Effectiveness of Self-Adhesive Resin Luting Cement in CAD-CAM Blocks—A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Databases and Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Quality Assessment Protocol
2.4. Data Extraction Workflow
2.5. Meta-Analysis
3. Results
3.1. General Aspects
3.2. BIAS Risk Assessment
3.3. Descriptive Data
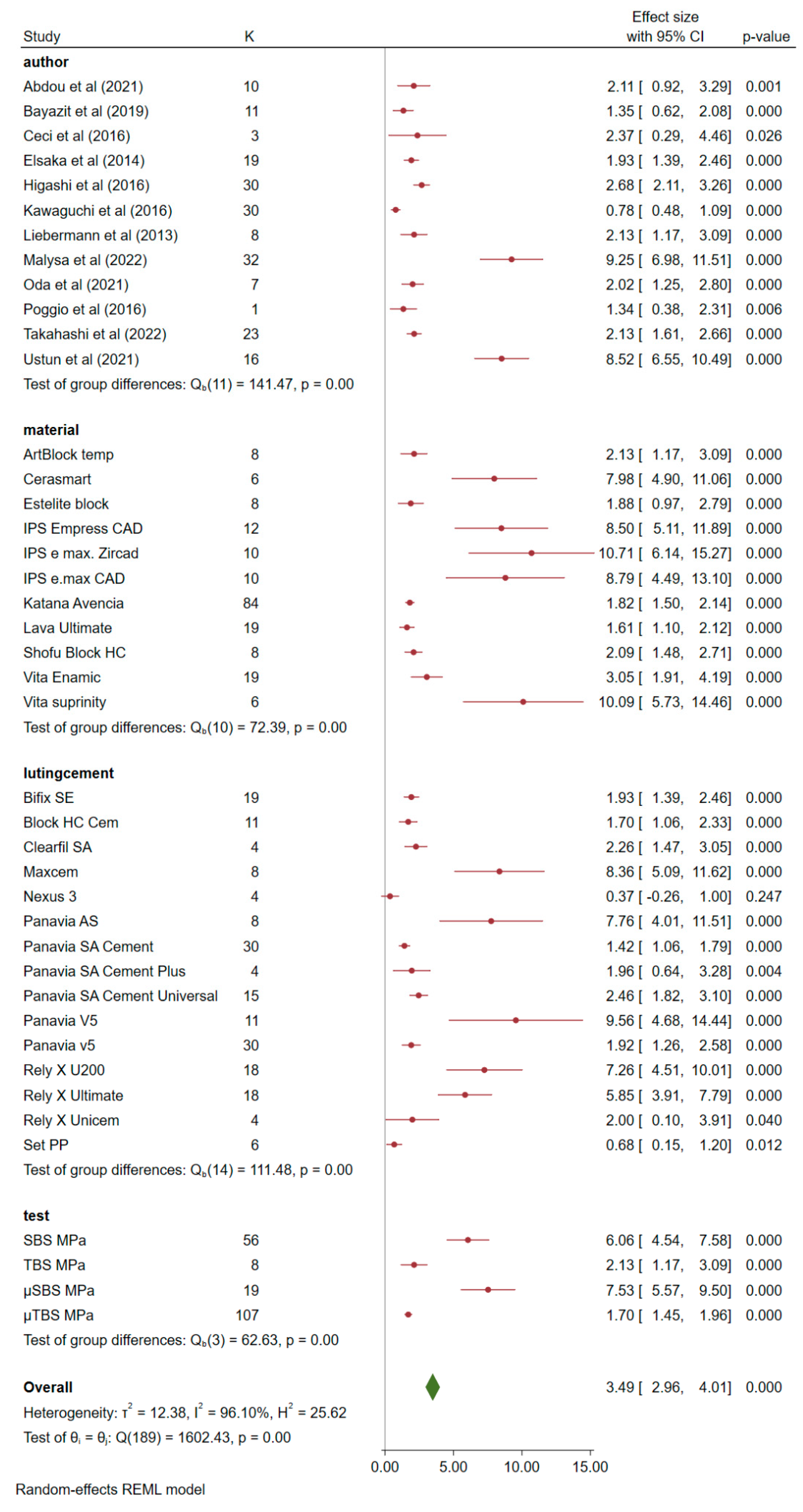
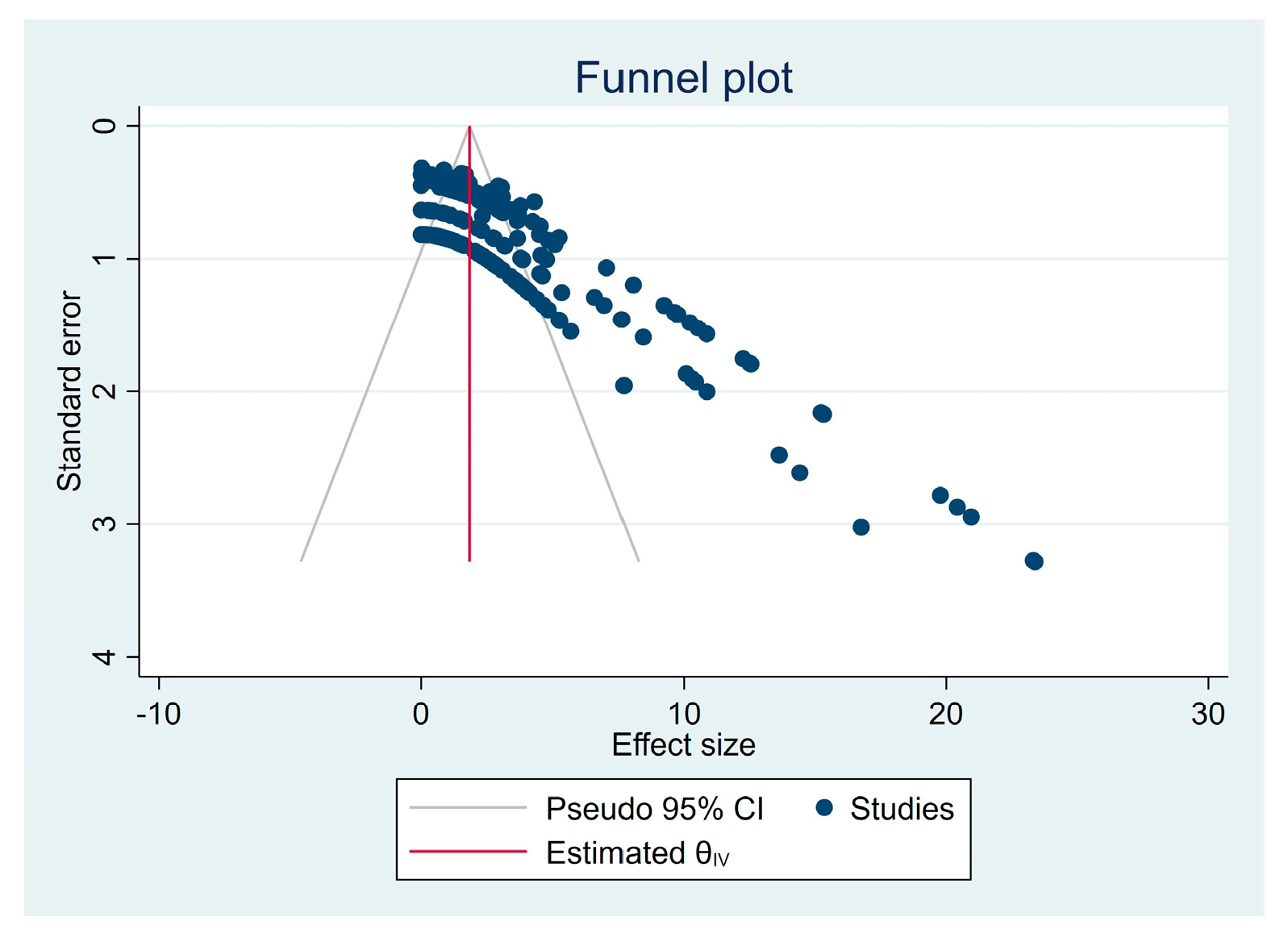
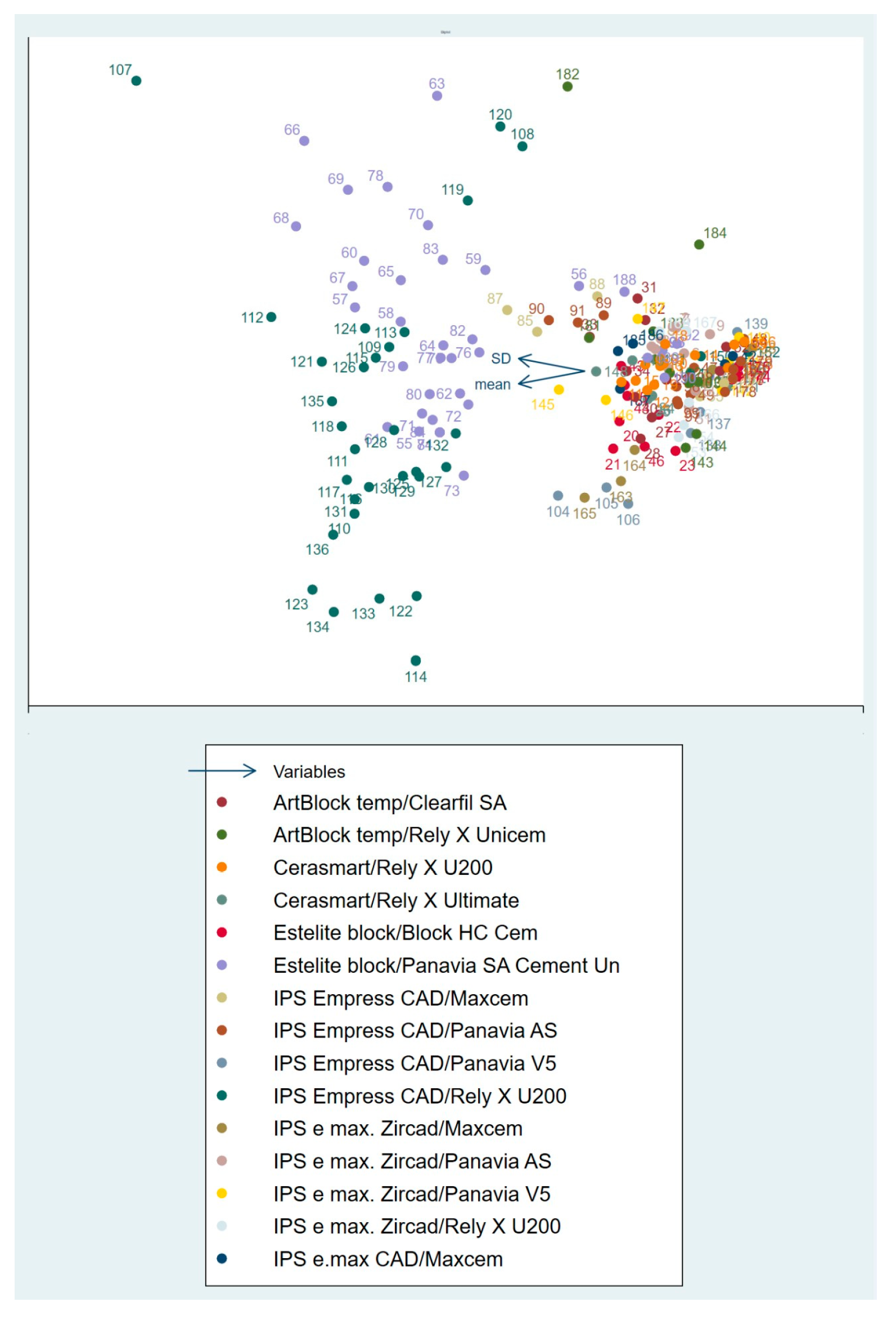
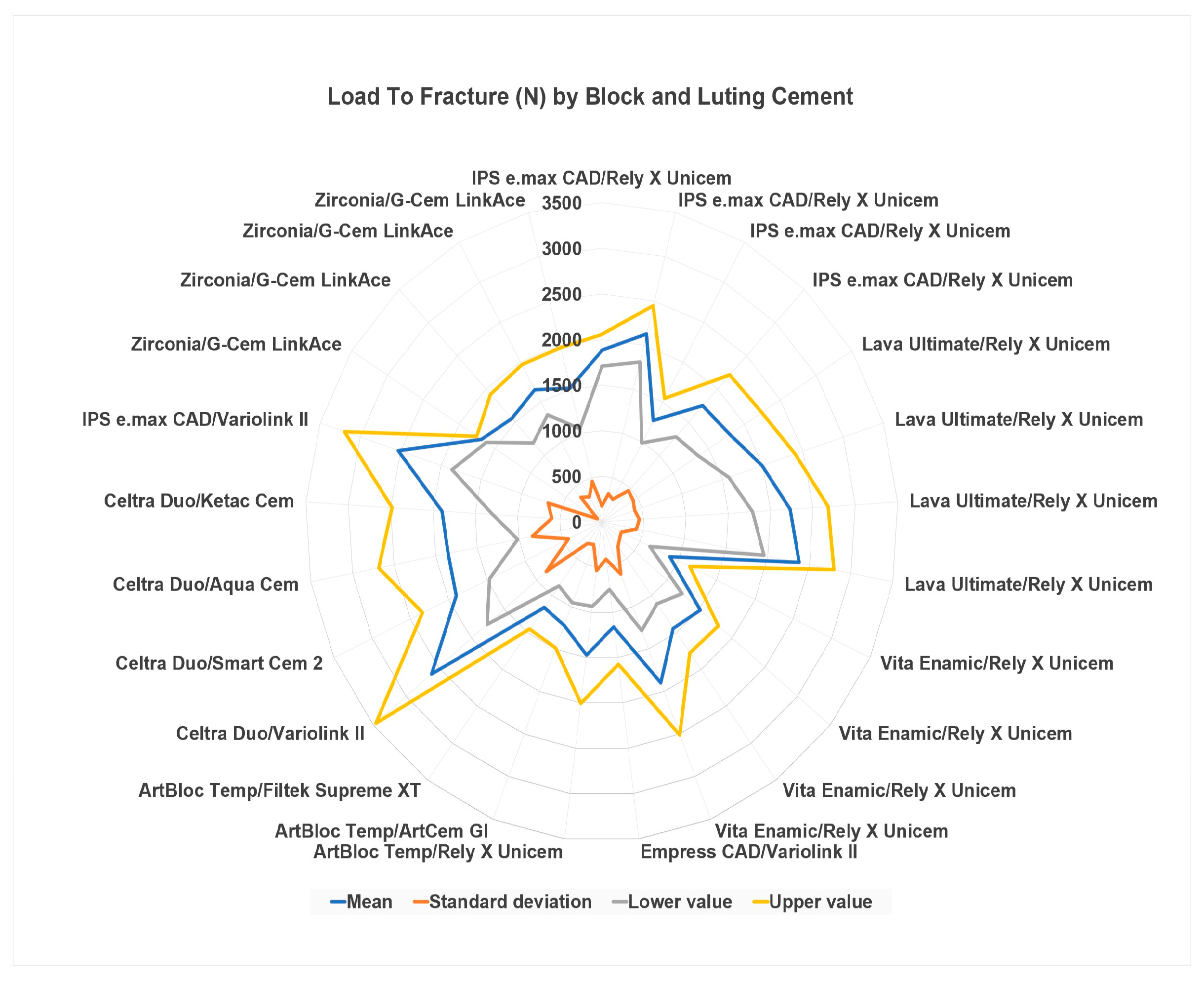
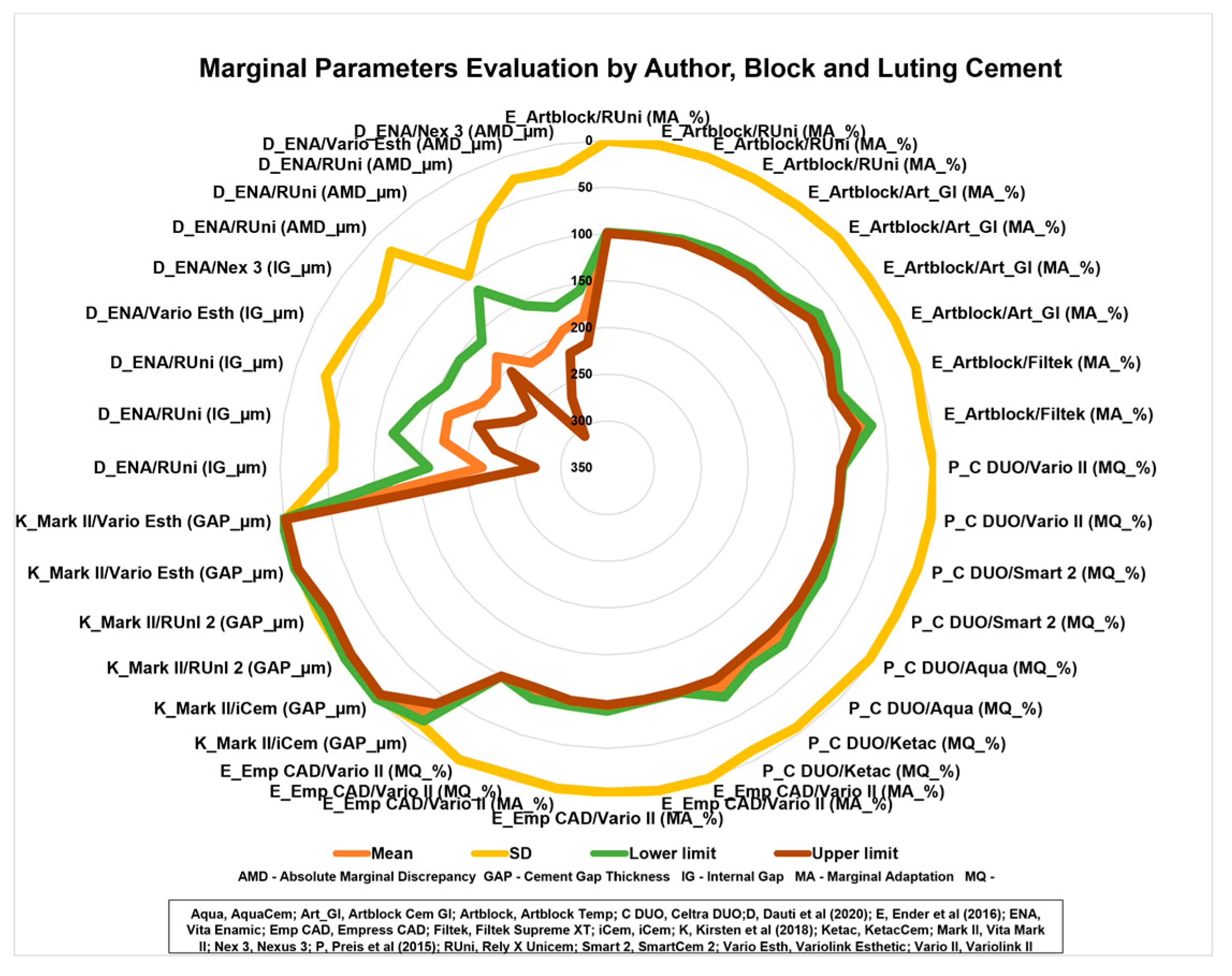
3.4. Meta-Analysis
4. Discussion
4.1. Surface Treatment
4.2. Interaction between Substrates
4.3. Adhesive Strategy
4.4. Coupling Agents
4.5. Dimensions of the Interface and Marginal Adaptation
4.6. Toxicity and Aging
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Higashi, M.; Matsumoto, M.; Kawaguchi, A.; Miura, J.; Minamino, T.; Kabetani, T.; Takeshige, F.; Mine, A.; Yatani, H. Bonding effectiveness of self-adhesive and conventional-type adhesive resin cements to CAD/CAM resin blocks. Part 1: Effects of sandblasting and silanization. Dent. Mater. J. 2016, 35, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Liebermann, A.; Keul, C.; Bähr, N.; Edelhoff, D.; Eichberger, M.; Roos, M.; Stawarczyk, B. Impact of plasma treatment of PMMA-based CAD/CAM blanks on surface properties as well as on adhesion to self-adhesive resin composite cements. Dent. Mater. 2013, 29, 935–944. [Google Scholar] [CrossRef] [PubMed]
- Ender, A.; Bienz, S.; Mörmann, W.; Mehl, A.; Attin, T.; Stawarczyk, B. Marginal adaptation, fracture load and macroscopic failure mode of adhesively luted PMMA-based CAD/CAM inlays. Dent. Mater. 2016, 32, e22–e29. [Google Scholar] [CrossRef] [PubMed]
- Preis, V.; Behr, M.; Hahnel, S.; Rosentritt, M. Influence of cementation on in vitro performance, marginal adaptation and fracture resistance of CAD/CAM-fabricated ZLS molar crowns. Dent. Mater. 2015, 31, 1363–1369. [Google Scholar] [CrossRef]
- Dauti, R.; Lilaj, B.; Heimel, P.; Moritz, A.; Schedle, A.; Cvikl, B. Influence of two different cement space settings and three different cement types on the fit of polymer-infiltrated ceramic network material crowns manufactured using a complete digital workflow. Clin. Oral Investig. 2020, 24, 1929–1938. [Google Scholar] [CrossRef]
- Poggio, C.; Pigozzo, M.; Ceci, M.; Scribante, A.; Beltrami, R.; Chiesa, M. Influence of different luting protocols on shear bond strength of computer aided design/computer aided manufacturing resin nanoceramic material to dentin. Dent. Res. J. 2016, 13, 91–97. [Google Scholar] [CrossRef]
- Abdou, A.; Takahashi, R.; Saad, A.; Nozaki, K.; Nikaido, T.; Tagami, J. Influence of resin-coating on bond strength of resin cements to dentin and CAD/CAM resin block in single-visit and multiple-visit treatment. Dent. Mater. J. 2021, 40, 674–682. [Google Scholar] [CrossRef]
- Bayazıt, E. Microtensile Bond Strength of Self-Adhesive Resin Cements to CAD/CAM Resin-Matrix Ceramics Prepared with Different Surface Treatments. Int. J. Prosthodont. 2019, 32, 433–438. [Google Scholar] [CrossRef]
- Ceci, M.; Pigozzo, M.; Scribante, A.; Beltrami, R.; Colombo, M.; Chiesa, M.; Poggio, C. Effect of glycine pretreatment on the shear bond strength of a CAD/CAM resin nano ceramic material to dentin. J. Clin. Exp. Dent. 2016, 8, e146–e152. [Google Scholar] [CrossRef]
