Repair Bond Strength of Conventionally and Digitally Fabricated Denture Base Resins to Auto-Polymerized Acrylic Resin: Surface Treatment Effects In Vitro
Abstract
1. Introduction
2. Materials and Methods
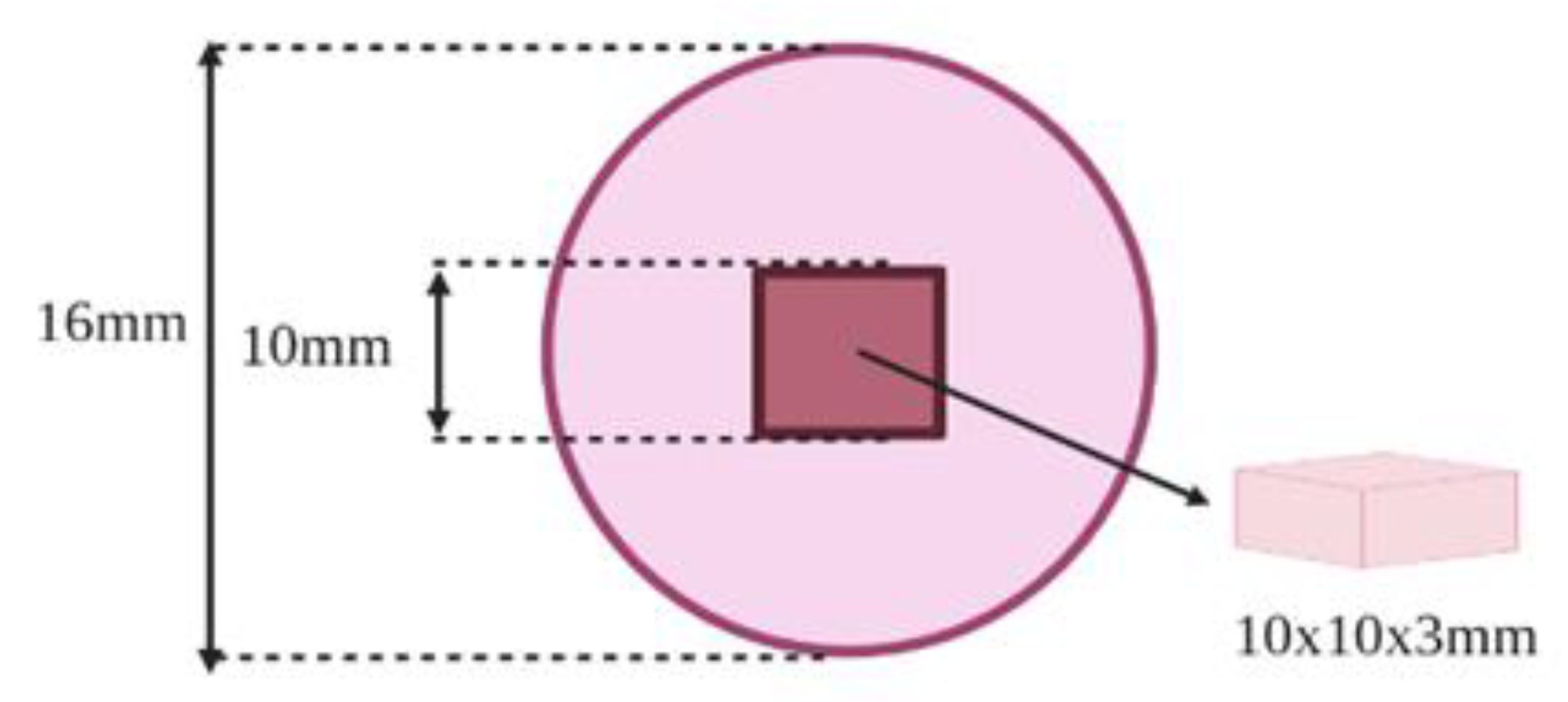
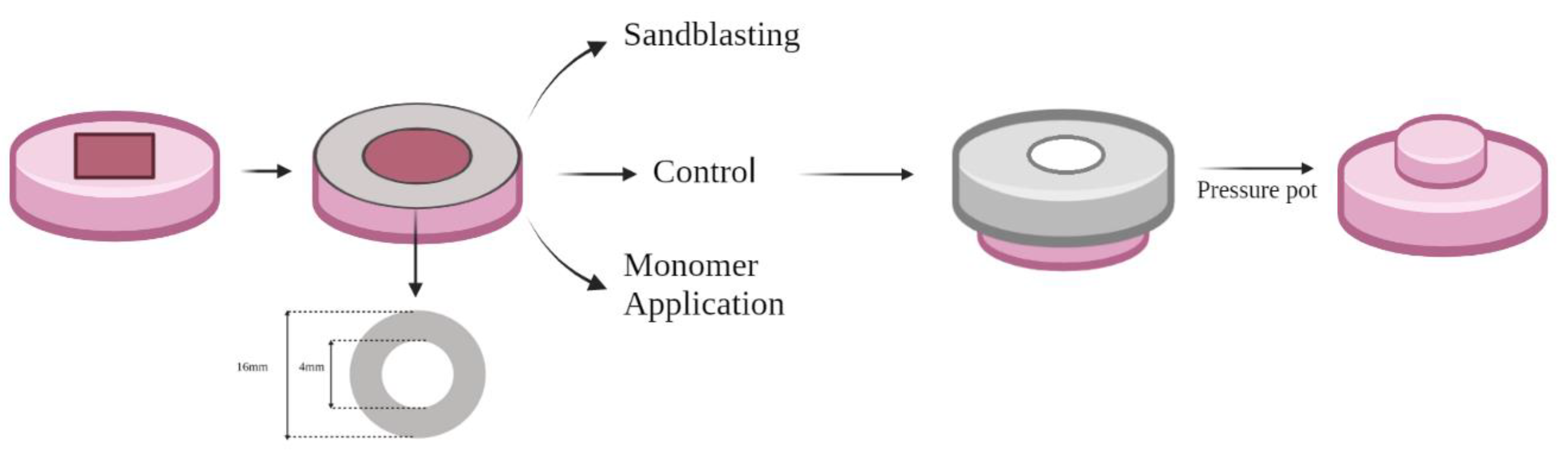
2.1. Specimens Preparation
2.2. Surface Treatment
2.3. Repair Procedures
2.4. SBS Testing
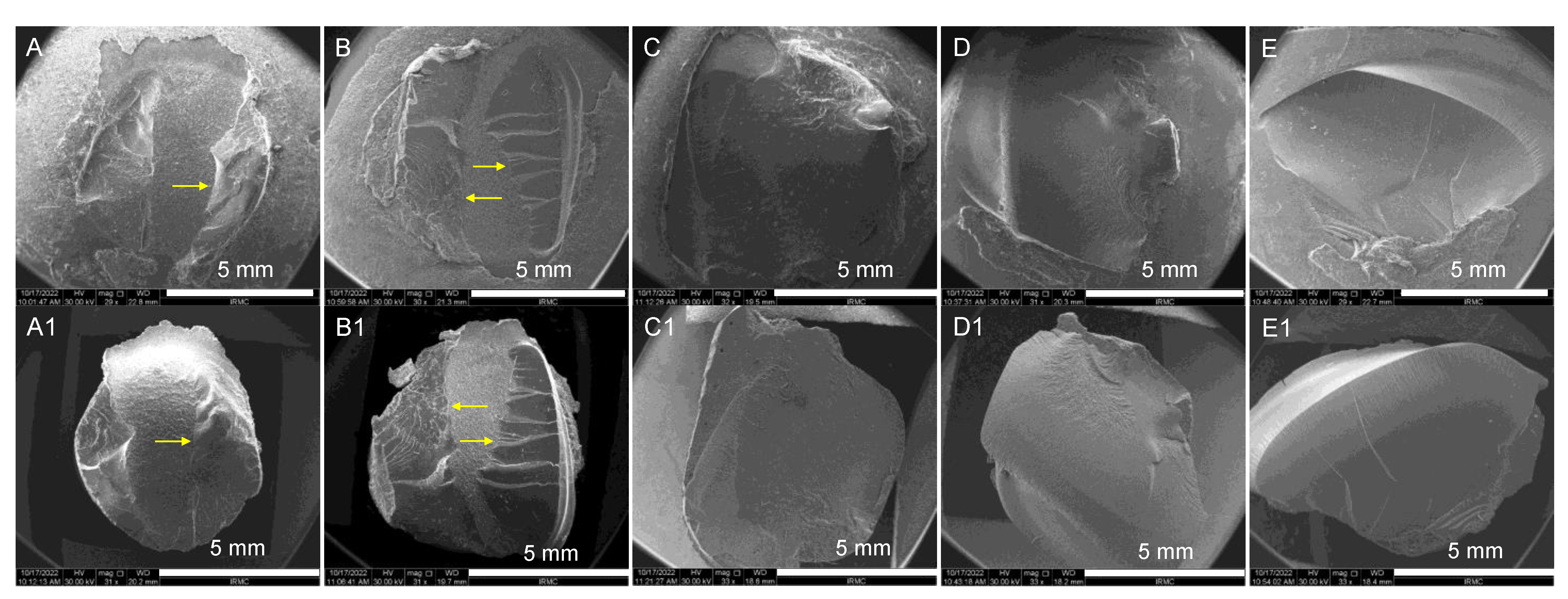
2.5. Scanning Electron Microscope (SEM) Analysis
2.6. Statistical Analysis
3. Results
Nature of Failure
4. Discussion
5. Conclusions
- Heat-polymerized and CAD-CAM milled resin showed high repair bond strength compared with 3D-printed resins.
- MMA and SB surface treatments increased repair bond strength between repair resins and conventional and CAD-CAM milled denture base resins.
- SB surface treatment of 3D-printed resins increased the SBS between repair resins and 3D-printed resins.
- There was a positive effect of the SB surface treatment on the investigated resins, making it a suitable surface treatment method for clinical application.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Goodacre, B.J.; Goodacre, C.J.; Baba, N.Z.; Kattadiyil, M.T. Comparison of denture base adaptation between CAD-CAM and conventional fabrication techniques. J. Prosthet. Dent. 2016, 116, 249–256. [Google Scholar] [CrossRef]
- Perea-Lowery, L.; Minja, I.K.; Lassila, L.; Ramakrishnaiah, R.; Vallittu, P.K. Assessment of CAD-CAM polymers for digitally fabricated complete dentures. J. Prosthet. Dent. 2021, 125, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, M.; Kalberer, N.; Kamnoedboon, P.; Mekki, M.; Durual, S.; Özcan, M.; Müller, F. CAD-CAM complete denture resins: An evaluation of biocompatibility, mechanical properties, and surface characteristics. J. Dent. 2021, 114, 103785. [Google Scholar] [CrossRef] [PubMed]
- Wimmer, T.; Eichberger, M.; Lümkemann, N.; Stawarczyk, B. Accuracy of digitally fabricated trial dentures. J. Prosthet. Dent. 2018, 119, 942–947. [Google Scholar] [CrossRef]
