Influence of Layer Thickness and Shade on the Transmission of Light through Contemporary Resin Composites
Abstract
1. Introduction
2. Materials and Methods
2.1. Test Samples
2.2. Light Transmission Measurement
2.3. Statistical Analysis
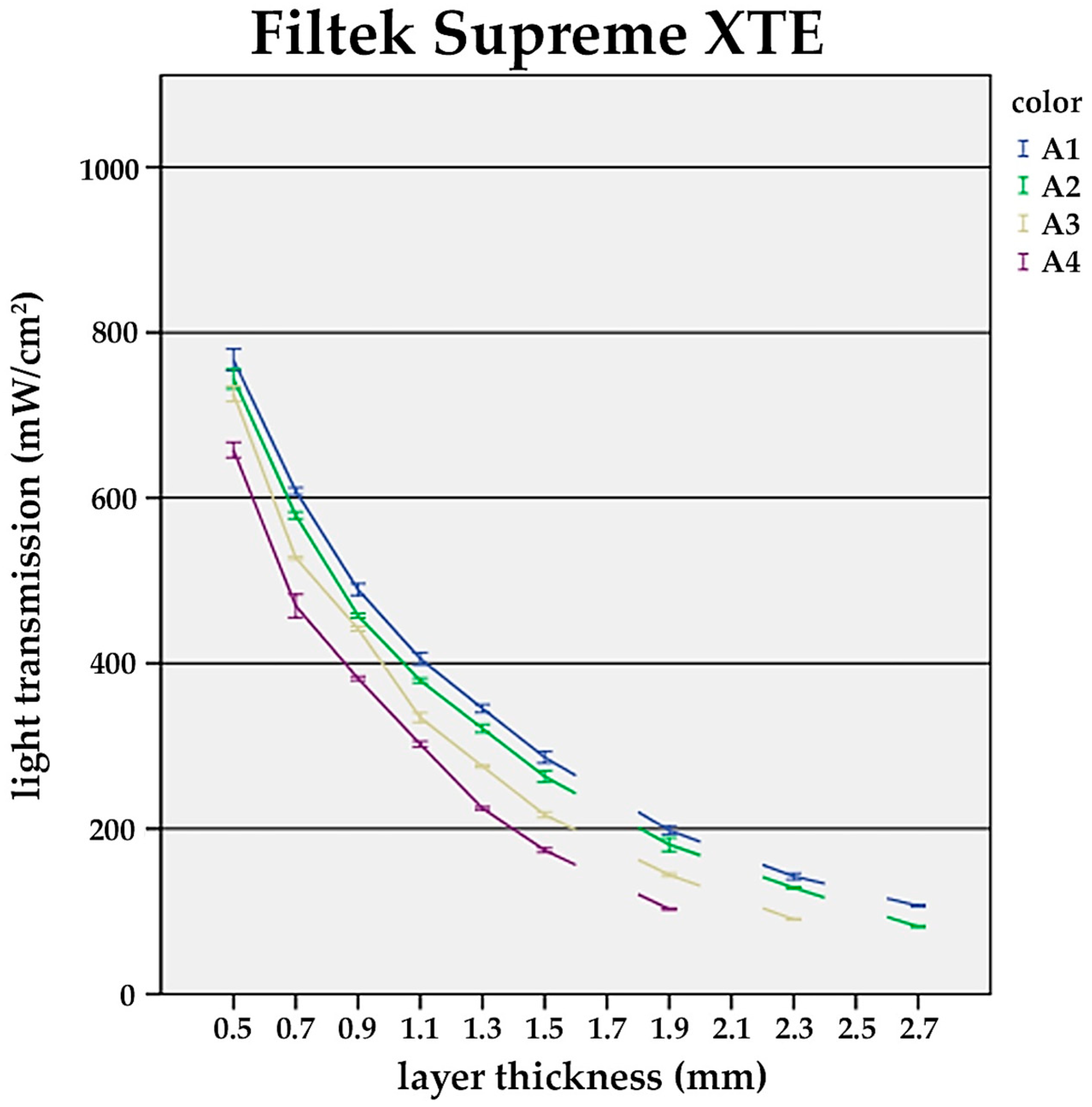
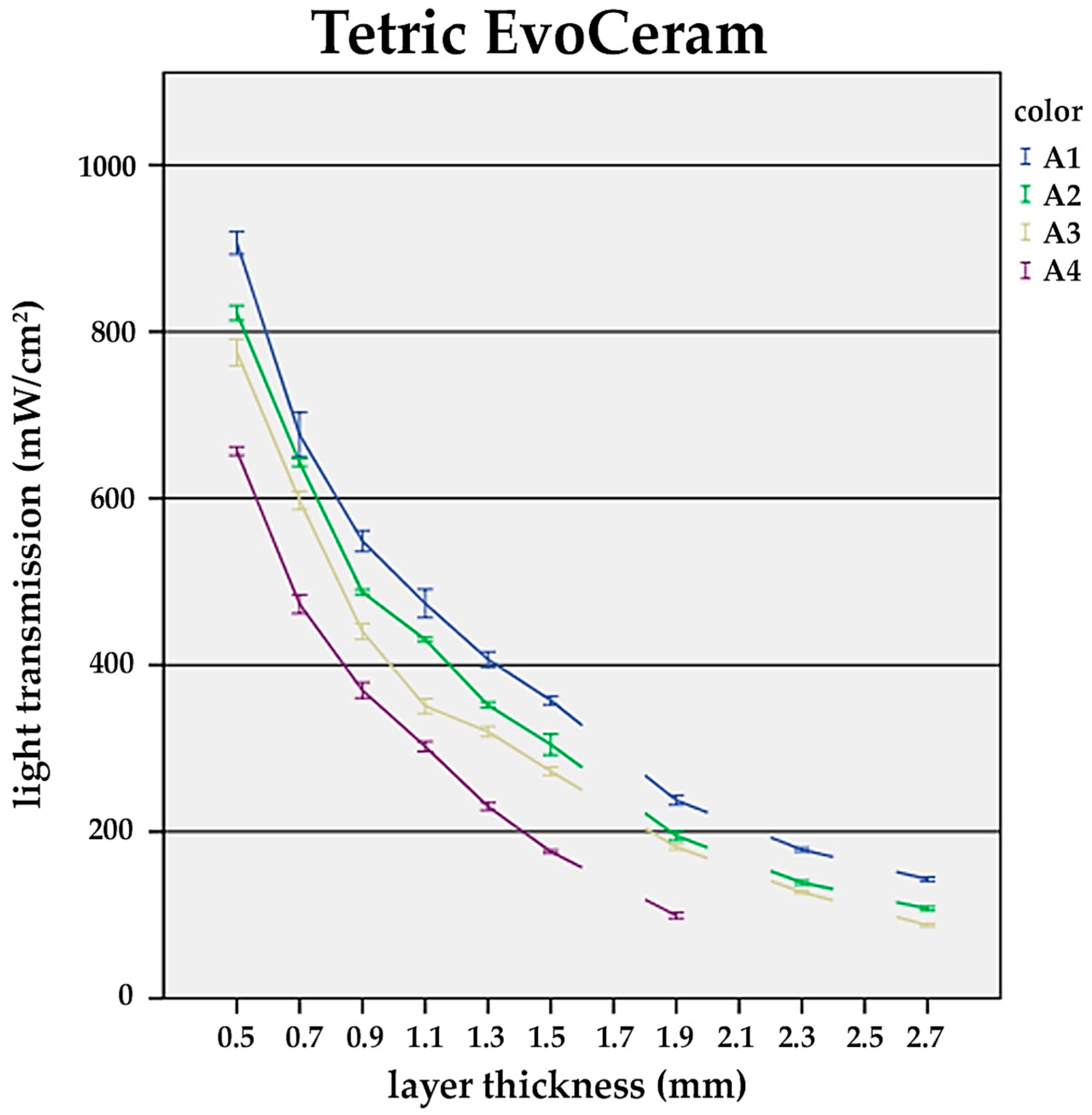
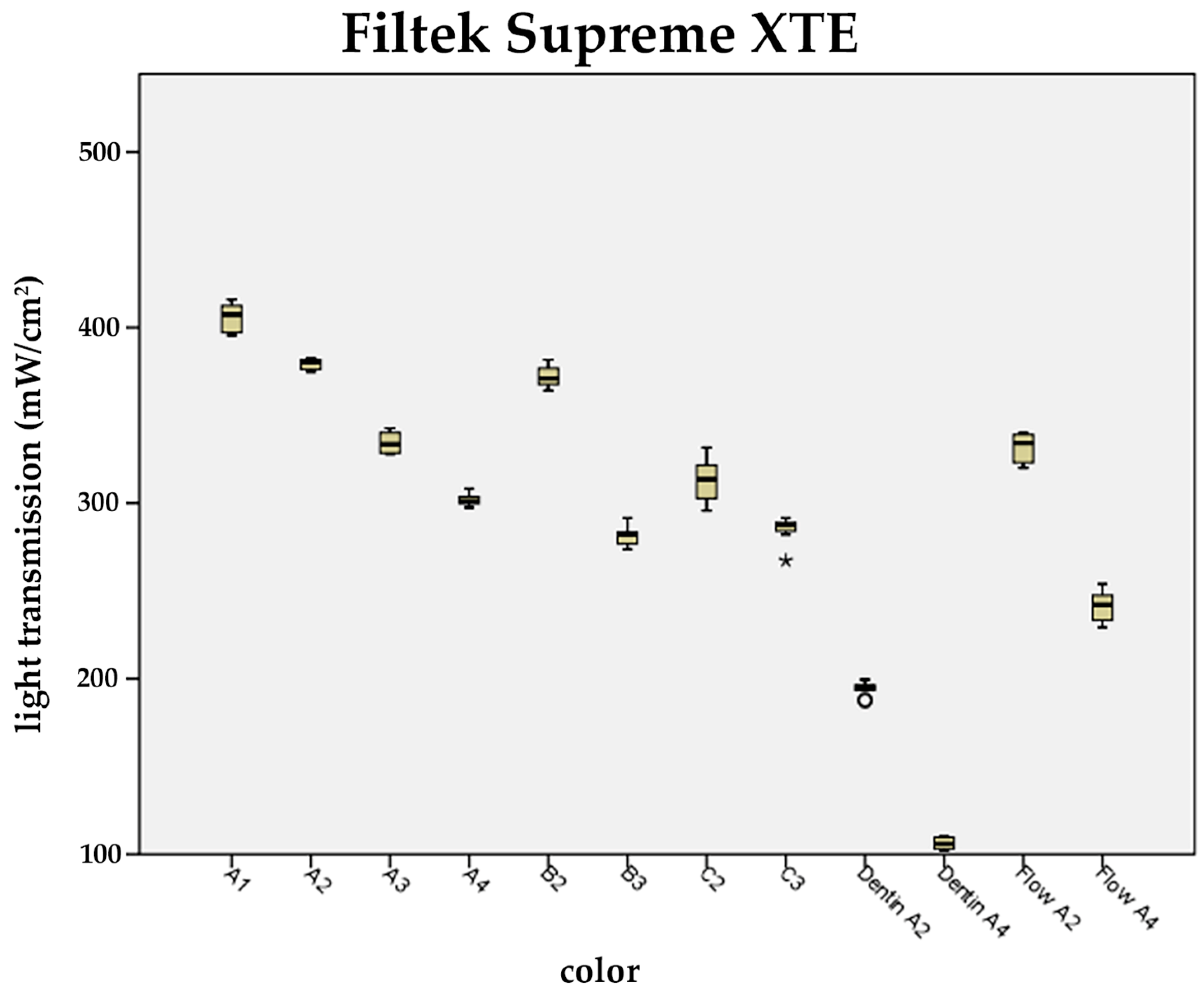
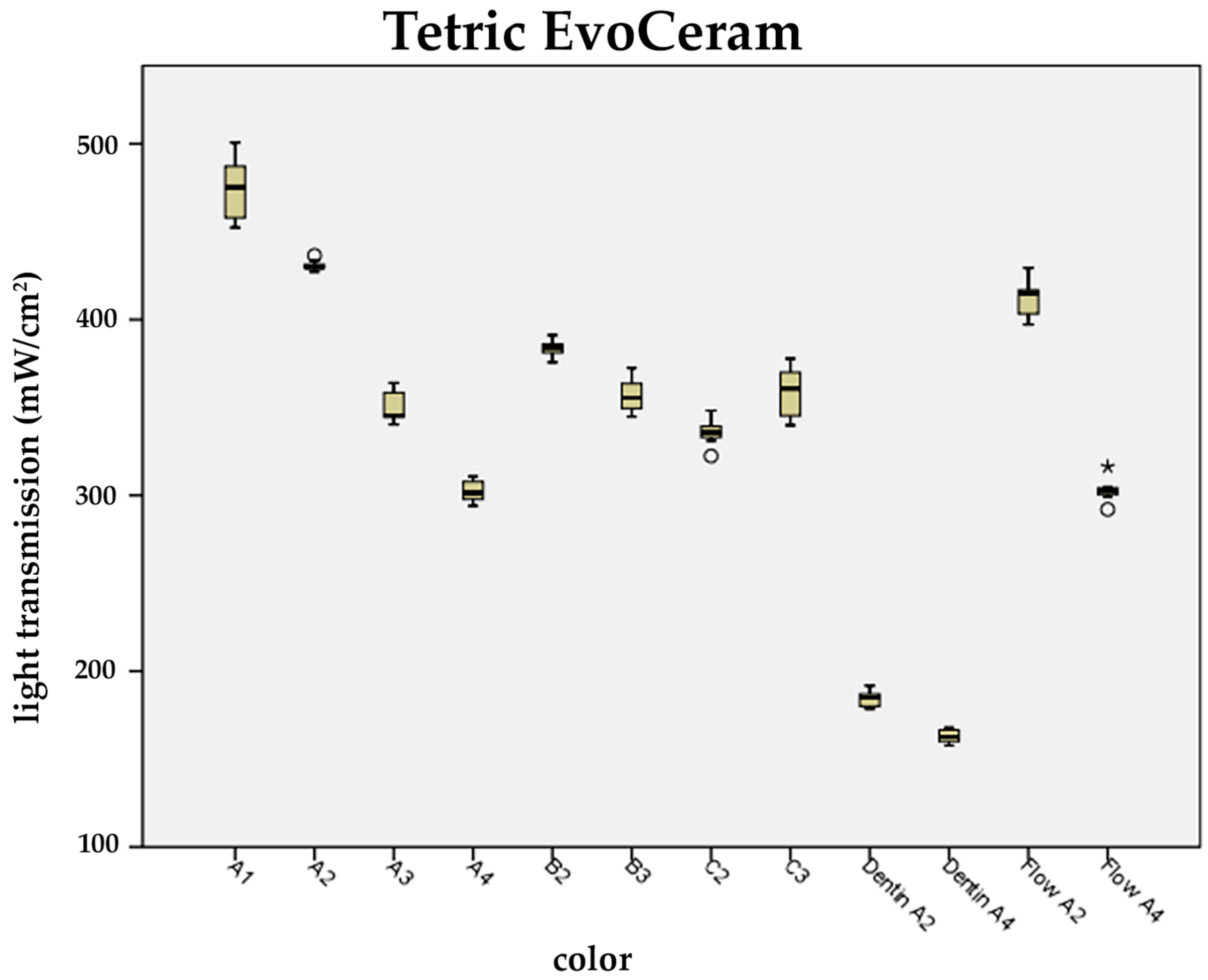
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Montag, R.; Dietz, W.; Nietzsche, S.; Lang, T.; Weich, K.; Sigusch, B.W.; Gaengler, P. Clinical and Micromorphologic 29-year Results of Posterior Composite Restorations. J. Dent. Res. 2018, 97, 1431–1437. [Google Scholar] [CrossRef]
- Yanishen, I.V.; Tkachenko, I.M.; Skrypnikov, P.M.; Hasiuk, P.A. Wear Resistance of Dental Materials Which Are Used for Anterior Teeth Restorations. Wiad. Lek. 2020, 73, 1677–1680. [Google Scholar] [CrossRef]
- Al-Senan, D.; Ageel, F.; Aldosari, A.; Maktabi, H. Knowledge and Attitude of Dental Clinicians towards Light-Curing Units: A Cross-Sectional Study. Int. J. Dent. 2021, 2021, 5578274. [Google Scholar] [CrossRef] [PubMed]
- Kojic, D.D.; El-Mowafy, O.; Price, R.; El-Badrawy, W. The Ability of Dental Practitioners to Light-Cure Simulated Restorations. Oper. Dent. 2021, 46, 160–172. [Google Scholar] [CrossRef] [PubMed]
- Maximov, J.; Dikova, T.; Duncheva, G.; Georgiev, G. Influence of Factors in the Photopolymerization Process on Dental Composites Microhardness. Materials 2022, 15, 6459. [Google Scholar] [CrossRef]
- Barszczewska-Rybarek, I.; Chladek, G. Studies on the Curing Efficiency and Mechanical Properties of Bis-GMA and TEGDMA Nanocomposites Containing Silver Nanoparticles. Int. J. Mol. Sci. 2018, 19, 3937. [Google Scholar] [CrossRef]
- Jandt, K.D.; Sigusch, B.W. Future perspectives of resin-based dental materials. Dent. Mater. 2009, 25, 1001–1006. [Google Scholar] [CrossRef]
- Pflaum, T.; Kranz, S.; Montag, R.; Güntsch, A.; Völpel, A.; Mills, R.; Jandt, K.; Sigusch, B. Clinical long-term success of contemporary nano-filled resin composites in class I and II restorations cured by LED or halogen light. Clin. Oral Investig. 2018, 22, 1651–1662. [Google Scholar] [CrossRef] [PubMed]