- Kawaguchi, A.; Matsumoto, M.; Higashi, M.; Miura, J.; Minamino, T.; Kabetani, T.; Takeshige, F.; Mine, A.; Yatani, H. Bonding effectiveness of self-adhesive and conventional-type adhesive resin cements to CAD/CAM resin blocks. Part 2: Effect of ultrasonic and acid cleaning. Dent. Mater. J. 2016, 35, 29–36. [Google Scholar] [CrossRef]
- Calheiros-Lobo, M.J.; Carbas, R.; da Silva, L.F.M.; Pinho, T. Impact of in vitro findings on clinical protocols for the adhesion of CAD-CAM blocks: A systematic integrative review and meta-analysis. J. Prosthet. Dent. 2022, in press. [CrossRef] [PubMed]
- Saravi, B.; Vollmer, A.; Hartmann, M.; Lang, G.; Kohal, R.J.; Boeker, M.; Patzelt, S.B.M. Clinical Performance of CAD/CAM All-Ceramic Tooth-Supported Fixed Dental Prostheses: A Systematic Review and Meta-Analysis. Materials 2021, 14, 2672. [Google Scholar] [CrossRef] [PubMed]
- Skorulska, A.; Piszko, P.; Rybak, Z.; Szymonowicz, M.; Dobrzyński, M. Review on Polymer, Ceramic and Composite Materials for CAD/CAM Indirect Restorations in Dentistry-Application, Mechanical Characteristics and Comparison. Materials 2021, 14, 1592. [Google Scholar] [CrossRef] [PubMed]
- Nagasawa, Y.; Eda, Y.; Shigeta, H.; Ferrari, M.; Nakajima, H.; Hibino, Y. Effect of sandblasting and/or priming treatment on the shear bond strength of self-adhesive resin cement to CAD/CAM blocks. Odontology 2022, 110, 70–80. [Google Scholar] [CrossRef]
- Heboyan, A.; Vardanyan, A.; Karobari, M.I.; Marya, A.; Avagyan, T.; Tebyaniyan, H.; Mustafa, M.; Rokaya, D.; Avetisyan, A. Dental Luting Cements: An Updated Comprehensive Review. Molecules 2023, 28, 1619. [Google Scholar] [CrossRef]
- Zhao, Z.; Wang, Q.; Zhao, J.; Zhao, B.; Ma, Z.; Zhang, C. Adhesion of Teeth. Front. Mater. 2021, 7, e615225. [Google Scholar] [CrossRef]
- Mine, A.; Kabetani, T.; Kawaguchi-Uemura, A.; Higashi, M.; Tajiri, Y.; Hagino, R.; Imai, D.; Yumitate, M.; Ban, S.; Matsumoto, M.; et al. Effectiveness of current adhesive systems when bonding to CAD/CAM indirect resin materials: A review of 32 publications. Jpn. Dent. Sci. Rev. 2019, 55, 41–50. [Google Scholar] [CrossRef]
- Moura, D.M.D.; Veríssimo, A.H.; Leite Vila-Nova, T.E.; Calderon, P.S.; Özcan, M.; Assunção Souza, R.O. Which surface treatment promotes higher bond strength for the repair of resin nanoceramics and polymer-infiltrated ceramics? A systematic review and meta-analysis. J. Prosthet. Dent. 2022, 128, 139–149. [Google Scholar] [CrossRef]
- May, M.M.; Fraga, S.; May, L.G. Effect of milling, fitting adjustments, and hydrofluoric acid etching on the strength and roughness of CAD-CAM glass-ceramics: A systematic review and meta-analysis. J. Prosthet. Dent. 2022, 128, 1190–1200. [Google Scholar] [CrossRef]
- da Rosa, L.S.; Dapieve, K.S.; Dalla-Nora, F.; Rippe, M.P.; Valandro, L.F.; Sarkis-Onofre, R.; Pereira, G.K.R. Does adhesive luting reinforce the mechanical properties of dental ceramics used as restorative materials? A systematic review and meta-analysis. J. Adhes. Dent. 2022, 24, 209–222. [Google Scholar] [CrossRef]
- Alsaeed, A.Y. Bonding CAD/CAM materials with current adhesive systems: An overview. Saudi Dent. J. 2022, 34, 259–269. [Google Scholar] [CrossRef] [PubMed]
- Melo Freire, C.A.; Borges, G.A.; Caldas, D.; Santos, R.S.; Ignácio, S.A.; Mazur, R.F. Marginal Adaptation and Quality of Interfaces in Lithium Disilicate Crowns-Influence of Manufacturing and Cementation Techniques. Oper. Dent. 2017, 42, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Perdigão, J. Current perspectives on dental adhesion: (1) Dentin adhesion-not there yet. Jpn. Dent. Sci. Rev. 2020, 56, 190–207. [Google Scholar] [CrossRef] [PubMed]
