Primary Implant Stability Analysis of Different Dental Implant Connections and Designs—An In Vitro Comparative Study
Abstract
:1. Introduction
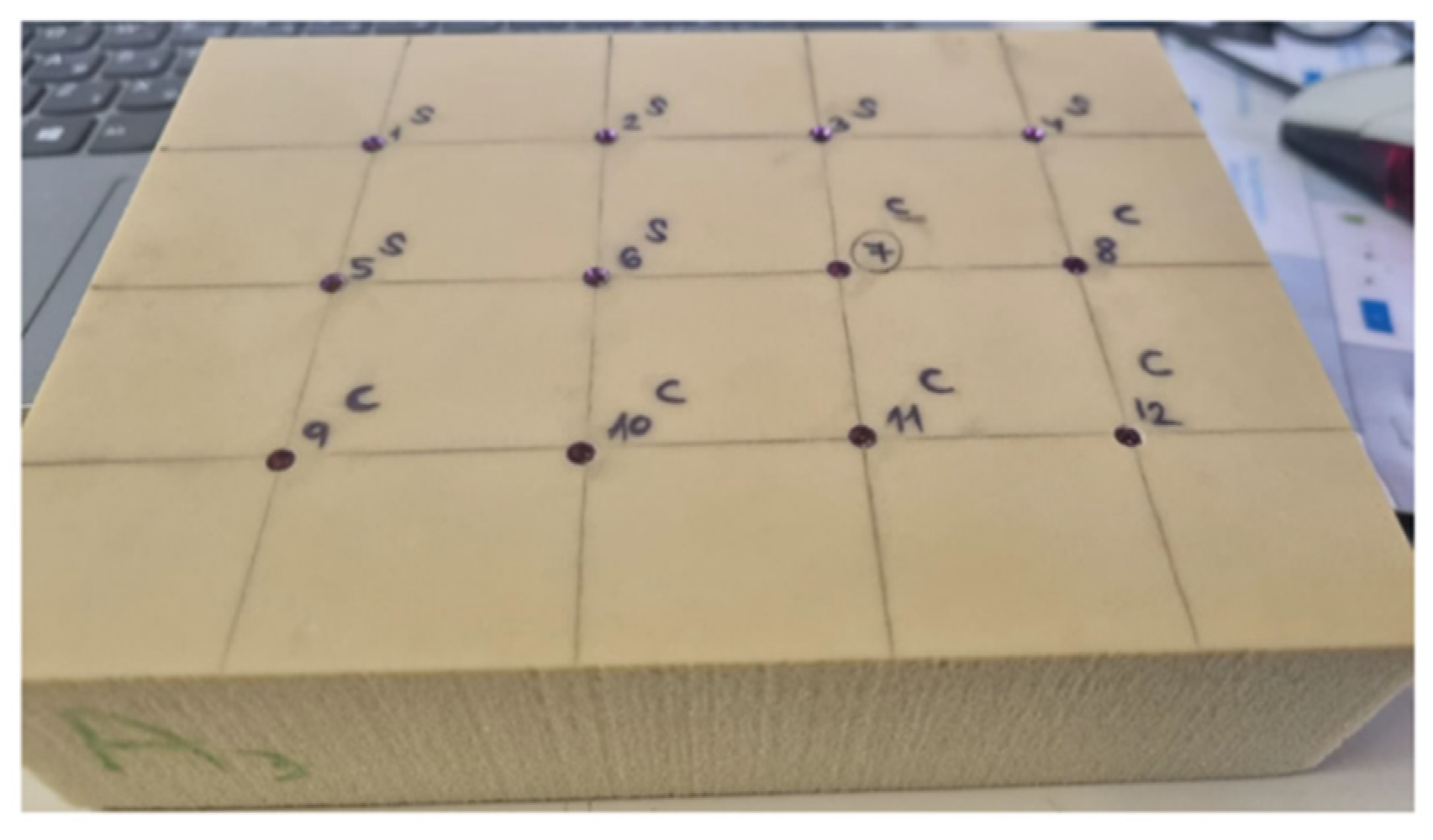
2. Materials and Methods
3. Statistical Analysis
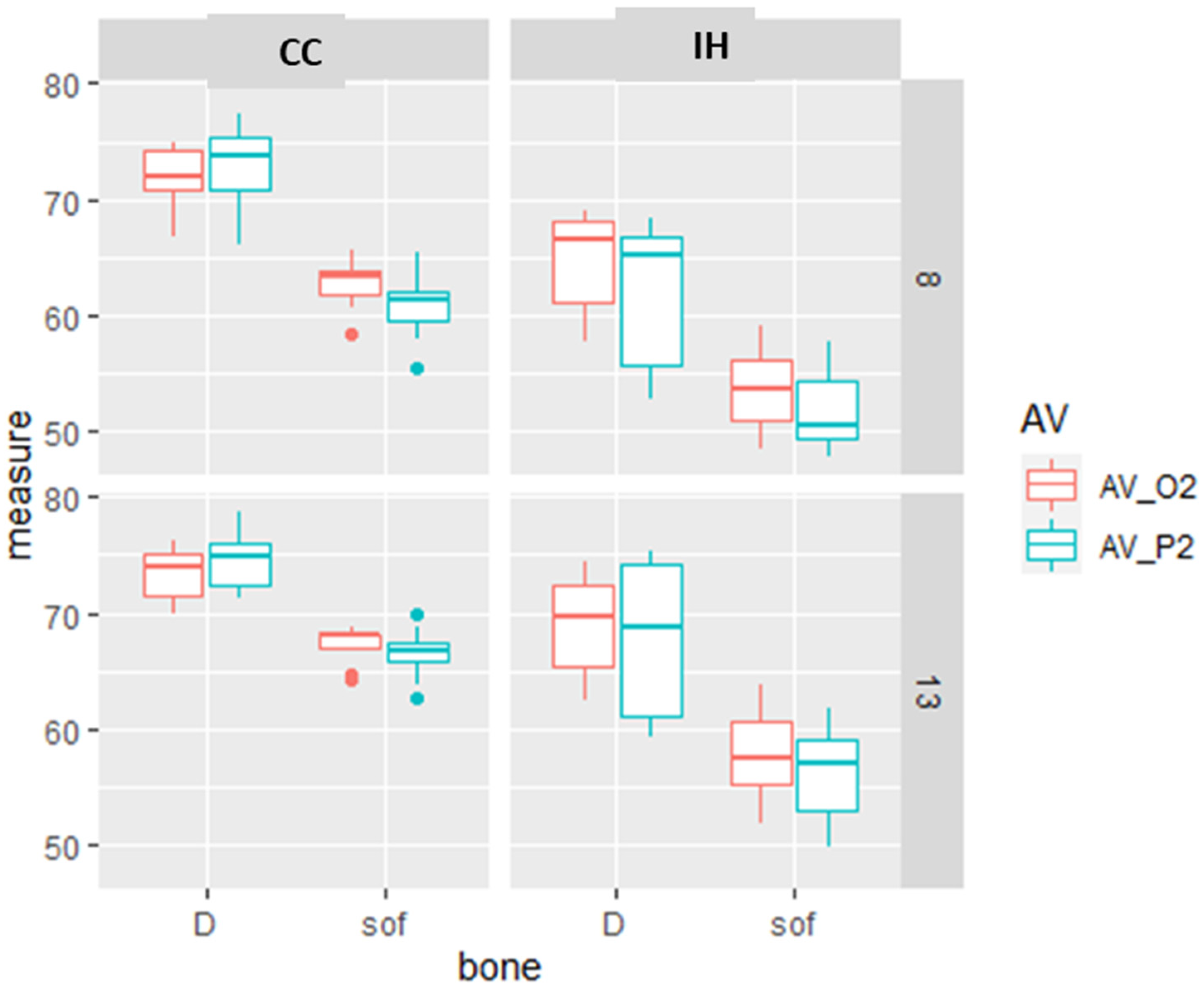
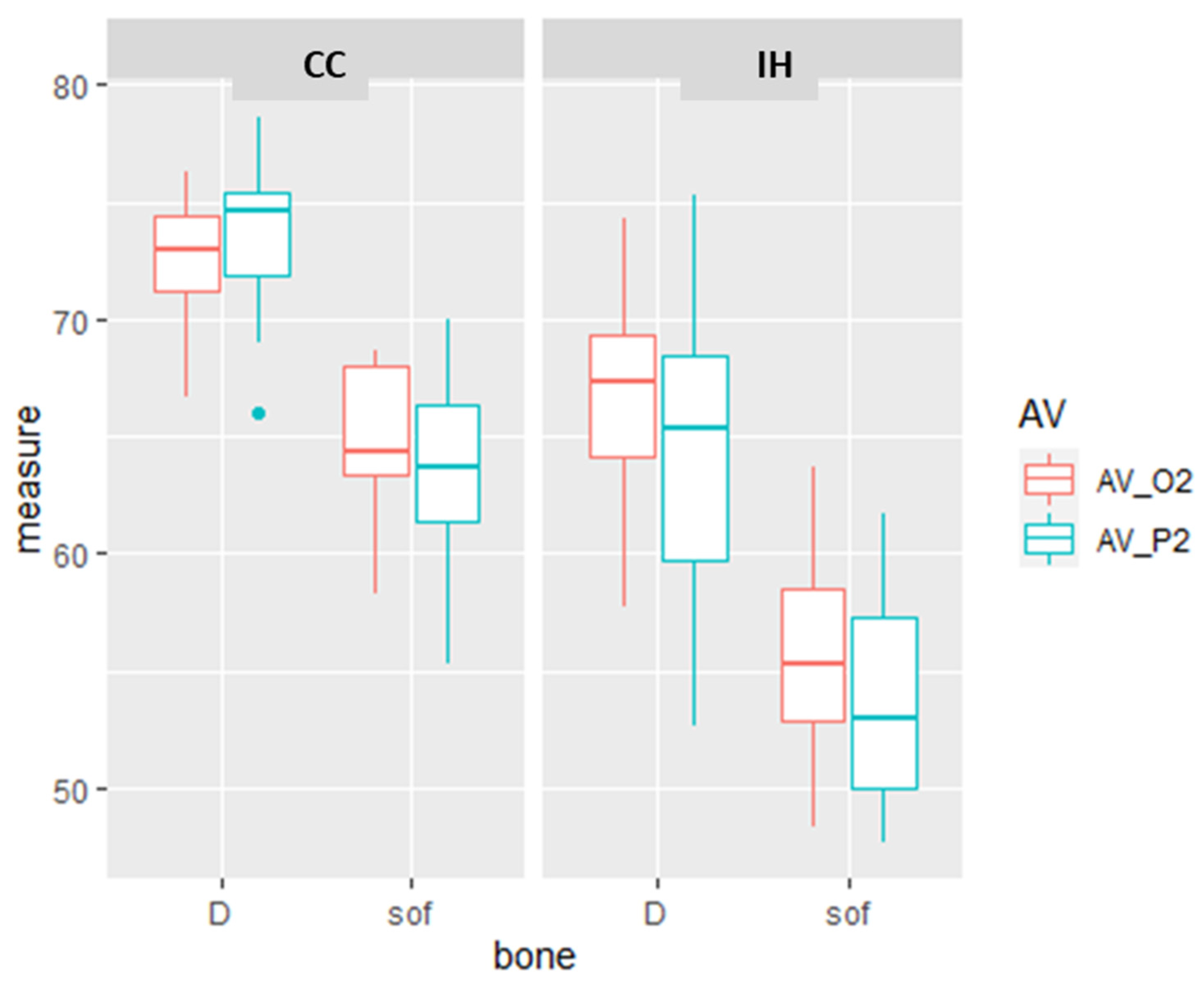
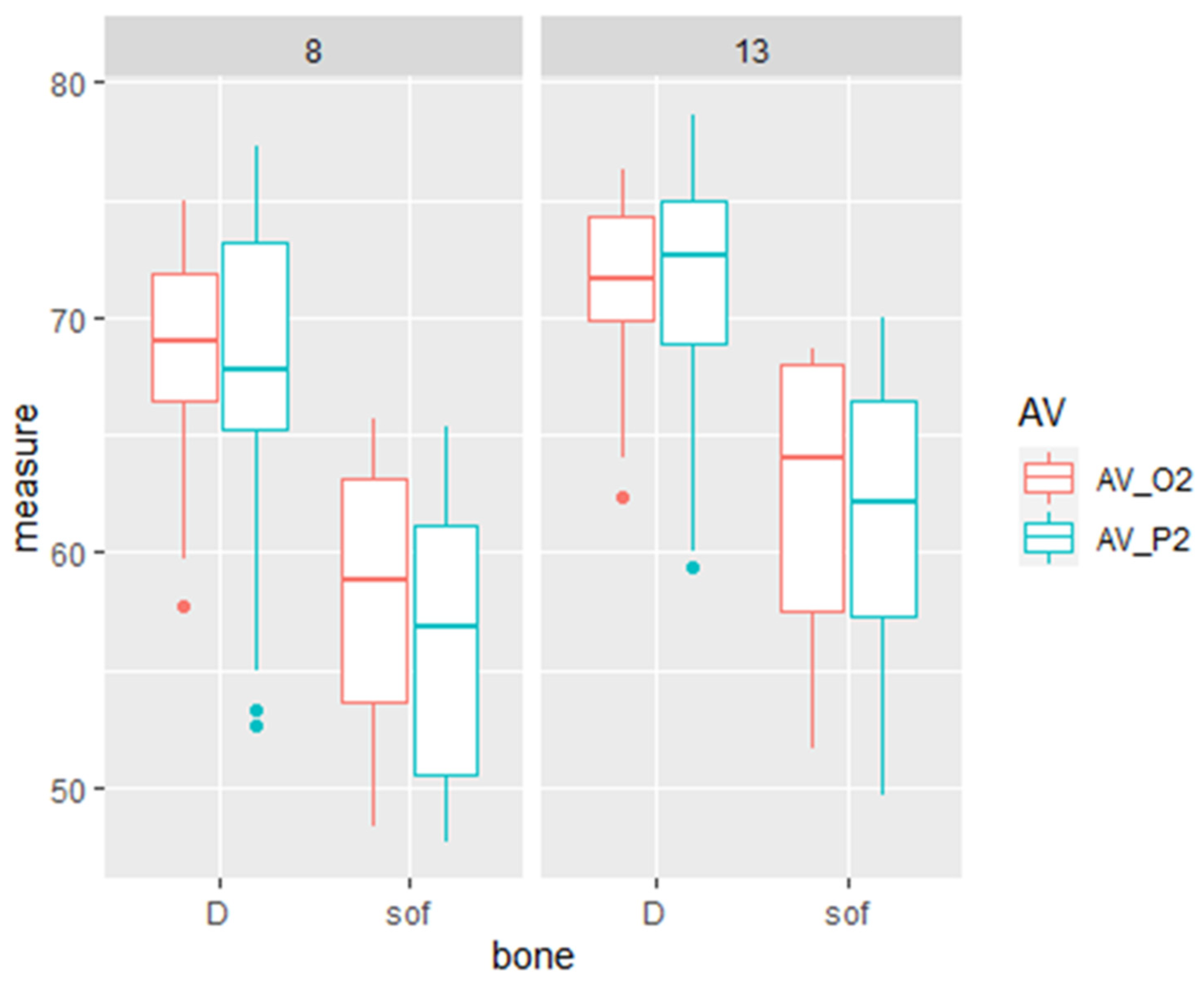
4. Results
5. Discussion
6. Conclusions and Clinical Relevance
- Primary stability measurements made by Osstell and Penguin devices reveal higher values for longer (13 mm) compared to shorter implants (8 mm), for dense bone compared to soft bone, and for implants with a CC rather than an IH design.
- The increased stability of the CC implant design may compensate for the low primary implant stability expected in soft bone.
- The effect of implant length in dense bone is significant but smaller than in soft bone. Dense bone may compensate for 8 mm implant insertion.
- The CC implant design may be used to enhance the primary implant stability in cases where insertion of an 8 mm implant is obligatory.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Bosshardt, D.D.; Chappuis, V.; Buser, D. Osseointegration of titanium, titanium alloy and zirconia dental implants: Current knowledge and open questions. Periodontol. 2000 2017, 73, 22–40. [Google Scholar] [CrossRef] [PubMed]
- Romanos, G.E. Present status of immediate loading of oral implants. J. Oral. Implantol. 2004, 30, 189–197. [Google Scholar] [CrossRef]
- Meredith, N. Assessment of implant stability as a prognostic determinant. Int. J. Prosthodont. 1998, 11, 491–501. [Google Scholar] [PubMed]