- Lovell, L.G.; Newman, S.M.; Donaldson, M.M.; Bowman, C.N. The effect of light intensity on double bond conversion and flexural strength of a model, unfilled dental resin. Dent. Mater. 2003, 19, 458–465. [Google Scholar] [CrossRef]
- Maktabi, H.; Balhaddad, A.A.; Alkhubaizi, Q.; Strassler, H.; Melo, M.A.S. Factors influencing success of radiant exposure in light-curing posterior dental composite in the clinical setting. Am. J. Dent. 2018, 31, 320–328. [Google Scholar]
- Moldovan, M.; Balazsi, R.; Soanca, A.; Roman, A.; Sarosi, C.; Prodan, D.; Vlassa, M.; Cojocaru, I.; Saceleanu, V.; Cristescu, I. Evaluation of the Degree of Conversion, Residual Monomers and Mechanical Properties of Some Light-Cured Dental Resin Composites. Materials 2019, 12, 2109. [Google Scholar] [CrossRef] [PubMed]
- Durner, J.; Obermaier, J.; Draenert, M.; Ilie, N. Correlation of the degree of conversion with the amount of elutable substances in nano-hybrid dental composites. Dent. Mater. 2012, 28, 1146–1153. [Google Scholar] [CrossRef] [PubMed]
- Tichy, A.; Simkova, M.; Vrbova, R.; Roubickova, A.; Duskova, M.; Bradna, P. Bisphenol A Release from Dental Composites and Resin-Modified Glass Ionomers under Two Polymerization Conditions. Polymers 2021, 14, 46. [Google Scholar] [CrossRef] [PubMed]
- Reichl, F.X.; Esters, M.; Simon, S.; Seiss, M.; Kehe, K.; Kleinsasser, N.; Folwaczny, M.; Glas, J.; Hickel, R. Cell death effects of resin-based dental material compounds and mercurials in human gingival fibroblasts. Arch. Toxicol. 2006, 80, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Sigusch, B.W.; Völpel, A.; Braun, I.; Uhl, A.; Jandt, K.D. Influence of different light curing units on the cytotoxicity of various dental composites. Dent. Mater. 2007, 23, 1342–1348. [Google Scholar] [CrossRef] [PubMed]
- Bhamra, G.S.; Fleming, G.J. Influence of halogen irradiance on short- and long-term wear resistance of resin-based composite materials. Dent. Mater. 2009, 25, 214–220. [Google Scholar] [CrossRef] [PubMed]
