A Systematic Review. J. Funct. Biomater. 2023, 14, 431. [Google Scholar] [CrossRef] [PubMed]
- Reymus, M.; Stawarczyk, B. Influence of Different Postpolymerization Strategies and Artificial Aging on Hardness of 3D-Printed Resin Materials: An In Vitro Study. Int. J. Prosthodont. 2020, 33, 634–640. [Google Scholar] [CrossRef]
- Da Silva, T.M.; Immich, F.; Araujo, T.S.D.; Lund, R.G.; Silva, A.F.D.; Piva, E.; Rosa, W.L.D.O.D. Photosensitive resins used in additive manufacturing for oral application in dentistry: A scoping review from lab to clinic. J. Mech. Behav. Biomed. Mater. 2023, 141, 105732. [Google Scholar] [CrossRef]
- Palin, W.M.; Fleming, G.J.P.; Burke, F.J.T.; Marquis, P.M.; Pintado, M.R.; Randall, R.C.; Douglas, W.H. The frictional coefficients and associated wear resistance of novel low-shrink resin-based composites. Dent. Mater. 2005, 21, 1111–1118. [Google Scholar] [CrossRef]
- Snarski-Adamski, A.; Pieniak, D.; Krzysiak, Z.; Firlej, M.; Brumerčík, F. Evaluation of the Tribological Behavior of Materials Used for the Production of Orthodontic Devices in 3D DLP Printing Technology, Due to Oral Cavity Environmental Factors. Materials 2025, 18, 301. [Google Scholar] [CrossRef]
- Mangal, U.; Min, Y.J.; Seo, J.-Y.; Kim, D.-E.; Cha, J.-Y.; Lee, K.-J.; Kwon, J.-S.; Choi, S.-H. Changes in tribological and antibacterial properties of poly(methyl methacrylate)-based 3D-printed intra-oral appliances by incorporating nanodiamonds. J. Mech. Behav. Biomed. Mater. 2020, 110, 103992. [Google Scholar] [CrossRef]
- Firlej, M.; Pieniak, D.; Niewczas, A.M.; Walczak, A.; Domagała, I.; Borucka, A.; Przystupa, K.; Igielska-Kalwat, J.; Jarosz, W.; Biedziak, B. Effect of Artificial Aging on Mechanical and Tribological Properties of CAD/CAM Composite Materials Used in Dentistry. Materials 2021, 14, 4678. [Google Scholar] [CrossRef]
- Alhareb, A.O.; Ahmad, Z.A. Effect of Al2O3/ZrO2 reinforcement on the mechanical properties of PMMA denture base. J. Reinf. Plast. Compos. 2011, 30, 86–93. [Google Scholar] [CrossRef]
- Persson, C.; Unosson, E.; Ajaxon, I.; Engstrand, J.; Engqvist, H.; Xia, W. Nano grain sized zirconia–silica glass ceramics for dental applications. J. Eur. Ceram. Soc. 2012, 32, 4105–4110. [Google Scholar] [CrossRef]
- El-Tamimi, K.M.; Bayoumi, D.A.; Ahmed, M.M.Z.; Albaijan, I.; El-Sayed, M.E. The Effect of Salinized Nano ZrO2 Particles on the Microstructure, Hardness, and Wear Behavior of Acrylic Denture Tooth Nanocomposite. Polymers 2022, 14, 302. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Kumar, V.; Kumar, R.; Kumar, R.; Pruncu, C.I. Fabrication and characterization of ZrO2 incorporated SiO2–CaO–P2O5 bioactive glass scaffolds. J. Mech. Behav. Biomed. Mater. 2020, 109, 103854. [Google Scholar] [CrossRef] [PubMed]
- Kj, A. Phillips’ science of dental materials. St. Louis WB Saunders 2003, 596, 41–43. [Google Scholar]
- Sun, L.; Gibson, R.F.; Gordaninejad, F.; Suhr, J. Energy absorption capability of nanocomposites: A review. Compos. Sci. Technol. 2009, 69, 2392–2409. [Google Scholar] [CrossRef]
- Taormina, G.; Sciancalepore, C.; Messori, M.; Bondioli, F. 3D printing processes for photocurable polymeric materials: Technologies, materials, and future trends. J. Appl. Biomater. Funct. Mater. 2018, 16, 151–160. [Google Scholar] [CrossRef]
- Lim, B.-S.; Ferracane, J.L.; Condon, J.R.; Adey, J.D. Effect of filler fraction and filler surface treatment on wear of microfilled composites. Dent. Mater. 2002, 18, 1–11. [Google Scholar] [CrossRef]
- Bayne, S.C.; Taylor, D.F.; Heymann, H.O. Protection hypothesis for composite wear. Dent. Mater. 1992, 8, 305–309. [Google Scholar] [CrossRef]
- Kumar, S.R.; Patnaik, A.; Bhat, I.K. Factors influencing mechanical and wear performance of dental composite: A review. Mater. Werkst. 2020, 51, 96–108. [Google Scholar] [CrossRef]
- Hu, X.; Marquis, P.M.; Shortall, A.C. Influence of filler loading on the two-body wear of a dental composite. J. Oral Rehabil. 2003, 30, 729–737. [Google Scholar] [CrossRef]
- Hatim, N.; Taqa, A.; Razzak, S.A. Evaluation of the effect of temperature and time on the conversion factor of acrylic resin denture base material. Al-Rafidain Dent. J. 2011, 11, 67–79. [Google Scholar] [CrossRef]
- El-Nawawy, M.; Koraitim, L.; Abouelatta, O.; Hegazi, H. Depth of cure and microhardness of nanofilled, packable and hybrid dental composite resins. Am. J. Biomed. Eng. 2012, 2, 241–250. [Google Scholar] [CrossRef][Green Version]
- Bablani, M.; Bagchi, A. Quantification of errors in rapid prototyping processes, and determination of preferred orientation of parts. Trans.-N. Am. Manuf. Res. Inst. SME 1995, 319–324. [Google Scholar]
- Vega, V.; Clements, J.; Lam, T.; Abad, A.; Fritz, B.; Ula, N.; Es-Said, O.S. The Effect of Layer Orientation on the Mechanical Properties and Microstructure of a Polymer. J. Mater. Eng. Perform. 2011, 20, 978–988. [Google Scholar] [CrossRef]
- Chladek, G.; Basa, K.; Żmudzki, J.; Malara, P.; Nowak, A.J.; Kasperski, J. Influence of aging solutions on wear resistance and hardness of selected resin-based dental composites. Acta Bioeng. Biomech. 2016, 18, 43–52. [Google Scholar]
- Wu, D.; Zhao, Z.; Zhang, Q.; Qi, H.J.; Fang, D. Mechanics of shape distortion of DLP 3D printed structures during UV post-curing. Soft Matter 2019, 15, 6151–6159. [Google Scholar] [CrossRef]
- Li, P.; Lambart, A.-L.; Stawarczyk, B.; Reymus, M.; Spintzyk, S. Postpolymerization of a 3D-printed denture base polymer: Impact of post-curing methods on surface characteristics, flexural strength, and cytotoxicity. J. Dent. 2021, 115, 103856. [Google Scholar] [CrossRef]
- Kim, D.; Shim, J.-S.; Lee, D.; Shin, S.-H.; Nam, N.-E.; Park, K.-H.; Shim, J.-S.; Kim, J.-E. Effects of Post-Curing Time on the Mechanical and Color Properties of Three-Dimensional Printed Crown and Bridge Materials. Polymers 2020, 12, 2762. [Google Scholar] [CrossRef]
- Oskui, S.M.; Diamante, G.; Liao, C.; Shi, W.; Gan, J.; Schlenk, D.; Grover, W.H. Assessing and Reducing the Toxicity of 3D-Printed Parts. Environ. Sci. Technol. Lett. 2016, 3, 1–6. [Google Scholar] [CrossRef]
- Burke, F.J.T. Fracture resistance of teeth restored with dentin-bonded crowns constructed in a leucite-reinforced ceramic. Dent. Mater. 1999, 15, 359–362. [Google Scholar] [CrossRef]
- Abo-Elsoud, A.A.E.; Mohamady, E.M.; Fathi Abdou, N.E.-S. Thermomechanical aging effects on vertical marginal gap and fracture resistance: A comparative study of Bioflx and traditional pediatric crowns. BMC Oral Health 2024, 24, 1334. [Google Scholar] [CrossRef] [PubMed]
- Yildirim, M.; Aykent, F.; Ozdogan, M.S. Comparison of fracture strength, surface hardness, and color stain of conventionally fabricated, 3D printed, and CAD-CAM milled interim prosthodontic materials after thermocycling. J. Adv. Prosthodont. 2024, 16, 115–125. [Google Scholar] [CrossRef] [PubMed]
- Alalawi, H.; Al-Qanas, S.; Al-Ghamdi, S.; Al-Fuhaid, R.; Khan, S.; Alghamdi, M.A.; Almulhim, K.S.; Aljofi, F.E.; Khan, Z.A.; Al-Dulaijan, Y.A. Effect of Dietary Simulating Solvents on the CAD-CAM Provisional Restorative Materials’ Microhardness and Color Stability Properties: An in vitro Study. Clin. Cosmet. Investig. Dent. 2024, 16, 237–248. [Google Scholar] [CrossRef]
- Burns, D.R.; Beck, D.A.; Nelson, S.K. A review of selected dental literature on contemporary provisional fixed prosthodontic treatment: Report of the Committee on Research in Fixed Prosthodontics of the Academy of Fixed Prosthodontics. J. Prosthet. Dent. 2003, 90, 474–497. [Google Scholar] [CrossRef]
- Al-Akhali, A.A.-R.M.; Al-Hamzi, M.; Al-Shami, I.Z.; Al-Kholani, A.I.; Madfa, A.A. Effect of khat extract on color stability of digitally and manually fabricated provisional restorations: An in vitro comparative study. BMC Oral Health 2023, 23, 700. [Google Scholar] [CrossRef]
- Almejrad, L.; Yang, C.-C.; Morton, D.; Lin, W.-S. The Effects of Beverages and Surface Treatments on the Color Stability of 3D-Printed Interim Restorations. J. Prosthodont. 2022, 31, 165–170. [Google Scholar] [CrossRef]
- Zhang, S.; Liu, F.; He, J. Enhanced anti-bacterial adhesion effect of FDMA/SR833s based dental resin composites by using 1H,1H-heptafluorobutyl methacrylate as partial diluent. Biomater. Investig. Dent. 2023, 10, 2281090. [Google Scholar] [CrossRef]
- Liang, X.; Huang, Q.; Liu, F.; He, J.; Lin, Z. Synthesis of novel antibacterial monomers (UDMQA) and their potential application in dental resin. J. Appl. Polym. Sci. 2013, 129, 3373–3381. [Google Scholar] [CrossRef]
- Leung, B.A.-y.; Joe, W.; Mofarah, S.S.; Sorrell, C.C.; Abbasi, R.; Azadeh, M.; Arsecularatne, J.A.; Koshy, P. Unveiling the mechanisms behind surface degradation of dental resin composites in simulated oral environments. J. Mater. Chem. B 2023, 11, 7707–7720. [Google Scholar] [CrossRef]
