Abstract
Magnetic resonance imaging (MRI) is a widely used diagnostic technique. Patients wearing orthodontic devices are often requested to remove their appliances before an MRI exam, even when the exam involves anatomical areas far from the head, in order to prevent the heating and detachment of the appliances. The present report aims to evaluate changes in temperature and adhesive forces of molar bands after MRI at two different strength outputs. Sixty stainless steel molar bands were bonded on permanent human upper molars using two different cements: Unitek Multi-Cure Glass Ionomer Band Cement (3M Unitek, Monrovia, CA, USA) and Transbond Plus Light Cure Band Adhesive (3M Unitek). Appliances were subjected to MRI with two different strengths (1.5 Tesla and 3 Tesla). Tubes and band temperature was measured before and after MRI. Subsequently, the shear bond strength (SBS) test was calculated. Data underwent statistical analysis (p < 0.05). After MRI, molar bands exhibited significant heating, even though not clinically relevant, with a temperature increase ranging between 0.48 °C and 1.25 °C (p < 0.05). SBS did not show significant differences (p > 0.05). The present study suggests that, under MRI, the molar bands tested are safe; therefore, their removal could be not recommended for non-head and neck MRI exams. Removal would be necessary just in artifact risk areas.
1. Introduction
Magnetic Resonance Imaging (MRI) is an advanced diagnostic tool, applied to assess various clinical conditions [1]. It is a non-invasive technology that produces 3-dimensional anatomical images without involving the use of ionizing radiation [2] Patients undergoing fixed orthodontic treatment or retention phase may require MRI scans of head and neck region for different reasons. To date, the effects of these appliances on MRI scans are not clear. Consequently, radiologists request to remove any metal object to prevent a possible interaction during the exam [3].
In fact, all objects are magnetized when placed in a magnetic field to a degree depending on their magnetic susceptibility [4]. First, metal items produce a signal loss, defined artifact, and are visible as a black spot in the radiographic image, affecting its diagnostic capability [5]. Moreover, this interaction could displace metallic appliances, leading to injuries for patients and damaging the diagnostic imaging equipment [2]. Lastly, magnetic resonance imaging examinations induce electrical currents in metallic implants which may be capable of causing localized tissue heating [6].
Orthodontists are frequently requested to remove orthodontic appliances before performing MRI to prevent these risks, since metallic alloys of nickel, titanium and stainless steel are widely used in orthodontics [7].
On the other hand, the removal of these devices could damage the enamel structure [8], it is laborious and time-consuming both for the orthodontist and the patient. Moreover, it could lengthen the treatment time and it may lead to unwanted tooth movement [6].
Since clear guidelines are not available, orthodontists are interested in understanding the effects of orthodontic appliances on MRI to minimize the need for their removal [7,9].
At present, many studies assessed the artifacts derived from molar bands [10,11,12], but little data are available about their interaction with the magnetic field and whether they should be removed. Molar bands are used in the fixed orthodontic treatment, both with metallic and ceramic brackets [13,14]. Headgears, lingual arches, transpalatal bars or quad-helixes require molar bands to be used [15].
Therefore, the aim of this study was to evaluate the in vitro effects of MRI at different magnetic field strengths (1.5 T and 3 T) on temperature and bond strength of molar bands cemented to human teeth with two different cements. The first null hypothesis was that there was no significant difference between temperature before and after MRI. The second null hypothesis was that there was no significant difference in the Shear Bond Strength (SBS) values among different groups between temperature before and after MRI.
2. Materials and Methods
2.1. Specimen Preparation
The present in vitro study was approved by the Unit Internal Review Board (2021-0414). A total of 60 permanent human upper molars from patients aging 18–50 were collected and stored in thymol at 0.1% (w/v) according to the following criteria: intact enamel, no carious lesions, restorations or fractures [16]. In detail, they were third molars unable to erupt and periodontally compromised first/second molars. They were carefully cleaned with Softbrush Coarse 2140 burs (Edenta, Scarborough, ON, Canada) at low speed, without water spray.