- Calheiros, F.C.; Daronch, M.; Rueggeberg, F.A.; Braga, R.R. Degree of conversion and mechanical properties of a BisGMA:TEGDMA composite as a function of the applied radiant exposure. J. Biomed. Mater. Res. B Appl. Biomater. 2008, 84, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Lee, I.B.; Cho, B.H.; Son, H.H.; Um, C.M. Curing effectiveness of a light emitting diode on dentin bonding agents. J. Biomed. Mater. Res. B Appl. Biomater. 2006, 77, 164–170. [Google Scholar] [CrossRef]
- Brambilla, E.; Gagliani, M.; Ionescu, A.; Fadini, L.; García-Godoy, F. The influence of light-curing time on the bacterial colonization of resin composite surfaces. Dent. Mater. 2009, 25, 1067–1072. [Google Scholar] [CrossRef]
- Janda, R.; Roulet, J.F.; Latta, M.; Kaminsky, M.; Rüttermann, S. Effect of exponential polymerization on color stability of resin-based filling materials. Dent. Mater. 2007, 23, 696–704. [Google Scholar] [CrossRef]
- Samaha, S.; Bhatt, S.; Finkelman, M.; Papathanasiou, A.; Perry, R.; Strassler, H.; Kugel, G.; Garcia-Godoy, F.; Price, R. Effect of instruction, light curing unit, and location in the mouth on the energy delivered to simulated restorations. Am. J. Dent. 2017, 30, 343–349. [Google Scholar] [PubMed]
- Szalewski, L.; Wójcik, D.; Sofińska-Chmiel, W.; Kuśmierz, M.; Różyło-Kalinowska, I. How the Duration and Mode of Photopolymerization Affect the Mechanical Properties of a Dental Composite Resin. Materials 2022, 16, 113. [Google Scholar] [CrossRef] [PubMed]
- Diab, R.A.; Yap, A.U.; Gonzalez, M.A.G.; Yahya, N.A. Impact of light-curing distance on the effectiveness of cure of bulk-fill resin-based composites. Saudi Dent. J. 2021, 33, 1184–1189. [Google Scholar] [CrossRef] [PubMed]
- Konerding, K.L.; Heyder, M.; Kranz, S.; Guellmar, A.; Voelpel, A.; Watts, D.C.; Jandt, K.D.; Sigusch, B.W. Study of energy transfer by different light curing units into a class III restoration as a function of tilt angle and distance, using a MARC Patient Simulator (PS). Dent. Mater. 2016, 32, 676–686. [Google Scholar] [CrossRef] [PubMed]
