Influence of Hydrofluoric and Nitric Acid Pre-Treatment and Type of Adhesive Cement on Retention of Zirconia Crowns
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Della Bona, A.; Pecho, O.E.; Alessandretti, R. Zirconia as a Dental Biomaterial. Materials 2015, 8, 4978–4991. [Google Scholar] [CrossRef] [PubMed]
- Al-Zordk, W.; Saker, S. Impact of sintering procedure and clinical adjustment on color stability and translucency of translucent zirconia. J. Prosthet. Dent. 2020, 124, 788.e1–788.e9. [Google Scholar] [CrossRef] [PubMed]
- Obradovic-Djuricic, K.; Medic, V.; Dodic, S.; Gavrilov, D.; Antonijevic, D.; Zrilic, M. Dilemmas in zirconia bonding: A review. Srp. Arh. Za Celok. Lek. 2013, 141, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Oumlzcan, M.; Bernasconi, M. Adhesion to zirconia used for dental restorations: A systematic review and meta-analysis. J. Adhes. Dent. 2015, 17, 7–26. [Google Scholar]
- Aboushelib, M.N.; Wang, H.; Kleverlaan, C.J.; Feilzer, A.J. Fatigue behavior of zirconia under different loading conditions. Dent. Mater. 2016, 32, 915–920. [Google Scholar] [CrossRef]
- Gargari, M.; Gloria, F.; Napoli, E.; Pujia, A. Zirconia: Cementation of prosthetic restorations. Literature review. Oral Implant. 2011, 3, 25–29. [Google Scholar]
- Maccauro, G.; Iommetti, P.R.; Muratori, F.; Raffaelli, L.; Manicone, P.F.; Fabbriciani, C. An Overview about Biomedical Applications of Micron and Nano Size Tantalum. Recent Pat. Biotechnol. 2009, 3, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Karimipour-Saryazdi, M.; Sadid-Zadeh, R.; Givan, D.; Burgess, J.O.; Ramp, L.C.; Liu, P.-R. Influence of surface treatment of yttrium-stabilized tetragonal zirconium oxides and cement type on crown retention after artificial aging. J. Prosthet. Dent. 2014, 111, 395–403. [Google Scholar] [CrossRef]
- Arai, M.; Takagaki, T.; Takahashi, A.; Tagami, J. The role of functional phosphoric acid ester monomers in the surface treatment of yttria-stabilized tetragonal zirconia polycrystals. Dent. Mater. J. 2017, 36, 190–194. [Google Scholar] [CrossRef]