- Ferracane, J.L. Resin composite—State of the art. Dent. Mater. 2011, 27, 29–38. [Google Scholar] [CrossRef]
- Duarte, S., Jr.; Phark, J.-H. Advances in Dental Restorations: A Comprehensive Review of Machinable and 3D-Printed Ceramic-Reinforced Composites. J. Esthet. Restor. Dent. 2024, 37, 257–276. [Google Scholar] [CrossRef] [PubMed]
- Sideridou, I.; Tserki, V.; Papanastasiou, G. Study of water sorption, solubility and modulus of elasticity of light-cured dimethacrylate-based dental resins. Biomaterials 2003, 24, 655–665. [Google Scholar] [CrossRef] [PubMed]
- Greil, V.; Mayinger, F.; Reymus, M.; Stawarczyk, B. Water sorption, water solubility, degree of conversion, elastic indentation modulus, edge chipping resistance and flexural strength of 3D-printed denture base resins. J. Mech. Behav. Biomed. Mater. 2023, 137, 105565. [Google Scholar] [CrossRef]
- Perea-Lowery, L.; Gibreel, M.; Vallittu, P.K.; Lassila, L.V. 3D-Printed vs. Heat-Polymerizing and Autopolymerizing Denture Base Acrylic Resins. Materials 2021, 14, 5781. [Google Scholar] [CrossRef]
- Barsby, M.J. A denture base resin with low water absorption. J. Dent. 1992, 20, 240–244. [Google Scholar] [CrossRef]
- Alsandi, Q.; Ikeda, M.; Arisaka, Y.; Nikaido, T.; Tsuchida, Y.; Sadr, A.; Yui, N.; Tagami, J. Evaluation of Mechanical and Physical Properties of Light and Heat Polymerized UDMA for DLP 3D Printer. Sensors 2021, 21, 3331. [Google Scholar] [CrossRef]
- Toledano, M.; Osorio, R.; Osorio, E.; Fuentes, V.; Prati, C.; García-Godoy, F. Sorption and solubility of resin-based restorative dental materials. J. Dent. 2003, 31, 43–50. [Google Scholar] [CrossRef]
- Pfeiffer, P.; Rosenbauer, E.-U. Residual methyl methacrylate monomer, water sorption, and water solubility of hypoallergenic denture base materials. J. Prosthet. Dent. 2004, 92, 72–78. [Google Scholar] [CrossRef]
- Sayed, M.E.; Reddy, N.K.; Reddy, N.R.; Mattoo, K.A.; Jad, Y.A.; Hakami, A.J.; Hakami, A.K.; Dighriri, A.M.; Hurubi, S.Y.; Hamdi, B.A.; et al. Evaluation of the Milled and ThreeDimensional Digital Manufacturing, 10-Degree and 20-Degree Preparation Taper, Groove and Box Auxiliary Retentive Features, and Conventional and Resin-Based Provisional Cement Type on the Adhesive Failure Stress of 3 mm Short Provisional Crowns. Med. Sci. Monit. 2024, 30, e943237-1. [Google Scholar]
- Sasany, R.; Jamjoom, F.Z.; Kendirci, M.Y.; Yilmaz, B. Effect of Printing Layer Thickness on Optical Properties and Surface Roughness of 3D-Printed Resins: An In Vitro Study. Int. J. Prosthodont. 2024, 37, S165–S173. [Google Scholar] [CrossRef]
- Shin, J.-W.; Kim, J.-E.; Choi, Y.-J.; Shin, S.-H.; Nam, N.-E.; Shim, J.-S.; Lee, K.-W. Evaluation of the Color Stability of 3D-Printed Crown and Bridge Materials against Various Sources of Discoloration: An In Vitro Study. Materials 2020, 13, 5359. [Google Scholar] [CrossRef] [PubMed]
- Karaokutan, I.; Sayin, G.; Kara, O. In vitro study of fracture strength of provisional crown materials. J. Adv. Prosthodont. 2015, 7, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Perea-Lowery, L.; Gibreel, M.; Vallittu, P.K.; Lassila, L. Characterization of the mechanical properties of CAD/CAM polymers for interim fixed restorations. Dent. Mater. J. 2020, 39, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Wadhwani, V.; Sivaswamy, V.; Rajaraman, V. Surface roughness and marginal adaptation of stereolithography versus digital light processing three-dimensional printed resins: An in-vitro study. J. Indian Prosthodont. Soc. 2022, 22, 377–381. [Google Scholar]
- Mohajeri, M.; Khazaei, S.; Vafaee, F.; Firouz, F.; Ghorbani Gholiabad, S.; Shisheian, A. Marginal Fit of Temporary Restorations Fabricated by the Conventional Chairside Method, 3D Printing, and Milling. Front. Dent. 2021, 18, 31. [Google Scholar] [CrossRef]
- van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef]
- Baig, M.R.; Tan, K.B.-C.; Nicholls, J.I. Evaluation of the marginal fit of a zirconia ceramic computer-aided machined (CAM) crown system. J. Prosthet. Dent. 2010, 104, 216–227. [Google Scholar] [CrossRef]
- Kokubo, Y.; Ohkubo, C.; Tsumita, M.; Miyashita, A.; von Steyern, P.V.; Fukushima, S. Clinical marginal and internal gaps of Procera AllCeram crowns. J. Oral Rehabil. 2005, 32, 526–530. [Google Scholar] [CrossRef]
- Al Wadei, M.H.D.; Sayed, M.E.; Jain, S.; Aggarwal, A.; Alqarni, H.; Gupta, S.G.; Alqahtani, S.M.; Alahmari, N.M.; Alshehri, A.H.; Jain, M.; et al. Marginal Adaptation and Internal Fit of 3D-Printed Provisional Crowns and Fixed Dental Prosthesis Resins Compared to CAD/CAM-Milled and Conventional Provisional Resins: A Systematic Review and Meta-Analysis. Coatings 2022, 12, 1777. [Google Scholar] [CrossRef]
- Cakmak, G.; Cuellar, A.R.; Donmez, M.B.; Schimmel, M.; Abou-Ayash, S.; Lu, W.-E.; Yilmaz, B. Effect of Printing Layer Thickness on the Trueness and Margin Quality of 3D-Printed Interim Dental Crowns. Appl. Sci. 2021, 11, 9246. [Google Scholar] [CrossRef]
- Ahlholm, P.; Sipila, K.; Tarvonen, P.-L.; Silvast, T.; Lappalainen, R. Accuracy of Dental Restorations Fabricated Using Milling vs 3D-Printed Molds: A Pilot Study. Int. J. Prosthodont. 2024, 37, S79–S88. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, N.; Alharbi, S.; Cuijpers, V.M.J.I.; Osman, R.B.; Wismeijer, D. Three-dimensional evaluation of marginal and internal fit of 3D-printed interim restorations fabricated on different finish line designs. J. Prosthodont. Res. 2018, 62, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Chaturvedi, S.; Alqahtani, N.M.; Addas, M.K.; Alfarsi, M.A. Marginal and internal fit of provisional crowns fabricated using 3D printing technology. Technol. Health Care 2020, 28, 635–642. [Google Scholar] [CrossRef] [PubMed]
- Othman, A.; Sandmair, M.; Alevizakos, V.; von See, C. The fracture resistance of 3D-printed versus milled provisional crowns: An in vitro study. PLoS ONE 2023, 18, e0285760. [Google Scholar] [CrossRef]
- Peng, C.-C.; Chung, K.-H.; Yau, H.-T.; Ramos, V. Assessment of the internal fit and marginal integrity of interim crowns made by different manufacturing methods. J. Prosthet. Dent. 2020, 123, 514–522. [Google Scholar] [CrossRef]
- Lee, W.-S.; Lee, D.-H.; Lee, K.-B. Evaluation of internal fit of interim crown fabricated with CAD/CAM milling and 3D printing system. J. Adv. Prosthodont. 2017, 9, 265–270. [Google Scholar] [CrossRef]
- Martins, L.M.; Lorenzoni, F.C.; de Melo, A.O.; da Silva, L.M.; de Oliveira, J.L.G.; de Oliveira, P.C.G.; Bonfante, G. Internal fit of two all-ceramic systems and metal-ceramic crowns. J. Appl. Oral Sci. 2012, 20, 235–240. [Google Scholar] [CrossRef]
- Soto-Montero, J.; Romano, B.d.C.; Noronha, M.d.S.; Andre, C.B.; Giannini, M. Microtensile bond strength of resin cements to 3-D printed and milled temporary restorative resins. Odovtos Int. J. Dent. Sci. 2023, 25, 82–98. [Google Scholar] [CrossRef]
- Ahmed, A.A.; Hassan, M.M.; Abdalla, A.I. Microshear bond strength of universal adhesives to dentin used in total-etch and self-etch modes. Tanta Dent. J. 2018, 15, 91–98. [Google Scholar] [CrossRef]
- Al Aali, K.; Alhamdan, R.; Maawadh, A.M.; Vohra, F.; Abduljabbar, T. Influence of contemporary CAD-CAM milling systems on the fit and adaptation of partially stabilized Zirconia fixed partial dentures. Pak. J. Med. Sci. 2020, 37, 45. [Google Scholar] [CrossRef]
- Kim, S.H.; Watts, D.C. Polymerization shrinkage-strain kinetics of temporary crown and bridge materials. Dent. Mater. 2004, 20, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Riccitiello, F.; Amato, M.; Leone, R.; Spagnuolo, G.; Sorrentino, R. In vitro evaluation of the marginal fit and internal adaptation of zirconia and lithium disilicate single crowns: Micro-CT comparison between different manufacturing procedures. Open Dent. J. 2018, 12, 160–172. [Google Scholar] [CrossRef] [PubMed]
- Givens Jr, E.J.; Neiva, G.; Yaman, P.; Dennison, J.B. Marginal Adaptation and Color Stability of Four Provisional Materials. J. Prosthodont. 2008, 17, 97–101. [Google Scholar] [CrossRef] [PubMed]
- Karaoğlanoğlu, S.; Aydın, N.; Oktay, E.; Ersöz, B. Comparison of the Surface Properties of 3D-printed Permanent Restorative Resins and Resin-based CAD/CAM Blocks. Oper. Dent. 2023, 48, 588–598. [Google Scholar] [CrossRef]
- HAMOUDA, I.M. Effects of Various Beverages on Hardness, Roughness, and Solubility of Esthetic Restorative Materials. J. Esthet. Restor. Dent. 2011, 23, 315–322. [Google Scholar] [CrossRef]
- Buergers, R.; Rosentritt, M.; Handel, G. Bacterial adhesion of Streptococcus mutans to provisional fixed prosthodontic material. J. Prosthet. Dent. 2007, 98, 461–469. [Google Scholar] [CrossRef]