- Kwon, H.J.; Oh, Y.J.; Jang, J.H.; Park, J.E.; Hwang, K.S.; Park, Y.D. The effect of polymerization conditions on the amounts of unreacted monomer and bisphenol A in dental composite resins. Dent. Mater. J. 2015, 34, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Davidson, C.L.; de Gee, A.J. Light-curing units, polymerization, and clinical implications. J. Adhes. Dent. 2000, 2, 167–173. [Google Scholar] [PubMed]
- Ferracane, J.L.; Aday, P.; Matsumoto, H.; Marker, V.A. Relationship between shade and depth of cure for light-activated dental composite resins. Dent. Mater. 1986, 2, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Moore, B.K.; Platt, J.A.; Borges, G.; Chu, T.M.; Katsilieri, I. Depth of cure of dental resin composites: ISO 4049 depth and microhardness of types of materials and shades. Oper. Dent. 2008, 33, 408–412. [Google Scholar] [CrossRef] [PubMed]
- Jain, P.; Pershing, A. Depth of cure and microleakage with high-intensity and ramped resin-based composite curing lights. J. Am. Dent. Assoc. 2003, 134, 1215–1223. [Google Scholar] [CrossRef]
- de Mendonça, B.C.; Soto-Montero, J.R.; de Castro, E.F.; Kury, M.; Cavalli, V.; Rueggeberg, F.A.; Giannini, M. Effect of extended light activation and increment thickness on physical properties of conventional and bulk-filled resin-based composites. Clin. Oral. Investig. 2022, 26, 3141–3150. [Google Scholar] [CrossRef]
- dos Santos, G.B.; Alto, R.V.; Filho, H.R.; da Silva, E.M.; Fellows, C.E. Light transmission on dental resin composites. Dent. Mater. 2008, 24, 571–576. [Google Scholar] [CrossRef]
- MM, A.L.; Haenel, T.; Sullivan, B.; Labrie, D.; Alqahtani, M.Q.; Price, R.B. Effect of a broad-spectrum LED curing light on the Knoop microhardness of four posterior resin based composites at 2, 4 and 6-mm depths. J. Dent. 2016, 45, 14–18. [Google Scholar] [CrossRef]
- De Angelis, F.; Vadini, M.; Capogreco, M.; D’Arcangelo, C.; D’Amario, M. Effect of Light-Sources and Thicknesses of Composite Onlays on Micro-Hardness of Luting Composites. Materials 2021, 14, 6849. [Google Scholar] [CrossRef]
