Three-Dimensional (3D) Stereolithographic Tooth Replicas Accuracy Evaluation: In Vitro Pilot Study for Dental Auto-Transplant Surgical Procedures
Abstract
:1. Introduction
2. Materials and Methods
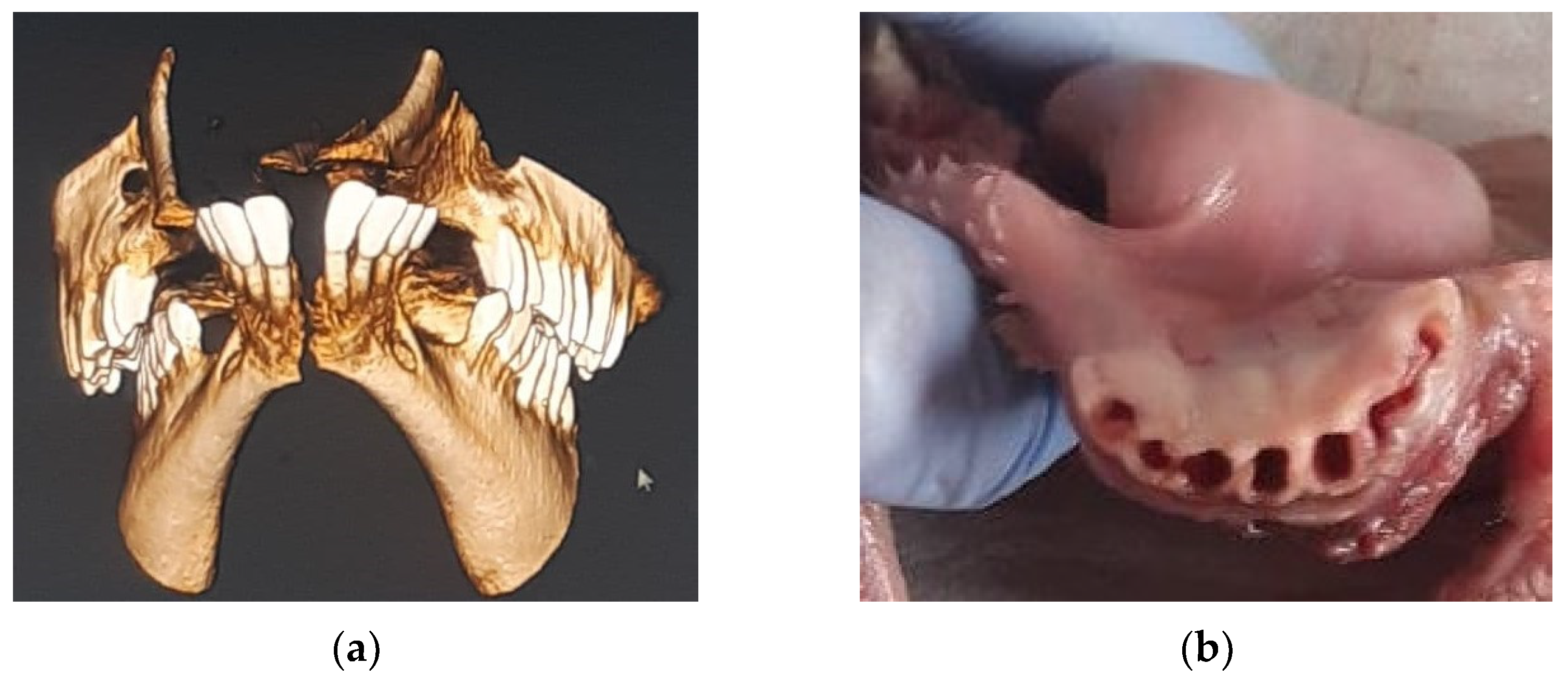
2.1. Radiological Acquisition and 3D Printing
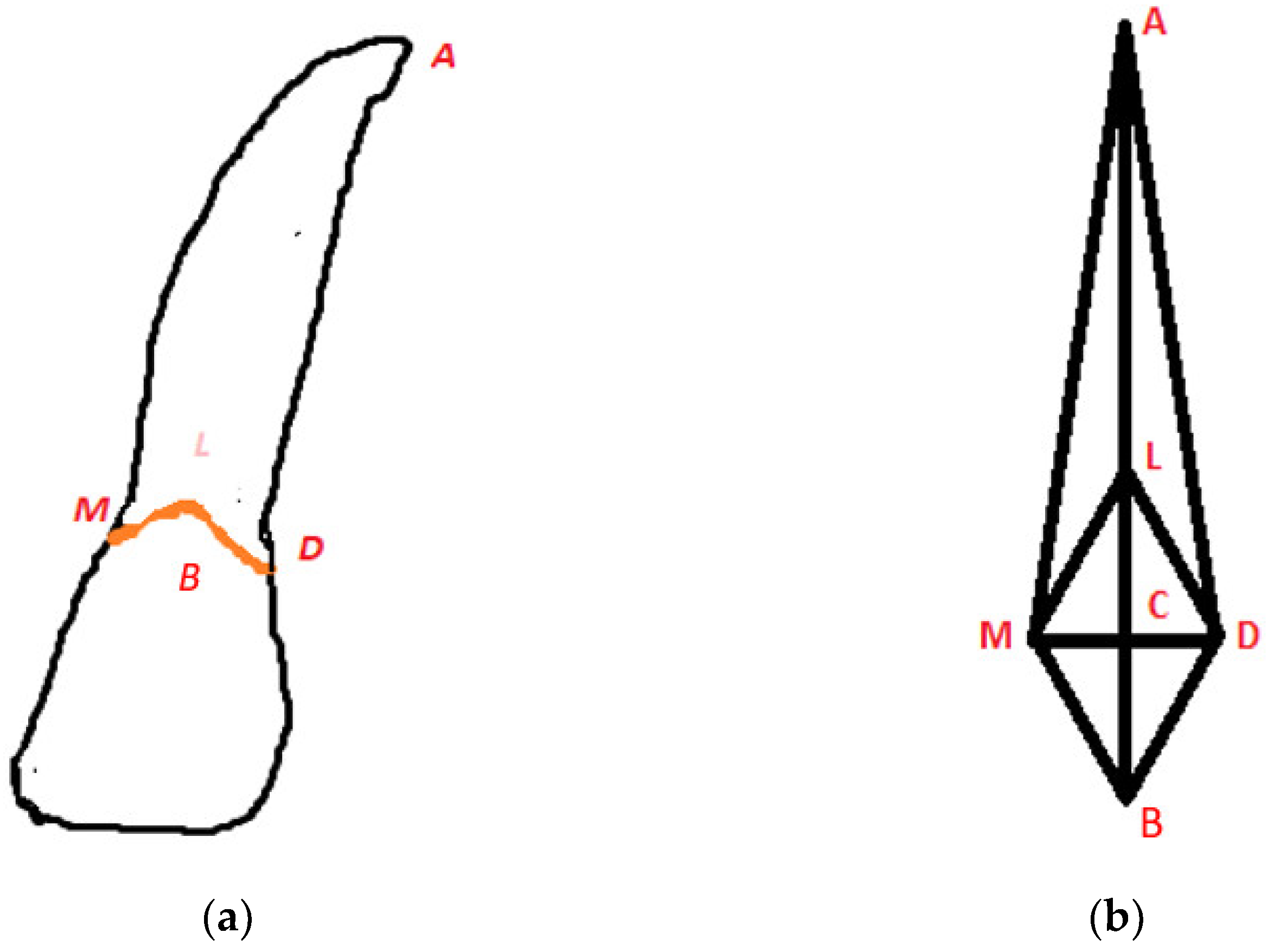
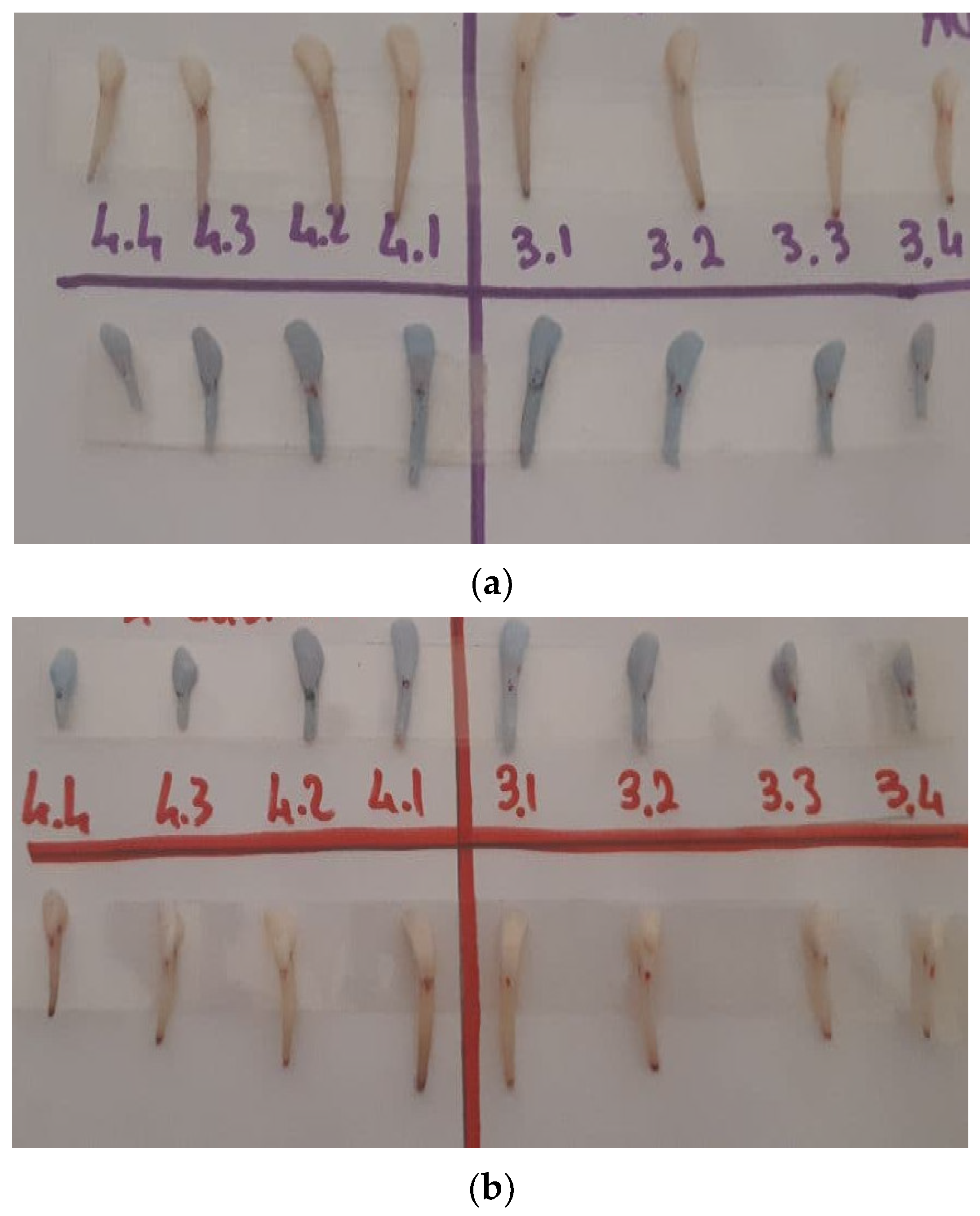
2.2. Tooth Extraction and Samples Measurement
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| A | Apex |
| AD | Distal point apex |
| AM | Mesial point apex |
| CBCT | Cone Beam Computer Tomography |
| CEJ | Cement–enamel junction |
| DICOM | Digital Imaging and Communications in Medicine |
| FOV | Field of View |
| LA | Lingual point apex |
| MD | Mesio-distal |
| PDL | Periodontal ligament |
| SD | Standard Deviation |
| STL | Standard Triangulation Language |
| BA | Buccal point apex |
| BL | Buccal lingual |
References
- Verweij, J.P.; Jongkees, F.A.; Moin, D.A.; Wismeijer, D.; Van Merkesteyn, J.P.R. Autotransplantation of teeth using computer-aided rapid prototyping of a three-dimensional replica of the donor tooth: A systematic literature review. Int. J. Oral Maxillofac. Surg. 2017, 46, 1466–1474. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.-S.; Jiang, H.B. A Review of 3D Printing in Dentistry: Technologies, Affecting Factors, and Applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef] [PubMed]
- Park, J.M.; Hong, Y.S.; Park, E.J.; Heo, S.J.; Oh, N. Clinical evaluations of cast gold alloy, machinable zirconia, and semiprecious alloy crowns: A multicenter study. J. Prosthet. Dent. 2016, 115, 684–691. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, J.O.; Paulsen, H.U.; Yu, Z.; Schwartz, O. A long-term study of 370 auto transplanted premolars. Part III. Periodontal healing subsequent to transplantation. Eur. J. Orthod. 1990, 12, 25–37. [Google Scholar] [CrossRef] [PubMed]