- Quesada-García, M.P.; Prados-Sánchez, E.; Olmedo-Gaya, M.V.; Muñoz-Soto, E.; González-Rodríguez, M.P.; Valllecillo-Capilla, M. Measurement of dental implant stability by resonance frequency analysis: A review of the literature. Med. Oral. Patol. Oral. Cir. Bucal. 2009, 14, e538–e546. [Google Scholar] [CrossRef] [Green Version]
- Davies, J.E. Mechanisms of endosseous integration. Int. J. Prosthodont. 1998, 11, 391–401. [Google Scholar]
- Fanuscu, M.I.; Chang, T.L.; Akça, K. Effect of surgical techniques on primary implant stability and peri-implant bone. J. Oral. Maxillofac. Surg. 2007, 65, 2487–2491. [Google Scholar] [CrossRef]
- Turkyilmaz, I.; Tozum, T.F. Enhancing primary implant stability by undersizing implant site preparation: A human cadaver study. J. Stomatol. Oral. Maxillofac. Surg. 2020, 121, 58–62. [Google Scholar] [CrossRef]
- Comuzzi, L.; Tumedei, M.; D’Arcangelo, C.; Piattelli, A.; Iezzi, G. An In Vitro Analysis on Polyurethane Foam Blocks of the Insertion Torque (IT) Values, Removal Torque Values (RTVs), and Resonance Frequency Analysis (RFA) Values in Tapered and Cylindrical Implants. Int. J. Environ. Res. Public Health 2021, 18, 9238. [Google Scholar] [CrossRef]
- Attanasio, F.; Antonelli, A.; Brancaccio, Y.; Averta, F.; Figliuzzi, M.M.; Fortunato, L.; Giudice, A. Primary Stability of Three Different Osteotomy Techniques in Medullary Bone: An in Vitro Study. Dent. J. 2020, 8, 21. [Google Scholar] [CrossRef] [Green Version]
- Ahn, S.J.; Leesungbok, R.; Lee, S.W.; Heo, Y.K.; Kang, K.L. Differences in implant stability associated with various methods of preparation of the implant bed: An in vitro study. J. Prosthet. Dent. 2012, 107, 366–372. [Google Scholar] [CrossRef]
- Brouwers, J.; Buis, S.; de Groot, P.G.; de Laat, B.; Remijn, J.A. Resonance frequency analysis with two different devices after conventional implant placement with ridge preservation: A prospective pilot cohort study. Clin. Implant. Dent. Relat. Res. 2021, 23, 789–799. [Google Scholar] [CrossRef] [PubMed]
