Optimized Erbium-Doped Yttrium Aluminum Garnet (Er:YAG) Laser Parameters for the Removal of Dental Ceramic Restorations
Abstract
:1. Introduction
2. Materials and Methods
2.1. Laser Parameters
2.2. Power Measurements
3. Statistical Analysis
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bayne, S.C.; Ferracane, J.L.; Marshall, G.W.; Marshall, S.J.; van Noort, R. The Evolution of Dental Materials over the Past Century: Silver and Gold to Tooth Color and Beyond. J. Dent. Res. 2019, 98, 257–265. [Google Scholar] [CrossRef]
- Zarone, F.; Di Mauro, M.I.; Ausiello, P.; Ruggiero, G.; Sorrentino, R. Current status on lithium disilicate and zirconia: A narrative review. BMC Oral Health 2019, 19, 134. [Google Scholar] [CrossRef] [PubMed]
- Sailer, I.; Makarov, N.A.; Thoma, D.S.; Zwahlen, M.; Pjetursson, B.E. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs). Dent. Mater. 2015, 31, 603–623. [Google Scholar] [CrossRef] [PubMed]
- Keeling, F.L.; Taft, R.M.; Haney, S.J. Bur Choice When Removing Zirconia Restorations. J. Prosthodont. 2023, 32, 347–352. [Google Scholar] [CrossRef]
- Zhang, X.; Dong, H.; Guo, C.; Zhang, X.; Zhang, D.; Wu, X.; Zhao, J. Effects of laser debonding treatment on the optical and mechanical properties of all-ceramic restorations. Lasers Med. Sci. 2021, 36, 1497–1504. [Google Scholar] [CrossRef]
- Karagoz-Yildirak, M.; Gozneli, R. Evaluation of rebonding strengths of leucite and lithium disilicate veneers debonded with an Er:YAG laser. Lasers Med. Sci. 2020, 35, 853–860. [Google Scholar] [CrossRef]
- Deeb, J.G.; Skrjanc, L.; Kanduti, D.; Carrico, C.; Saturno, A.M.; Grzech-Lesniak, K. Evaluation of Er:YAG and Er,Cr:YSGG laser irradiation for the debonding of prefabricated zirconia crowns. Adv. Clin. Exp. Med. 2021, 30, 7–15. [Google Scholar] [CrossRef]
- Grzech-Lesniak, K.; Bencharit, S.; Dalal, N.; Mroczka, K.; Deeb, J.G. In Vitro Examination of the Use of Er:YAG Laser to Retrieve Lithium Disilicate Crowns from Titanium Implant Abutments. J. Prosthodont. 2019, 28, 672–676. [Google Scholar] [CrossRef]
- Giraldo-Cifuentes, H.; Espana-Tost, A.; Arnabat-Dominguez, J. Er,Cr:YSGG Laser in the Debonding of Feldspathic Porcelain Veneers: An In Vitro Study of Two Different Fluences. Photobiomodul. Photomed. Laser. Surg. 2020, 38, 640–645. [Google Scholar] [CrossRef] [PubMed]
- Rechmann, P.; Buu, N.C.; Rechmann, B.M.; Le, C.Q.; Finzen, F.C.; Featherstone, J.D. Laser all-ceramic crown removal-a laboratory proof-of-principle study-phase 1 material characteristics. Lasers Surg. Med. 2014, 46, 628–635. [Google Scholar] [CrossRef] [PubMed]