- Sakrana, A.A.; Özcan, M. Effect of chemical etching solutions versus air abrasion on the adhesion of self-adhesive resin cement to IPS e.max ZirCAD with and without aging. Int. J. Esthet. Dent. 2017, 12, 72–85. [Google Scholar]
- Zhang, Y.; Lawn, B.R.; Rekow, E.D.; Thompson, V.P. Effect of sandblasting on the long-term performance of dental ceramics. J. Biomed. Mater. Res. 2004, 71, 381–386. [Google Scholar] [CrossRef]
- Blatz, M.B.; Phark, J.-H.; Ozer, F.; Mante, F.K.; Saleh, N.; Bergler, M.; Sadan, A. In vitro comparative bond strength of contemporary self-adhesive resin cements to zirconium oxide ceramic with and without air-particle abrasion. Clin. Oral Investig. 2009, 14, 187–192. [Google Scholar] [CrossRef]
- Özcan, M.; Nijhuis, H.; Valandro, L.F. Effect of Various Surface Conditioning Methods on the Adhesion of Dual-cure Resin Cement with MDP Functional Monomer to Zirconia after Thermal Aging. Dent. Mater. J. 2008, 27, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Lawn, B.R.; Malament, K.A.; Van Thompson, P.; Rekow, E.D. Damage accumulation and fatigue life of particle-abraded ceramics. Int. J. Prosthodont. 2007, 19, 442–448. [Google Scholar]
- Zarone, F.; Di Mauro, M.I.; Ausiello, P.; Ruggiero, G.; Sorrentino, R. Current status on lithium disilicate and zirconia: A narrative review. BMC Oral Heal. 2019, 19, 134. [Google Scholar] [CrossRef] [PubMed]
- Lohbauer, U.; Zipperle, M.; Rischka, K.; Petschelt, A.; Müller, F.A. Hydroxylation of dental zirconia surfaces: Characterization and bonding potential. J. Biomed. Mater. Res. Part. B Appl. Biomater. 2008, 87, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Feitosa, S.A.; Lima, N.B.; Yoshito, W.K.; Campos, F.; Bottino, M.A.; Valandro, L.F. Bonding strategies to full-contour zirconia: Zirconia pretreatment with piranha solution, glaze and airborne-particle abrasion. Int. J. Adhes. 2017, 77, 151–156. [Google Scholar] [CrossRef]
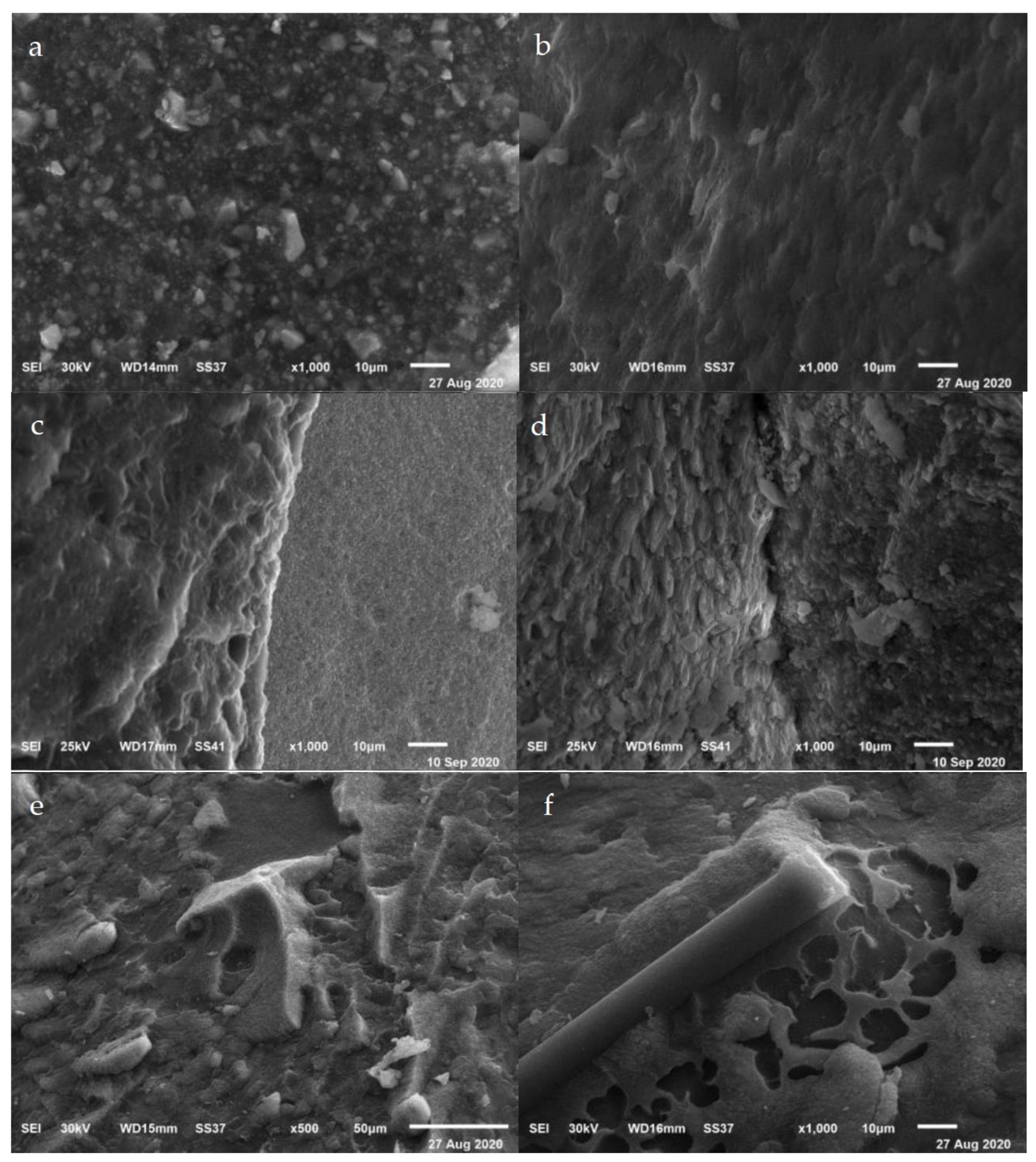
- Casucci, A.; Osorio, E.; Osorio, R.; Monticelli, F.; Toledano, M.; Mazzitelli, C.; Ferrari, M. Influence of different surface treatments on surface zirconia frameworks. J. Dent. 2009, 37, 891–897. [Google Scholar] [CrossRef]