- Ceballos, L.; Fuentes, M.V.; Tafalla, H.; Martínez, A.; Flores, J.; Rodríguez, J. Curing effectiveness of resin composites at different exposure times using LED and halogen units. Med. Oral Patol. Oral Cir. Bucal 2009, 14, E51–E56. [Google Scholar] [PubMed]
- Price, R.B.; Dérand, T.; Loney, R.W.; Andreou, P. Effect of light source and specimen thickness on the surface hardness of resin composite. Am. J. Dent. 2002, 15, 47–53. [Google Scholar] [PubMed]
- Ilie, N.; Ionescu, A.C.; Huth, K.C.; Moldovan, M. Light Transmission Characteristics and Cytotoxicity within A Dental Composite Color Palette. Materials 2023, 16, 3773. [Google Scholar] [CrossRef]
- Sigusch, B.W.; Pflaum, T.; Völpel, A.; Gretsch, K.; Hoy, S.; Watts, D.C.; Jandt, K.D. Resin-composite cytotoxicity varies with shade and irradiance. Dent. Mater. 2012, 28, 312–319. [Google Scholar] [CrossRef] [PubMed]
- Thomé, T.; Steagall, W., Jr.; Tachibana, A.; Braga, S.R.; Turbino, M.L. Influence of the distance of the curing light source and composite shade on hardness of two composites. J. Appl. Oral Sci. 2007, 15, 486–491. [Google Scholar] [CrossRef]
- Busemann, I.; Lipke, C.; Schattenberg, A.; Willershausen, B.; Ernst, C.P. Shortest exposure time possible with LED curing lights. Am. J. Dent. 2011, 24, 37–44. [Google Scholar]
- Emami, N.; Sjödahl, M.; Söderholm, K.J. How filler properties, filler fraction, sample thickness and light source affect light attenuation in particulate filled resin composites. Dent. Mater. 2005, 21, 721–730. [Google Scholar] [CrossRef]
- Masotti, A.S.; Onófrio, A.B.; Conceição, E.N.; Spohr, A.M. UV-vis spectrophotometric direct transmittance analysis of composite resins. Dent. Mater. 2007, 23, 724–730. [Google Scholar] [CrossRef] [PubMed]
- Dieckmann, P.; Mohn, D.; Zehnder, M.; Attin, T.; Tauböck, T.T. Light Transmittance and Polymerization of Bulk-Fill Composite Materials Doped with Bioactive Micro-Fillers. Materials 2019, 12, 4087. [Google Scholar] [CrossRef] [PubMed]
- Ilie, N.; Bucuta, S.; Draenert, M. Bulk-fill resin-based composites: An in vitro assessment of their mechanical performance. Oper. Dent. 2013, 38, 618–625. [Google Scholar] [CrossRef] [PubMed]
