Dentin Bond Strength of Dental Adhesives Functionalized with Polyhedral Oligomeric Silsesquioxanes
Abstract
1. Introduction
2. Materials and Methods
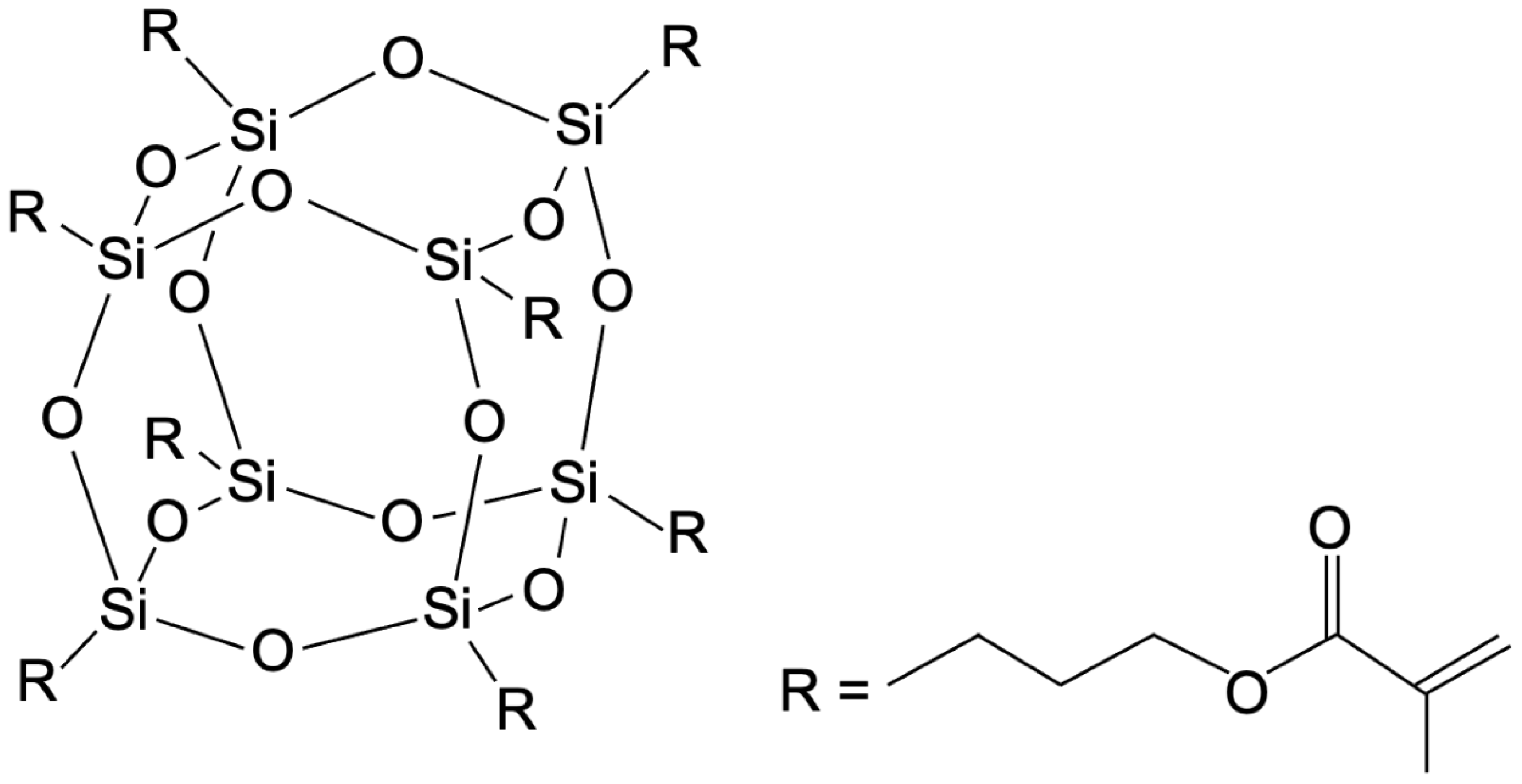
2.1. Adhesive Modification
2.2. Specimen Preparation
2.3. Shear Bond Strength and Failure Mode Analysis
2.4. Statistical Analysis
3. Results
3.1. Shear Bond Strength
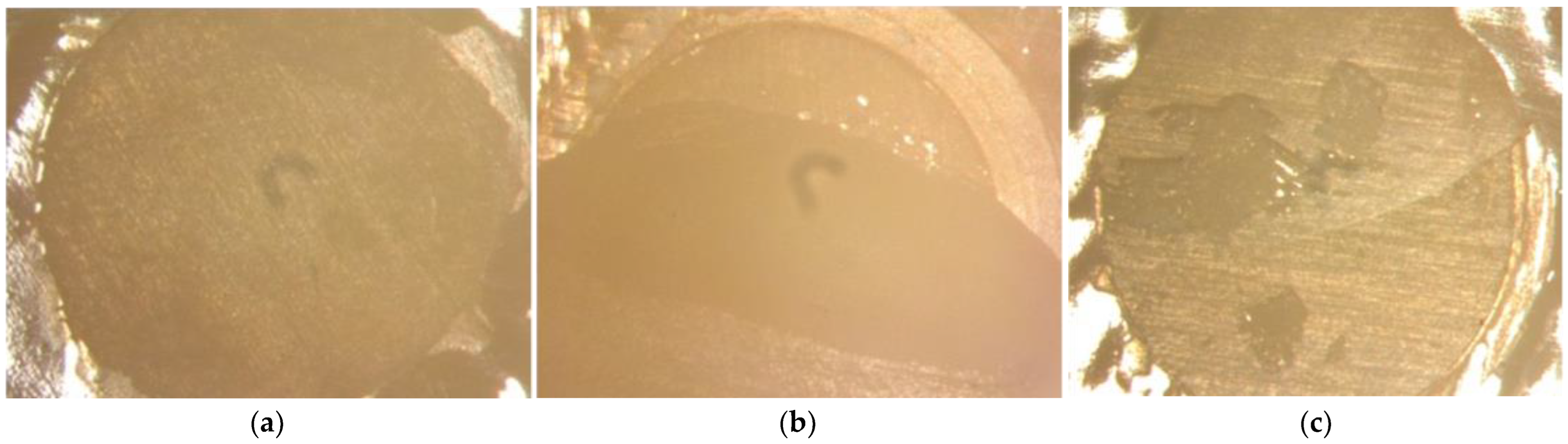
3.2. Failure Mode Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tjäderhane, L.; Nascimento, F.D.; Breschi, L.; Mazzoni, A.; Tersariol, I.L.S.; Geraldeli, S.; Tezvergil-Mutluay, A.; Carrilho, M.; Carvalho, R.M.; Tay, F.R.; et al. Strategies to Prevent Hydrolytic Degradation of the Hybrid Layer-A Review. Dent. Mater. 2013, 29, 999–1011. [Google Scholar] [CrossRef]
- Tjäderhane, L. Dentin Bonding: Can We Make It Last? Oper. Dent. 2015, 40, 4–18. [Google Scholar] [CrossRef]
- Kharouf, N.; Eid, A.; Hardan, L.; Bourgi, R.; Arntz, Y.; Jmal, H.; Foschi, F.; Sauro, S.; Ball, V.; Haikel, Y.; et al. Antibacterial and Bonding Properties of Universal Adhesive Dental Polymers Doped with Pyrogallol. Polymers 2021, 13, 1538. [Google Scholar] [CrossRef]