- Revilla-Leon, M.; Ozcan, M. Additive manufacturing technologies used for processing polymers: Current status and potential application in prosthetic dentistry. J. Prosthet. 2019, 28, 146–158. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira Limírio, J.P.J.; de Gomes, J.M.L.; Alves Rezende, M.C.R.; Lemos, C.A.A.; Rosa, C.D.D.R.D.; Pellizzer, E.P. Mechanical properties of polymethyl methacrylate as a denture base: Conventional versus CAD-CAM resin—A systematic review and meta-analysis of in vitro studies. J. Prosthet. Dent. 2021, 128, 1221–1229. [Google Scholar] [CrossRef]
- Helal, M.A.; Abdelrahim, R.A.; Zeidan, A.A.E. Comparison of Dimensional Changes between CAD-CAM Milled Complete Denture Bases and 3D Printed Complete Denture Bases: An in vitro Study. J. Prosthodont. 2022; online ahead of print. [Google Scholar] [CrossRef]
- Chen, S.G.; Yang, J.; Jia, Y.-G.; Lu, B.; Ren, L. TiO2 and PEEK Reinforced 3D Printing PMMA Composite Resin for Dental Denture Base Applications. Nanomaterials 2019, 9, 1049. [Google Scholar] [CrossRef]
- Wang, C.; Shi, Y.F.; Xie, P.J.; Wu, J.H. Accuracy of digital complete dentures: A systematic review of in vitro studies. J. Prosthet. Dent. 2020, 125, 249–256. [Google Scholar] [CrossRef]
- Alaseef, N.; Albasarah, S.; Al Abdulghani, H.; Al-Harbi, F.A.; Gad, M.M.; Akhtar, S.; Khan, S.Q.; Ateeq, I.S.; Al-Qarni, F.D. CAD-CAM Fabricated Denture Base Resins: In Vitro Investigation of the Minimum Acceptable Denture Base Thickness. J. Prosthodont. 2022; online ahead of print. [Google Scholar] [CrossRef]
- Mann, R.S.; Ruse, N.D. Fracture toughness of conventional, milled and 3D printed denture bases. Dent. Mater. 2022, 38, 1443–1451. [Google Scholar] [CrossRef] [PubMed]
- Kumari, R.; Bala, S. Assessment of Cases of Complete Denture Fracture. J. Pharm. Bioallied. Sci. 2021, 13, S1558–S1560. [Google Scholar]
- Gad, M.M.; Rahoma, A.; Khan, Z.A.; Al-Thobity, A.M.; Abualsaud, R.; Alkaltham, N.; Akhtar, S.; Ateeq, I.S.; Al-Harbi, F.A. Closed Repair Technique: Innovative Surface Design for Polymethylmethacrylate Denture Base Repair. J. Prosthodont. 2021, 31, 257–265. [Google Scholar] [CrossRef]
- Alkurt, M.; Yeşil Duymuş, Z.; Gundogdu, M. Effect of repair resin type and surface treatment on the repair strength of heat-polymerized denture base resin. J. Prosthet. Dent. 2014, 111, 71–78. [Google Scholar] [CrossRef]