- Fujita, K.; Nishiyama, N.; Nemoto, K.; Okada, T.; Ikemi, T. Effect of base monomer’s refractive index on curing depth and polymerization conversion of photo-cured resin composites. Dent. Mater. J. 2005, 24, 403–408. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.K.; Powers, J.M. Influence of background color on the color changes of resin composites after accelerated aging. Am. J. Dent. 2007, 20, 27–30. [Google Scholar] [PubMed]
- Ota, M.; Ando, S.; Endo, H.; Ogura, Y.; Miyazaki, M.; Hosoya, Y. Influence of refractive index on optical parameters of experimental resin composites. Acta Odontol. Scand. 2012, 70, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, T.; Murata, Y.; Sano, H. Translucency of opaque-shade resin composites. Am. J. Dent. 2004, 17, 127–130. [Google Scholar] [PubMed]
- Shortall, A.C.; Wilson, H.J.; Harrington, E. Depth of cure of radiation-activated composite restoratives—Influence of shade and opacity. J. Oral Rehabil. 1995, 22, 337–342. [Google Scholar] [CrossRef] [PubMed]
- Shortall, A.C. How light source and product shade influence cure depth for a contemporary composite. J. Oral Rehabil. 2005, 32, 906–911. [Google Scholar] [CrossRef]
- Hervás-García, A.; Martínez-Lozano, M.A.; Cabanes-Vila, J.; Barjau-Escribano, A.; Fos-Galve, P. Composite resins. A review of the materials and clinical indications. Med. Oral Patol. Oral Cir. Bucal. 2006, 11, E215–E220. [Google Scholar]
- Jafarpour, D.; Ferooz, R.; Ferooz, M.; Bagheri, R. Physical and Mechanical Properties of Bulk-Fill, Conventional, and Flowable Resin Composites Stored Dry and Wet. Int. J. Dent. 2022, 2022, 7946239. [Google Scholar] [CrossRef]
- de Deus, R.A.; Oliveira, L.; Braga, S.; Ribeiro, M.; Price, R.B.; Núñez, A.; Loguercio, A.D.; Soares, C.J. Effect of Radiant Exposure on the Physical and Mechanical Properties of 10 Flowable and High-viscosity Bulk-fill Resin Composites. Oper. Dent. 2024, 49, 136–156. [Google Scholar] [CrossRef]