- Di Stefano, D.A.; Arosio, P.; Gastaldi, G.; Gherlone, E. The insertion torque-depth curve integral as a measure of implant primary stability: An in vitro study on polyurethane foam blocks. J. Prosthet. Dent. 2018, 120, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Daprile, G.; Piattelli, A.; Iezzi, G. Development of a new implant primary stability parameter: Insertion torque revisited. Clin. Implant. Dent. Relat. Res. 2013, 15, 637–644. [Google Scholar] [CrossRef] [PubMed]
- Sennerby, L.; Meredith, N. Implant stability measurements using resonance frequency analysis: Biological and biomechanical aspects and clinical implications. Periodontol. 2000 2008, 47, 51–66. [Google Scholar] [CrossRef] [PubMed]
- Lages, F.S.; Douglas-de Oliveira, D.W.; Costa, F.O. Relationship between implant stability measurements obtained by insertion torque and resonance frequency analysis: A systematic review. Clin. Implant. Dent. Relat. Res. 2018, 20, 26–33. [Google Scholar] [CrossRef]
- Monje, A.; Ravidà, A.; Wang, H.L.; Helms, J.A.; Brunski, J.B. Relationship Between Primary/Mechanical and Secondary/Biological Implant Stability. Int. J. Oral. Maxillofac. Implant. 2019, 34, s7–s23. [Google Scholar] [CrossRef]
- Valderrama, P.; Oates, T.W.; Jones, A.A.; Simpson, J.; Schoolfield, J.D.; Cochran, D.L. Evaluation of two different resonance frequency devices to detect implant stability: A clinical trial. J. Periodontol. 2007, 78, 262–272. [Google Scholar] [CrossRef]
- Rittel, D.; Dorogoy, A.; Haïat, G.; Shemtov-Yona, K. Resonant frequency analysis of dental implants. Med. Eng. Phys. 2019, 66, 65–74. [Google Scholar] [CrossRef] [Green Version]