- Federlin, M.; Hiller, K.A.; Schmalz, G. Effect of selective enamel etching on clinical performance of CAD/CAM partial ceramic crowns luted with a self-adhesive resin cement. Clin. Oral Investig. 2014, 18, 1975–1984. [Google Scholar] [CrossRef]
- Oda, Y.; Takahashi, R.; Nikaido, T.; Tagami, J. Influence of the resin-coating technique on the bonding performance of self-adhesive resin cements in single-visit computer-aided design/computer-aided manufacturing resin restorations. J. Esthet. Restor. Dent. 2021, 34, 721–728. [Google Scholar] [CrossRef]
- Kirsten, M.; Matta, R.E.; Belli, R.; Lohbauer, U.; Wichmann, M.; Petschelt, A.; Zorzin, J. Hygroscopic expansion of self-adhesive resin cements and the integrity of all-ceramic crowns. Dent. Mater. 2018, 34, 1102–1111. [Google Scholar] [CrossRef]
- Ustun, S.; Ayaz, E.A. Effect of different cement systems and aging on the bond strength of chairside CAD-CAM ceramics. J. Prosthet. Dent. 2021, 125, 334–339. [Google Scholar] [CrossRef]
- Han, S.H.; Shimada, Y.; Sadr, A.; Tagami, J.; Kum, K.Y.; Park, S.H. Effect of Pretreatment and Activation Mode on the Interfacial Adaptation of Nanoceramic Resin Inlay and Self-adhesive Resin Cement. Dent. Mater. 2020, 36, 1170–1182. [Google Scholar] [CrossRef]
- Fidalgo-Pereira, R.; Carpio, D.; Torres, O.; Carvalho, O.; Silva, F.; Henriques, B.; Özcan, M.; Souza, J.C.M. The influence of inorganic fillers on the light transmission through resin-matrix composites during the light-curing procedure: An integrative review. Clin. Oral Investig. 2022, 26, 5575–5594. [Google Scholar] [CrossRef]
- Zhang, C.Y.; Cheng, Y.L.; Tong, X.W.; Yu, H.; Cheng, H. In Vitro Cytotoxicity of Self-Adhesive Dual-Cured Resin Cement Polymerized Beneath Three Different Cusp Inclinations of Zirconia. Biomed. Res. Int. 2019, 2019, 7404038. [Google Scholar] [CrossRef]
- Albelasy, E.; Hamama, H.H.; Tsoi, J.K.H.; Mahmoud, S.H. Influence of material type, thickness and storage on fracture resistance of CAD/CAM occlusal veneers. J. Mech. Behav. Biomed. Mater. 2021, 119, 104485. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Ali, A.O.; Kelly, J.R.; Zandparsa, R. The influence of different convergence angles and resin cements on the retention of zirconia copings. J. Prosthodont. 2012, 21, 614–621. [Google Scholar] [CrossRef]
- Augusti, D.; Augusti, G.; Re, D. Undetected Excess Cement at Marginal Areas of Zirconia Crown Copings: In Vitro Analysis of Two Luting Agents and Their Influence on Retention. Int. J. Prosthodont. 2020, 33, 202–211. [Google Scholar] [CrossRef]
- Elsaka, S.E. Bond strength of novel CAD/CAM restorative materials to self-adhesive resin cement: The effect of surface treatments. J. Adhes. Dent. 2014, 16, 531–540. [Google Scholar] [CrossRef] [PubMed]
- Magne, P.; Carvalho, A.O.; Bruzi, G.; Giannini, M. Fatigue resistance of ultrathin CAD/CAM complete crowns with a simplified cementation process. J. Prosthet. Dent. 2015, 114, 574–579. [Google Scholar] [CrossRef]
- Malysa, A.; Wezgowiec, J.; Grzebieluch, W.; Danel, D.P.; Wieckiewicz, M. Effect of Thermocycling on the Bond Strength of Self-Adhesive Resin Cements Used for Luting CAD/CAM Ceramics to Human Dentin. Int. J. Mol. Sci. 2022, 23, 745. [Google Scholar] [CrossRef]