- Fadaie, P.; Atai, M.; Imani, M.; Karkhaneh, A.; Ghasaban, S. Cyanoacrylate-POSS Nanocomposites: Novel Adhesives with Improved Properties for Dental Applications. Dent. Mater. 2013, 29, e61–e69. [Google Scholar] [CrossRef]
- Tauböck, T.T.; Zehnder, M.; Schweizer, T.; Stark, W.J.; Attin, T.; Mohn, D. Functionalizing a Dentin Bonding Resin to Become Bioactive. Dent. Mater. 2014, 30, 868–875. [Google Scholar] [CrossRef]
- Rizk, M.; Hohlfeld, L.; Thanh, L.T.; Biehl, R.; Lühmann, N.; Mohn, D.; Wiegand, A. Bioactivity and Properties of a Dental Adhesive Functionalized with Polyhedral Oligomeric Silsesquioxanes (POSS) and Bioactive Glass. Dent. Mater. 2017, 33, 1056–1065. [Google Scholar] [CrossRef]
- Ghanbari, H.; Cousins, B.G.; Seifalian, A.M. A Nanocage for Nanomedicine: Polyhedral Oligomeric Silsesquioxane (POSS). Macromol. Rapid Commun. 2011, 32, 1032–1046. [Google Scholar] [CrossRef]
- Lungova, M.; Krutyeva, M.; Pyckhout-Hintzen, W.; Wischnewski, A.; Monkenbusch, M.; Allgaier, J.; Ohl, M.; Sharp, M.; Richter, D. Nanoscale Motion of Soft Nanoparticles in Unentangled and Entangled Polymer Matrices. Phys. Rev. Lett. 2016, 117, 147803. [Google Scholar] [CrossRef] [PubMed]
- Hybrid Plastics Inc. POSS® User’s Guide Version 2.06. Available online: https://www.hybridplastics.com/wp-content/uploads/2015/04/user-v2.06.pdf (accessed on 20 February 2024).