- Qaw, M.S.; Abushowmi, T.H.; Almaskin, D.F.; AlZaher, Z.A.; Gad, M.M.; Al-Harbi, F.A.; Abualsaud, R.; Ammar, M.M. A novel approach to improve repair bond strength of repaired acrylic resin: An in vitro study on the shear bond strength. J. Prosthodont. 2018, 29, 323–333. [Google Scholar] [CrossRef]
- Seó, R.S.; Neppelenbroek, K.H.; Filho, J.N. Factors affecting the strength of denture repairs. J. Prosthodont. 2007, 16, 302–310. [Google Scholar] [CrossRef]
- Barbosa, D.B.; Monteiro, D.R.; Barao, V.A.R.; Pero, A.C.; Compagnoni, M.A. Effect of monomer treatment and polymerization methods on the bond strength of resin teeth to denture base material. Gerodontology 2009, 26, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Sarac, Y.S.; Sarac, D.; Kulunk, T.; Kulunk, S. The effect of chemical surface treatments of different denture base resins on the shear bond strength of denture repair. J. Prosthet. Dent. 2005, 94, 259–266. [Google Scholar] [CrossRef] [PubMed]
- AlZaher, Z.A.; Almaskin, D.F.; Qaw, M.S.; Abu Showmi, T.H.; Abualsaud, R.; Akhtar, S.; Gad, M.M. Chemo-Mechanical Approach to Improve Repair Bond Strength of Denture Teeth. Int. J. Dent. 2020, 2020, 8870361. [Google Scholar] [CrossRef] [PubMed]
- Li, P.; Krämer-Fernandez, P.; Klink, A.; Xu, Y.; Spintzyk, S. Repairability of a 3D printed denture base polymer: Effects of surface treatment and artificial aging on the shear bond strength. J. Mech. Behav. Biomed. Mater. 2020, 114, 104227. [Google Scholar] [CrossRef]
- Minami, H.; Suzuki, S.; Minesaki, Y.; Kurashige, H.; Tanaka, T. In Vitro evaluation of the influence of repairing condition of denture base resin on the bonding of autopolymerizing resins. J. Prosthet. Dent. 2004, 91, 164–170. [Google Scholar] [CrossRef]
- Cucci, A.L.; Vergani, C.E.; Giampaolo, E.T.; Afonso, M.C. Water sorption, solubility, and bond strength of two autopolymerizing acrylic resins and one heat-polymerizing acrylic resin. J. Prosthet. Dent. 1998, 80, 434–438. [Google Scholar] [CrossRef]
- Taghva, M.; Enteghad, S.; Jamali, A.; Mohaghegh, M. Comparison of shear bond strength of CAD/CAM and conventional heat-polymerized acrylic resin denture bases to auto-polymerized and heat-polymerized acrylic resins after aging. J. Clin. Exp. Dent. 2022, 14, e72–e78. [Google Scholar] [CrossRef] [PubMed]