- Neppelenbroek, K.H.; Kuroishi, E.; Hotta, J.; Marques, V.R.; Moffa, E.B.; Soares, S.; Urban, V.M. Surface properties of multilayered, acrylic resin artificial teeth after immersion in staining beverages. J. Appl. Oral Sci. 2015, 23, 376–382. [Google Scholar] [CrossRef]
- Gautam, R.; Singh, R.D.; Sharma, V.P.; Siddhartha, R.; Chand, P.; Kumar, R. Biocompatibility of polymethylmethacrylate resins used in dentistry. J. Biomed. Mater. Res. Part B Appl. Biomater. 2012, 100B, 1444–1450. [Google Scholar] [CrossRef]
- Wuersching, S.N.; Hickel, R.; Edelhoff, D.; Kollmuss, M. Initial biocompatibility of novel resins for 3D printed fixed dental prostheses. Dent. Mater. 2022, 38, 1587–1597. [Google Scholar] [CrossRef]
- Rogers, H.B.; Zhou, L.T.; Kusuhara, A.; Zaniker, E.; Shafaie, S.; Owen, B.C.; Duncan, F.E.; Woodruff, T.K. Dental resins used in 3D printing technologies release ovo-toxic leachates. Chemosphere 2021, 270, 129003. [Google Scholar] [CrossRef]
- Hwangbo, N.-K.; Nam, N.-E.; Choi, J.-H.; Kim, J.-E. Effects of the Washing Time and Washing Solution on the Biocompatibility and Mechanical Properties of 3D Printed Dental Resin Materials. Polymers 2021, 13, 4410. [Google Scholar] [CrossRef] [PubMed]
- Hardiman, K. Post-processing Considerations for Biomedical 3D Printing of Polymers. In Polymer-Based Additive Manufacturing: Biomedical Applications; Devine, D.M., Ed.; Springer International Publishing: Cham, Switzerland, 2019; pp. 219–241. [Google Scholar]
- Kim, G.-T.; Go, H.-B.; Yu, J.-H.; Yang, S.-Y.; Kim, K.-M.; Choi, S.-H.; Kwon, J.-S. Cytotoxicity, Colour Stability and Dimensional Accuracy of 3D Printing Resin with Three Different Photoinitiators. Polymers 2022, 14, 979. [Google Scholar] [CrossRef] [PubMed]
- Schwengberg, S.; Bohlen, H.; Kleinsasser, N.; Kehe, K.; Seiss, M.; Walther, U.I.; Hickel, R.; Reichl, F.X. In vitro embryotoxicity assessment with dental restorative materials. J. Dent. 2005, 33, 49–55. [Google Scholar] [CrossRef]
- Atria, P.J.; Bordin, D.; Marti, F.; Nayak, V.V.; Conejo, J.; Jalkh, E.B.; Witek, L.; Sampaio, C.S. 3D-printed resins for provisional dental restorations: Comparison of mechanical and biological properties. J. Esthet. Restor. Dent. 2022, 34, 804–815. [Google Scholar] [CrossRef]
- Yang, Y.; Reichl, F.-X.; Shi, J.; He, X.; Hickel, R.; Högg, C. Cytotoxicity and DNA double-strand breaks in human gingival fibroblasts exposed to eluates of dental composites. Dent. Mater. 2018, 34, 201–208. [Google Scholar] [CrossRef]
- Yadav, R.; Meena, A.; Patnaik, A. Biomaterials for dental composite applications: A comprehensive review of physical, chemical, mechanical, thermal, tribological, and biological properties. Polym. Adv. Technol. 2022, 33, 1762–1781. [Google Scholar] [CrossRef]
- Sa, L.; Kaiwu, L.; Shenggui, C.; Junzhong, Y.; Yongguang, J.; Lin, W.; Li, R. 3D printing dental composite resins with sustaining antibacterial ability. J. Mater. Sci. 2019, 54, 3309–3318. [Google Scholar] [CrossRef]
- Pye, A.D.; Lockhart, D.E.A.; Dawson, M.P.; Murray, C.A.; Smith, A.J. A review of dental implants and infection. J. Hosp. Infect. 2009, 72, 104–110. [Google Scholar] [CrossRef]
- Huang, Q.; Huang, S.; Liang, X.; Qin, W.; Liu, F.; Lin, Z.; He, J. The antibacterial, cytotoxic, and flexural properties of a composite resin containing a quaternary ammonium monomer. J. Prosthet. Dent. 2018, 120, 609–616. [Google Scholar] [CrossRef]
- Altarazi, A.; Jadaan, L.; McBain, A.J.; Haider, J.; Kushnerev, E.; Yates, J.M.; Alhotan, A.; Silikas, N.; Devlin, H. 3D-printed nanocomposite denture base resin: The effect of incorporating TiO2 nanoparticles on the growth of Candida albicans. J. Prosthodont. 2024, 33 (Suppl. S1), 25–34. [Google Scholar] [CrossRef]
- Zhou, S.; Deng, C.; Liu, H.; Sun, Y.; Zhang, J. Investigating the antibacterial activity of Thyme Oil/TiO2 modified resins against oral pathogenic bacteria. Alex. Eng. J. 2024, 89, 195–201. [Google Scholar] [CrossRef]
- ElMalah, N.S.; Hanafy, S.A.; Osman, E.M.; Aboulgheit, S.A.; Baz, A.S. Effect of nanomodified 3D printed photopolymerizable resin on flexural strength, color, and antimicrobial efficacy: An in vitro study. J. Prosthet. Dent. 2024, 132, e1–e268. [Google Scholar] [CrossRef] [PubMed]
- Jo, Y.-H.; Cho, J.-H.; Park, D.H.; Yoon, H.-I.; Han, S.H.; Yilmaz, B. Antimicrobial activity, surface properties, and cytotoxicity of microencapsulated phytochemicals incorporated into three-dimensionally printable dental polymers. J. Dent. 2024, 141, 104820. [Google Scholar] [CrossRef]
- Bisharat, M.; Ghosal, K.; Kana’an, N.; Khamaisi, B.; Nassar-Marjiya, E.; Jindal, S.; Farah, S. Engineering fully quaternized (Dimethylamino)ethyl methacrylate-based photoresins for 3D printing of biodegradable antimicrobial polymers. Chem. Eng. J. 2024, 499, 155417. [Google Scholar] [CrossRef]
- Li, Z.; Wang, C.; Qiu, W.; Liu, R. Antimicrobial Thiol–ene–acrylate Photosensitive Resins for DLP 3D Printing. Photochem. Photobiol. 2019, 95, 1219–1229. [Google Scholar] [CrossRef]
- Wu, T.; Ding, X.; Liu, T.; Lai, G.; Zhang, X.; Chen, Q. Advancements in developing biomaterials for 3D printing photosensitive resins containing quaternary ammonium molecules for enhanced oral healthcare. Next Mater. 2024, 4, 100211. [Google Scholar] [CrossRef]
- Jin, G.; Ravichandran, V.; Shim, M.S.; Kim, J.-E. Incorporating an artificially synthesized fluoride complex into urethane-acrylate-based 3D printing resin: Effects on mechanical properties, cytotoxicity, antimicrobial actions, and its long-term fluoride-releasing properties. J. Dent. 2024, 150, 105363. [Google Scholar] [CrossRef]
- Holmer, L.; Othman, A.; Luhrs, A.-K.; von See, C. Comparison of the shear bond strength of 3D printed temporary bridges materials, on different types of resin cements and surface treatment. J. Clin. Exp. Dent. 2019, 11, e367–e372. [Google Scholar] [CrossRef]
- Yukihiro, T.; Jessica, L.; Hesham, N.; Hiroshi, H. A 3D printing replication technique for fabricating digital dentures. J. Prosthet. Dent. 2020, 124, 251–256. [Google Scholar]
- Scotti, C.K.; de Amoedo Campos Velo, M.M.; Piola Rizzante, F.A.; de Lima Nascimento, T.R.; Lia Mondelli, R.F.; Soares Bombonatti, J.F. Physical and surface properties of a 3D-printed composite resin for a digital workflow. J. Prosthet. Dent. 2020, 124, 614.e1–614.e5. [Google Scholar] [CrossRef]
- Bayarsaikhan, E.; Gu, H.; Hwangbo, N.-K.; Lim, J.-H.; Shim, J.-S.; Lee, K.-W.; Kim, J.-E. Influence of different postcuring parameters on mechanical properties and biocompatibility of 3D printed crown and bridge resin for temporary restorations. J. Mech. Behav. Biomed. Mater. 2022, 128, 105127. [Google Scholar] [CrossRef] [PubMed]
- Alzahrani, S.J.; Hajjaj, M.S.; Azhari, A.A.; Ahmed, W.M.; Yeslam, H.E.; Carvalho, R.M. Mechanical Properties of Three-Dimensional Printed Provisional Resin Materials for Crown and Fixed Dental Prosthesis: A Systematic Review. Bioengineering 2023, 10, 663. [Google Scholar] [CrossRef] [PubMed]
- Bayne, S.C. Correlation of clinical performance with ‘in vitro tests’ of restorative dental materials that use polymer-based matrices. Dent. Mater. 2012, 28, 52–71. [Google Scholar] [CrossRef] [PubMed]
- del Hougne, M.; Di Lorenzo, I.; Höhne, C.; Schmitter, M. A retrospective cohort study on 3D printed temporary crowns. Sci. Rep. 2024, 14, 17295. [Google Scholar] [CrossRef]
- Schepke, U.; Meijer, H.J.A.; Kerdijk, W.; Cune, M.S. Digital versus analog complete-arch impressions for single-unit premolar implant crowns: Operating time and patient preference. J. Prosthet. Dent. 2015, 114, 403–406. [Google Scholar] [CrossRef]
- Mangano, F.G.; Yang, K.R.; Lerner, H.; Porrà, T.; Khachatryan, L.G.; Gordienko, I.D.; Admakin, O. 3D-printed short-span hybrid composite implant-supported restorations fabricated through tilting stereolithography: A retrospective clinical study on 85 patients with 1 year of follow-up. J. Dent. 2024, 147, 105095. [Google Scholar] [CrossRef]
- Giannetti, L.; Apponi, R.; Mordini, L.; Presti, S.; Breschi, L.; Mintrone, F. The occlusal precision of milled versus printed provisional crowns. J. Dent. 2022, 117, 103924. [Google Scholar] [CrossRef]
- Xu, X.; He, L.; Zhu, B.; Li, J.; Li, J. Advances in polymeric materials for dental applications. Polym. Chem. 2017, 8, 807–823. [Google Scholar] [CrossRef]
- Tigmeanu, C.V.; Ardelean, L.C.; Rusu, L.-C.; Negrutiu, M.-L. Additive Manufactured Polymers in Dentistry, Current State-of-the-Art and Future Perspectives-A Review. Polymers 2022, 14, 3658. [Google Scholar] [CrossRef]