- Sim, C.P.; Lang, N.P. Factors influencing resonance frequency analysis assessed by Osstell mentor during implant tissue integration: I. Instrument positioning, bone structure, implant length. Clin. Oral. Implant. Res. 2010, 21, 598–604. [Google Scholar] [CrossRef]
- Herrero-Climent, M.; Santos-García, R.; Jaramillo-Santos, R.; Romero-Ruiz, M.M.; Fernández-Palacin, A.; Lázaro-Calvo, P.; Bullón, P.; Ríos-Santos, J.V. Assessment of Osstell ISQ’s reliability for implant stability measurement: A cross-sectional clinical study. Med. Oral. Patol. Oral. Cir. Bucal. 2013, 18, e877–e882. [Google Scholar] [CrossRef]
- Raz, P.; Meir, H.; Levartovsky, S.; Peleg, M.; Sebaoun, A.; Beitlitum, I. Reliability and Correlation of Different Devices for the Evaluation of Primary Implant Stability: An In Vitro Study. Materials 2021, 14, 5537. [Google Scholar] [CrossRef] [PubMed]
- Devlin, H.; Horner, K.; Ledgerton, D. A comparison of maxillary and mandibular bone mineral densities. J. Prosthet. Dent. 1998, 79, 323–327. [Google Scholar] [CrossRef]
- Farronato, D.; Manfredini, M.; Stocchero, M.; Caccia, M.; Azzi, L.; Farronato, M. Influence of Bone Quality, Drilling Protocol, Implant Diameter/Length on Primary Stability: An In Vitro Comparative Study on Insertion Torque and Resonance Frequency Analysis. J. Oral. Implantol. 2020, 46, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Silva, R.; Villalón, P.; Cáceres, F. Effect of macro-design in the primary stability of short and extra-short implants using resonance frequency analysis. An ex vivo study. J. Oral. Biol. Craniofac. Res. 2020, 10, 603–607. [Google Scholar] [CrossRef] [PubMed]