- Ahlberg, K.; Bystedt, H.; Eliasson, S.; Odenrick, L. Long-Term Evaluation of Autotransplanted Maxillary Canines with Completed Root Formation. Acta Odontol. Scand. 1983, 41, 23–31. [Google Scholar] [CrossRef]
- Andersson, L.; Andreasen, J.O.; Day, P.; Heithersay, G.; Trope, M.; Di Angelis, A.J.; Kenny, D.J.; Sigurdsson, A.; Bourguignon, C.; Flores, M.T.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent. Traumatol. 2020, 28, 370–375. [Google Scholar] [CrossRef]
- Armstrong, L.; O’Reilly, C.; Ahmed, B. Autotransplantation of third molars: A literature review and preliminary protocols. Br. Dent. J. 2020, 228, 247–251. [Google Scholar] [CrossRef]
- Anssari Moin, D.; Verweij, J.P.; Waars, H.; van Merkesteyn, R.; Wismeijer, D. Accuracy of Computer-Assisted Template-Guided Autotransplantation of Teeth with Custom Three-Dimensional Designed/Printed Surgical Tooling: A Cadaveric Study. J. Oral Maxillofac. Surg. 2017, 75, 925.e1–925.e7. [Google Scholar] [CrossRef]
- Tsukiboshi, M. Autotransplantation of teeth: Requirements for predictable success. Dent. Traumatol. 2002, 18, 157–180. [Google Scholar] [CrossRef]
- Verweij, J.P.; Moin, D.A.; Mensink, G.; Nijkamp, P.; Wismeijer, D.; van Merkesteyn, J.P.R. Autotransplantation of Premolars With a 3-Dimensional Printed Titanium Replica of the Donor Tooth Functioning as a Surgical Guide: Proof of Concept. J. Oral Maxillofac. Surg. 2016, 74, 1114–1119. [Google Scholar] [CrossRef]
- Berry, E.; Brown, J.M.; Connell, M.; Craven, C.M.; Efford, N.D.; Radjenovic, A.; Smith, M.A. Preliminary experience with medical applications of rapid prototyping by selective laser sintering. Med. Eng. Phys. 1997, 19, 90–96. [Google Scholar] [CrossRef]