- Nagasawa, Y.; Hibino, Y.; Eda, Y.; Nakajima, H. Effect of surface treatment of CAD/CAM resin composites on the shear bond strength of self-adhesive resin cement. Dent. Mater. J. 2021, 40, 364–378. [Google Scholar] [CrossRef]
- Nakamura, K.; Mouhat, M.; Nergård, J.M.; Lægreid, S.J.; Kanno, T.; Milleding, P.; Örtengren, U. Effect of cements on fracture resistance of monolithic zirconia crowns. Acta Biomater. Odontol. Scand. 2016, 2, 12–19. [Google Scholar] [CrossRef]
- Peumans, M.; Valjakova, E.B.; De Munck, J.; Mishevska, C.B.; Van Meerbeek, B. Bonding Effectiveness of Luting Composites to Different CAD/CAM Materials. J. Adhes. Dent. 2016, 18, 289–302. [Google Scholar] [CrossRef]
- Sorrentino, R.; Triulzio, C.; Tricarico, M.G.; Bonadeo, G.; Gherlone, E.F.; Ferrari, M. In vitro analysis of the fracture resistance of CAD-CAM monolithic zirconia molar crowns with different occlusal thickness. J. Mech. Behav. Biomed. Mater. 2016, 61, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, N.; Kurokawa, H.; Wakamatsu, K.; Hirokane, E.; Takamizawa, T.; Miyazaki, M.; Kitahara, N. Bonding ability of resin cements to different types of CAD/CAM composite blocks. Dent. Mater. J. 2022, 41, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Zahoui, A.; Bergamo, E.T.; Marun, M.M.; Silva, K.P.; Coelho, P.G.; Bonfante, E.A. Cementation Protocol for Bonding Zirconia Crowns to Titanium Base CAD/CAM Abutments. Int. J. Prosthodont. 2020, 33, 527–535. [Google Scholar] [CrossRef]
- Yoshihara, K.; Nagaoka, N.; Maruo, Y.; Nishigawa, G.; Yoshida, Y.; Van Meerbeek, B. Silane-coupling effect of a silane-containing self-adhesive composite cement. Dent. Mater. 2020, 36, 914–926. [Google Scholar] [CrossRef] [PubMed]
- Manso, A.P.; Carvalho, R.M. Dental Cements for Luting and Bonding Restorations: Self-Adhesive Resin Cements. Dent. Clin. N. Am. 2017, 61, 821–834. [Google Scholar] [CrossRef]
- Şişmanoğlu, S.; Demirci, M.; Schweikl, H.; Ozen-Eroglu, G.; Cetin-Aktas, E.; Kuruca, S.; Tuncer, S.; Tekce, N. Cytotoxic effects of different self-adhesive resin cements: Cell viability and induction of apoptosis. J. Adv. Prosthodont. 2020, 12, 89–99. [Google Scholar] [CrossRef]
- Canatan, S.; Oz, F.D.; Bolay, S. A randomized, controlled clinical evaluation of two resin cement systems in the adhesion of CAD/CAM-fabricated resin nanoceramic restorations: 18-month preliminary results. J. Esthet. Restor. Dent. 2022, 34, 1005–1014. [Google Scholar] [CrossRef]
- Scholz, K.J.; Tabenski, I.M.; Vogl, V.; Cieplik, F.; Schmalz, G.; Buchalla, W.; Hiller, K.A.; Federlin, M. Randomized clinical split-mouth study on the performance of CAD/CAM-partial ceramic crowns luted with a self-adhesive resin cement or a universal adhesive and a conventional resin cement after 39 months. J. Dent. 2021, 115, 103837. [Google Scholar] [CrossRef]
- Ghodsi, S.; Arzani, S.; Shekarian, M.; Aghamohseni, M. Cement selection criteria for full coverage restorations: A comprehensive review of literature. J. Clin. Exp. Dent. 2021, 13, e1154–e1161. [Google Scholar] [CrossRef]
- Leung, G.K.; Wong, A.W.; Chu, C.H.; Yu, O.Y. Update on Dental Luting Materials. Dent. J. 2022, 10, 208. [Google Scholar] [CrossRef]
- Zhang, C.Y.; Yu, H.; Tong, X.W.; Cheng, H. Effects of Cusp Inclination and Light-curing Time on Microshear Bond Strength of a Dual-cure, Self-adhesive Composite Cement to Zirconia. J. Adhes. Dent. 2018, 20, 107–112. [Google Scholar] [CrossRef] [PubMed]