- Gad, M.M.; Rahoma, A.; Abualsaud, R.; Al-Thobity, A.M.; Fouda, S.M. Effect of Repair Gap Width on the Strength of Denture Repair: An In Vitro Comparative Study. J. Prosthodont. 2019, 28, 684–691. [Google Scholar] [CrossRef] [PubMed]
- Abushowmi, T.H.; AlZaher, Z.A.; Almaskin, D.F.; Qaw, M.S.; Abualsaud, R.; Akhtar, S.; Al-Thobity, A.M.; Al-Harbi, F.A.; Gad, M.M.; Baba, N.Z. Comparative Effect of Glass Fiber and Nano-Filler Addition on Denture Repair Strength. J. Prosthodont. 2019, 29, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Gad, M.M.; Al-Thobity, A.M. The impact of nanoparticles-modified repair resin on denture repairs: A systematic review. Jpn. Dent. Sci. Rev. 2021, 57, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Rached, R.N.; Powers, J.M.; Del Bel Cury, A.A. Repair strength of autopolymerizing, microwave, and conventional heat-polymerized acrylic resins. J. Prosthet. Dent. 2004, 92, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Gad, M.M.; Rahoma, A.; Abualsaud, R.; Al-Thobity, A.M.; Akhtar, S.; Helal, M.A.; Al-Harbi, F.A. Impact of different surface treatments and repair material reinforcement on the flexural strength of repaired PMMA denture base material. Dent. Mater. J. 2020, 39, 471–482. [Google Scholar] [CrossRef]
- Gundogdu, M.; Yanikoglu, N.; Bayindir, F.; Ciftci, H. Effect of repair resin type and surface treatment on the repair strength of polyamide denture base resin. Dent. Mater. J. 2015, 34, 485–489. [Google Scholar] [CrossRef]
- Marra, J.; De Souza, R.F.; Barbosa, D.B.; Pero, A.C.; Compagnoni, M.A. Evaluation of the bond strength of denture base resins to acrylic resin teeth: Effect of thermocycling. J. Prosthodont. 2009, 18, 438–443. [Google Scholar] [CrossRef]
- Shimizu, H.; Kakigi, M.; Fujii, J.; Tsue, F.; Takahashi, Y. Effect of surface preparation using ethyl acetate on the shear bond strength of repair resin to denture base resin. J. Prosthodont. 2008, 17, 451–455. [Google Scholar] [CrossRef]
- Choi, J.J.E.; Uy, C.E.; Plaksina, P.; Ramani, R.S.; Ganjigatti, R.; Waddell, J.N. Bond Strength of denture teeth to heat-cured, CAD/CAM and 3D printed denture acrylics. J. Prosthodont. 2020, 29, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Gad, M.M.; Fouda, S.M.; Abualsaud, R.; Alshahrani, F.A.; Al-Thobity, A.M.; Khan, S.Q.; Akhtar, S.; Ateeq, I.S.; Helal, M.A.; Al-Harbi, F.A. Strength and Surface Properties of a 3D-Printed Denture Base Polymer. Prosthodont 2021, 31, 412–418. [Google Scholar] [CrossRef] [PubMed]