- Sokolowski, A.A.; Sokolowski, A.A.; Kammerhofer, J.; Madreiter-Sokolowski, C.T.; Payer, M.; Koller, M.; Jakse, N.; Wegscheider, W.A. Accuracy assessment of 3D-printed tooth replicas. Int. J. Comput. Dent. 2019, 22, 321–329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rebong, R.E.; Stewart, K.T.; Utreja, A.; Ghoneima, A.A. Accuracy of three-dimensional dental resin models created by fused deposition modeling, stereolithography, and Polyjet prototype technologies: A comparative study. Angle Orthod. 2018, 88, 363–369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.M.; Jeon, J.; Koak, J.Y.; Kim, S.K.; Heo, S.J. Dimensional accuracy and surface characteristics of 3D-printed dental casts. J. Prosthet. Dent. 2020, 126, 427–437. [Google Scholar] [CrossRef]
- Teixeira, C.S.; Pasternak, B., Jr.; Vansan, L.P.; Sousa-Neto, M.D. Autogenous transplantation of teeth with complete root formation: Two case reports. J. Endod. 2006, 39, 977–985. [Google Scholar] [CrossRef]
- Jang, J.H.; Lee, S.J.; Kim, E. Autotransplantation of Immature Third Molars Using a Computer-aided Rapid Prototyping Model: A Report of 4 Cases. J. Endod. 2013, 39, 1461–1466. [Google Scholar] [CrossRef]
- Lee, S.J.; Kim, E. Minimizing the extra-oral time in autogeneous tooth transplantation: Use of computer-aided rapid prototyping (CARP) as a duplicate model tooth. Restor. Dent. Endod. 2012, 37, 136–141. [Google Scholar] [CrossRef] [Green Version]
- Van der Meer, W.J.; Jansma, J.; Delli, K.; Livas, C. Computer-aided planning and surgical guiding system fabrication in premolar autotransplantation: A 12-month follow up. Dent. Traumatol. 2015, 32, 336–340. [Google Scholar] [CrossRef]
- Chang, P.S.; Parker, T.H.; Patrick, C.W., Jr.; Miller, M.J. The Accuracy of Stereolithography in Planning Craniofacial Bone Replacement. J. Craniofac. Surg. 2003, 14, 164–170. [Google Scholar] [CrossRef]
- Lill, W.; Solar, P.; Ulm, C.; Watzek, G.; Blahout, R.; Matejka, M. Reproducibility of three-dimensional CT-assisted model production in the maxillofacial area. Br. J. Oral Maxillofac. Surg. 1992, 30, 233–236. [Google Scholar] [CrossRef]
