Stain Susceptibility of 3D-Printed Nanohybrid Composite Restorative Material and the Efficacy of Different Stain Removal Techniques: An In Vitro Study
Abstract
:1. Introduction
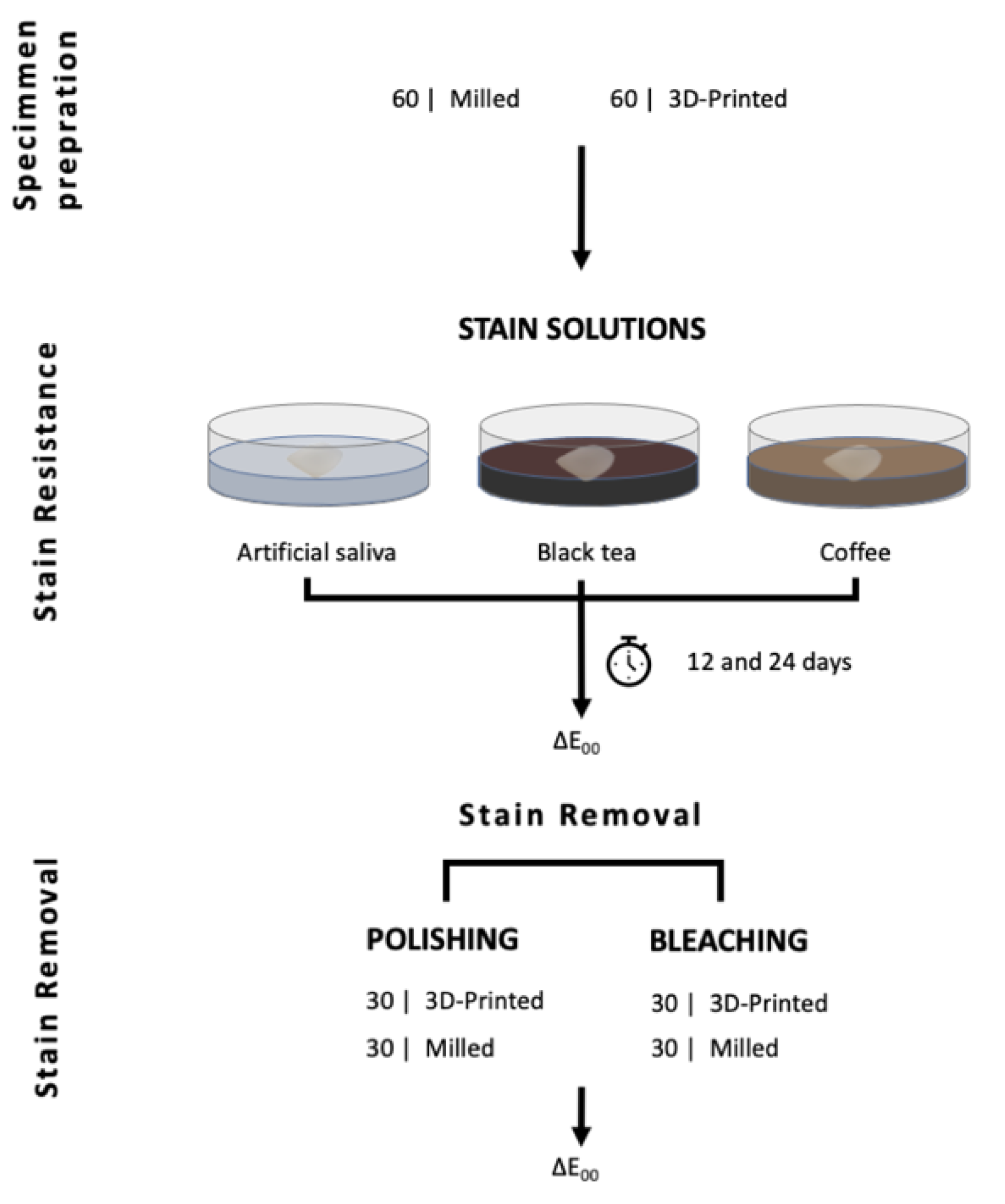
2. Materials and Methods
2.1. Color Measurement
2.2. Stain Removal
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Van Noort, R. The future of dental devices is digital. Dent. Mater. 2012, 28, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Abduo, J.; Lyons, K.; Bennamoun, M. Trends in computer-aided manufacturing in prosthodontics: A review of the available streams. Int. J. Dent. 2014, 2014, 783948. [Google Scholar] [CrossRef] [Green Version]
- Branco, A.C.; Silva, R.; Santos, T.; Jorge, H.; Rodrigues, A.; Fernandes, R.; Bandarra, S.; Barahona, I.; Matos, A.; Lorenz, K.; et al. Suitability of 3D printed pieces of nanocrystalline zirconia for dental applications. Dent. Mater. 2020, 36, 442–455. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, N.; Wismeijer, D.; Osman, R.B. Additive Manufacturing Techniques in Prosthodontics: Where Do We Currently Stand? A Critical Review. Int. J. Prosthodont. 2017, 30, 474–484. [Google Scholar] [CrossRef] [PubMed]
- Al Mortadi, N.; Eggbeer, D.; Lewis, J.; Williams, R.J. CAD/CAM/AM applications in the manufacture of dental appliances. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 727–733. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R. Does build angle have an influence on surface roughness of anterior 3D-printed restorations? An in-vitro study. Int. J. Prosthodont. 2021, 34, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Mostafavi, D.; Methani, M.; Piedra-Cascón, W.; Zandinejad, A.; Att, W.; Revilla-León, M. Influence of the polymerization post-processing procedures on the accuracy of additively manufactured dental model material. Int. J. Prosthodont. 2021. [Google Scholar] [CrossRef]