- Falco, A.; Berardini, M.; Trisi, P. Correlation Between Implant Geometry, Implant Surface, Insertion Torque, and Primary Stability: In Vitro Biomechanical Analysis. Int. J. Oral. Maxillofac. Implant. 2018, 33, 824–830. [Google Scholar] [CrossRef]
- Turkyilmaz, I.; Sennerby, L.; McGlumphy, E.A.; Tözüm, T.F. Biomechanical aspects of primary implant stability: A human cadaver study. Clin. Implant. Dent. Relat. Res. 2009, 11, 113–119. [Google Scholar] [CrossRef]
- Friberg, B.; Sennerby, L.; Linden, B.; Gröndahl, K.; Lekholm, U. Stability measurements of one-stage Brånemark implants during healing in mandibles. A clinical resonance frequency analysis study. Int. J. Oral. Maxillofac. Surg. 1999, 28, 266–272. [Google Scholar] [CrossRef]
- Aparicio, C.; Lang, N.P.; Rangert, B. Validity and clinical significance of biomechanical testing of implant/bone interface. Clin. Oral. Implant. Res. 2006, 17 (Suppl. S2), 2–7. [Google Scholar] [CrossRef]
- Bischof, M.; Nedir, R.; Szmukler-Moncler, S.; Bernard, J.P.; Samson, J. Implant stability measurement of delayed and immediately loaded implants during healing. Clin. Oral. Implant. Res. 2004, 15, 529–539. [Google Scholar] [CrossRef]
- Balshi, S.F.; Allen, F.D.; Wolfinger, G.J.; Balshi, T.J. A resonance frequency analysis assessment of maxillary and mandibular immediately loaded implants. Int. J. Oral. Maxillofac. Implant. 2005, 20, 584–594. [Google Scholar]
- Ostman, P.O.; Hellman, M.; Wendelhag, I.; Sennerby, L. Resonance frequency analysis measurements of implants at placement surgery. Int. J. Prosthodont. 2006, 19, 77–83; discussion 84. [Google Scholar] [PubMed]
- Zix, J.; Kessler-Liechti, G.; Mericske-Stern, R. Stability measurements of 1-stage implants in the maxilla by means of resonance frequency analysis: A pilot study. Int. J. Oral. Maxillofac. Implant. 2005, 20, 747–752. [Google Scholar]