- Wu, X.; Sun, Y.; Xie, W.; Liu, Y.; Song, X. Development of Novel Dental Nanocomposites Reinforced with Polyhedral Oligomeric Silsesquioxane (POSS). Dent. Mater. 2010, 26, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Engstrand, J.; López, A.; Engqvist, H.; Persson, C. Polyhedral Oligomeric Silsesquioxane (POSS)-Poly(Ethylene Glycol) (PEG) Hybrids as Injectable Biomaterials. Biomed. Mater. 2012, 7, 035013. [Google Scholar] [CrossRef] [PubMed]
- Chew, S.L.; Wang, K.; Chai, S.P.; Goh, K.L. Elasticity, Thermal Stability and Bioactivity of Polyhedral Oligomeric Silsesquioxanes Reinforced Chitosan-Based Microfibres. J. Mater. Sci. Mater. Med. 2011, 22, 1365–1374. [Google Scholar] [CrossRef]
- Mousavinasab, S.M.; Atai, M.; Barekatain, M.; Fattahi, P.; Fattahi, A.; Rakhshan, V. Effects of Ethanol Concentrations of Acrylate-Based Dental Adhesives on Microtensile Composite-Dentin Bond Strength and Hybrid Layer Structure of a 10 Wt% Polyhedral Oligomeric Silsesquioxane (POSS)-Incorporated Bonding Agent. Dent. Res. J. 2018, 15, 25–32. [Google Scholar] [CrossRef]
- Rizk, M.; Pohle, A.; Dieckmann, P.; Tauböck, T.T.; Biehl, R.; Wiegand, A. Mineral Precipitation, Polymerization Properties and Bonding Performance of Universal Dental Adhesives Doped with Polyhedral Oligomeric Silsesquioxanes. Int. J. Adhes. Adhes. 2020, 100, 102573. [Google Scholar] [CrossRef]
- Kreutz, M.; Wiegand, A.; Stawarczyk, B.; Lümkemann, N.; Rizk, M. Characterization of Methacrylate-based Resins Containing Methacryl-polyhedral Oligomeric Silsesquioxanes (Ma-poss-8). Materials 2021, 14, 1680. [Google Scholar] [CrossRef]
- Ozimek, J.; Łukaszewska, I.; Pielichowski, K. POSS and SSQ Materials in Dental Applications: Recent Advances and Future Outlooks. Int. J. Mol. Sci. 2023, 24, 4493. [Google Scholar] [CrossRef] [PubMed]
- Van Meerbeek, B.; Yoshihara, K.; Yoshida, Y.; Mine, A.; De Munck, J.; Van Landuyt, K.L. State of the Art of Self-Etch Adhesives. Dent. Mater. 2011, 27, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Van Meerbeek, B.; Peumans, M.; Poitevin, A.; Mine, A.; Van Ende, A.; Neves, A.; De Munck, J. Relationship between Bond-Strength Tests and Clinical Outcomes. Dent. Mater. 2010, 26, e100–e121. [Google Scholar] [CrossRef]
- Hashimoto, M.; Ohno, H.; Sano, H.; Kaga, M.; Oguchi, H. In Vitro Degradation of Resin-Dentin Bonds Analyzed by Microtensile Bond Test, Scanning and Transmission Electron Microscopy. Biomaterials 2003, 24, 3795–3803. [Google Scholar] [CrossRef]
- Carrilho, M.R.O.; Carvalho, R.M.; Tay, F.R.; Pashley, D.H. Effects of Storage Media on Mechanical Properties of Adhesive Systems. Am. J. Dent. 2004, 17, 104–108. [Google Scholar]