- Polara, G.; Pistone, F.; Alfredo, S.G. Digital immediate tooth restoration: Fabricating acrylic resin interim crowns from CBCT scans for immediate implant-supported prostheses: A case series. J. Prosthet. Dent. 2022, 127, 578–584. [Google Scholar] [CrossRef]
- Li, X.; Xie, B.; Jin, J.; Chai, Y.; Chen, Y. 3D Printing Temporary Crown and Bridge by Temperature Controlled Mask Image Projection Stereolithography. Procedia Manuf. 2018, 26, 1023–1033. [Google Scholar] [CrossRef]
- Alammar, A.; Att, W.; Beuer, F. The Accuracy of 3D-Printed Fixed Dental Restorations. J. Esthet. Restor. Dent. 2024, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Heboyan, A.; Yazdanie, N.; Ahmed, N. Glimpse into the future of prosthodontics: The synergy of artificial intelligence. World J. Clin. Cases 2023, 11, 7940–7942. [Google Scholar] [CrossRef] [PubMed]
- Alammar, A.; Kois, J.C.; Revilla-León, M.; Att, W. Additive Manufacturing Technologies: Current Status and Future Perspectives. J. Prosthodont. 2022, 31 (Suppl. S1), 4–12. [Google Scholar] [CrossRef]
- Cai, H.; Xu, X.; Lu, X.; Zhao, M.; Jia, Q.; Jiang, H.-B.; Kwon, J.-S. Dental Materials Applied to 3D and 4D Printing Technologies: A Review. Polymers 2023, 15, 2405. [Google Scholar] [CrossRef]
- Sreeramulu, D.; Venkatesh, M.; Bammidi, R.; Azad, D.; Madivada, H. Implementation of 3D and 4D Printing in Dental Applications and Future Opportunities; Recent Advances in Additive, Manufacturing; Mallaiah, M., Thapliyal, S., Chandra Bose, S., Eds.; Springer Nature: Singapore, 2025; Volume 1, pp. 129–140. [Google Scholar]



| Name | Matrix | Inorganic Fillers |
|---|---|---|
| Detax FreePrint Temp (detax, Ettlingen, Germany) | Isopropylidenediphenol Peg-2 Dimethacrylat (45-<60 wt%); HEMA (1-<5 wt%); TPO (1-<5 wt%); HPMA (1-<5 wt%); Phenyl-bis(2,4,6-trimethylbenzoyl)-phosphinoxid (<1 wt%) | Not specified |
| DWS Temporis (DWS, Thiene, Italy) | Not specified | Not specified |
| Envisiontec E-dent 100 (DeltaMed GmbH, Friedberg, Germany) | Methacrylates | May include inorganic or organic fillers |
| Envisiontec E-dent 400 (DeltaMed GmbH, Friedberg, Germany) | Methacrylates | Contains inorganic or organic fillers |
| NextDent (vertex dental) C&B (Vertex-Dental B.V., Soesterberg, The Netherlands) | Not specified | Inorganic fillers |
| NextDent (vertex dental) C&B MFH (Vertex-Dental B.V., Soesterberg, The Netherlands) | 7,7,9 (or 7,9,9)-trimethyl-4,13-dioxo-3,14-dioxa-5,12-diazahexadecane-1,16-diyl bismethacrylate; ethylene dimethacrylate; HEMA; TPO; E-BPA; mequinol; 4-methoxyphenol; hydroquinone monomethyl ether | Silicon dioxide |
| Stratasys VeroGlaze, MED620 (Stratasys, Minnetonka, MN, USA) | Acrylates | May include organic or inorganic fillers |
| 3Delta temp (Deltamed, Friedberg, Germany) | Methacrylates | Silicon dioxide; dental glass (30% vol) |
| GC temp Print (GC America Inc., Alsip, IL, USA) | UDMA(50-<75%), TEGDMA (10-<25%); 4,4′-isopropylidenediphenol, ethoxylated and 2-methylprop-2-enoic acid (2.5-<5%); TPO (1-<2.5%); 2-(2 H-benzotriazol-2-yl)-p-cresol (0.1 < 0.2%) | Quartz 10-<25% vol |
| Grandio disc (Voco, Cuxhaven, Germany) | UDMA+ DMA (14%) | Nanohybrid fillers (86% w/w) |
| Luxatemp (DMG, Hamburg, Germany) | UDMA; Aromatic dimethacrylate; Glycol methacrylate | Glass; silica filler |
| CLEAR FLGP04 (Formlabs, MA, USA) | Methacrylate oligomer (75–95%); methacrylate monomer (25–50%); and diphenyl oxide (2,4,6-trimethylbenzoyl) phosphine (<1%) | Not specified |
| Everes Temporary (Sisma, Vicenza, Italy) | Aliphatic difunctional methacrylate (<50%); 2.2-ethylenedioxydiethyl dimethacrylate (<40%); aliphatic urethane acrylate (<20%); phosphine oxide (<2.5%); and ethylenedioxydiethyl dimethacrylate (<40%) | Not specified |
| Author and Year | Studied Characteristics | Evaluated Materials | Specimen Fabrication | 3D Printing Parameters | Key Findings: |
|---|---|---|---|---|---|
| Mârtu et al. (2022) [71] | Surface roughness, mechanical strength | 1. Superpont C + B: Heat-cured PMMA 2. Zotion PMMA: Milled PMMA 3. Freeprint Temp: Methacrylate-based resin | 1. Conventional heat-curing 2. Subtractive CAD/CAM 3. Additive 3D printing | Not specified | -CAD/CAM milled PMMA exhibited highest mechanical strength -3D-printed resin showed highest initial surface roughness -All materials demonstrated significant roughness reduction post-polishing (p < 0.001) |
| Sang-Mo Park et al. (2020) [72] | Flexural strength of 3-unit fixed dental prostheses fabricated using different 3D printing technologies (DLP, SLA, FDM) versus conventional and subtractive methods | 1. CV: Jet Tooth Shade™ Powder 2. SM: ViPi block monocolor 3. DLP: NextDent C&B 4. SLA: Standard (GPGR04) 5. FDM: PLA -CV/SM/DLP/SLA: Polymethyl methacrylate (PMMA)-based resins | 1. CV: Self-cured PMMA resin 2. SM: Milled PMMA resin disk 3–4. DLP/SLA: Printed with PMMA-based photopolymer resin, post-cured 5. FDM: Printed with PLA filament (no post-curing) | -DLP/SLA: 100 μm layer thickness, 30° build angle Washed in 100% isopropyl alcohol, post-cured (DLP: 120 min; SLA: 60 min) -FDM: 200 μm layer thickness, 30° build angle | -DLP/SLA: Significantly higher flexural strength than CV group (p < 0.001) -SLA: Highest flexural strength (1323 N) -FDM: No fracture (only deformation) -DLP vs. SM: No significant difference |
| Al-Qahtani et al. 2021 [73] | Fabrication techniques for interim dental resins: CAD/CAM, 3D printing (stereolithography), heat-activated PMMA | 1. CAD/CAM: Ceramill Temp 2. 3D Printing: Freeprint Temp 3. Conventional: Jet Tooth Shade -CAD/CAM and conventional: Polymethylmethacrylate (PMMA) | 1. CAD/CAM: Milled from PMMA blanks 2. 3D Printing: SLA 3. Conventional: Heat-activated PMMA poured into molds | -Not explicitly specified -3D Printing: UV light curing (5 min in 220 V chamber) after 99% isopropyl alcohol rinse | -Surface Roughness: 3D > CAD/CAM ≈ Conventional -Microhardness: 3D > CAD/CAM ≈ Conventional -Flexural Strength: CAD/CAM ≈ 3D > Conventional |
| Pantea et al. 2022 [62] | Mechanical behavior (compressive strength, flexural strength) | 1. 3DCS: DLP NextDent C&B MFH, microfilled hybrid PMMA resin 2. 3DOS: LCD-based vat polymerization; microfilled composite PMMA-like resin 3. CAP: Duracyl 4. CHP: Superpont C + B | 1–2. 3D-printed: CAD/CAM (NextDent 5100 DLP printer, Vertex B.V., Soesterberg, The Netherlands for 3DCS; Phrozen Sonic Mini 4K LCD printer, Phrozen Technology, Xiangshan Dist., Hsinchu, Taiwan for 3DOS) 3–4 Conventional: Auto-polymerized (CAP) and pressure/heat-cured (CHP) acrylic resins | -50 μm (for 3DCS) -3DCS: 30 min UV curing at 60 °C -3DOS: 30 min UV curing | -3D-printed resins showed 2× higher elastic moduli (2.4–2.6 GPa vs. 1.3 GPa conventional) -40–88% higher bending strength in 3D-printed resins -Additive manufacturing produced more homogeneous materials compared to conventional methods |
| Tasın & Ismatullaev et al. (2022) [74] | Mechanical properties under thermal aging | 1. Auto-polymerized PMMA 2. Bis-acryl resin 3. CAD/CAM PMMA 4. 3D-printed composite resin | 1. PMMA: Manual packing 2. Bis-acryl: Injection molding 3. CAD/CAM: Milling 4. 3D-printed: SLA | -Layer thickness: 60 µm -Build orientation: 90° -Laser scanning speed: 5000 mm/s -Ultraviolet polymerization unit for 30 min | 1. Digitally fabricated materials (CAD/CAM/3D-printed) showed superior mechanical properties vs. conventional 2. But CAD/CAM/Milled had highest toughness and stability after thermocycling |
| Henderson et al. (2022) [49] | -Effects of loading rate (1 mm/min vs. 10 mm/min) -Effects of storage time (1 day vs. 30 days in 100% humidity) | 1. Milled PMMA: Solid Shade Clinical PMMA Disk (TD Dental Supply) 2. 3D-printed bis-acryl: Dentca Crown and Bridge Resin: dimethacrylate-based: bis-GMA/UDMA 3. Chairside bis-acryl: 3M-Paradigm (3M Oral Care) | 1. Milled: Subtractive CAD/CAM (Sirona inLab MC x5) 2. 3D-printed: DLP 3. Chairside: Autopolymerizing resin injection via PVS matrix | -3D-printed: Layer orientation not specified (anisotropic properties noted) -Post-processing: Manufacturer-dependent polymerization | -Milled PMMA: Highest initial failure load (729 ± 113 N at 1 day), reduced after 30 days -3D-printed bis-acryl: Lowest failure load (363–523 N), further reduced after 30 days -Chairside bis-acryl: Stable strength over 30 days -Milled PMMA’s strength advantage over chairside bis-acryl diminished after 30 days -3D-printed specimens showed anisotropic properties due to layer orientation |
| Anthony Tahayeri et al. (2018) [15] | Printing parameters (orientation, layer thickness, resin color), mechanical properties, degree of conversion | 1. 3D-Printed: NextDent C&B 2. Conventional: Integrity® (Acrylates, methacrylates, barium glass fillers), Jet® (Methyl methacrylate (MMA)) | 1. 3D-Printed: SLA 2. Conventional: Silicon mold curing (same dimensions) | -Layer thickness: 25 µm, 50 µm, 100 µm -Orientation: Optimized at 90° (reduced support usage and post-processing) | -3D-printed samples: Comparable modulus to Jet®, higher peak stress than Jet®, similar to Integrity® -Higher degree of conversion vs. conventional materials -Printing accuracy error: Up to 22% (width) |