Each molar was inserted inside a plastic cylindrical mold (2.0 cm height × 2.5 cm diameter) in which cold-curing fast-setting acrylic (Leocryl, Leone s.p.a., Sesto Fiorentino, Italy) was poured. Then, the mold was removed in order to cement the upper right molar bands (Calibra lower molar bands, Leone SpA). The appropriate diameter of the ring was chosen for each tooth and a palatal button and buccal double tube (Leone SpA) were welded on the band using a welding and soldering unit (Assistant 3000 110–240 V, Dentaurum GmbH & Co., Ispringen, Germany), adopting the maximum available power to avoid detachments during the SBS test. Then, teeth were divided into 6 groups of 10 specimens each, depending on the cement used and the magnetic field strength between Unitek Multi-Cure Glass Ionomer Band Cement (3M Unitek, Monrovia, CA, USA), abbreviated as RMGIC (resin-modified glass ionomer cement) and Transbond Plus Light Cure Band Adhesive (3M Unitek), abbreviated as Composite (Table 1).

Table 1.
Groups tested in the present study. *: RMGIC = Unitek Multi-Cure Glass Ionomer Band Cement; Composite = Transbond Plus Light Cure Band Adhesive.
Multi-Cure cement consists of two different components (powder and liquid) that require chair mixing, while Transbond Plus is sold in syringes, containing the material ready for use. Cementation was performed according to the manufacturer’s instructions and the light curing unit was performed with Starlight Pro light-emitting diode (LED) unit (Mectron SPA, Carasco, Italy), with a power output of 1400 mW/cm2 (Table 2).

Table 2.
Protocols used to cement bands.
Then, samples were stored in thymol at 0.1% (w/v).
2.2. Temperature Test and MRI
Specimens were left in the magnet room for 24 h before the MRI test to standardize their temperature in the testing room. A contact thermometer (PeakTech® Digital Thermometer 5135/5140 Prilf—und Messtechnik GmbH, Ahrensburg, Germany) was used to measure the temperature (in Celsius degrees) of each sample. The band temperature was measured by contacting the thermometer probe at the middle height of the ring. The tube temperature was measured at the center of the mesial top border. Temperature measurements were performed immediately before (T0) and after (T1) the MRI exam.
Groups 1 and 2 did not undergo an MRI exam, while groups 3 to 6 underwent the MRI test and were carefully prepared.
Samples of every tested group were placed in a plastic box at a distance of 43 mm to simulate the intermolar width [17] and locked on a plaster base to keep them in place. Then, the plastic box was located inside the support of the patient’s head in the machine.
Groups 3 and 4 underwent magnetic resonance imaging at 1.5 T strength (model Magnetom Aera, Siemens AG, Munich, Germany), while Groups 5 and 6 underwent a 3 T MRI (Magnetom Skyra Fit model, Siemens AG, Munich, Germany).
The parameters used in MRI are provided in the Supplementary Materials (Tables S1 and S2).
The total scanning time was approximately 20 min for each group.
After MRI and temperature measurement, all the specimens were stored in thymol at 0.1% (w/v).
2.3. Shear Bond Strength Test (SBS)
An Instron universal testing machine (Model 3343, Instron Corp, Canton, MA, USA) was used to measure SBS. Each sample was fixed in the mechanical jaw, keeping the band wall parallel to the shearing force. The maximum load required to debond the bands was recorded in Newton (N) and converted into MegaPascals (MPa) knowing the surface area of 1.50 cm² [17]. The vertical force was set at 1 mm/min [18].
2.4. Statistical Analysis
Statistical analysis was performed using R software (version 3.1.3, R Development Core Team, R Foundation for Statistical Computing, Wien, Austria). Descriptive statistics, including mean, standard deviation, minimum, median and maximum values, were calculated for all groups.
The normality of distribution was calculated with the Kolmogorov and Smirnov tests. Inferential statistics were performed with the ANOVA and Tukey post hoc tests for temperatures and SBS values.
Linear regression models for tube temperature, band temperature and SBS were performed, adding as covariates the cement used and the MRI strength.
The significance was predetermined at p < 0.05 for all tests.
3. Results
3.1. Temperature Test
Descriptive statistics of vestibular tube temperatures recorded are shown in Table 3. ANOVA indicated the presence of significant differences between the groups (p < 0.0001). Considering the Tukey post hoc test, at 1.5 T no significant increase from T0 to T1 both for RMGIC and Composite materials (p > 0.05). At 3 T, a significant difference was found comparing RMGIC and Composite at T1 (p < 0.05). A significant difference was found for Composite material at T1 between 1.5 T and 3 T RMI (p < 0.05). Tube temperature variations are shown in Figure 1.

Table 3.
Descriptive statistics tube temperatures (°C) in the various groups tested (T0: before MRI and T1: after MRI). * denotes Tukey grouping: means with the same letters are not significantly different.