- de Carvalho, M.F.F.; Leijôto-Lannes, A.C.N.; Rodrigues, M.C.N.; Nogueira, L.C.; Ferraz, N.K.L.; Moreira, A.N.; Yamauti, M.; Zina, L.G.; Magalhães, C.S. Viability of Bovine Teeth as a Substrate in Bond Strength Tests: A Systematic Review and Meta-analysis. J. Adhes. Dent. 2018, 20, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Soares, F.Z.; Follak, A.; da Rosa, L.S.; Montagner, A.F.; Lenzi, T.L.; Rocha, R.O. Bovine tooth is a substitute for human tooth on bond strength studies: A systematic review and meta-analysis of in vitro studies. Dent. Mater. 2016, 32, 1385–1393. [Google Scholar] [CrossRef] [PubMed]


| Study | Abdou et al. (2021) [7] | Albelasy et al. (2021) [31] | Ali et al. (2012) [33] | Augusti et al. (2020) [34] | Bayazit et al. (2019) [8] | Ceci et al. (2016) [9] | Dauti et al. (2020) [5] | Elsaka et al. (2014) [35] | Ender et al. (2016) [3] | Melo Freire et al. (2017) [22] | Han et al. (2020) [28] | Higashi et al. (2016) [1] | Kawaguchi et al. (2016) [10] | Kirsten et al. (2018) [26] | Liebermann et al. (2013) [2] | Magne et al. (2015) [36] | Malysa et al. (2022) [37] | Nagasawa et al. (2021) [38] | Nagasawa et al. (2022) [14] | Nakamura et al. (2016) [39] | Oda et al. (2021) [25] | Peumans et al. (2016) [40] | Poggio et al. (2016) [6] | Preis et al. (2015) [4] | Sorrentino et al. (2016) [42] | Takahashi et al. (2022) [43] | Ustun et al. (2021) [27] | Zahoui et al. (2020) [44] | Zhang et al. (2018) [30] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Specimen Randomization | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 |
| Single Operator | 2 | 2 | 0 | 0 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 2 |
| Operator Blinded | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Standardized Specimens | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Control Group | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 0 | 0 | 2 | 0 | 0 | 0 | 2 | 0 | 2 | 0 | 0 | 0 | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 0 | 2 |
| Fractographic analysis | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 |
| Manufacturer’s Instructions | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Sample Size Calculation | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 0 | 0 | 2 | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 2 | 2 |
| International Standards | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 |
| Proper statistical analysis | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| TOTAL | 8 | 9 | 5 | 4 | 5 | 5 | 6 | 7 | 2 | 9 | 5 | 7 | 5 | 9 | 10 | 10 | 5 | 6 | 8 | 8 | 9 | 5 | 7 | 6 | 9 | 10 | 10 | 10 | 9 |
| Risk of Bias | M | M | M | L | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M | M |
| Journal SJR score by date of publication | Q2 | Q2 | Q2 | Q2 | Q2 | Q2 | Q1 | Q2 | Q1 | Q1 | Q1 | Q1 | Q1 | Q1 | Q1 | Q2 | Q1 | Q2 | Q1 | Q1 | Q1 | Q1 | Q3 | Q1 | Q1 | Q2 | Q1 | Q2 | Q2 |
| Author, Year | Material | Sample Pairing | Type of Test | Surface Treatment | Coupling Agent | Adhesive System | Luting Cement |
|---|---|---|---|---|---|---|---|
| Abdou et al. (2021) [7] | Katana Avencia | Bovine incisors (n = 15) | μTBS | 50 μm Al2O3 37.5% PA | Kerr Silane primer SB-UA Clearfil Universal Bond Quick | Clearfil Universal Bond Quick SB-UA Optibond all-in-one | Panavia V5 Rely X Ultimate NX3 Nexus |
| Albelasy et al. (2021) [31] | IPS. e max CAD Vita Enamic Lava Ultimate | Human molars (n = 14) | Ultimate fracture test; thermocycling failure pattern | 50 μm Al2O3 8% HF 37% PA | Dentobond Silane | N/A | Rely X Unicem |