- Casucci, A.; Mazzitelli, C.; Monticelli, F.; Toledano, M.; Osorio, R.; Osorio, E.; Papacchini, F.; Ferrari, M. Morphological analysis of three zirconium oxide ceramics: Effect of surface treatments. Dent. Mater. 2010, 26, 751–760. [Google Scholar] [CrossRef]
- Guazzato, M.; Quach, L.; Albakry, M.; Swain, M.V. Influence of surface and heat treatments on the flexural strength of Y-TZP dental ceramic. J. Dent. 2005, 33, 9–18. [Google Scholar] [CrossRef]
- Ersu, B.; Narin, D.; Aktas, G.; Yuzugullu, B.; Canay, S. Effect of preparation taper and height on strength and retention of zirconia crowns. Int. J. Prosthodont. 2012, 25, 582–584. [Google Scholar]
- Yenisey, M.; Dede, D.Ö.; Rona, N. Effect of surface treatments on the bond strength between resin cement and differently sintered zirconium-oxide ceramics. J. Prosthodont. Res. 2016, 60, 36–46. [Google Scholar] [CrossRef]
- Narula, S.; Punia, V.; Khandelwal, M.; Sharma, V.; Pamecha, S. Retention in conventional fixed partial dentures: A review. J. Clin. Diagn. Res. 2011, 5, 1128–1133. [Google Scholar]
- Zidan, O.; Ferguson, G.C. The retention of complete crowns prepared with three different tapers and luted with four different cements. J. Prosthet. Dent. 2003, 89, 565–571. [Google Scholar] [CrossRef]
- Grasel, R.; Santos, M.J.; Rêgo, H.C.; Rippe, M.P.; Valandro, L.F. Effect of Resin Luting Systems and Alumina Particle Air Abrasion on Bond Strength to Zirconia. Oper. Dent. 2018, 43, 282–290. [Google Scholar] [CrossRef] [PubMed]
- Hill, E.E. Dental Cements for Definitive Luting: A Review and Practical Clinical Considerations. Dent. Clin. N. Am. 2007, 51, 643–658. [Google Scholar] [CrossRef]
- De Munck, J.; Van Landuyt, K.; Peumans, M.; Poitevin, A.; Lambrechts, P.; Braem, M.; Van Meerbeek, B. A Critical Review of the Durability of Adhesion to Tooth Tissue: Methods and Results. J. Dent. Res. 2005, 84, 118–132. [Google Scholar] [CrossRef]
- Aguiar, T.R.; Francescantonio, M.D.; Arrais, C.A.G.; Ambrosano, G.M.B.; DaVanzo, C.; Giannini, M. Influence of Curing Mode and Time on Degree of Conversion of One Conventional and Two Self-adhesive Resin Cements. Oper. Dent. 2010, 35, 295–299. [Google Scholar] [CrossRef]