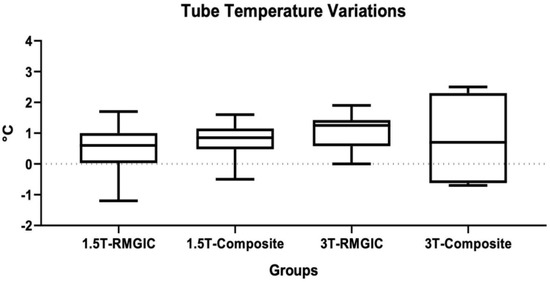
Figure 1.
Tube temperature variation (°C) for each material before and after the 1.5 T and 3 T MRIs.
Descriptive statistics of band temperatures recorded are shown in Table 4. ANOVA showed significant differences among the groups (p < 0.0001). Considering the Tukey post hoc test, at 1.5 T no significant differences were found for each material between T0 and T1 (p > 0.05). A significant difference was found between RMGIC T1 and Composite T0 (p < 0.05). At 3 T, significant differences were found between T0 and T1 for both materials (p < 0.05). No significant differences were found between the materials both at T0 and T1 (p > 0.05). Moreover, no significant differences were found among the groups between 1.5 T and 3 T (p > 0.05). Band temperature variations are shown in Figure 2.

Table 4.
Descriptive statistics of band temperatures (°C) in the various groups tested (T0: before MRI and T1: after MRI). * denotes Tukey grouping means with the same letters are not significantly different.

Figure 2.
Band temperature variations (°C) for each material before and after the 1.5 T and 3 T MRIs.
3.2. SBS Test
Descriptive statistics of SBS values are reported in Table 5. ANOVA showed no significant difference in the SBS values among the various groups tested (p = 0.8369).

Table 5.
Descriptive statistics of SBS values (MPa) tested at different magnetic field strengths. * denotes Tukey grouping: means with the same letters are not significantly different.
3.3. Linear Regressions
Linear regression models showed that tubes and band temperatures were significantly affected by the MRI strength and time frame (Table 6). On the other hand, the bonding material did not significantly influence tube and band temperatures (p > 0.05). SBS values were not significantly affected by the MRI strength, time or bonding material (p > 0.05).

Table 6.
Results of the linear regression models of the different variables (band and tube temperature). Predictors were bonding, time and magnetic field strength. * denotes significant regressions. ns: not significant.
4. Discussion
Patients wearing orthodontic devices are frequently asked to remove their appliances before an MRI exam, even when this latter regards anatomical districts far from the head and neck, in order to prevent heating and detachment of the appliances. As in other fields of dentistry, even in orthodontics, the chemical and physical characteristics of metal alloys as well as the connections between the tooth and these materials deserves to be deeply evaluated [19,20].
The first null hypothesis of this study was partially rejected. Significant differences in band and tube temperatures were reported. Linear regressions revealed significant effects of magnetic field strength and time on the temperatures of the orthodontic devices tested.
Indeed, after MRI, every group showed a temperature increase, especially after MRI at 3 T, according to the fact that heating effects are particularly relevant to high-field MRI investigations [21].
Group 6 (Composite, 3 T) revealed the highest heating of bands and tubes. These results were numerically significant, but not clinically relevant, since heating was limited to a few degrees. In fact, the temperature increase in the dental devices ranged between 0.48 °C and 1.25 °C, so it was far below the safety limit of 5.6 °C for pulpal tissue [22].
Furthermore, the heating of orthodontic devices was not clinically relevant and resulted safe for the patient or surrounding tissues [11].
Currently, many Authors evaluated artifacts derived from orthodontic devices, including molar bands [23], but only a few studies examined temperature changes after the MRI [11,20,24].
Yassi et al. [24] considered the heating of orthodontic devices after MRI at 1 T and 1.5 T and molar bands showed no significative temperature increase.
Hasegawa et al. [11] considered an orthodontic device made of orthodontic brackets, a wire and molar bands attached to a maxillary tooth model. The aim of the study was to evaluate the risk of injury during 3 T MRI. This orthodontic appliance showed heating, even though not clinically significant. Therefore, the Authors concluded that a spacer might be required between the appliance and the oral mucosa and the wire should be removed from the brackets before MRI.
In addition, Regier et al. [20] studied the effect of 3 T MRI on ten stainless steel orthodontic devices, each of them attached to molar bands. Relevant temperature increases were not observed during the exam. These results are in agreement with the present report.