- Hale, M.L. Autogenous transplants. Oral Surg. 1956, 9, 76. [Google Scholar] [CrossRef]
- Reich, P.P. Autogenous Transplantation of Maxillary and Mandibular Molars. J. Oral Maxillofac. Surg. 2008, 66, 2314–2317. [Google Scholar] [CrossRef] [PubMed]
- Pecci Lloret, M.P.; Martínez, E.P.; Rodríguez Lozano, F.J.; Pecci Lloret, M.R.; Guerrero Gironés, J.; Riccitiello, F.; Spagnuolo, G. Influencing Factors in Autotransplantation of Teeth with Open Apex: A Review of the Literature. Appl. Sci. 2021, 11, 4037. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Paulsen, H.U.; Yu, Z.; Bayer, T.; Schwartz, O. A long-term study of 370 autotransplanted premolars. Part II. Tooth survival and pulp healing subsequent to transplantation. Eur. J. Orthod. 1990, 12, 14–24. [Google Scholar] [CrossRef]
- Jakobsen, C.; Stokbro, K.; Kier-Swiatecka, E.; Ingerslev, J.; Thorn, J.J. Autotransplantation of premolars: Does surgeon experience matter? Int. J. Oral Maxillofac. Surg. 2018, 47, 1604–1608. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Chen, J.; Xie, F.; Liu, H.; Niu, G.; Zhou, L. Autotransplantation of mature impacted tooth to a fresh molar socket using a 3D replica and guided bone regeneration: Two years retrospective case series. BMC Oral Health 2019, 19, 248. [Google Scholar] [CrossRef] [Green Version]
- Czochrowska, E.M.; Stenvik, A.; Bjercke, B.; Zachrisson, B.U. Outcome of tooth transplantation: Survival and success rates 17–41 years posttreatment. Am. J. Orthod. Dentofac. Orthop. 2002, 121, 110–119. [Google Scholar] [CrossRef] [Green Version]
- Jonsson, T.; Sigurdsson, T.J. Autotransplantation of premolars to premolar sites. A long-term follow-up study of 40 consecutive patients. Am. J. Orthod. Dentofac. Orthop. 2004, 125, 668–675. [Google Scholar] [CrossRef]