- Kim, J.-E.; Choi, W.-H.; Lee, D.; Shin, Y.; Park, S.-H.; Roh, B.-D.; Kim, D. Color and Translucency Stability of Three-Dimensional Printable Dental Materials for Crown and Bridge Restorations. Materials 2021, 14, 650. [Google Scholar] [CrossRef]
- Shin, J.-W.; Kim, J.-E.; Choi, Y.-J.; Shin, S.-H.; Nam, N.-E.; Shim, J.-S.; Lee, K.-W. Evaluation of the color stability of 3D-printed crown and bridge materials against various sources of discoloration: An in vitro study. Materials 2020, 13, 5359. [Google Scholar] [CrossRef]
- Almejrad, L.; Yang, C.; Morton, D.; Lin, W. The Effects of Beverages and Surface Treatments on the Color Stability of 3D-Printed Interim Restorations. J. Prosthodont. 2021. [Google Scholar] [CrossRef]
- Fernandes, B.M.; Tanaka, M.H.; De Oliveira, A.L.B.M.; Scatolin, R.S. Color stability of dental enamel bleached with violet LED associated with or without low concentration peroxide gels. Photodiagn. Photodyn. Ther. 2021, 33, 102101. [Google Scholar] [CrossRef]
- Al-Angari, S.S.; Eckert, G.J.; Sabrah, A.H. Color stability, Roughness, and Microhardness of Enamel and Composites Submitted to Staining/Bleaching Cycles. Saudi Dent. J. 2021, 33, 215–221. [Google Scholar] [CrossRef]
- Sinjari, B.; D’Addazio, G.; Bozzi, M.; Santilli, M.; Traini, T.; Murmura, G.; Caputi, S. SEM Analysis of Enamel Abrasion after Air Polishing Treatment with Erythritol, Glycine and Sodium Bicarbonate. Coatings 2019, 9, 549. [Google Scholar] [CrossRef] [Green Version]
- Alharbi, A.; Ardu, S.; Bortolotto, T.; Krejci, I. In-office bleaching efficacy on stain removal from CAD/CAM and direct resin composite materials. J. Esthet. Restor. Dent. 2018, 30, 51–58. [Google Scholar] [CrossRef]
- DWS. DFAB Performance and Desing. 2019, p. 15. Available online: https://www.dwssystems.com/blog/wp-content/uploads/2019/03/DWS-DFAB_en_low.pdf (accessed on 20 September 2021).