- Rechmann, P.; Buu, N.C.; Rechmann, B.M.; Finzen, F.C. Laser all-ceramic crown removal-a laboratory proof-of-principle study-phase 2 crown debonding time. Lasers Surg. Med. 2014, 46, 636–643. [Google Scholar] [CrossRef] [PubMed]
- Gurney, M.L.; Sharples, S.D.; Phillips, W.B.; Lee, D.J. Using an Er,Cr:YSGG laser to remove lithium disilicate restorations: A pilot study. J. Prosthet. Dent. 2016, 115, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Yildiz, P.; Gunes Unlu, D.; Talay Cevlik, E.; Usumez, A. Removal of lithium disilicate veneers with Er,Cr:YSGGL laser: Now? Or after ageing? Lasers Med. Sci. 2022, 38, 12. [Google Scholar] [CrossRef]
- Gozneli, R.; Sendurur, T.; Silahtar, E. A Preliminary Study in Er:YAG Laser Debonding of Lithium Disilicate Crowns: Laser Power Setting vs Crown Thickness. Int. J. Med. Sci. 2023, 20, 1212–1219. [Google Scholar] [CrossRef] [PubMed]
- Al-Karadaghi, S.S.; Jawad, H.; Al-Karadaghi, T. The influence of pulse duration and exposure time of Er,Cr:YSGG laser on lithium disilicate laminate debonding, an in vitro study. Heliyon 2023, 9, e14600. [Google Scholar] [CrossRef]
- Kellesarian, S.V.; Ros Malignaggi, V.; Aldosary, K.M.; Javed, F. Laser-assisted removal of all ceramic fixed dental prostheses: A comprehensive review. J. Esthet. Restor. Dent. 2018, 30, 216–222. [Google Scholar] [CrossRef]
- Gozneli, R.; Sendurur, T. Er:YAG laser lithium disilicate crown removal: Removal time and pulpal temperature change. Lasers Med. Sci. 2023, 38, 164. [Google Scholar] [CrossRef]
- Zhang, X.; Dong, H.; Wu, X.; Zhao, J.; Jiang, Q. Evaluation of Er:YAG laser energy transmitted through novel dental zirconia ceramics. Dent. Mater. J. 2023, 2022-259. [Google Scholar] [CrossRef]
- Mocuta, D.E.; Miron, M.I.; Lungeanu, D.; Mateas, M.; Ogodescu, E.; Todea, C.D. Laser Er:YAG-Assisted Debonding May Be a Viable Alternative to the Conventional Method for Monocrystalline Ceramic Brackets. Int. J. Environ. Res. Public Health 2022, 19, 14564. [Google Scholar] [CrossRef]
- Downarowicz, P.; Noszczyk, P.; Mikulewicz, M.; Nowak, R. Thermal effect of Er:YAG and Er,Cr:YSGG used for debonding ceramic and metal orthodontic brackets: An experimental analysis. Adv. Clin. Exp. Med. 2020, 29, 557–563. [Google Scholar] [CrossRef]
- Grzech-Lesniak, K.; Matys, J.; Zmuda-Stawowiak, D.; Mroczka, K.; Dominiak, M.; Brugnera Junior, A.; Gruber, R.; Romanos, G.E.; Sculean, A. Er:YAG Laser for Metal and Ceramic Bracket Debonding: An In Vitro Study on Intrapulpal Temperature, SEM, and EDS Analysis. Photomed. Laser Surg. 2018, 36, 595–600. [Google Scholar] [CrossRef]