- Boschini, L.; Melillo, M.; Berton, F. Long term survival of mature autotransplanted teeth: A retrospective single center analysis. J. Dent. 2020, 98, 103371. [Google Scholar] [CrossRef]
- Kafourou, V.; Tong, H.J.; Day, P.; Houghton, N.; Spencer, R.J.; Duggal, M. Outcomes and prognostic factors that influence the success of tooth autotransplantation in children and adolescents. Dent. Traumatol. 2017, 33, 393–399. [Google Scholar] [CrossRef]
- Tang, H.; Shen, Z.; Hou, M.; Wu, L. Autotransplantation of mature and immature third molars in 23 Chinese patients: A clinical and radiological follow-up study. BMC Oral Health 2017, 17, 163. [Google Scholar] [CrossRef] [Green Version]
- Strbac, G.D.; Giannis, K.; Mittlböck, M.; Fuerst, G.; Zechner, W.; Stavropoulos, A.; Ulm, C. Survival rate of autotransplanted teeth after 5 years—A retrospective cohort study. J. Cranio Maxillofac. Surg. 2017, 45, 1143–1149. [Google Scholar] [CrossRef] [PubMed]
- Denys, D.; Shahbazian, M.; Jacobs, R.; Laenen, A.; Wyatt, J.; Vinckier, F.; Willems, G. Importance of root development in autotransplantations: A retrospective study of 137 teeth with a follow-up period varying from 1 week to 14 years. Eur. J. Orthod. 2013, 35, 680–688. [Google Scholar] [CrossRef] [PubMed]
- Ronchetti, M.F.; Valdec, S.; Pandis, N.; Locher, M.; van Waes, H. A retrospective analysis of factors influencing the success of autotransplanted posterior teeth. Prog. Orthod. 2015, 16, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ezeldeen, M.; Wyatt, J.; Al-Rimawi, A.; Coucke, W.; Shaheen, E.; Lambrichts, I.; Willems, G.; Politis, C.; Jacobs, R. Use of CBCT Guidance for Tooth Autotransplantation in Children. J. Dent. Res. 2019, 98, 406–413. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Jung, J.Y.; Cha, I.H.; Kum, K.Y.; Lee, S.J. Evaluation of the prognosis and causes of failure in 182 cases of autogenous tooth transplantation. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2005, 100, 112–119. [Google Scholar] [CrossRef]