- Ibrahim, A.; Heitzer, M.; Bock, A.; Peters, F.; Möhlhenrich, S.C.; Hölzle, F.; Modabber, A.; Kniha, K. Relationship between Implant Geometry and Primary Stability in Different Bony Defects and Variant Bone Densities: An In Vitro Study. Materials 2020, 13, 4349. [Google Scholar] [CrossRef]
- Herrero-Climent, M.; Lemos, B.F.; Herrero-Climent, F.; Falcao, C.; Oliveira, H.; Herrera, M.; Gil, F.J.; Ríos-Carrasco, B.; Ríos-Santos, J.V. Influence of Implant Design and Under-Preparation of the Implant Site on Implant Primary Stability. An In Vitro Study. Int. J. Environ. Res. Public Health 2020, 17, 4436. [Google Scholar] [CrossRef] [PubMed]
- Giudice, A.; Bennardo, F.; Antonelli, A.; Barone, S.; Wagner, F.; Fortunato, L.; Traxler, H. Influence of clinician’s skill on primary implant stability with conventional and piezoelectric preparation techniques: An ex-vivo study. J. Biol. Regul. Homeost. Agents 2020, 34, 739–745. [Google Scholar] [CrossRef] [PubMed]

| Difference | IT (N/Cm) | AV_O2 (ISQ) | AV_P2 (ISQ) |
|---|---|---|---|
| Bone (D-S) | 2.566 ** | 9.669 ** | 10.47 ** |
| Length (13–8) | −1.619 * | 3.521 ** | 4.402 ** |
| Implant (CC-IH) | 6.729 ** | 7.607 ** | 9.491 ** |
| Diff | p < 0.05 * p < 0.01 ** | IT (N/Cm) | AV_O2 (ISQ) | AV_P2 (ISQ) |
|---|---|---|---|---|
| Bone& Implant design | sof:CC-D:CC | −4.111 ** | −7.836 * | −10.05 * |
| D:IH-D:CC | −8.346 ** | −5.856 * | −9.173 * | |
| sof:IH-D:CC | −9.189 ** | −17.23 * | −19.87 * | |
| D:IH-sof:CC | −4.235 ** | 1.98 | 0.8741 | |
| sof:IH-sof:CC | −5.078 ** | −9.398 * | −9.818 * | |
| sof:IH-D:IH | −0.8429 | −11.38 * | −10.69 * |
| Diff | p < 0.05 * p < 0.01 ** | IT (N/Cm) | AV_O2 (ISQ) | AV_P2 (ISQ) |
|---|---|---|---|---|
| Bone & length | sof:8–D:8 | −3.362 * | −10.45 * | −11.14 * |