Taking into account SBS, the second null hypothesis of this study was accepted. MRI Strength, bonding and time did not significantly affect SBS values. No significant differences in the adhesion values were reported among the tested groups. The Composite groups showed a slight decrease in SBS after MRI, but these values were not numerically or clinically relevant. In fact, an orthodontic biomaterial should have bonding forces between 5 and 50 MPa, to support masticatory forces without risk of enamel loss [25].
To date, no studies have evaluated the SBS of molar bands after MRI, but Sfondrini et al. [9] have recently investigated the effects of MRI on orthodontic brackets by measuring the SBS. Values obtained under all conditions tested were clinically acceptable, consequently, this is in agreement with the present report.
In addition, a previous report [24] assessed the risk of orthodontic devices displacement during MRI, considering deflection angles and translational forces evaluating many orthodontic appliances, including molar bands, to MRI at 1 T and 1.5 T. The values obtained were lower than the orthodontic and orthopedic forces. The Authors considered the risk of detachment and displacement as non-existent, the importance of following the usual recommendations and checking the proper fixation of devices prior to MRI.
When a patient with an orthodontic device requires an MRI exam, radiologists have to decide whether or not to remove it. Therefore, this report aims to give a contribution to future guidelines in order to assist radiologists and orthodontists in their work.
In the present study, molar bands did not exhibit clinically significant heating; in addition, after MRI, the adhesive forces did not change, and the devices were not displaced.
Indeed, it can be assumed that the tested devices are safe during MRI; therefore, they could not be removed prior to 1.5 T and 3 T MRI body except for head and neck imaging. On the other hand, if a head and neck MRI is required, molar bands need to be removed to avoid artifacts [7,26].
The same applies to patients undergoing multibracket therapy with molar bands: in fact, a recent study [9] showed that the removal of orthodontic brackets is not recommended for non-head and neck MRI, as temperature and SBS did not show any difference after MRI.
As regards removable devices attached to the molar bands, such as lip-bumpers or headgears, they could be easily removed by the patients prior to the MRI exam.
Appliances attached to the bands with sheets and held in place by frictional forces, as quad-helixes or palatal bars, can be removed by the orthodontist before the MRI, and then repositioned with no time-consuming procedures.
On the other hand, devices welded to molar bands such as Herbst appliances, rapid maxillary expanders, welded quad-helixes, palatal bars or lip-bumpers, cannot be removed without considerable effort, costs and interruption of orthodontic treatment. In these situations, clinicians should assess the study area, in order to decide whether to remove fixed devices and bands.
According to Regier et al. [20], who tested the heating of many orthodontic appliances such as a lip-bumper, quad-helix and a palatal expander during a 3 T MRI, a routine head examination can be safely carried out in patients. In addition, Kemper et al. [27] evaluated the translational and rotational forces of some orthodontic devices used for fixed orthodontic therapy, revealing that adequate fixation must be checked prior to MRI to minimize the possible effects of the magnetic field.
However, further studies are required to assess the potential interactions of welded orthodontic appliances with the magnetic field.
The major limitation of the present report is that it is an in vitro investigation, therefore clinical studies are necessary to confirm the finding of the study. Additionally, the results here obtained are valid only for the materials tested, as there may be variations in the induced magnetic moments among devices of different manufacturers. Moreover, since 6 T MRI appliances are available, future studies are recommended to analyze possible different interactions between orthodontic appliances and the higher magnetic field. Investigating the possible effects of RMI on a full arch with brackets, archwires and tubes could probably complete the results here obtained. At last, an interesting aspect could be investigating patients’ perspective during MRI while they are wearing orthodontic devices.
5. Conclusions
In conclusion, the present report suggests that molar bands are safe as the tested materials did not exhibit clinically significant heating (from 0.48 °C to 1.25 °C), so the magnetic field did not affect temperature or adhesion in any group, and it did not cause their displacement. Therefore, the removal could not be recommended routinely but just in case of artifact risk which could compromise the diagnostic quality of the exam.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ma16020651/s1, Table S1: Parameters of 1.5 T RMI; Table S2: Parameters of 3 T RMI.