- Alharbi, N.; Osman, R.B.; Wismeijer, D. Factors Influencing the Dimensional Accuracy of 3D-Printed Full-Coverage Dental Restorations Using Stereolithography Technology. Int. J. Prosthodont. 2016, 29, 503–510. [Google Scholar] [CrossRef] [Green Version]
- Olms, C.; Setz, J.M. The repeatability of digital shade measurement—A clinical study. Clin. Oral Investig. 2013, 17, 1161–1166. [Google Scholar] [CrossRef] [PubMed]
- Dozić, A.; Kleverlaan, C.J.; El-Zohairy, A.; Feilzer, A.J.; Khashayar, G. Performance of five commercially available tooth color-measuring devices. J. Prosthodont. 2007, 16, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Ardu, S.; Duc, O.; Di Bella, E.; Krejci, I.; Daher, R. Color stability of different composite resins after polishing. Odontology 2018, 106, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Paravina, R.D.; Pérez, M.M.; Ghinea, R. Acceptability and perceptibility thresholds in dentistry: A comprehensive review of clinical and research applications. J. Esthet. Restor. Dent. 2019, 31, 103–112. [Google Scholar] [CrossRef]
- Jang, J.-H.; Kim, H.-Y.; Shin, S.-M.; Lee, C.-O.; Kim, D.; Choi, K.-K.; Kim, S.-Y. Clinical Effectiveness of Different Polishing Systems and Self-Etch Adhesives in Class V Composite Resin Restorations: Two-Year Randomized Controlled Clinical Trial. Oper. Dent. 2017, 42, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Al-Nahedh, H.N.; Awliya, W.Y. The effectiveness of four methods for stain removal from direct resin-based composite restorative materials. Saudi Dent. J. 2013, 25, 61–67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peñate, L.; Mercade, M.; Arregui, M.; Roig, M.; Basilio, J.; Cedeño, R. Color Stability of CAD/CAM Interim Material for Long-Term Fixed Dental Prostheses vs. Conventional Materials after Immersion in Different Staining Solutions. J. Compos. Sci. 2021, 5, 106. [Google Scholar] [CrossRef]
- Ardu, S.; Braut, V.; DI Bella, E.; Lefever, D. Influence of background on natural tooth colour coordinates: An in vivo evaluation. Odontology 2014, 102, 267–271. [Google Scholar] [CrossRef] [Green Version]
- Shetty, P.; Purayil, T.-P.; Ginjupalli, K.; Pentapati, K.-C. Effect of polishing technique and immersion in beverages on color stability of nanoceramic composites. J. Oral Biol. Craniofac. Res. 2021, 11, 53–56. [Google Scholar] [CrossRef] [PubMed]
- Sheriff, A.H.; Nasim, I. Effect of different beverages on staining ability of the composite resins. Drug Invent. Today 2019, 12, 184–188. [Google Scholar]
- Alaqeel, S. Effect of Grit-blasting on the Color Stability of Zirconia Ceramics Following Exposure to Beverages. Cureus 2020, 12, e7170. [Google Scholar] [CrossRef] [Green Version]
- Al Amri, M.D.; Labban, N.; Alhijji, S.; Alamri, H.; Iskandar, M.; Platt, J.A. In Vitro Evaluation of Translucency and Color Stability of CAD/CAM Polymer-Infiltrated Ceramic Materials after Accelerated Aging. J. Prosthodont. 2021, 30, 318–328. [Google Scholar] [CrossRef]
- Gruber, S.; Kamnoedboon, P.; Özcan, M.; Srinivasan, M. CAD/CAM Complete denture resins: An in vitro evaluation of color stability. J. Prosthodont. 2021, 30, 430–439. [Google Scholar] [CrossRef]
- Kang, Y.-A.; Lee, H.-A.; Chang, J.; Moon, W.; Chung, S.H.; Lim, B.-S. Color Stability of Dental Reinforced CAD/CAM Hybrid Composite Blocks Compared to Regular Blocks. Materials 2020, 13, 4722. [Google Scholar] [CrossRef]
- Arif, R.; Yilmaz, B.; Johnston, W.M. In vitro color stainability and relative translucency of CAD-CAM restorative materials used for laminate veneers and complete crowns. J. Prosthet. Dent. 2019, 122, 160–166. [Google Scholar] [CrossRef]
- Flaitz, C.M.; Hicks, M.J. Effects of carbamide peroxide whitening agents on enamel surfaces and caries-like lesion formation: An SEM and polarized light microscopic in vitro study. ASDC J. Dent. Child. 1996, 63, 249–256. [Google Scholar] [PubMed]



| Mean ∆E00 (±SD) | |||||
|---|---|---|---|---|---|