| D:13–D:8 | −2.415 | 2.679 | 3.665 * | |
| sof:13–D:8 | −4.167 ** | −6.071 * | −5.983 * | |
| D:13–sof:8 | 0.9477 | 13.13 * | 14.81 * | |
| sof:13–sof:8 | −0.8048 | 4.384 * | 5.158 * | |
| sof:13–D:13 | −1.753 | −8.75 * | −9.647 * |
| Diff | p < 0.05 * p < 0.01 ** | IT (N/Cm) | AV_O2 (ISQ) | AV_P2 (ISQ) |
|---|---|---|---|---|
| Length & Implant design | 13:CC–8:CC | 0.3635 | 2.907 * | 3.548 * |
| 8:IH–8:CC | −4.716 ** | −8.126 * | −10.22 * | |
| 13:IH–8:CC | −8.515 ** | −4.148 * | −5.162 * | |
| 8:IH–13:CC | −5.08 ** | −11.03 * | −13.77 * | |
| 13:IH–13:CC | −8.878 ** | −7.054 * | −8.71 * | |
| 13:IH–8:IH | 3.798 ** | 3.979 * | 5.063 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raz, P.; Meir, H.; Levartovsky, S.; Sebaoun, A.; Beitlitum, I. Primary Implant Stability Analysis of Different Dental Implant Connections and Designs—An In Vitro Comparative Study. Materials 2022, 15, 3072. https://doi.org/10.3390/ma15093072
Raz P, Meir H, Levartovsky S, Sebaoun A, Beitlitum I. Primary Implant Stability Analysis of Different Dental Implant Connections and Designs—An In Vitro Comparative Study. Materials. 2022; 15(9):3072. https://doi.org/10.3390/ma15093072
Chicago/Turabian StyleRaz, Perry, Haya Meir, Shifra Levartovsky, Alon Sebaoun, and Ilan Beitlitum. 2022. "Primary Implant Stability Analysis of Different Dental Implant Connections and Designs—An In Vitro Comparative Study" Materials 15, no. 9: 3072. https://doi.org/10.3390/ma15093072
APA StyleRaz, P., Meir, H., Levartovsky, S., Sebaoun, A., & Beitlitum, I. (2022). Primary Implant Stability Analysis of Different Dental Implant Connections and Designs—An In Vitro Comparative Study. Materials, 15(9), 3072. https://doi.org/10.3390/ma15093072