Author Contributions
Conceptualization, A.S., M.F.S., L.P. and P.G.; methodology, A.S.; software, A.S.; validation, M.F.S.; formal analysis, A.S.; investigation, A.B., C.R., L.A., S.S. and M.S.P.G.; resources, P.G. and L.P.; data curation, M.P. and A.S.; writing—original draft preparation, C.R., M.P. and S.G.; writing—review and editing, M.P., S.G. and A.S.; visualization, M.F.S.; supervision, P.G. and L.P.; project administration, M.F.S. and A.S.; funding acquisition, P.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by the Unit Internal Review Board (Approval Date: 14 April 2021; Approval Number: 2021-0414).
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are available upon motivated request to the corresponding authors.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Reda, R.; Zanza, A.; Mazzoni, A.; Cicconetti, A.; Testarelli, L.; Di Nardo, D. An Update of the Possible Applications of Magnetic Resonance Imaging (MRI) in Dentistry: A Literature Review. J. Imaging 2021, 7, 75. [Google Scholar] [CrossRef] [PubMed]
- Chockattu, S.J.; Suryakant, D.B.; Thakur, S. Unwanted effects due to interactions between dental materials and magnetic resonance imaging: A review of the literature. Restor. Dent. Endod. 2018, 43, 39. [Google Scholar] [CrossRef] [PubMed]
- Poorsattar-Bejeh Mir, A.; Rahmati-Kamel, M. Should the orthodontic brackets always be removed prior to magnetic resonance imaging (MRI)? J. Oral Biol. Craniofac. Res. 2016, 6, 142–152. [Google Scholar] [CrossRef] [PubMed]
- Görgülü, S.; Ayyildiz, S.; Kamburoglu, K.; Gökçe, S.; Ozen, T. Effect of orthodontic brackets and different wires on radiofrequency heating and magnetic field interactions during 3-T MRI. Dentomaxillofac. Radiol. 2014, 43, 20130356. [Google Scholar] [CrossRef]
- Dalili Kajan, Z.; Khademi, J.; Alizadeh, A.; Babaei Hemmaty, Y.; Atrkar Roushan, Z. A comparative study of metal artifacts from common metal orthodontic brackets in magnetic resonance imaging. Imaging Sci. Dent. 2015, 45, 159–168. [Google Scholar] [CrossRef]
- Shalish, M.; Dykstein, N.; Friedlander-Barenboim, S.; Ben-David, E.; Gomori, J.M.; Chaushu, S. Influence of common fixed retainers on the diagnostic quality of cranial magnetic resonance images. Am. J. Orthod. Dentofac. Orthop. 2015, 147, 604–609. [Google Scholar] [CrossRef]
- Hasanin, M.; Kaplan, S.E.F.; Hohlen, B.; Lai, C.; Nagshabandi, R.; Zhu, X.; Al-Jewair, T. Effects of orthodontic appliances on the diagnostic capability of magnetic resonance imaging in the head and neck region: A systematic review. Int. Orthod. 2019, 17, 403–414. [Google Scholar] [CrossRef]
- Degrazia, F.W.; Genari, B.; Ferrazzo, V.A.; Santos-Pinto, A.D.; Grehs, R.A. Enamel Roughness Changes after Removal of Orthodontic Adhesive. Dent. J. 2018, 6, 39. [Google Scholar] [CrossRef]
- Sfondrini, M.F.; Preda, L.; Calliada, F.; Carbone, L.; Lungarotti, L.; Bernardinelli, L.; Gandini, P.; Scribante, A. Magnetic Resonance Imaging and Its Effects on Metallic Brackets and Wires: Does It Alter the Temperature and Bonding Efficacy of Orthodontic Devices? Materials 2019, 12, 3971. [Google Scholar] [CrossRef]
- Wylezinska, M.; Pinkstone, M.; Hay, N.; Scott, A.D.; Birch, M.J.; Miquel, M.E. Impact of orthodontic appliances on the quality of craniofacial anatomical magnetic resonance imaging and real-time speech imaging. Eur. J. Orthod. 2015, 37, 610–617. [Google Scholar] [CrossRef]
- Hasegawa, M.; Miyata, K.; Abe, Y.; Ishigami, T. Radiofrequency heating of metallic dental devices during 3.0 T MRI. Dentomaxillofac. Radiol. 2013, 42, 20120234. [Google Scholar] [CrossRef]