- Al-Karadaghi, S.S.; Jawad, H.A. Debonding of LDSVs utilising Er,Cr:YSGG laser irradiation with fractional technique: An in vitro study. Aust. Dent. J. 2023, 68, 125–134. [Google Scholar] [CrossRef]
- Tozlu, M.; Oztoprak, M.O.; Arun, T. Comparison of shear bond strengths of ceramic brackets after different time lags between lasing and debonding. Lasers Med. Sci. 2012, 27, 1151–1155. [Google Scholar] [CrossRef]
- Giraldo Cifuentes, H.; Gomez, J.C.; Guerrero, A.N.L.; Munoz, J. Effect of an Er,Cr:YSGG Laser on the Debonding of Lithium Disilicate Veneers With Four Different Thicknesses. J. Lasers Med. Sci. 2020, 11, 464–468. [Google Scholar] [CrossRef] [PubMed]
- Rechmann, P.; Buu, N.C.; Rechmann, B.M.; Finzen, F.C. Laser all-ceramic crown removal and pulpal temperature—A laboratory proof-of-principle study. Lasers Med. Sci. 2015, 30, 2087–2093. [Google Scholar] [CrossRef] [PubMed]
- Ghazanfari, R.; Azimi, N.; Nokhbatolfoghahaei, H.; Alikhasi, M. Laser Aided Ceramic Restoration Removal: A Comprehensive Review. J. Lasers Med. Sci. 2019, 10, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Sari, T.; Tuncel, I.; Usumez, A.; Gutknecht, N. Transmission of Er:YAG laser through different dental ceramics. Photomed. Laser Surg. 2014, 32, 37–41. [Google Scholar] [CrossRef]
- AlBalkhi, M.; Hamadah, O. Influence of pulse duration and water/air cooling ratio on the efficiency of Er:YAG 2940 nm laser in debonding of porcelain laminate veneers: An in vitro study. Clin. Exp. Dent. Res. 2022, 8, 843–848. [Google Scholar] [CrossRef]
- Abdel Sadek, H.M.; Abdel Khalek, A.M.; Wahsh, M.M. The effect of Er, Cr:YSGG laser debonding on the bond strength of two ceramic materials to dentin. BMC Oral Health 2023, 23, 17. [Google Scholar] [CrossRef]
- Knappe, V.; Frank, F.; Rohde, E. Principles of lasers and biophotonic effects. Photomed. Laser Surg. 2004, 22, 411–417. [Google Scholar] [CrossRef]



| Group | Type | Name | Company |
|---|---|---|---|
| I | Lithium disilicate (LDS) | IPS e.max® CAD | Ivoclar Vivadent |
| II | Zirconium-reinforced lithium silicate (ZLS) | VITA SUPRINITY® | Vita Zahnfabrik |
| III | Feldspathic ceramic (FC) | VITABLOCS® Mark II | Vita Zahnfabrik |
| IV | Zirconium dioxide (ZD) | IPS e.max® ZirCAD LT | Ivoclar Vivadent |
| Power | Tickness | I LDS | II ZLS | III FC | IV ZD |
|---|---|---|---|---|---|
| 1.5 W | 1 mm | 52.0% | 53.3% | 19.3% | 40.0% |
| 2.5 W | 1 mm | 53.2% | 54.8% | 19.2% | 40.4% |
| 3.5 W | 1 mm | 53.4% | 55.1% | 19.7% | 40.8% |
| 4.5 W | 1 mm | 54.0% | 55.1% | 19.5% | 41.1% |