- Vinci, R.; Manacorda, M.; Abundo, R.; Lucchina, A.G.; Scarano, A.; Crocetta, C.; Lo Muzio, L.; Gherlone, E.F.; Mastrangelo, F. Accuracy of Edentulous Computer-Aided Implant Surgery as Compared to Virtual Planning: A Retrospective Multicenter Study. J. Clin. Med. 2020, 9, 774. [Google Scholar] [CrossRef] [Green Version]
- Barker, T.M.; Earwaker, W.J.S.; Lisle, D.A. Accuracy of stereolithographic models of human anatomy. Australas. Radiol. 1994, 38, 106–111. [Google Scholar] [CrossRef]
- Hada, T.; Kanazawa, M.; Iwaki, M.; Arakida, T.; Soeda, Y.; Katheng, A.; Otake, R.; Minakuchi, S. Effect of Printing Direction on the Accuracy of 3D-Printed Dentures Using Stereolithography Technology. Materials 2020, 13, 3405. [Google Scholar] [CrossRef]
- Kim, Y.H.; Jung, B.Y.; Han, S.S.; Woo, C.W. Accuracy evaluation of 3D printed interim prosthesis fabrication using a CBCT scanning based digital model. PLoS ONE 2020, 15, e0240508. [Google Scholar] [CrossRef]
- Ligon, S.C.; Liska, R.; Stampfl, J.; Gurr, M.; Mülhaupt, R. Polymers for 3D Printing and Customized Additive Manufacturing. Chem. Rev. 2017, 117, 10212–10290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gundrati, N.B.; Chakraborty, P.; Zhou, C.; Chung, D.D.L. Effects of printing conditions on the molecular alignment of three-dimensionally printed polymer. Compos. Part B Eng. 2018, 134, 164–168. [Google Scholar] [CrossRef]
- Sood, A.K.; Ohdar, R.K.; Mahapatra, S.S. Improving dimensional accuracy of Fused Deposition Modelling processed part using grey Taguchi method. Mater. Des. 2009, 30, 4243–4252. [Google Scholar] [CrossRef]
- Jiang, K.Y.; Gu, Y.H. Controlling Parameters for Polymer Melting and Extrusion in FDM. Key Eng. Mater. 2004, 259–260, 667–671. [Google Scholar] [CrossRef]