- Freitas, R.F.C.P.; Duarte, S.; Feitosa, S.; Dutra, V.; Lin, W.S.; Panariello, B.H.D.; Carreiro, A.D.F.P. Physical, Mechanical, and Anti-Biofilm Formation Properties of CAD-CAM Milled or 3D Printed Denture Base Resins: In Vitro Analysis. J. Prosthodont. 2022; online ahead of print. [Google Scholar] [CrossRef]
- Neshandar Asli, H.; Rahimabadi, S.; Babaee Hemmati, Y.; Falahchai, M. Effect of different surface treatments on surface roughness and flexural strength of repaired 3D-printed denture base: An in vitro study. J. Prosthet. Dent. 2021, 126, 595.e1–595.e8. [Google Scholar] [CrossRef] [PubMed]
- Zeidan, A.A.E.; Sherif, A.F.; Baraka, Y.; Abualsaud, R.; Abdelrahim, R.A.; Gad, M.M.; Helal, M.A. Evaluation of the Effect of Different Construction Techniques of CAD-CAM Milled, 3D-Printed, and Polyamide Denture Base Resins on Flexural Strength: An in vitro Comparative Study. J. Prosthodont. 2022; online ahead of print. [Google Scholar] [CrossRef]
- Prpic, V.; Schauperl, Z.; Catic, A.; Dulcic, N.; Cimic, S. Comparison of mechanical properties of 3D-Printed, CAD/CAM, and conventional denture base materials. J. Prosthodont. 2020, 29, 524–528. [Google Scholar] [CrossRef] [PubMed]
- Alifui-Segbaya, F.; Bowman, J.; White, A.R.; George, R.; Fidan, I. Characterization of the Double Bond Conversion of Acrylic Resins for 3D Printing of Dental Prostheses. Compend. Contin. Educ. Dent. 2019, 40, e7–e11. [Google Scholar]
- Jeong, K.-W.; Kim, S.-H. Influence of surface treatments and repair materials on the shear bond strength of CAD/CAM provisional restorations. J. Adv. Prosthodont. 2019, 11, 95–104. [Google Scholar] [CrossRef]
- Vallittu, P.K.; Lassila, V.P.; Lappalainen, R. Wetting the repair surface with methyl methacrylate affects the transverse strength of repaired heat-polymerized resin. J. Prosthet. Dent. 1994, 72, 639–643. [Google Scholar] [CrossRef]
- Palitsch, A.; Hannig, M.; Ferger, P.; Balkenhol, M. Bonding of acrylic denture teeth to MMA/PMMA and light-curing denture base materials: The role of conditioning liquids. J. Dent. 2012, 40, 210–221. [Google Scholar] [CrossRef]