| 1.5 W | 2 mm | 35.3% | 35.3% | 10.0% | 31.3% |
| 2.5 W | 2 mm | 35.2% | 35.2% | 10.0% | 32.4% |
| 3.5 W | 2 mm | 36.0% | 36.0% | 10.2% | 32.8% |
| 4.5 W | 2 mm | 36.0% | 36.2% | 10.2% | 33.1% |
| Time (s) Mean ± SD (Median; Range) | I (LDS) N = 5 | II (ZLS) N = 5 | III (FC) N = 5 | IV (ZD) N = 5 |
|---|---|---|---|---|
| 1 mm 1.5 W | 31.4 ± 22.3 (23; 15–69) | 7.0 ± 4.7 (5; 2–13) | 18.4 ± 4.9 (17; 13–24) | 8.2 ± 3.8 (7; 5–14) |
| 1 mm 2.5 W | 27.4 ± 9.5 (24; 18–39) | 16.0 ± 15.8 (14; 4–43) | 8.2 ± 2.9 (8; 5–12) | 4.0 ± 3.9 (2; 1–10) |
| 1 mm 3.5 W | 5.6 ± 2.1 (6; 3–8) | 6.2 ± 5.4 (6; 1–13) | 7.2 ± 3.6 (6; 4–13) | 6.6 ± 8.2 (1; 1–19) |
| 1 mm 4.5 W | 5.6 ± 6.6 (4; 1–17) | 6.2 ± 5.8 (7; 1–15) | 2.8 ± 2.0 (3; 1–6) | 3.8 ± 3.9 (1; 1–9) |
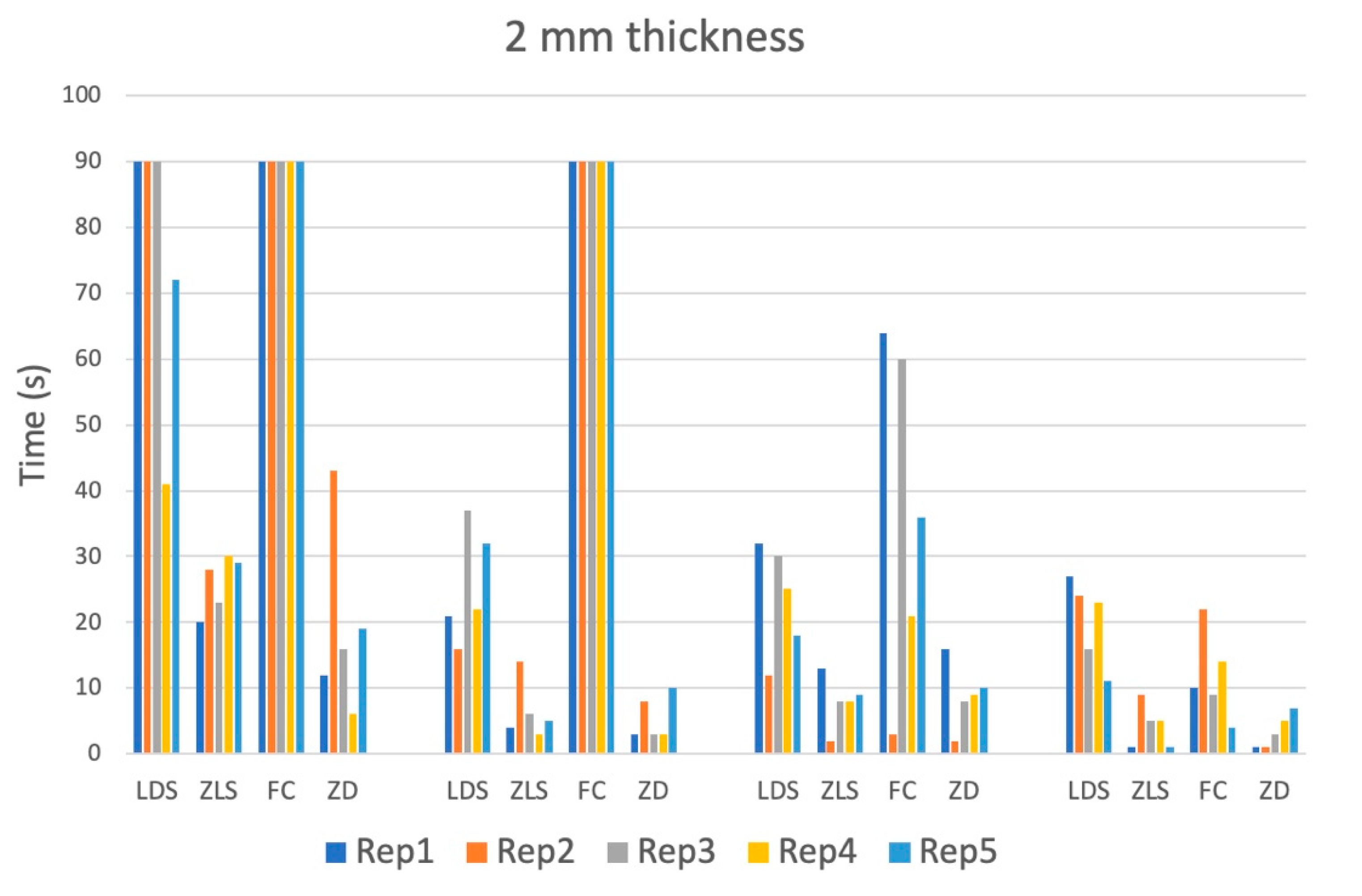
| 2 mm 1.5 W | >90 | 26.0 ± 4.3 (26; 20–30) | >90 | 19.2 ± 14.2 (16; 6–43) |
| 2 mm 2.5 W | 25.6 ± 8.6 (22; 16–37) | 6.4 ± 4.4 (5; 2–13) | >90 | 5.4 ± 3.4 (3; 3–10) |
| 2 mm 3.5 W | 23.4 ± 8.4 (25; 12–32) | 8.0 ± 4.0 (8; 2–13) | 36.8 ± 25.8 (36; 3–64) | 9.0 ± 5.0 (9; 2–16) |
| 2 mm 4.5 W | 20.2 ± 6.5 (23; 11–27) | 4.2 ± 3.3 (5; 1–9) | 11.8 ± 6.7 (10; 4–22) | 3.4 ± 2.6 (3; 1–7) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Laky, M.; Toth, P.; Laky, B.; Vaskovich, T.; Kurzmann, C.; Arslan, M.; Nguyen, M.; Rausch-Fan, X.; Moritz, A.; Shokoohi-Tabrizi, H.A. Optimized Erbium-Doped Yttrium Aluminum Garnet (Er:YAG) Laser Parameters for the Removal of Dental Ceramic Restorations. Materials 2023, 16, 5835. https://doi.org/10.3390/ma16175835
Laky M, Toth P, Laky B, Vaskovich T, Kurzmann C, Arslan M, Nguyen M, Rausch-Fan X, Moritz A, Shokoohi-Tabrizi HA. Optimized Erbium-Doped Yttrium Aluminum Garnet (Er:YAG) Laser Parameters for the Removal of Dental Ceramic Restorations. Materials. 2023; 16(17):5835. https://doi.org/10.3390/ma16175835
Chicago/Turabian StyleLaky, Markus, Peter Toth, Brenda Laky, Tom Vaskovich, Christoph Kurzmann, Muazzez Arslan, Mariano Nguyen, Xiaohui Rausch-Fan, Andreas Moritz, and Hassan Ali Shokoohi-Tabrizi. 2023. "Optimized Erbium-Doped Yttrium Aluminum Garnet (Er:YAG) Laser Parameters for the Removal of Dental Ceramic Restorations" Materials 16, no. 17: 5835. https://doi.org/10.3390/ma16175835
APA StyleLaky, M., Toth, P., Laky, B., Vaskovich, T., Kurzmann, C., Arslan, M., Nguyen, M., Rausch-Fan, X., Moritz, A., & Shokoohi-Tabrizi, H. A. (2023). Optimized Erbium-Doped Yttrium Aluminum Garnet (Er:YAG) Laser Parameters for the Removal of Dental Ceramic Restorations. Materials, 16(17), 5835. https://doi.org/10.3390/ma16175835