- Heintze, S.D. Clinical Relevance of Tests on Bond Strength, Microleakage and Marginal Adaptation. Dent. Mater. 2013, 29, 59–84. [Google Scholar] [CrossRef]
- Kreutz, M.; Kreutz, C.; Kanzow, P.; Tauböck, T.T.; Burrer, P.; Noll, C.; Bader, O.; Rohland, B.; Wiegand, A.; Rizk, M. Effect of Bioactive and Antimicrobial Nanoparticles on Properties and Applicability of Dental Adhesives. Nanomaterials 2022, 12, 3862. [Google Scholar] [CrossRef]
- Feng, D.; Dong, S.; Shi, Z.; Cui, Z.; Zhu, S. Investigation of Aging Resistance for Dental Resin Composites with and without Glass Flakes. Clin. Oral Investig. 2023, 27, 6903–6914. [Google Scholar] [CrossRef] [PubMed]
- Guan, R.; Takagaki, T.; Matsui, N.; Sato, T.; Burrow, M.F.; Palamara, J.; Nikaido, T.; Tagami, J. Dentin Bonding Performance Using Weibull Statistics and Evaluation of Acid-Base Resistant Zone Formation of Recently Introduced Adhesives. Dent. Mater. J. 2016, 35, 684–693. [Google Scholar] [CrossRef] [PubMed]
- Manfroi, F.B.; Marcondes, M.L.; Somacal, D.C.; Borges, G.A.; Júnior, L.H.B.; Spohr, A.M. Bond Strength of a Novel One Bottle Multi-Mode Adhesive to Human Dentin After Six Months of Storage. Open Dent. J. 2016, 10, 268–277. [Google Scholar] [CrossRef] [PubMed]
- Moritake, N.; Takamizawa, T.; Ishii, R.; Tsujimoto, A.; Barkmeier, W.W.; Latta, M.A.; Miyazaki, M. Effect of Active Application on Bond Durability of Universal Adhesives. Oper. Dent. 2019, 44, 188–199. [Google Scholar] [CrossRef] [PubMed]
- Lovell, L.G.; Berchtold, K.A.; Elliott, J.E.; Lu, H.; Bowman, C.N. Understanding the Kinetics and Network Formation of Dimethacrylate Dental Resins. Polym. Adv. Technol. 2001, 12, 335–345. [Google Scholar] [CrossRef]
- Carrilho, E.; Cardoso, M.; Marques Ferreira, M.; Marto, C.M.; Paula, A.; Coelho, A.S. 10-MDP Based Dental Adhesives: Adhesive Interface Characterization and Adhesive Stability-A Systematic Review. Materials 2019, 12, 790. [Google Scholar] [CrossRef]
- Perdigão, J.; Araujo, E.; Ramos, R.Q.; Gomes, G.; Pizzolotto, L. Adhesive Dentistry: Current Concepts and Clinical Considerations. J. Esthet. Restor. Dent. 2021, 33, 51–68. [Google Scholar] [CrossRef]
- Sarner, S. Elektronenoptische Charakterisierung der Hydroxylapatit-Führenden Hybridschicht Im Zahn-Füllungs-Verbund; Georg-August-Universität Göttingen: Göttingen, Germany, 2020. [Google Scholar]
- Mazze, R. Growth of Hydroxyapatite Crystals from Solutions with PH Controlled by Novel Vapor Diffusion Techniques. Effects of Temperature and of the Acidic Phosphoprotein Osteopontin on Crystals Growth. Period. Mineral. 2009, 78, 19–43. [Google Scholar] [CrossRef]