| Ali et al. (2012) [33] | Zirconia | Human molars (n = 12) | Load-to-fracture; thermocycling | 50 μm Al2O3 | N/A | ED primer | Panavia F 2.0 Rely X Unicem Clearfil SA |
| Augusti et al. (2020) [34] | Zirconia | Zirconia abutments (n = 10) | Pull-out test | 50 μm Al2O3 | N/A | N/A | Rely X Unicem 2 |
| Bayazit et al. (2019) [8] | Lava Ultimate Vita Enamic | Blocks (n = 15) | μTBS | 50 μm Al2O3 9.5% HF | N/A | SB-UA | Rely X U200 Set PP |
| Ceci et al. (2016) [9] | Lava Ultimate | Bovine incisors (n = 10) | μSBS | 50 μm Al2O3 35% PA Clinpro powder (glycine) | SB-UA | SB-UA | Rely X Ultimate Rely X Unicem 2 |
| Elsaka et al. (2014) [35] | Vita Enamic Lava Ultimate | Composite resin block (n = 3) | μTBS; aging | 50 μm Al2O3 9.5% HF | Silane | N/A | Bifix SE |
| Ender et al. (2016) [3] | IPS. Empress CAD ArtBlock Temp | Human molars (n = 12) | SBS | 50 μm Al2O3 | Monobond Plus | Heliobond | Rely X Unicem Variolink II |
| Higashi et al. (2016) [1] | Katana Avencia | Luting cement (n = 8) | μTBS; aging | 50 μm Al2O3 | Clearfil Ceramic Primer Plus | N/A | Panavia V5 Panavia SA |
| Kawaguchi et al. (2016) [10] | Katana Avencia | Luting cement (n = 8) | μTBS; aging | 50 μm Al2O3 40% PA K-Etchant gel | Clearfil Ceramic Primer Plus | N/A | Panavia V5 Panavia SA |
| Liebermann et al. (2013) [2] | ArtBlock temp | Luting cement (n = 20) | TBS; surface energy; surface roughness | 50 μm Al2O3 | N/A | Visiolink | Clearfil SA Rely X Unicem |
| Magne et al. (2015) [36] | Vita Mark II IPS. e max CAD Lava Ultimate | Human molars (n = 15) | Fatigue test | 50 μm Al2O3 27 μm Al2O3 5% HF | Rely X Ceramic Primer | N/A | Rely X Unicem 2 |
| Malysa et al. (2022) [37] | IPS Empress CAD IPS. e max CAD IPS. e max ZirCAD | Human Molars (n = 12) | SBS; load-to-fracture; thermocycling | 9% HF 37% PA | N/A | N/A | Panavia V5 Maxcem Elite Rely X U200 Panavia SA |
| Nagasawa et al. (2021) [38] | Cerasmart Shofu Block HC HZR-CAD HR2 Estelite Vita Enamic Katana Avencia | Resin composite disk (n = 15) | SBS | 70 μm Al2O3 15-40% PA 9% HF | GC G-Multiprimer | N/A | G-Cem ONE |
| Nagasawa et al. (2022) [14] | GN I Ceramic Block Cerasmart | Resin composite disk (n = 15) | SBS | 70 μm Al2O3 | GC G-Multiprimer GC Ceramic Primer II | N/A | G-Cem ONE |
| Nakamura et al. (2016) [39] | Zirconia | Luting cement (n = 10) Crown (n = 6) | Load-to-failure test; micro-CT analysis | N/A | ED primer | N/A | RelyX Unicem 2 Panavia F2.0 |
| Oda et al. (2021) [25] | Katana Avencia | Human molars (n = 5) | μTBS; irradiance measurements | 50 μm Al2O3 35% PA | Clearfil Ceramic Primer Plus | Clearfil SE Bond 2 | Panavia SA Plus Panavia SA |
| Peumans et al. (2016) [40] | Celtra Duo IPS. e max CAD IPS Empress CAD Vita Enamic Vita Mark II Lava Ultimate | Block to block (n = 10) | μTBS | 27 μm Al2O3 30 μm Al2O3 <5% HF 600-grit Sic Paper Cojet-SiO2 | Monobond Plus Heliobond | N/A | Clearfil Esthetic Panavia SA |
| Poggio et al. (2016) [6] | Lava Ultimate | Bovine incisors (n = 10) | SBS | 35% PA | SB-UA | SB-UA | Rely X Ultimate Rely X Unicem 2 |
| Preis et al. (2015) [4] | Celtra Duo IPS. e max CAD | Human molars (n = 8) | Thermal cycling and mechanical loading (chewing machine) | 5% HF | Monobond S | Heliobond | Smart Cem 2 Variolink II |
| Sorrentino et al. (2016) [41] | Zirconia | Human molars (n = 10) | Load-to-fracture | 50 μm Al2O3 | N/A | N/A | G-Cem LinkAce |