- Migliau, G. Classification review of dental adhesive systems: From the IV generation to the universal type. Ann. Stomatol. 2017, 8, 1–17. [Google Scholar] [CrossRef]
- Higashi, M.; Matsumoto, M.; Kawaguchi, A.; Miura, J.; Minamino, T.; Kabetani, T.; Takeshige, F.; Mine, A.; Yatani, H. Bonding effectiveness of self-adhesive and conventional-type adhesive resin cements to CAD/CAM resin blocks. Part 1: Effects of sandblasting and silanization. Dent. Mater. J. 2016, 35, 21–28. [Google Scholar] [CrossRef]
- Monticelli, F.; Osorio, R.; Mazzitelli, C.; Ferrari, M.; Toledano, M. Limited Decalcification/Diffusion of Self-adhesive Cements into Dentin. J. Dent. Res. 2008, 87, 974–979. [Google Scholar] [CrossRef] [PubMed]
- Han, L.; Okamoto, A.; Fukushima, M.; Okiji, T. Evaluation of physical properties and surface degradation of self-adhesive resin cements. Dent. Mater. J. 2007, 26, 906–914. [Google Scholar] [CrossRef]
- Quigley, N.P.; Loo, D.S.; Choy, C.; Ha, W.N. Clinical efficacy of methods for bonding to zirconia: A systematic review. J. Prosthet. Dent. 2021, 125, 231–240. [Google Scholar] [CrossRef] [PubMed]
- May, L.G.; Passos, S.P.; Capelli, D.B.; Özcan, M.; Bottino, M.A.; Valandro, L.F. Effect of silica coating combined to a MDP-based primer on the resin bond to Y-TZP ceramic. J. Biomed. Mater. Res. Part. B Appl. Biomater. 2010, 95, 69–74. [Google Scholar] [CrossRef]
- Sakrana, A.A.; Al-Zordk, W.; Shoukry, H.; Özcan, M. Bond Strength Durability of Adhesive Cements to Translucent Zirconia: Effect of Surface Conditioning. Eur J. Prosthodont Restor. Dent. 2020, 28, 161–171. [Google Scholar]
- Burgess, J.O.; Ghuman, T.; Cakir, D.; Swift, J., Jr. Self-adhesive resin cements. J. Esthet. Restor. Dent. 2010, 22, 412–419. [Google Scholar] [CrossRef]
- Tanış, M.Ç.; Akçaboy, T.C. Effects of Different Surface Treatment Methods and MDP Monomer on Resin Cementation of Zirconia Ceramics an In Vitro Study. J. Lasers Med. Sci. 2015, 6, 174–181. [Google Scholar] [CrossRef]
- Lepe, X.; Streiff, K.R.; Johnson, G.H. Long-term retention of zirconia crowns cemented with current automixed cements. J. Prosthet. Dent. 2020, 12, 0022. [Google Scholar] [CrossRef]
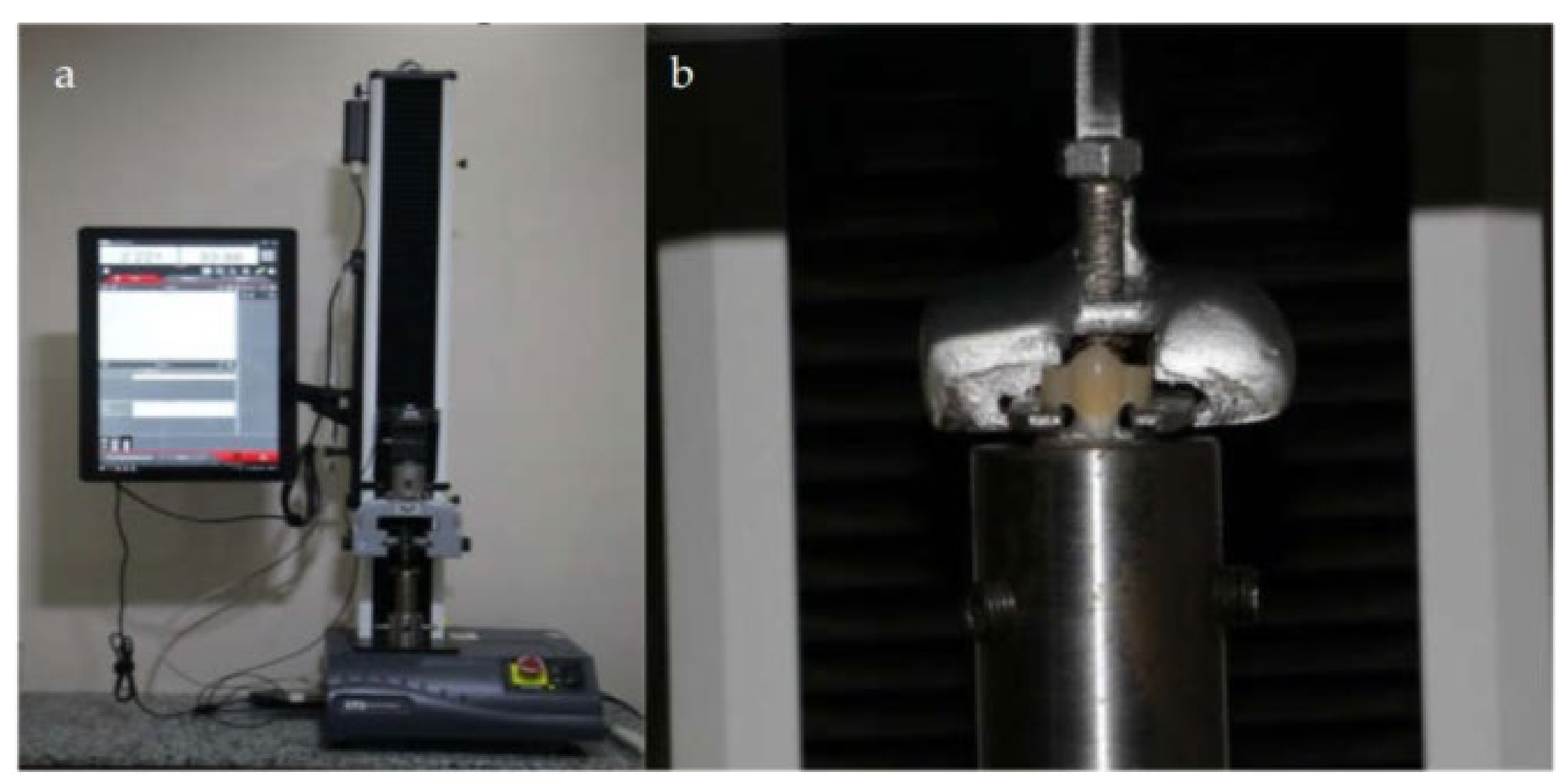