- Thrimurthulu, K.; Pandey, P.M.; Reddy, N.V. Optimum part deposition orientation in fused deposition modeling. Int. J. Mach. Tools Manuf. 2004, 44, 585–594. [Google Scholar] [CrossRef]
- Biron, M. Material Selection of Thermoplastic. Practical and Advanced Information for Plastic Engineers; Elsevier: Oxford, UK, 2014; pp. 391–393. [Google Scholar]
- National Center for Biotechnology Information. PubChem Substance Record for SID 134996936, 14GUK8I73Z. Available online: https://pubchem.ncbi.nlm.nih.gov/substance/134996936 (accessed on 9 December 2021).

| Error Percentage (%) | ||||||
|---|---|---|---|---|---|---|
| CEJ | Root | |||||
| Tooth | Mesio/Distal | Vestib/Lingual | M/A | D/A | B/A | L/A |
| 3.1 a1 | 0.01 | 0.04 | 0.29 | 0.33 | 0.37 | 0.35 |
| 3.2 a1 | 0.04 | 0.02 | 0.33 | 0.37 | 0.53 | 0.54 |
| 3.3 a1 | 0.04 | 0.02 | 0.39 | 0.39 | 0.42 | 0.40 |
| 3.3 a1 | 0.04 | 0.07 | 0.42 | 0.43 | 0.53 | 0.42 |
| 4.1 a1 | 0.05 | 0.09 | 0.26 | 0.27 | 0.23 | 0.24 |
| 4.2 a1 | 0.03 | 0.00 | 0.39 | 0.35 | 0.41 | 0.33 |
| 4.3 a1 | 0.07 | 0.01 | 0.59 | 0.59 | 0.41 | 0.39 |
| 4.4 a1 | 0.01 | 0.02 | 0.51 | 0.53 | 0.53 | 0.45 |
| 3.1 a2 | 0.06 | 0.03 | 0.26 | 0.26 | 0.35 | 0.30 |
| 3.2 a2 | 0.02 | 0.36 | 0.29 | 0.31 | 0.40 | 0.37 |
| 3.3 a2 | 0.05 | 0.07 | 0.32 | 0.39 | 0.39 | 0.41 |
| 3.3 a2 | 0.06 | 0.03 | 0.32 | 0.30 | 0.36 | 0.35 |
| 4.1 a2 | 0.07 | 0.03 | 0.29 | 0.30 | 0.34 | 0.31 |
| 4.2 a2 | 0.02 | 0.00 | 0.45 | 0.37 | 0.50 | 0.42 |
| 4.3 a2 | 0.01 | 0.15 | 0.56 | 0.51 | 0.55 | 0.55 |
| 4.4 a2 | 0.07 | 0.00 | 0.53 | 0.51 | 0.52 | 0.52 |
| Average | 0.04 | 0.06 | 0.39 | 0.39 | 0.43 | 0.40 |
| Error (%) | 4.17 | 6.13 | 39.42 | 39.22 | 43.11 | 39.92 |
| Stand Dev | 0.02 | 0.09 | 0.11 | 0.09 | 0.09 | 0.08 |
| Error Percentage (%) | |
|---|---|
| Tooth Number | Basic Area |
| 3.1 a1 | 0.05 |
| 3.2 a1 | 0.06 |
| 3.3 a1 | 0.05 |
| 3.3 a1 | 0.11 |