| Takahashi et al. (2022) [42] | Estelite P Katana Avencia Shofu Black HC Super Hard | Luting cement (n = 10) | SBS | 50 μm Al2O3 | N/A | HC Primer | Panavia SA Block HC Cem |
| Ustun et al. (2021) [27] | Vita Suprinity Vita Enamic Cerasmart | Human molars (n = 7) | SBS; thermocycling | 5% HF 37% PA | Ultradent Porcelain Silane | SB-UA | Rely X Ultimate Rely X U200 |
| Zahoui et al. (2020) [43] | Zirconia | Ti-base CAD/CAM abutments (n = 10) | Pull-out test | 30 μm Al2O3 45 μm Al2O3 | SB-UA | SB-UA | Rely X U200 Rely X Ultimate |
| Zhang et al. (2018) [51] | Zirconia | Luting cement (n = 20) | μSBS | 50 μm Al2O3 | SB-UA | SB-UA | Multilink Speed |
| Author, Year | Material | Sample Pairing | Type of Test | Surface Treatment | Coupling Agent | Adhesive System | Luting Cement |
|---|---|---|---|---|---|---|---|
| Dauti et al. (2020) [5] | Vita Enamic | Model resin (n = 10) | Micro CT scan Marginal adaptation measurements | 5% HF | Monobond Plus | AdheSE primer AdheSE Adhesive Optibond XTR OptiBond XTR Primer OptiBond XTR Bond | Rely X Unicem Variolink Esthetic NX3 Nexus |
| Ender et al. (2016) [3] | IPS. Empress CAD ArtBlock Temp | Human molars (n = 12) | Marginal adaptation, chewing fatigue test | 50 μm Al2O3 | Monobond Plus | Heliobond | Rely X Unicem Variolink II |
| Han et al. (2020) [28] | Lava Ultimate | Human molars (n = 6) | Thermocycling; interfacial adaptation | 50 μm Al2O3 Polyacrylic acid | N/A | Universal dentine adhesive Clearfil Universal bond quick Ceramic Primer Plus | Panavia V5 Rely X U200 G-Cem LinkAce SmartCem2 Multilink speed |
| Kirsten et al. (2018) [26] | Vita Mark II | Human molars (n = 8) | Evaluation of crown integrity and cement gap thickness | 35 μm Al2O3 37% PA 5% HF | N/A | Syntac | iCEM Rely X Unicem 2 Variolink Esthetic |
| Melo Freire et al. (2017) [22] | IPS. e max CAD IPS. e max Press | Bovine teeth (n = 64) | Marginal adaptation SEM | 10% HF 35% PA | Rely X Ceramic Primer | Adper Single Bond Plus | Rely X ARC Rely X U200 |
| Preis et al. (2015) [4] | Celtra Duo IPS. e max CAD | Human molars (n = 8) | Thermocycling; marginal quality (i) intact margin (ii) marginal gap | 5% HF | Monobond S | Heliobond | Smart Cem 2 Variolink II |
| Material | Type of Material | Physical Properties | Manufacturer |
|---|---|---|---|
| ArtBlock Temp | Bis-acrylic composite blocks for temporary crowns and bridges. Highly cross-linked interpenetrated PMMA, the OMP-N (organic modified polymer network), without inorganic fillers | Flexural strength: > 90 MPa Module of elasticity: 2.680 MPa Organic curing agent OMP-N Does not contain inorganic fillers | Merz Dental GmbH, Germany |
| Celtra Duo | Zirconia-reinforced lithium silicate ceramic | Median load fracture: 725 N Fracture toughness: 2.6 MPa·m1/2 | Dentsply Sirona, Germany |
| Cerasmart | Hybrid ceramic composite | Flexural strength: 238 MPa Breaking energy: 2.2 N/cm Preserved marginal integrity | GC Corporation, Japan |
| Estelite | Submicron-filled composite | Flexural strength: 259 MPa Elastic modulus: 13.8 GPa | Tokuyama Dental Corporation, Japan |
| GN I Ceramic Block | Hybrid ceramic composite material with inorganic fillers (silica, zirconia, and alumina) | Flexural strength: > 500 MPa Low thermal conductivity Color stability | GC Corporation, Japan |
| HZR-CAD HR2 | Hybrid ceramic with ceramic cluster filler (1–20 µm) | Flexural strength: > 250 MPa Sustained fluoride release High abrasion resistance | Yamakin, Japan |