- Thanoon, H.; Price, R.B.; Watts, D.C. Thermography and conversion of fast-cure composite photocured with quad-wave and laser curing lights compared to a conventional curing light. Dent. Mater. 2024, 40, 546–556. [Google Scholar] [CrossRef]
- Cender, E.U.; Guler, C.; Odabasi, D. The effects of polymerization mode and layer thickness on monomer released from bulk fill composite resins. Niger. J. Clin. Pract. 2021, 24, 1442–1449. [Google Scholar] [CrossRef]
- Naeimi Akbar, H.; Moharamzadeh, K.; Wood, D.J.; Van Noort, R. Relationship between Color and Translucency of Multishaded Dental Composite Resins. Int. J. Dent. 2012, 2012, 708032. [Google Scholar] [CrossRef][Green Version]
- Rueggeberg, F.A.; Cole, M.A.; Looney, S.W.; Vickers, A.; Swift, E.J. Comparison of manufacturer-recommended exposure durations with those determined using biaxial flexure strength and scraped composite thickness among a variety of light-curing units. J. Esthet. Restor. Dent. 2009, 21, 43–61. [Google Scholar] [CrossRef]


| Manufacturer | Composite | Composition |
|---|---|---|
| 3M ESPE, St. Paul, MN, USA | Filtek Supreme XTE | Filler: 72.5 wt.% (55.6 vol.%); zirconium oxide/silicon dioxide cluster (0.6–10 µm) consisting of 20 nm silicon and 4–11 nm zirconium particles, non- agglomerized/non-aggregated silicon nanofillers (20 nm), and zirconium nanofillers (4–11 nm) Matrix: Bis-GMA, BisEMA, UDMA, TEGDMA, PEGDMA |
| Filtek Supreme XTE Flowable | Filler: 65 wt.% (46 vol.%); zirconium oxide/silicon dioxide cluster (0.6–10 µm) consisting of 20 nm silicon, 4–11 nm zirconium particles, ytterbium trifluoride (0.1–0.5 µm), non-agglomerized/non-aggregated surface-modified 20 nm silica filler, and 75 nm silica filler Matrix: Bis-GMA, Bis-EMA, TEGDMA | |
| Ivoclar Vivadent, Schaan, Liechtenstein | Tetric EvoCeram | Filler: 75–76 wt.% (53–55 vol.%) inorganic fillers; barium glass, ytterbium trifluoride, mixed oxide (particle size of the inorganic fillers 40 nm–3000 nm, mean size 550 nm) and prepolymer (34 wt.%) Matrix: BisGMA, UDMA, ethoxylated Bis-EMA |