| 4.1 a1 | 0.14 |
| 4.2 a1 | 0.04 |
| 4.3 a1 | 0.08 |
| 4.4 a1 | 0.03 |
| 3.1 a2 | 0.09 |
| 3.2 a2 | 0.38 |
| 3.3 a2 | 0.12 |
| 3.3 a2 | 0.09 |
| 4.1 a2 | 0.10 |
| 4.2 a2 | 0.02 |
| 4.3 a2 | 0.14 |
| 4.4 a2 | 0.07 |
| Average | 0.098 |
| Error (%) | 9.80 |
| Stand Dev | 0.083 |
| Error Percentage (%) | |
|---|---|
| Tooth Number | Volume |
| 3.1 a1 | 0.37 |
| 3.2 a1 | 0.48 |
| 3.3 a1 | 0.44 |
| 3.3 a1 | 0.52 |
| 4.1 a1 | 0.38 |
| 4.2 a1 | 0.40 |
| 4.3 a1 | 0.55 |
| 4.4 a1 | 0.53 |
| 3.1 a2 | 0.36 |
| 3.2 a2 | 0.36 |
| 3.3 a2 | 0.46 |
| 3.3 a2 | 0.39 |
| 4.1 a2 | 0.38 |
| 4.2 a2 | 0.42 |
| 4.3 a2 | 0.62 |
| 4.4 a2 | 0.57 |
| Average | 0.46 |
| Error (%) | 45.54 |
| Stand Dev | 0.082 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mastrangelo, F.; Battaglia, R.; Natale, D.; Quaresima, R. Three-Dimensional (3D) Stereolithographic Tooth Replicas Accuracy Evaluation: In Vitro Pilot Study for Dental Auto-Transplant Surgical Procedures. Materials 2022, 15, 2378. https://doi.org/10.3390/ma15072378
Mastrangelo F, Battaglia R, Natale D, Quaresima R. Three-Dimensional (3D) Stereolithographic Tooth Replicas Accuracy Evaluation: In Vitro Pilot Study for Dental Auto-Transplant Surgical Procedures. Materials. 2022; 15(7):2378. https://doi.org/10.3390/ma15072378
Chicago/Turabian StyleMastrangelo, Filiberto, Rossella Battaglia, Dario Natale, and Raimondo Quaresima. 2022. "Three-Dimensional (3D) Stereolithographic Tooth Replicas Accuracy Evaluation: In Vitro Pilot Study for Dental Auto-Transplant Surgical Procedures" Materials 15, no. 7: 2378. https://doi.org/10.3390/ma15072378
APA StyleMastrangelo, F., Battaglia, R., Natale, D., & Quaresima, R. (2022). Three-Dimensional (3D) Stereolithographic Tooth Replicas Accuracy Evaluation: In Vitro Pilot Study for Dental Auto-Transplant Surgical Procedures. Materials, 15(7), 2378. https://doi.org/10.3390/ma15072378