| Simoneti et al. (2022) [75] | 3D-printed (SLA/SLS) vs. conventional (acrylic/bis-acryl resin) interim crowns | 1. Acrylic resin (Polymethyl methacrylate) 2. Bis-acryl resin (Dimethacrylates, nanoparticles) 3. SLS resin: Nylon 12 (PA2201) 4. SLA resin: Methacrylates, photoinitiators | 1–2 Conventional: Matrix-assisted elastomeric impression technique 3–4 3D-Printed: Digital design + SLA/SLS printing | -Layer thickness: Not specified -Orientation: Printed horizontally (only protocol tested) -SLA: 60 °C for 30 min via LED curing -SLS: None (per manufacturer) | -SLS: Highest flexural strength (+30% vs. conventional) -SLA: Lowest Vickers hardness and fatigue resistance (4/10 specimens fractured) -3D-printed materials: Lower elastic moduli (~50% vs. conventional) -Surface roughness: SLA ≈ bis-acryl resin (lowest); SLS = highest -No biofilm formation differences |
| Ellakany et al. (2022) [76] | -CAD/CAM milling vs. 3D printing (SLA and DLP) vs. conventional PMMA. -Effects of thermo-mechanical aging on mechanical properties | 1. Conventional: Unifast Trad, auto-polymerized PMMA 2. Milled: Telio CAD, Cross-linked PMMA 3. SLA ND: NextDent C&B MFH 4. DLP AS: ASIGA Denta Tooth, methacrylate resin | 1. Conventional: Manual mixing and molding 2. Milled: CAD/CAM milling 3–4. 3D-Printed: SLA and DLP | -Layer thickness: 50 μm -Orientation: 90° for both SLA and DLP -SLA ND: LC-D Print Box (3D Systems) for post-curing -DLP AS: Asiga Flash UV Curing Chamber | -Milled PMMA: Highest flexural strength (174.42 MPa) and microhardness (27.13 μm) -SLA ND: Comparable to milled PMMA except in elastic modulus -DLP AS: Similar to conventional PMMA |
| Reeponmaha et al. (2020) [77] | Fracture strength and patterns after thermo-mechanical aging; CAD/CAM vs. conventional methods | 1. Unifast Trad: Mono methacrylate resin 2. Protemp 4: Bis-acryl composite 3. Brylic Solid: PMMA 4. Freeprint Temp: Bis-acrylate resin | 1–2: Conventional direct 3: CAD/CAM milling 4: CAD/CAM 3D printing | -Post-printing: External surface light-cured -5000 thermocycles (5–55 °C) +100,000 occlusal cycles (100 N) | -Unifast Trad showed lowest fracture strength (657.87 N ± 82.84) -CAD/CAM and bis-acryl groups had comparable strength (953–1125 N) -Mono methacrylates showed Class I fractures vs. Class II in bis-acryls |
| Alam et al. (2022) [78] | Fracture resistance of anterior provisional crowns fabricated by different techniques | 1. Group I: Protemp 4 (Bis-acryl-based resin) 2. Group II: Dentsply Sirona PMMA disk 3. Group III: NextDent C&B Resin, methacrylate-based resin | Conventional indirect (Group I), CAD/CAM milling (Group II), 3D printing (Group III) | -Layer thickness: 50 μm -Vertical building orientation -Post-printing: 30 min curing in NextDent LC-3DPrint Box (350–550 nm wavelength) | -3D-printed crowns showed highest fracture resistance (1243.18 N ± 68.18) > CAD/CAM (960.84 N ± 37.49) > Conventional (558.85 N ± 22.33) -Post-polymerization with dedicated curing units significantly enhanced material properties in 3D-printed group |
| Martín-Ortega et al. (2022) [79] | Fracture resistance of anterior (central incisor) and posterior (premolar) screw-retained implant-supported interim crowns fabricated via subtractive (milled) and additive (DLP) manufacturing methods | 1. Milled subgroup: Vivodent CAD Multi (PMMA-based interim material) 2. Additive subgroup: Photopolymer resin, SHERAprint-cb (Rapid Shape GmbH, Heimsheim, Germany), printed with SHERAprint 30 (Rapid Shape GmbH, Heimsheim, Germany) | -Milled: 5-axis milling machine -Additive: DLP 3D printing | -Layer thickness: 50 µm -Building orientation: 45° (additive subgroup) -Ultrasonic cleaning in 98% isopropyl alcohol (2 baths), followed by UV polymerization (25 min at 220 W) | -Milled specimens exhibited significantly higher fracture resistance than additive groups (anterior: 988.4 N vs. 636.5 N; posterior: 423.8 N vs. 321.3 N) -Anterior crowns outperformed posterior crowns in both methods -All fractures occurred in crowns, not abutments |
| Majed M. Alsarani et al. (2023) [80] | -Milled vs. 3D-printed provisional crowns -Crown thickness (1.5 mm vs. 0.9 mm) -Thermal aging (5000 cycles between 5 °C and 55 °C) | 1. Milled Material: Telio CAD PMMA) 2. 3D-Printed Material: NextDent C&B MFH (Microfilled hybrid resin) | -Milling: Zenotec t1 5-axis dental milling machine -3D Printing: NextDent 5100 printer | -3D-printed layer thickness: 0.075 mm (horizontal orientation inferred but not explicitly stated) | -Milled crowns (non-aged, 1.5 mm) showed highest fracture resistance (1706.36 N) -3D-printed crowns (aged, 0.9 mm) had lowest fracture resistance (552.49 N) -Thermocycling significantly reduced strength (p < 0.01) |
| Abad-Coronel et al. (2023) [81] | Fracture resistance of CAD/CAM materials (milled-derived PMMA vs. 3D-printed resins: 3DPPa and 3DPPb) | 1. PMMA: Ivoclar Vivadent 2. 3DPPa: SprintRay (Hybrid resin (ceramic-polymer composite)) 3. 3DPPb: SprintRay (Nano ceramic hybrid (ceramic-resin composite)) | -PMMA: CNC milling -3DPPa/3DPPb: DLP | -Layer thickness: 50 μm -UV light curing for 9 min | -PMMA showed highest fracture resistance (1427.9 N ± 36.9), followed by 3DPPa (1231 N ± 380.1) and 3DPPb (1029.9 N ± 166.46) -All materials exceeded average masticatory forces (~720 N) |
| Revilla-León et al. (2021) [82] | Chemical composition, Knoop hardness, surface roughness, shear bond strength | 1. CNV Group: -Protemp 4 (3M ESPE, High silica (42.99% Si)) -Anaxdent (Anaxdent) 2. AM Group: -FreePrint Temp -AM-2: E-Dent 400 C&B MFH, High Titanium (8.64%) -AM-3: NextDent C&B MFH, Mixed elements (Na, Si, K, Cl, Ti) -AM-4: Med620 VEROGlaze, Oxygen (84.66%), Sodium (3.06%), Titanium (2.05%) | CNV: Silicone index + glass tile AM: CAD-designed disks printed with 90° build orientation | -Layer thickness: 50 μm, -Building orientation: 90° for all AM groups -Post-polymerization: UV curing (6–30 min): -AM-1: 6 min -AM-2: 15 min -AM-3: 30 min -AM-4: None required | -Significant chemical variations between AM/CNV groups -AM-4 (13.45 KHN) and CNV-2 (13.35 KHN) showed highest hardness -AM-1 had highest roughness (1.88 Ra) -No significant bond strength differences |
| Soto-Montero et al. (2022) [83] | Effect of post-curing time (0, 5, 10, 15, 20 min) on -Flexural strength (FS) -Flexural modulus (FM) -Microhardness (KHN) at varying depths | 1. Cosmos Temp3D (COS) (Methacrylate oligomers, diphenyl-2,4,6-trimethylbenzoyl phosphine oxide, TiO2, carbon black) 2. SmartPrint BioTemp (SMA) (Methacrylic ester monomers, stabilizers, fillers, pigments) 3. Resilab3D Temp (RES) (Undisclosed) 4. Prizma3D BioProv (PRI) Methacrylic acid esters, acrylic oligomers, pigments | 3D-printed using DLP technology (Anycubic Photon printer, Anycubic Technology Co., Shenzen, China) | -50 μm printed at 0° angulation -Anycubic Wash and Cure 2.0 unit (violet LED, 390–410 nm peak at 401 nm), irradiance 4–10 mW/cm2, rotational curing platform | -Post-curing time significantly influenced ΔE00, FS, FM, and KHN -COS and SMA exceeded ΔE00 acceptability thresholds after 5 and 10 min, respectively -FS plateaued earlier for RES (5 min), PRI/SMA (10 min) -Longer post-curing increased surface KHN but reduced depth polymerization efficiency |
| Bayarsaikhan et al. (2021) [84] | Post-curing temperature (40 °C, 60 °C, 80 °C) and duration (15–120 min) | Denture Teeth Resin A2 (Formlabs, Somerville, MA, USA): PMMA-based acrylic resin with (meth)acrylate monomers (exact composition not specified) | SLA | -Layer thickness: 50 µm -Bars: 120° orientation, Disks: 0° orientation -FormCure UV-light chamber (405 nm, 13 LEDs) at 40–80 °C for 15–120 min; cleaned with 90% isopropanol | -Higher post-curing temperature (80 °C) and longer duration (120 min) improved flexural strength (147.48 MPa) and cell viability (89.51%) -Lower cytotoxicity and protein adsorption at 80 °C -Post-curing time > 60 min showed minimal incremental benefits |
| Mayer et al. (2021) [85] | Cleaning methods (Isopropanol, Yellow Magic 7, Centrifugation) and their impact on wear/fracture load; comparison of 3D-printed vs. milled PMMA FDPs | 1. Freeprint Temp (FPT: Methacrylates, photoinitiators (no fillers)) 2. GC Temp PRINT (GCT: Methacrylates, quartz fillers) -C&B MFH (NMF: Unspecified resin with inorganic fillers) 3. TelioCAD (TEL: PMMA polymer (no fillers)) | -3D-printed: DLP -Milled: Wet grinding process | Not specified in the provided content | -Printed FDPs showed superior wear resistance but lower fracture load vs. milled PMMA -Isopropanol cleaning reduced fracture load vs. centrifugation/Yellow Magic -Fillers improved wear resistance but not fracture load |