| IPS Empress CAD | Lithium disilicate glass-ceramic | Biaxial flexural strength: 185 MPa | Ivoclar Vivadent, Liechtenstein |
| IPS. e max CAD | Biaxial flexural strength: 530 MPa Fracture toughness: 2.11 MPa·m1/2 Rapid crystallization: 11 min | ||
| IPS. e max Press | Flexural strength: 470 MPa Fracture toughness: 2.5-3 MPa·m1/2 | ||
| IPS. e max ZirCAD | Zirconium oxide | Flexural strength: 850–1200 MPa | |
| Katana Avencia | Hybrid ceramic (nanosized fillers densely compressed into block and infused with resin monomer) | Flexural strength: > 220 MPa Compressive strength: > 600 MPa Excellent wear resistance | Kuraray Noritake, Japan |
| Lava Ultimate | Highly cross-linked polymeric matrix embedded with 80% of nanoceramic components | Elastic modulus similar to dentin High resistance to fracture | 3M ESPE, USA |
| Shofu Block HC | Pre-sintered, highly filled hybrid ceramic block made of zirconia-reinforced lithium silicate | Stress-absorbing hybrid-ceramic material Flexural strength: > 190 MPa Excellent handling and milling properties | SHOFU Dental GmbH, Japan |
| Vita Enamic | Hybrid ceramic with a dual ceramic-polymer network structure | Flexural strength: ± 160 MPa Module of elasticity: 3 MPa Fracture toughness: 1.5 MPa·m1/2 | Vita Zahnfabrik, Germany |
| Vita Mark II | Fine-structure (4 µm) feldspar ceramic | Flexural strength: 150-160 MPa Elastic modulus: 30.0 GPa Static fracture load: 2.766 N | |
| Vita Suprinity | High-strength zirconia-reinforced lithium silicate ceramic material | Flexural strength: ± 420 MPa Module of elasticity: 7 MPa Fracture toughness: ± 2.0 MPa·m1/2 | |
| Zenostar | Zirconium oxide | Flexural strength > 900 MPa Good abrasive characteristics Gingiva-friendly | Wieland, Germany |
| Material | Frequency | Percent | Cumulative |
|---|---|---|---|
| Artblock Temp | 12 | 4.48 | 4.58 |
| Cerasmart | 28 | 10.69 | 15.27 |
| Estelite block | 13 | 4.96 | 20.23 |
| HZR-CAD-HR2 | 5 | 1.91 | 22.14 |
| IPS Empress CAD | 12 | 4.58 | 26.72 |
| IPS e. max Zircad | 12 | 4.58 | 31.30 |
| IPS e. max CAD | 12 | 4.58 | 35.88 |
| Katana Avencia | 97 | 37.02 | 72.90 |
| Lava Ultimate | 25 | 9.54 | 82.44 |
| Shofu Block Hc | 13 | 4.96 | 87.40 |
| Vita Enamic | 27 | 10.31 | 97.71 |
| Vita Suprinity | 6 | 2.29 | 100.00 |
| Total | 262 | 100.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calheiros-Lobo, M.J.; Vieira, T.; Carbas, R.; da Silva, L.F.M.; Pinho, T. Effectiveness of Self-Adhesive Resin Luting Cement in CAD-CAM Blocks—A Systematic Review and Meta-Analysis. Materials 2023, 16, 2996. https://doi.org/10.3390/ma16082996
Calheiros-Lobo MJ, Vieira T, Carbas R, da Silva LFM, Pinho T. Effectiveness of Self-Adhesive Resin Luting Cement in CAD-CAM Blocks—A Systematic Review and Meta-Analysis. Materials. 2023; 16(8):2996. https://doi.org/10.3390/ma16082996
Chicago/Turabian StyleCalheiros-Lobo, Maria João, Tatiana Vieira, Ricardo Carbas, Lucas F. M. da Silva, and Teresa Pinho. 2023. "Effectiveness of Self-Adhesive Resin Luting Cement in CAD-CAM Blocks—A Systematic Review and Meta-Analysis" Materials 16, no. 8: 2996. https://doi.org/10.3390/ma16082996
APA StyleCalheiros-Lobo, M. J., Vieira, T., Carbas, R., da Silva, L. F. M., & Pinho, T. (2023). Effectiveness of Self-Adhesive Resin Luting Cement in CAD-CAM Blocks—A Systematic Review and Meta-Analysis. Materials, 16(8), 2996. https://doi.org/10.3390/ma16082996