- Okano, Y.; Yamashiro, M.; Kaneda, T.; Kasai, K. Magnetic resonance imaging diagnosis of the temporomandibular joint in patients with orthodontic appliances. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2003, 95, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Veiga Jardim, A.F.; Azevedo, M.N.; Souza, J.B.; Freitas, J.C.; Estrela, C. Evaluation of bond strength of molar orthodontic tubes subjected to reinforcement with flowable and bonding resins. J. Orofac. Orthop. 2020, 81, 350–359. [Google Scholar] [CrossRef] [PubMed]
- Elison, J.M.; Leggitt, V.L.; Thomson, M.; Oyoyo, U.; Wycliffe, N.D. Influence of common orthodontic appliances on the diagnostic quality of cranial magnetic resonance images. Am. J. Orthod. Dentofacial. Orthop. 2008, 134, 563–572. [Google Scholar] [CrossRef] [PubMed]
- Nazir, M.; Walsh, T.; Mandall, N.A.; Matthew, S.; Fox, D. Banding versus bonding of first permanent molars: A multi-centre randomized controlled trial. J. Orthod. 2011, 38, 81–89. [Google Scholar] [CrossRef]
- Cacciafesta, V.; Sfondrini, M.F.; Calvi, D.; Scribante, A. Effect of fluoride application on shear bond strength of brackets bonded with a resin-modified glass-ionomer. Am. J. Orthod. Dentofacial Orthop. 2005, 127, 580–583. [Google Scholar] [CrossRef]
- Millett, D.T.; Cummings, A.; Letters, S.; Roger, E.; Love, J. Resin-modified glass ionomer, modified composite or conventional glass ionomer for band cementation?--an in vitro evaluation. Eur. J. Orthod. 2003, 25, 609–614. [Google Scholar] [CrossRef]
- Eliades, T.; Brantley, W.A. The inappropriateness of conventional orthodontic bond strength assessment protocols. Eur. J. Orthod. 2000, 22, 13–23. [Google Scholar] [CrossRef]
- Artun, J.; Bergland, S. Clinical trials with crystal growth conditioning as an alternative to acid-etch enamel pretreatment. Am. J. Orthod. 1984, 85, 333–340. [Google Scholar] [CrossRef]
- Regier, M.; Kemper, J.; Kaul, M.G.; Feddersen, M.; Adam, G.; Kahl-Nieke, B.; Klocke, A. Radiofrequency-induced heating near fixed orthodontic appliances in high field MRI systems at 3.0 Tesla. J. Orofac. Orthop. 2009, 70, 485–494. [Google Scholar] [CrossRef]
- Raszewski, Z.; Brząkalski, D.; Derpeński, Ł.; Jałbrzykowski, M.; Przekop, R.E. Aspects and Principles of Material Connections in Restorative Dentistry—A Comprehensive Review. Materials 2022, 15, 7131. [Google Scholar] [CrossRef]
- Ottl, P.; Lauer, H.C. Temperature response in the pulpal chamber during ultrahigh-speed tooth preparation with diamond burs of different grit. J. Prosthet. Dent. 1998, 80, 12–19. [Google Scholar] [CrossRef]
- Wang, Z.J.; Rollins, N.K.; Liang, H.; Park, Y.J. Induced magnetic moment in stainless steel components of orthodontic appliances in 1.5 T MRI scanners. Med. Phys. 2015, 42, 5871–5878. [Google Scholar] [CrossRef] [PubMed]
- Yassi, K.; Ziane, F.; Bardinet, E.; Moinard, M.; Veyret, B.; Chateil, J.F. Evaluation des risques d’échauffement et de déplacement des appareils orthodontiques en imagerie par resonance. J. Radiol. 2007, 88, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Scribante, A.; Contreras-Bulnes, R.; Montasser, M.A.; Vallittu, P.K. Orthodontics: Bracket Materials, Adhesives Systems, and Their Bond Strength. Biomed. Res. Int. 2016, 2016, 1329814. [Google Scholar] [CrossRef] [PubMed]
- Costa, A.L.; Appenzeller, S.; Yasuda, C.L.; Pereira, F.R.; Zanardi, V.A.; Cendes, F. Artifacts in brain magnetic resonance imaging due to metallic dental objects. Med. Oral Patol. Oral Cir. Bucal. 2009, 14, E278–E282. [Google Scholar]
- Kemper, J.; Priest, A.N.; Schulze, D.; Kahl-Nieke, B.; Adam, G.; Klocke, A. Orthodontic springs and auxiliary appliances: Assessment of magnetic field interactions associated with 1.5 T and 3 T magnetic resonance systems. Eur. Radiol. 2007, 17, 533–540. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).