| Aldahian et al. (2021) [86] | Marginal integrity, surface roughness, wear of interim crowns | 1. Conventional (CN): Jet Tooth Shade™ Self-Curing Acrylic Resin (Lang Dental Manufacturing Co. Inc.) 2. CAD/CAM (CC): Cercon base PMMA blocks (DeguDent GmbH, Hanau, Germany) 3. 3D Printing (3D): Freeprint Temp resin (DETAX GmbH & Co. KG, Ettlingen, Germany) | -CN: Manual mixing, molding, and polymerization -CC: CAD/CAM milling (Versamill machine) -3D: SLA | -Layer Thickness: 50 μm -Orientation: 0° (flat printing) -Soaked in 99% isopropyl alcohol (60 s), UV-cured (90 s in curing chamber) | -Adaptation:CN and CC showed comparable adaptation (p > 0.05); 3D had lowest values (197.82 ± 11.72 μm) -Marginal Misfit:CN had highest misfit (395.89 ± 80.33 μm); 3D and CC performed better (p < 0.05) -Surface Roughness: CC had lowest Ra (3.28 ± 0.34 μm); 3D had highest (5.61 ± 0.33 μm) -Surface Wear: 3D showed lowest wear (10.81 ± 2.00 mm3); CN had highest (17.79 ± 2.78 mm3) -Post-Treatment: Critical for 3D-printed specimens to achieve optimal mechanical properties |
| Park et al. (2018) [40] | Wear resistance of 3D-printed, milled, and self-cured resin materials opposing zirconia and CoCr alloy antagonists | 1. C&B: NextDent 2. Vipi Block: VIPI 3. Jet™: Lang Dental Mfg -All materials: PMMA-based (Poly Methyl Methacrylate) | -3D-printed resin: DLP 3D printing (Veltz3D D1-150) -Milled resin: Dry milling (Roland DWX-51D) -Self-cured resin: Conventional pressure curing in a mold | -Layer thickness: 100 μm -Build angle: 0° (tested surface parallel to build platform) -Post-wash with 100% isopropyl alcohol -Post-curing for 120 min (Denstar-300 machine) | -No significant difference in wear resistance between 3D-printed, milled, and self-cured resins -SEM revealed cracks and interlayer bond separation in 3D-printed resin when opposing metal abraders -No significant wear difference between zirconia and metal antagonists |
| Kessler et al. (2019) [87] | Three-body wear resistance of temporary dental materials | 1. 3Delta temp 2. NextDent C&B 3. Freeprint temp 4. Telio CAD 5. Tetric EvoCeram (Bis-GMA, UDMA, barium glass (75–76 wt% filler)) | -3D-printed: DLP -Telio CAD: Milled from blocks -Tetric EvoCeram: Direct light-curing | -Layer thickness: Not explicitly stated -Parallel to build platform -ltrasonic cleaning (ethanol) -Post-curing: 2 × 2000 flashes under nitrogen (Otoflash G171) | -Lowest wear: Tetric EvoCeram (50 ± 15 µm), 3Delta temp (62 ± 4 µm) -Highest wear: Freeprint temp (257 ± 24 µm) -Filler content directly correlated with wear resistance -3Delta temp outperformed other 3D-printed materials due to higher filler content |
| Digholkar et al. (2016) [88] | Fabrication methods: Rapid prototyping (RP), CAD/CAM milling (CC), conventional heat-activated PMMA (CH) | 1. RP: Envision TEC E-Dent 100 (Light-cured micro-hybrid filled composite) 2. CAD/CAM: Ceramill TEMP (PMMA) 3. Conventional: Heat-activated PMMA (GC Corporation) | -RP: 3D printing with UV light polymerization -CAD/CAM: Milling of pre-polymerized blanks -Conventional: Compression molding | -Layer-by-layer additive manufacturing (vertical stacking) -UV oven curing for RP specimens | -Highest flexural strength: CAD/CAM (104.20 MPa) -Highest microhardness: RP (32.77 KHN) -No significant difference between CAD/CAM and conventional flexural strength (p = 0.64) |
| Reymus et al. (2020) [89] | -Build direction (occlusal, buccal, distal) -Post-curing methods -Artificial aging (H2O immersion for 21 days at 37 °C) | 1. 3D-printed resins: Experimental (EXP, GC Europe), NextDent C&B (CB, NextDent), Freeprint temp (FT, Detax), 3Delta temp (DT, Deltamed) -Methylmethacrylate for all 3D-printed materials 2. Controls: TelioCAD (TC, Ivoclar-Vivadent) | -3D-printed using SLA/DLP technology (D20II printer, Rapid shape, Heimsheim, Germany) -Positive control (TC) milled from PMMA blocks -Negative control (LT) fabricated via conventional interim material technique | -Long-axis orientations: occlusal, buccal, or distal relative to the printer’s platform -Labolight DUO (6 min LED curing) -Otoflash G171 (4000 flashes -LC-3DPrint Box (30 min UV curing) | -Distal build direction yielded higher fracture load vs. occlusal -CB showed highest fracture load, EXP the lowest -Post-curing strategy significantly impacted mechanical stability -EXP and DT exhibited reduced fracture load after artificial aging |
| Schulz et al. (2023) [42] | Interim resin (VarseoSmile Temp A2) vs. permanent ceramic-filled hybrid resin (VarseoSmile Crown Plus A2) | 1. Interim resin: Methacrylic acid esters, diphenyl phosphine oxide 2. Permanent resin: Methacrylic acid esters, silanized dental glass, inorganic fillers (30–50% by mass) | 3D printing via DLP | Not explicitly stated in the paper (marked N/A) -Ultrasonic cleaning in ethanol (96%) -Nitrogen gas (1.0–1.2 bar) + otoflash device (1500 flashes, 10 Hz) | -No significant difference in fracture resistance: 365.90 ± 86.67 N (interim) vs. 363.45 ± 87.57 N (permanent) -Both materials exhibited sufficient resistance to masticatory forces |
| Alshamrani et al. (2023) [45] | Mechanical properties (flexural strength), biocompatibility (cell viability) | 1. Resin: B2 Everes Temporary (Sisma, Vicenza, Italy) 2. Nanoparticles: Glass silica (GM35429) and zirconia (GM018-307) (Schott, Landshut, Germany) | 3D-printed using DLP | Layer Thickness: Not explicitly stated in the provided content; 90-degree orientation from the build platform | -5% glass silica and 10–20% zirconia significantly improved flexural strength (113.8–114.6 MPa) -All groups showed >80% cell viability (non-cytotoxic) -Higher zirconia concentrations enhanced biocompatibility (>94%) |
| KEßLER et al. (2021) [90] | Printing direction (horizontal parallel, horizontal perpendicular, vertical), aging (thermocycling: 10,000 cycles at 5–55 °C) | 1. NextDent C&B 2. 3Delta temp 3. Freeprint temp | DLP | -Layer Thickness: 1. NextDent C&B: 50 μm 2. Freeprint temp: 50 μm 3. 3Delta temp: 100 μm -Layer Orientation: 1. Horizontal parallel (force perpendicular to layers) 2. Horizontal perpendicular (force parallel to layers) 3. Vertical (force perpendicular to layers) -Post-curing: 1. NextDent C&B: LC-3D Print Box (30 min) 2. Freeprint temp and 3Delta temp: Otoflash G171 (2 × 2000 flashes under nitrogen) | 1. Printing direction significantly affected FS/FM (ηp2 = 0.407 for FS in 3Delta temp) 2. Aging reduced FS by 12–25% 3. 3Delta temp (highest filler content) outperformed others in FS and FM |
| Eun-Hyuk Lee et al. (2022) [91] | Layer thickness (25 µm, 100 µm), printing orientation (0°, 45°, 90°) | C&B 5.0 Hybrid (ARUM) | DLP 3D printing, post-cleaned with isopropyl alcohol, UV-polymerized, ground with abrasive paper | -Layer thickness: 25 and 100 µm -Layer Orientation: 0°, 45°, 90° -Post-curing: UV light polymerization (PURE PRO unit) | -Thinner layers (25 µm) showed higher discoloration -0° orientation had better color stability vs. 45°/90° -Red wine caused continuous discoloration; coffee peaked at 15 days -Surface roughness and contact angle unaffected by parameters |
| Scherer et al. (2023) [92] | Layer thickness (10–150 μm) and artificial aging (thermocycling) effects | NextDent C&B MFH (3D Systems) | DLP | -Layer thickness: 10, 25, 50 (control), 75, 100, 125, 150 μm -Orientation: Perpendicular to load direction -Post-curing: 30 min in LC-3DPrint Box (300–550 nm light), after 3 + 2 min IPA rinsing | -Layer thickness did not significantly affect flexural strength -Artificial aging reduced flexural strength (80.33% variance explained) -Highest Weibull modulus for nonaged 50/75 μm and aged 125 μm specimens |
| Almira Ada Diken Turksayar et al. (2022) [93] | Fracture strength of 3-unit interim FDPs under different printing orientations (0°, 30°, 45°, 90°, 150°) and manufacturing methods | 1. Additive: Temporary CB (Methacrylate-based resin) 2. Subtractive: DuoCAD (PMMA, FSM Dental) | -Additive: SLA -Subtractive: Milled with CEREC MC X5 | -Layer thickness: 50 μm for SLA printing -Orientation: 0°, 30°, 45°, 90°, 150° relative to the build platform -Post-curing: -Washed in isopropyl alcohol -Cured twice (20 min each, 60 °C) in Form Cure unit | -0° and 30° printed FDPs showed fracture strength comparable to milled PMMA -90° orientation had the lowest strength -Milled FDPs outperformed 45° and 150° printed FDPs |