- Guzman, A.; Moore, B.K. Influence of surface treatment on bond strength between a heat-activated and a light-activated resin composite. Int. J. Prosthodont. 1995, 8, 179–186. [Google Scholar]
- Lim, N.K.; Shin, S.Y. Bonding of conventional provisional resin to 3D printed resin: The role of surface treatments and type of repair resins. J. Adv. Prosthodont. 2020, 12, 322–328. [Google Scholar] [CrossRef]
- Ng, E.; Tan, L.; Chew, B.; Thean, H. Shear bond strength of microwaveable acrylic resin for denture repair. J. Oral Rehabil. 2004, 31, 798–802. [Google Scholar] [CrossRef]
- Memarian, M.; Shayestehmajd, M. The effect of chemical and mechanical treatment of the denture base resin surface on the shear bond strength of denture repairs. Arch. Oral Res. 2009. [Google Scholar] [CrossRef]
- Stipho, H.D.; Talic, Y.F. Repair of denture base resins with visible lightpolymerized reline material: Effect on tensile and shear bond strengths. J. Prosthet. Dent. 2001, 86, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Alzaid, M.; AlToraibily, F.; Al-Qarni, F.D.; Al-Thobity, A.M.; Akhtar, S.; Ali, S.; Al-Harbi, F.A.; Gad, M.M. The Effect of Salivary pH on the Flexural Strength and Surface Properties of CAD/CAM Denture Base Materials. Eur. J. Dent. 2022; online ahead of print. [Google Scholar] [CrossRef]
| Materials | Brand Name | Composition | Specimens’ Fabrication Method |
|---|---|---|---|
| Heat-polymerized acrylic resin (HP) | Major Base.20 (Major Prodotti Dentari Spa, Momcalieri, Italy) | Powder: Polymer (PMMA) þ initiator (benzoyl peroxide [BPO]) (0.5%) þ pigments (salts of cadmium or iron or organic dyes) Liquid: Monomer (MMA) þ cross-linking agent (Ethylene glycol dimethacrylate (EGDMA) 10%) þ inhibitor (hydroquinone) | Conventional heat polymerization method. Polymerization cycle: 90 min in a water bath by heating to 74 °C, then 100 °C for 30 min |
| CAD/CAM Milled (IvoCad) | IvoCad (Ivoclar Vivadent, Schaan, Liechtenstein) | Prepolymerized PMMA discs 50–100% methyl methacrylate 2.5–10% 1,4-butanediol dimethacrylate | Cut from pre-polymerized acrylic disc using diamond saw (Isomet 5000 Linear Precision Saw, Buehler Ltd., Bluff, IL, USA) |