- De Munck, J.; Van Landuyt, K.; Peumans, M.; Poitevin, A.; Lambrechts, P.; Braem, M.; Van Meerbeek, B. A Critical Review of the Durability of Adhesion to Tooth Tissue: Methods and Results. J. Dent. Res. 2005, 84, 118–132. [Google Scholar] [CrossRef]
- Soares, F.Z.M.; Follak, A.; da Rosa, L.S.; Montagner, A.F.; Lenzi, T.L.; Rocha, R.O. Bovine Tooth Is a Substitute for Human Tooth on Bond Strength Studies: A Systematic Review and Meta-Analysis of in Vitro Studies. Dent. Mater. 2016, 32, 1385–1393. [Google Scholar] [CrossRef] [PubMed]
- Muench, A.; da Silva, E.M.; Ballester, R.Y. Influence of Different Dentinal Substrates on the Tensile Bond Strength of Three Adhesive Systems. J. Adhes. Dent. 2000, 2, 209–212. [Google Scholar] [PubMed]
- Braga, R.R.; Meira, J.B.C.; Boaro, L.C.C.; Xavier, T.A. Adhesion to Tooth Structure: A Critical Review of “Macro” Test Methods. Dent. Mater. 2010, 26, e38–e49. [Google Scholar] [CrossRef]
- El Mourad, A.M. Assessment of Bonding Effectiveness of Adhesive Materials to Tooth Structure Using Bond Strength Test Methods: A Review of Literature. Open Dent. J. 2018, 12, 664–678. [Google Scholar] [CrossRef]
- Scherrer, S.S.; Cesar, P.F.; Swain, M.V. Direct Comparison of the Bond Strength Results of the Different Test Methods: A Critical Literature Review. Dent. Mater. 2010, 26, e78–e93. [Google Scholar] [CrossRef]
| Adhesive | LOT | Manufacturer | Components |
|---|---|---|---|
| Scotchbond Universal | 902198 905248 | 3M, St. Paul, MN, USA | 15–25 wt.% 2-hydroxyethyl methacrylate; 15–25 wt.% bisphenol A diglycidyl ether dimethacrylate 10–20 wt.% 2-propenoic acid, 2-methyl-, reaction products with 1,10-decanediol and phosphorus oxide 10–15 wt.% ethanol 10–15 wt.% water 7–13 wt.% 2-propenoic acid, 2-methyl-,3- (trimethoxysilyl)propyl ester, reaction products with vitreous silica 1–5 wt.% copolymer of acrylic and itaconic acid <2 wt.% camphorquinone <2 wt.% dimethylaminobenzoat(-4) <1 wt.% (dimethylamino)ethyl methacrylate |
| Solobond Plus | Primer: 1913352 2117451 Bonding: 1915318 2122279 | VOCO GmbH, Cuxhaven, Germany | Primer: 10–25 wt.% 2-hyydroxyethyl methacrylate 10–25 wt.% acetone 10–25 wt.% hydroxypropylmethacrylate ≤2.5 wt.% catalyst Bonding: 10–25 wt.% bisphenol A-glycidyl methacrylate 10–25 wt.% triethylene glycol dimethacrylate 5–10 wt.% 2-hydroxyethyl methacrylate ≤2.5 wt.% catalyst |
| Parameter | POSS (wt.%) | 24 h Aging | 6 Months Aging | 12 Months Aging | 24 Months Aging |
|---|---|---|---|---|---|
| SBS MPa (mean ± SD) | 0 | 17.4 ± 4.9 aA | 18.2 ± 4.1 aA | 18.7 ± 5.2 bA | 14.6 ± 3.6 aA |
| 5 | 14.3 ± 4.3 aA | 18.3 ± 4.8 aA | 17.3 ± 4.9 abA | 17.9 ± 5.1 bA | |
| 10 | 13.7 ± 4.4 aA | 15.1 ± 4.9 aA | 14.3 ± 3.0 aA | 12.8 ± 4.1 aA | |
| σ0 MPa [95% CI] | 0 | 19.2 [17.2–21.5] | 19.8 [18.2–21.6] | 20.7 [18.5–23.1] | 15.9 [14.4–17.6] |