| Tetric EvoFlow | Filler: 57. wt.% (30.7 vol.%) inorganic fillers; barium glass, ytterbium trifluoride, high-dispersion silicon dioxide, mixed oxide (particle size of the inorganic fillers 40 nm–3000 nm, mean size 550 nm), and prepolymer (20.4 wt.-%) Matrix: Bis-GMA, UDMA, DDDMA | |
| Heraeus Kulzer, Hanau, Germany | Venus Diamond | Filler: 80–82 wt.% (64 vol.%); barium–aluminium fluoride glass, discrete nanoparticles (particle size: 5 nm–20 µm) Matrix: TCD-DI-HEA, UDMA |
| Venus Diamond Flow | Filler: 65 wt.% (41 vol.%); barium–aluminium fluoride silicate glass, ytterbium trifluoride, and silicon dioxide (particle size: 20 nm–5 µm) Matrix: UDMA, EBADMA |
| Composite | Universal | Dentin | Flowable |
|---|---|---|---|
| Filtek Supreme XTE | A1; A2; A3; A4 B2; B3 C2; C3 | A2; A4 | A2; A4 |
| Tetric EvoCeram | A1; A2; A3; A4 B2; B3 C2; C3 | A2; A4 | A2; A4 |
| Venus Diamond | A1; A2; A3; A4 B2; B3 C2; C3 | OL; OD | A2; A4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heyder, M.; Kranz, S.; Beck, J.; Wettemann, M.; Hennig, C.-L.; Schulze-Späte, U.; Sigusch, B.W.; Reise, M. Influence of Layer Thickness and Shade on the Transmission of Light through Contemporary Resin Composites. Materials 2024, 17, 1554. https://doi.org/10.3390/ma17071554
Heyder M, Kranz S, Beck J, Wettemann M, Hennig C-L, Schulze-Späte U, Sigusch BW, Reise M. Influence of Layer Thickness and Shade on the Transmission of Light through Contemporary Resin Composites. Materials. 2024; 17(7):1554. https://doi.org/10.3390/ma17071554
Chicago/Turabian StyleHeyder, Markus, Stefan Kranz, Julius Beck, Marlene Wettemann, Christoph-Ludwig Hennig, Ulrike Schulze-Späte, Bernd W. Sigusch, and Markus Reise. 2024. "Influence of Layer Thickness and Shade on the Transmission of Light through Contemporary Resin Composites" Materials 17, no. 7: 1554. https://doi.org/10.3390/ma17071554
APA StyleHeyder, M., Kranz, S., Beck, J., Wettemann, M., Hennig, C.-L., Schulze-Späte, U., Sigusch, B. W., & Reise, M. (2024). Influence of Layer Thickness and Shade on the Transmission of Light through Contemporary Resin Composites. Materials, 17(7), 1554. https://doi.org/10.3390/ma17071554