| CAD/CAM Milled (AvaDent) | AvaDent (AvaDent Digital Dental Solutions, Scottsdale, AZ, USA) | Prepolymerized PMMA (PMMA 99.5%, pigments < 1.0%) | |
| 3D-printed (ASIGA) | DentaBASE (ASIGA, Erfurt, Germany) | Ethoxylated bisphenol A dimethacrylate 7,7,9 (or 7,9,9)-trimethyl-4,13-dioxo-3,14-dioxa-5,12-diazahexadecane-1,16-diyl bismethacrylate 2- hydroxyethyl methacrylate silicon dioxide diphenyl (2,4,6-trimethylbenzoyl) phosphine oxide titanium dioxide | 3D-printed specimens Technology: Printer: ASIGA MAX™ Printing layer thickness: 50 µm Printing orientation: 0-degree Post-curing machine: Asiga-Flash Post-curing time/temp.: 20 min/60 °C |
| 3D-printed (NextDent) | Denture 3D+ NextDent B.V., Soesterberg, The Netherlands | Ester-based monomer; Bisacylphosphine oxide (BAPO) phenylbis (2, 4, 6- trimethylbenzoyl)-phosphine oxide (Omnirad 819) | 3D-printed specimens Technology: Printer: NextDent 5100 Printing layer thickness: 50 µm Printing orientation: 0-degree Post-curing machine: LC-D Print Box Post-curing time/temp.: 30 min/60 °C |
| 3D-printed (Formlabs) | Denture Base Resin LP Formlabs Inc., Somerville, MA, USA | 55–75% w/w urethane dimethacrylate, 15–25% w/w methacrylate monomers, and <0.9% w/w phenyl bis(2,4,6-trimethylbenzoyl)-phosphine oxide | 3D-printed specimens Technology: Printer: Form 2 Printing layer thickness: 50 µm Printing orientation: 0-degree Post-curing machine: FormCure Post-curing time/temp.: 30 min/60 °C |
| Materials | Surface Treatments | |||
|---|---|---|---|---|
| Control | MMA | SB | p-Value | |
| HP | 6.67 ± 1.13 a | 10.67 ± 0.87 | 14.54 ± 1.15 | 0.000 * |
| IVOCad | 6.87 ± 0.89 a | 12.19 ± 1.39 a | 16.14 ± 0.95 a | 0.000 * |
| AvaDent | 7.08 ± 1.04 a | 11.84 ± 1.05 a | 16.64 ± 1.58 a | 0.000 * |
| ASIGA | 2.77 ± 0.35 b,A | 3.47 ± 0.99 b,A | 5.81 ± 0.88 b | 0.000 * |
| NextDent | 1.91 ± 0.23 b,A | 2.23 ± 0.35 b,A | 5.85 ± 0.97 b | 0.000 * |
| FormLabs | 2.26 ± 0.32 b,A | 3.81 ± 0.72 b,A | 6.46 ± 0.92 b | 0.000 * |
| p-value | 0.000 * | 0.000 * | 0.000 * | |
| Source | Type III Sum of Squares | df | Mean Square | F-Test | p-Value |
|---|---|---|---|---|---|
| Material | 2608.361 | 5 | 521.672 | 579.472 | 0.000 * |
| Surface treatment | 1201.135 | 2 | 600.567 | 667.109 | 0.000 * |
| Material * Surface treatment | 233.158 | 10 | 23.316 | 25.899 | 0.000 * |