| Derban et al. (2021) [43] | Printing angle (0°, 45°, 90°) and load direction (parallel vs. perpendicular) | 1. NextDent MFH Vertex Dental (Vertex Dental B.V, Soesterberg, The Netherlands) 2. Detax Freeprint Temp (Detax GmbH & Co KG, Ettlingen, Germany) | SLA | -Layer thickness: 50 microns -Orientation: 0°, 45°, 90° (additional 0° specimens for load direction testing) -Post-curing: -Ultrasonic cleaning in ethyl alcohol (3 cycles) -Nitrogen gas curing in Otoflash unit | -Printing angle significantly affects flexural strength (p < 0.001) -0° and 90° orientations showed better mechanical performance than 45° -Parallel loading direction to layer growth increased strength. |
| Unkovskiy et al. (2018) [94] | Build orientation (0°, 45°, 90°), positioning on build platform, curing methods | Dental SG: Photopolymer resin (class I biocompatible, ISO 10993-1 [95]) | -Layer thickness: 50 µm -Orientation: 0°, 45°, 90° -Post-curing: 15 min curing in three units: Dentacolor XS, Speed Laborlight, Visio Beta Vario (320–520 nm wavelength) -Uncured “green state” specimens as control | -45° orientation showed highest dimensional accuracy -90° orientation had superior flexural strength/modulus -Edge positioning caused higher inaccuracies -Curing units had no significant impact on accuracy or mechanical properties -Final polymerization improved flexural properties but did not affect dimensions | |
| Chen et al. (2023) [96] | Post-polymerization temperature (RT, 40 °C, 60 °C, 80 °C) and time (0–120 min) | AA Temp (Methacrylate-based resin (photopolymerizable)) | 3D-printed via DLP, cleaned with 95% alcohol | -Layer thickness: 50 μm; orientation not specified -Post-curing: FormCure unit (405 nm, 40–80 °C, 15–120 min) | -Optimal flexural properties at 60 °C/90 min -Curing depth: 3–4 mm with heating -Surface hardness improved with post-polymerization -60 °C showed superior mechanical properties compared to other temperatures -Post-polymerization without heating resulted in shallow curing depth (<1–2 mm) |
| Crispim et al. (2024) [97] | Build direction (30° vs. 90°), post-polymerization time (15, 30, 45 min), aging (90-day water storage at 37 °C) | Provisional resin: Cosmos TEMP | 3D-printed provisional crowns | -Layer thickness: 50 μm. -Orientation: 30° and 90° relative to the horizontal plane -UV post-curing (405 nm, 40 W) with Anycubic Wash & Cure Plus (Anycubic Technology Co., Shenzen, China), durations: 15, 30, 45 min | -30° build direction improved marginal/internal adaptation, fracture resistance, and margin quality -Post-polymerization for 30 min maximized fracture resistance -Aging (90 days) reduced strength but enhanced degree of conversion -Lower MD/ID in aged 30° groups versus 90° -98.6% of 30° crowns had defect-free margins vs. 90° group with higher irregularities |
| Britto et al. (2022) [39] | Flexural strength (σf), elastic modulus (E), water sorption (Wsp), solubility (Wsl), biocompatibility | 1. 3D: Oligomers, monomers, photoinitiators, stabilizer, pigments 2. BA: Bis-acryl composite resin 3. AR: Heat-cured acrylic resin (PMMA-based) | 1. 3D: Varseo 3D printer (Bego, Bremen, Germany) 2. BA: Silicone molds from 3D prints 3. AR: Traditional flasking/heat curing | -Layer thickness: 0.03 mm -Orientation: Horizontal -Resolution: 25 μm -LED light curing (400–450 nm, 13 min) | -3D showed increased σf vs. AR after aging -BA had lowest σf/E values -All materials met ISO 10477 [98] for Wsp/Wsl -AR showed reduced cell viability (71.9% vs. 92.9% for 3D) in SRB test |
| Author and Year | Studied Property | Evaluated Materials | Fabrication Technique | 3D Printing Parameters | Key Results |
|---|---|---|---|---|---|
| Cristina Espinar et al. (2023) [1] | Color difference (ΔE00) and relative translucency parameter (RTP00) | -DFT: Detax Freeprint Temp (A1,A2,A3, GmbH) -FP: Formlabs Permanent Crown (A2,A3,B1,C2, Formlabs Inc., Somerville, MA, USA) -FT: Formlabs Temporary CB (A2,A3,B1,C2) -GCT: GC TempPrint (Light/Medium, GC Corporation, Tokyo, Japan) | -DFT and GCT: DLP (Asiga Max UV) -FP and FT: SLA (Form 3B+) | -Layer thickness: 50 µm -Orientation: 0° and 90° | -Printing orientation caused perceptible ΔE00 (>0.81) for DFT-A1/A2/A3, FP-B1/C2, FT-A2/B1 -DFT-A1 showed highest ΔE00 (2.94) exceeding acceptability threshold -Significant RTP changes in DFT-A1/A3, FP-B1, FT-B1 (>0.62 perceptibility threshold) -GC TempPrint showed minimal color/translucency variations -Color changes were primarily driven by ΔL* (lightness) or ΔC* (chroma), except GCT-M (hue) -Translucency Direction: Depended on material/shade (e.g., DFT increased at 90°, GCT decreased at 90°) |
| Soto-Montero et al. (2022) [83] | Color change (ΔE00) | 1. Cosmos Temp3D (COS) 2. SmartPrint BioTemp (SMA) 3. Resilab3D Temp (RES) 4. Prizma3D BioProv (PRI) | DLP | -Layer thickness: 50 μm layer thickness -Orientation: 0° | -Post-curing time significantly influenced ΔE00, FS, FM, and KHN -COS and SMA exceeded ΔE00 acceptability thresholds after 5 and 10 min, respectively |
| Lee et al. (2022) [91] | Color stability (ΔE00) and stainability under aging media | C&B 5.0 Hybrid resin (ARUM), ASIGA MAX UV 3D printer (ASIGA Sydney, Australian): Methacrylate-based photopolymer resin (exact composition not specified) | DLP | -Layer thickness: 25 µm, 100 µm -Orientation: 0°, 45°, 90° | -25 µm layers showed higher ΔE00 than 100 µm -0° orientation had lowest discoloration -Coffee caused initial ΔE00 increase then decrease; wine caused continuous increase |
| Al-Akhali et al. (2023) [131] | Color stability (ΔE*) after 1 and 7 days of immersion in khat extract vs. distilled water | -PMMA CAD/CAM milling: Poly-methyl methacrylate -3D Printing: Liquid resin (unspecified polymer) -PMMA SC acrylic resin: Self-cured PMMA -LC composite: Light-cured composite -Bis-acrylic SC composite: Bis-acrylate resin | -Manual: Metallic mold (PMMA SC, LC composite, Bis-acrylic) -CAD/CAM: Milled from PMMA blocks -3D Printing: DLP | -Layer thickness: 50 μm -Orientation: Not specified | -3D printing: Significant color increase over time (ΔE* = 1.96 at 1 day; 10.67 at 7 days) -Khat extract caused greater discoloration than distilled water (p < 0.05) -3D printing limitations: Surface roughness and lower polymerization rates contributed to higher color instability |
| Yıldırım et al. (2024) [128] | Aging resistance after thermocycling | 1. PEMA: Dentalon Plus 2. BRC: Prevision Temp 3. Milled: Tempo CAD 4. Printed: Cura Temp | Not specified | -Layer thickness: layer thickness 100 μm -Orientation: perpendicular (90°) orientation to build platform | -Highest ΔE00 in BRC (3.2) and printed (3.0) -Lowest ΔE00 in PEMA (1.1) and milled (1.3) -Printed/BRC exceeded clinical acceptability threshold (ΔE00 > 1.8) |
| Alalawi et al. (2024) [129] | Color stability | 1. UNIFAST III: Methyl methacrylate 2. NextDent C&B MFH: Methacrylic oligomers + phosphine oxides 3. FormLabs Temporary CB Resin: Biocompatible photopolymer resin 4. TelioCAD: 99.5% PMMA + 0.5% pigment | 1. Cold-cured mold 2–3. 3D-printed 4. CAD/CAM milled | Not specified | -Coffee/tea caused greatest ΔE (3.22–19.03 NBS units), especially on unpolished surfaces -3D-printed materials exhibited greater susceptibility to dietary solvents compared to milled -Surface finishing significantly impacted results (unpolished surfaces more vulnerable) |
| Almejrad et al. (2021) [132] | Color stability (ΔE, ΔL*) using CIE Lab* system | NextDent Crown & Bridge A3.5: Methacrylate-based photopolymerizing resin | 3D-printed full-coverage interim crowns | Not specified | -Highest ΔE: Wine (24.92 ± 4.6 for polish, 19.17 ± 2.5 for Optiglaze) -Optiglaze reduced coffee-induced discoloration (ΔE 2.82 vs. 7.89 in polish) -All groups exceeded ΔE acceptability threshold (2.7) |
| Author and Year | Evaluated Materials | Shape and Dimension of Tested Resins Samples | Result of Water Sorption (Wsp) | Result of Water Solubility (Wsl) |
|---|---|---|---|---|
| Britto et al. (2022) [39] | 1. 3D-printed polymer (Cosmos Temp) 2. Bis-acryl composite resin (Yprov Bis-acryl) 3. Heat-cured acrylic resin (Coroas e Pontes) | Bar-shaped specimens: -Length: 25 ± 2 mm -Height: 2 ± 0.1 mm -Width: 2 ± 0.1 mm Disk-shaped specimens: -Diameter: 15 ± 1 mm -Thickness: 1 ± 0.1 mm | -3D-printed polymer: 14.4 μg/mm3 -Lowest water sorption among tested materials -Well below ISO 10477:2020 limit of 40 μg/mm3 | -3D-printed polymer: 3.5 μg/mm3 -Shared value with Bis-acryl resin -Significantly lower than the ISO 10477:2020 limit of 7.5 μg/mm3 |
| Leila Perea-Lowery et al., 2021 [140] | 1. Imprimo® LC Denture (Scheu-Dental GmbH, Iserlohn, Germany) 2. Paladon® 65 (Kulzer GmbH, Mitsui Chemicals, Hanau, Germany) 3. Palapress® (Kulzer GmbH, Mitsui Chemicals, Hanau, Germany) | Bar-shaped specimens 10.0 × 65.0 × 3.3 ± 0.2 mm3 | Mean values: -3D-printed Imprimo Cure®: 2.2 ± 0.01% -3D-printed Form Cure®: 2.2 ± 0.008% | Mean values: -3D-printed Imprimo Cure®: 0.67 ± 0.024% -3D-printed Form Cure®: 0.55 ± 0.027% -Paladon®: 0.32 ± 0.024% (lowest) |