| 5 | 15.9 [14.1–17.9] | 20.2 [18.0–22.6] | 19.2 [16.9–21.8] | 19.8 [17.5–22.4] | |
| 10 | 15.3 [13.3–17.5] | 16.8 [14.6–19.2] | 15.5 [14.1–16.9] | 14.2 [12.5–16.1] | |
| m [95% CI] | 0 | 4.1 [2.9–5.9] | 5.4 [3.8–7.6] | 4.1 [2.9–5.8] | 4.6 [3.3–6.4] |
| 5 | 3.8 [2.7–5.4] | 4.0 [2.9–5.5] | 3.7 [2.7–5.0] | 3.8 [2.7–5.2] | |
| 10 | 3.4 [2.5–4.7] | 3.4 [2.4–4.7] | 5.1 [3.7–7.0] | 3.7 [2.6–5.2] | |
| Failure mode % (adhesive; cohesive; mixed) | 0 | 25; 35; 40 | 20; 30; 50 | 15; 45; 40 | 65; 10; 25 |
| 5 | 15; 10; 75 | 20; 20; 60 | 15; 30; 55 | 25; 50; 25 | |
| 10 | 10; 15; 75 | 25; 25; 50 | 10; 5; 85 | 70; 5; 25 |
| Parameter | POSS (wt.%) | 24 h Aging | 6 Months Aging | 12 Months Aging | 24 Months Aging |
|---|---|---|---|---|---|
| SBS MPa (mean ± SD) | 0 | 19.1 ± 5.2 aA | 25.8 ± 4.4 aB | 25.1 ± 3.0 aB | 23.6 ± 4.6 aB |
| 5 | 20.0 ± 4.6 aA | 24.2 ± 5.4 aB | 24.8 ± 4.4 aB | 23.9 ± 3.8 aB | |
| 10 | 18.6 ± 4.1 aA | 22.2 ± 4.8 aAB | 24.2 ± 4.1 aB | 21.8 ± 6.3 aAB | |
| σ0 MPa [95% CI] | 0 | 21.0 [18.8–23.3] | 27.7 [25.8–29.7] | 26.4 [25.2–27.6] | 25.5 [23.7–27.4] |
| 5 | 21.7 [20.0–23.5] | 26.2 [24.1–28.6] | 26.7 [24.8–28.7] | 25.4 [23.9–27.0] | |
| 10 | 20.2 [18.5–22.0] | 24.0 [22.0–26.1] | 25.9 [24.3–27.7] | 23.8 [21.6–26.3] | |
| m [95% CI] | 0 | 4.3 [3.1–6.1] | 6.6 [4.7–9.2] | 10.2 [7.2–14.6] | 6.2 [4.4–8.9] |
| 5 | 5.8 [3.9–8.4] | 5.4 [3.8–7.7] | 6.3 [4.6–8.8] | 7.6 [5.4–10.5] | |
| 10 | 5.3 [3.8–7.4] | 5.5 [3.9–7.6] | 7.0 [4.9–9.8] | 4.6 [3.1–6.8] | |
| Failure mode % (adhesive; cohesive; mixed) | 0 | 5; 75; 20 | 0; 70; 30 | 0; 75; 25 | 0; 70; 30 |
| 5 | 0; 85; 15 | 0; 80; 20 | 0; 55; 45 | 0; 85; 15 | |
| 10 | 0; 90; 10 | 0; 80; 20 | 0; 90; 10 | 0; 70; 30 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Biermann, J.; Bień, C.E.; Lechte, C.; Kanzow, P.; Wiegand, A. Dentin Bond Strength of Dental Adhesives Functionalized with Polyhedral Oligomeric Silsesquioxanes. Materials 2024, 17, 1321. https://doi.org/10.3390/ma17061321
Biermann J, Bień CE, Lechte C, Kanzow P, Wiegand A. Dentin Bond Strength of Dental Adhesives Functionalized with Polyhedral Oligomeric Silsesquioxanes. Materials. 2024; 17(6):1321. https://doi.org/10.3390/ma17061321
Chicago/Turabian StyleBiermann, Jana, Charlyn Elise Bień, Clemens Lechte, Philipp Kanzow, and Annette Wiegand. 2024. "Dentin Bond Strength of Dental Adhesives Functionalized with Polyhedral Oligomeric Silsesquioxanes" Materials 17, no. 6: 1321. https://doi.org/10.3390/ma17061321
APA StyleBiermann, J., Bień, C. E., Lechte, C., Kanzow, P., & Wiegand, A. (2024). Dentin Bond Strength of Dental Adhesives Functionalized with Polyhedral Oligomeric Silsesquioxanes. Materials, 17(6), 1321. https://doi.org/10.3390/ma17061321