| Time | Immersion 12 Days | Immersion 24 Days | |||
| Fabrication | Background | Black | White | Black | White |
| Stain | |||||
| 3D-Printing | Artificial saliva | 0.64 (±26) | 0.63 (±0.26) | 1.15 (±0.26) | 1.34 (±0.25) |
| Tea | 9.61 (±0.68) | 9.36 (±0.84) | 14.83 (±0.84) | 14.79 (±1.07) | |
| Coffee | 19.65 (±1.35) | 19.66 (±1.11) | 32.47 (±1.29) | 32.68 (±1.51) | |
| Total | 9.97 (±7.88) | 9.88 (±7.88) | 16.15 (±12.96) | 16.27 (±12.99) | |
| Milling | Artificial saliva | 1.43 (±0.33) | 1.53 (±0.34) | 1.41 (±0.71) | 1.48 (±0.74) |
| Tea | 3.83 (±1.33) | 3.85 (±1.27) | 7.80 (±1.78) | 7.61 (±1.89) | |
| Coffee | 3.95 (±1.02) | 3.62 (±0.73) | 5.42 (±0.71) | 5.33 (±0.58) | |
| Total | 3.07 (±0.52) | 3.00 (±1.36) | 4.88 (±2.90) | 4.81 (±2.82) | |
| Total | Artificial saliva | 1.03 (±0.5) | 1.08 (±0.54) | 1.28 (±0.55) | 1.41 (±0.55) |
| Tea | 6.72 (±3.11) | 6.60 (±2.99) | 11.31 (±3.82) | 11.20 (±3.94) | |
| Coffee | 11.80 (±8.04) | 11.64 (±8.18) | 18.95 (±13.73) | 19.01 (±13.89) | |
| Total | 6.52 (±6.63) | 6.44 (±6.61) | 10.51 (±10.93) | 10.54 (±10.99) | |
| Source—Background | Type III Sum of Squares | df | Mean Square | F | Sig | |
|---|---|---|---|---|---|---|
| 12 days | Fabrication * Stain—Black | 1378.51 | 2 | 689.25 | 786.23 | <0.001 |
| Fabrication * Stain—White | 1462.95 | 2 | 731.48 | 1022.98 | <0.001 | |
| 24 days | Fabrication * Stain—Black | 3998.87 | 2 | 1999.44 | 1809.49 | <0.001 |
| Fabrication * Stain—White | 4052.27 | 2 | 2026.13 | 1524.09 | <0.001 |
| Fabrication | Stain | Treatment | Mean ∆E00 (±SD) |
|---|---|---|---|
| 3D-Printing | Artificial saliva | Bleaching | 1.46 (±0.27) |
| Polishing | 1.19 (±0.56) | ||
| Total | 1.33 (±0.45) | ||
| Tea | Bleaching | 8.53 (±0.56) | |
| Polishing | 5.17 (±0.76) | ||
| Total | 6.85 (±1.84) | ||
| Coffee | Bleaching | 13.67 (±1.10) | |
| Polishing | 4.25 (±1.08) | ||
| Total | 8.96 (±4.95) | ||
| Total | Bleaching | 7.89 (±5.14) | |
| Polishing | 3.53 (±1.90) | ||
| Total | 5.71 (±4.42) | ||
| Milling | Artificial saliva | Bleaching | 1.60 (±0.65) |
| Polishing | 1.63 (±0.80) | ||
| Total | 1.62 (±0.71) | ||
| Tea | Bleaching | 5.37 (±1.79) | |
| Polishing | 3.69 (±1.50) | ||
| Total | 4.53 (±1.82) | ||
| Coffee | Bleaching | 3.00 (±0.50) | |
| Polishing | 3.33 (±0.74) | ||
| Total | 3.17 (±0.64) | ||
| Total | Bleaching | 3.33 (±1.93) | |
| Polishing | 2.88 (±1.38) | ||
| Total | 3.11 (±1.67) | ||
| Total | Artificial saliva | Bleaching | 1.53 (±0.49) |
| Polishing | 1.41 (±0.71) | ||
| Total | 1.47 (±0.60) | ||
| Tea | Bleaching | 6.95 (±2.07) | |
| Polishing | 4.43 (±1.38) | ||
| Total | 5.69 (±2.16) | ||
| Coffee | Bleaching | 8.33 (±5.53) | |
| Polishing | 3.79 (±1.02) | ||
| Total | 6.06 (±4.55) | ||
| Total | Bleaching | 5.61 (±4.48) | |
| Polishing | 3.21 (±1.68) | ||
| Total | 4.41 (±3.58) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alharbi, N.; Alharbi, A.; Osman, R. Stain Susceptibility of 3D-Printed Nanohybrid Composite Restorative Material and the Efficacy of Different Stain Removal Techniques: An In Vitro Study. Materials 2021, 14, 5621. https://doi.org/10.3390/ma14195621
Alharbi N, Alharbi A, Osman R. Stain Susceptibility of 3D-Printed Nanohybrid Composite Restorative Material and the Efficacy of Different Stain Removal Techniques: An In Vitro Study. Materials. 2021; 14(19):5621. https://doi.org/10.3390/ma14195621
Chicago/Turabian StyleAlharbi, Nawal, Amal Alharbi, and Reham Osman. 2021. "Stain Susceptibility of 3D-Printed Nanohybrid Composite Restorative Material and the Efficacy of Different Stain Removal Techniques: An In Vitro Study" Materials 14, no. 19: 5621. https://doi.org/10.3390/ma14195621
APA StyleAlharbi, N., Alharbi, A., & Osman, R. (2021). Stain Susceptibility of 3D-Printed Nanohybrid Composite Restorative Material and the Efficacy of Different Stain Removal Techniques: An In Vitro Study. Materials, 14(19), 5621. https://doi.org/10.3390/ma14195621