| Veronika Greil et al., 2023 [139] | 1. NextDent Denture 3D+ (DEN)—NextDent, Soesterberg, Netherlands 2. Fotodent Denture (FOT)—Dreve ProDiMed, Unna, Germany 3. Freeprint Denture (FRE)—DETAX, Ettlingen, Germany 4. V-Print dentbase (VPR)—VOCO, Cuxhaven, Germany 5. Ivotion Base (IVO)—Ivoclar Vivadent, Schaan, Liechtenstein 6. PalaXpress (PAL)—Kulzer, Hanau, Germany | Rectangular specimens in three geometries: -5 × 10 × 25 mm (for degree of conversion) -Specific dimensions for water sorption, flexural strength tests | -3D-printed resins: 25.31–37.94 μg/mm3 -Exceeds ISO norm (32 μg/mm3) for most materials -Highest: VPR and DEN -Lowest: FOT | -3D-printed resins: 0.08–8.27 μg/mm3 -Exceeds ISO norm (8 μg/mm3) for most materials -Highest initial values: VPR -Lowest initial values: FOT |
| Jain et al., 2022 [17] | Not specified in detail in the paper | Not specifically detailed in the review | -3D-printed PMMA: Higher than conventional polycarbonate, lower than conventional PMMA -3D-printed photopolymer: Higher than CAD/CAM milled PMMA and conventional bis-acrylic | -3D-printed PMMA: Higher than conventional polycarbonate and PMMA resins -3D-printed photopolymer: Higher than conventional PMMA, bis-acrylic, and CAD/CAM milled PMMA |
| Author and Year | Evaluated Materials | Specimen Fabrication Technique | Key Results |
|---|---|---|---|
| Atria et al. (2022) [181] | -Crowntec (CT) -Temporary C&B (FL) -C&B MFH (ND) -Permanent Bridge (PB) | 3D printing followed by post-processing steps (washing, UV curing, etc.) | No significant differences in cell viability and proliferation among materials; cytotoxicity was low for all materials, with ND showing the highest LDH activity (13.7%) |
| Britto et al. (2022) [39] | -3D: Cosmos Temp -BA: Yprov Bis-acryl -AR: Coroas e Pontes | -3D: 3D printing (Varseo 3D printer, Bego, Bremen, Germany) with 25 μm resolution and 20–40 mm/h building rate -BA: Laboratory condensation silicone matrices -AR: Heat-cured acrylic resin | -3D structures showed higher cell viability (92.9%) compared to AR (71.9%) in SRB test -No significant difference in MTT assay (p > 0.05) |
| Folwaczny et al. 2023 [61] | -NextDent MFH -3Delta temp -GC Temp -Freeprint temp -Grandio disc -Luxatemp | -3D-printed materials: Additive manufacturing (NextDent MFH, 3Delta temp, GC Temp, Freeprint temp) -Subtractive material: Grandio disc (Voco) -Conventional material: Luxatemp (DMG) | -Luxatemp and 3Delta temp caused significant reduction in cell viability (<10% of control) and strong inhibition of IL-6 and IL-8 expression -Grandio disc and other 3D-printed materials (MFH, GC Temp, Freeprint) showed higher cell viability (>70% of control) and moderate cytokine expression |
| Alshamrani, A. et al. 2023 [45] | -B2 Everes Temporary (dental resin)—Sisma, Italy; Glass fillers (GM35429)—Schott, Landshut, Germany; Zirconia glass (GM018-307)—Shofu Inc., Ratingen, Germany | DLP 3D printing | Cell viability > 80% for all groups, indicating non-toxicity and biocompatibility |
| Wuersching et al. [175] | Permanent FDP: -Tetric EvoCeram -Tetric CAD -VarseoSmile Crown plus -NextDent C&B MFH Temporary FDP: -Protemp 4 -Telio CAD -VarseoSmile Temp -Temp PRINT -P Pro Crown & Bridge | -Additive (DLP 3D printing): Varseo XS/BEGO, P30/RapidShape, NextDent 5100 -Subtractive: Milled resin blocks (Tetric CAD, Telio CAD) -Conventional: Light-cured (Tetric EvoCeram)/self-cured (Protemp 4) | -Tetric CAD/Telio CAD (subtractive resins): Slight toxicity -All other resins: Moderate–severe cytotoxicity -VarseoSmile Crown+/P Pro Crown & Bridge: Significantly elevated PGE2 -Telio CAD/VarseoSmile Temp/P Pro: Increased oxidative stress (↑GSSG) -All printable resins: Induced slight apoptosis |
| Rogers, H.B. et al. (2021) [176] | -Dental SG (DSG) and Dental LT Clear (DLT), manufactured by Formlabs. | 3D printing using SLA technology—specimens were post-processed with ethanol washes and UV curing | -DLT resin leachates, particularly Tinuvin 292, caused severe oocyte toxicity and chromosomal misalignment. -Plasma-treated DSG reduced oocyte degeneration but caused chromosomal abnormalities |
| Author and Year | Evaluated Materials | Main Chemical Composition | 3D Printing Technique | 3D Printing Parameters | Key Results |
|---|---|---|---|---|---|
| Liu Sa et al. (2019) [184] | No specific trade name mentioned | -Resin components: UDMA (60 wt%), TEGDMA (40 wt%), TPO (1 wt%), -Antibacterial agent: Ag-HNT (1%, 2%, 3%) | DLP | 1. Z-resolution: 50 µm 2. Layer exposure time: 12 s 3. Additional UV curing for 0.5 h after printing | -The composite resin demonstrated sustained antibacterial activity, maintaining 99% efficiency even after repeated extraction for 7 days |
| ElMalah et al. (2024) [189] | VarseoSmile Crown plus; BEGO | -Antibacterial agent: TiO2 NPs and silanized chitosan nanoparticles (sCS NPs) | DLP | 1. Resolution: 25 µm 2. Layer thickness: 0.03 mm 3. Post-polymerized in a high-performance unit at 200 W for 15 min | -TiO2 NPs showed the highest antibacterial activity against Streptococcus mutans |
| Ye-Hyeon Jo et al. (2024) [190] | DentaBASE (Asiga, Sydney, Australia) | -Antibacterial agent: Phytochemical microcapsules (MPs) derived from phytoncide oil: (−)-α-pinene, (+)-3-carene, para-cymene | DLP | 1. Layer thickness: 50 μm 2. Build orientation: 0° horizontally positioned 3. UV-based polymerization system with a light-emitting diode (LED) power output of 200 W for 200 s | -MPs reduced colony counts (p ≤ 0.001) and biofilm formation (p ≤ 0.009) for all tested species; (−)-α-pinene suppressed microbial growth effectively without cytotoxicity (p = 0.310) |
| Li et al. (2019) [192] | No specific trade name mentioned | -Resin components: TMPTA3EO (acrylate), TTT (ene), PETMP (thiol) -Antibacterial agent: QAC/SH-QAC | DLP | 1. Print time: 10 min 2. Ethanol wash (1–2 min) + 405 nm LED post-curing (3–5 min) | -4 wt% QAC: >99.99% efficacy against E. coli and S. aureus -10 wt% SH-QAC: 100% efficacy against S. aureus -First thiol-ene-acrylate ternary system for DLP with 8.67% shrinkage (vs. >10% in conventional acrylates) -Maintained >85% double-bond conversion rate despite antibacterial additives |
| Wu et al. (2024) [193] | No specific trade name mentioned | -Resin components: ACMO, IBOMA, 3,3,5-trimethylcyclohexyl acrylate, bifunctional urethane acrylate resins, TPO photoinitiator -Antibacterial agent: IPDI-HEMA-choline chloride copolymer (N3) | DLP | 1. Post-curing: 2 h in UV light box | -10% N3 concentration achieved >99% antibacterial rate against E. coli/S. aureus -Maintained >99% efficacy after 35 days’ storage |
| Gan Jin et al. (2024) [194] | -Synthesized UA resin with 0 wt% (0F-UA), 5 wt% (5F-UA), and 10 wt% (10F-UA) fluoride complex -Reference material: DENTCA Denture Base II (Torrance, CA, USA) | -Base resin: Urethane-acrylate (ethoxylated pentaerythritol tetraacrylate, aliphatic urethane hexa-acrylate, methyl methacrylate, isobornyl acrylate) -Antibacterial agent: Zirconium(IV) fluoride complex | DLP | 1. Post-washing: 10 min in tripropylene glycol methyl ether 2. Post-curing: 20 min in Form cure (Formlabs) | -10F-UA showed strongest inhibition of S. mutans growth (direct contact: 9.96% viability; indirect: 48.75% viability) -Fluoride release correlated with antibacterial efficacy |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liang, X.; Yu, B.; Dai, Y.; Wang, Y.; Hu, M.; Zhong, H.-J.; He, J. Three-Dimensional Printing Resin-Based Dental Provisional Crowns and Bridges: Recent Progress in Properties, Applications, and Perspectives. Materials 2025, 18, 2202. https://doi.org/10.3390/ma18102202
Liang X, Yu B, Dai Y, Wang Y, Hu M, Zhong H-J, He J. Three-Dimensional Printing Resin-Based Dental Provisional Crowns and Bridges: Recent Progress in Properties, Applications, and Perspectives. Materials. 2025; 18(10):2202. https://doi.org/10.3390/ma18102202
Chicago/Turabian StyleLiang, Xiaoxu, Biao Yu, Yuan Dai, Yueyang Wang, Mingye Hu, Hai-Jing Zhong, and Jingwei He. 2025. "Three-Dimensional Printing Resin-Based Dental Provisional Crowns and Bridges: Recent Progress in Properties, Applications, and Perspectives" Materials 18, no. 10: 2202. https://doi.org/10.3390/ma18102202
APA StyleLiang, X., Yu, B., Dai, Y., Wang, Y., Hu, M., Zhong, H.-J., & He, J. (2025). Three-Dimensional Printing Resin-Based Dental Provisional Crowns and Bridges: Recent Progress in Properties, Applications, and Perspectives. Materials, 18(10), 2202. https://doi.org/10.3390/ma18102202