| Error | 145.841 | 162 | 0.900 | ||
| Total | 14,658.535 | 180 |
| Martials | Surface Treatment | Nature of Failure % | ||
|---|---|---|---|---|
| Adhesive | Cohesive | Mixed | ||
| HP | Control | 7(70) | -- | 3(30) |
| MMA | 4(40) | 2(20) | 4(40) | |
| SB | 3(30) | -- | 7(70) | |
| IvoCad | Control | 6(60) | 1(10) | 3(30) |
| MMA | 3(30) | 1(10) | 6(60) | |
| SB | --- | 3(30) | 7(70) | |
| AvaDent | Control | 4(40) | 1(10) | 5(50) |
| MMA | 2(20) | 2(20) | 6(60) | |
| SB | -- | 4(40) | 6(60) | |
| ASIGA | Control | 10(100) | -- | -- |
| MMA | 8(80) | 1(10) | 1(10) | |
| SB | 3(30) | 5(50) | 2(20) | |
| NextDent | Control | 10(100) | -- | -- |
| MMA | 7(70) | 1(10) | 2(20) | |
| SB | 2(20) | 5(5) | 3(30) | |
| FormLabs | Control | 9(90) | -- | 1(10) |
| MMA | 6(60) | - | 4(40) | |
| SB | 3(30) | 5(50) | 2(20) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gad, M.M.; Albazroun, Z.; Aldajani, F.; Elakel, A.M.; El Zayat, M.; Akhtar, S.; Khan, S.Q.; Ali, S.; Rahoma, A.M. Repair Bond Strength of Conventionally and Digitally Fabricated Denture Base Resins to Auto-Polymerized Acrylic Resin: Surface Treatment Effects In Vitro. Materials 2022, 15, 9062. https://doi.org/10.3390/ma15249062
Gad MM, Albazroun Z, Aldajani F, Elakel AM, El Zayat M, Akhtar S, Khan SQ, Ali S, Rahoma AM. Repair Bond Strength of Conventionally and Digitally Fabricated Denture Base Resins to Auto-Polymerized Acrylic Resin: Surface Treatment Effects In Vitro. Materials. 2022; 15(24):9062. https://doi.org/10.3390/ma15249062
Chicago/Turabian StyleGad, Mohammed M., Zainab Albazroun, Fatimah Aldajani, Ahmed M. Elakel, Mai El Zayat, Sultan Akhtar, Soban Q. Khan, Saqib Ali, and Ahmed M. Rahoma. 2022. "Repair Bond Strength of Conventionally and Digitally Fabricated Denture Base Resins to Auto-Polymerized Acrylic Resin: Surface Treatment Effects In Vitro" Materials 15, no. 24: 9062. https://doi.org/10.3390/ma15249062
APA StyleGad, M. M., Albazroun, Z., Aldajani, F., Elakel, A. M., El Zayat, M., Akhtar, S., Khan, S. Q., Ali, S., & Rahoma, A. M. (2022). Repair Bond Strength of Conventionally and Digitally Fabricated Denture Base Resins to Auto-Polymerized Acrylic Resin: Surface Treatment Effects In Vitro. Materials, 15(24), 9062. https://doi.org/10.3390/ma15249062