- Heintze, S. Crown pull-off test (crown retention test) to evaluate the bonding effectiveness of luting agents. Dent. Mater. 2010, 26, 193–206. [Google Scholar] [CrossRef] [PubMed]
- Colombo, M.; Gallo, S.; Padovan, S.; Chiesa, M.; Poggio, C.; Scribante, A. Influence of Different Surface Pretreatments on Shear Bond Strength of an Adhesive Resin Cement to Various Zirconia Ceramics. Materials 2020, 13, 652. [Google Scholar] [CrossRef]
- Ali, A.O.; Kelly, J.R.; Zandparsa, R. The Influence of Different Convergence Angles and Resin Cements on the Retention of Zirconia Copings. J. Prosthodont. 2012, 21, 614–621. [Google Scholar] [CrossRef]
- Aleisa, K.; Alwazzan, K.; Al-Dwairi, Z.N.; AlMoharib, H.; Alshabib, A.; Aleid, A.; Lynch, E. Retention of zirconium oxide copings using different types of luting agents. J. Dent. Sci. 2013, 8, 392–398. [Google Scholar] [CrossRef]
- Monteiro, R.V.; Dos Santos, D.M.; Bernardon, J.K.; De Souza, G.M. Effect of surface treatment on the retention of zirconia crowns to tooth structure after aging. J. Esthet. Restor. Dent. 2020, 32, 699–706. [Google Scholar] [CrossRef]
- Estevan, L.F.; Martínez, D.M.; Font, A.F.; Panadero, R.A.; Rodríguez, J.L.R. Methodology in specimen fabrication for in vitro dental studies: Standardization of extracted tooth preparation. J. Clin. Exp. Dent. 2017, 9, e897–e900. [Google Scholar] [CrossRef][Green Version]
- Kasem, A.T.; Sakrana, A.A.; Ellayeh, M.; Özcan, M. Evaluation of zirconia and zirconia-reinforced glass ceramic systems fabricated for minimal invasive preparations using a novel standardization method. J. Esthet. Restor. Dent. 2020, 32, 560–568. [Google Scholar] [CrossRef]
- Liu, D.; Tsoi, J.K.-H.; Matinlinna, J.P.; Wong, H.M. Effects of some chemical surface modifications on resin zirconia adhesion. J. Mech. Behav. Biomed. Mater. 2015, 46, 23–30. [Google Scholar] [CrossRef]
- Bergamo, E.T.; Bordin, D.; Ramalho, I.S.; Lopes, A.C.; Gomes, R.S.; Kaizer, M.; Witek, L.; Bonfante, E.A.; Coelho, P.G.; Cury, A.A.D.B. Zirconia-reinforced lithium silicate crowns: Effect of thickness on survival and failure mode. Dent. Mater. 2019, 35, 1007–1016. [Google Scholar] [CrossRef] [PubMed]
- Ehlers, V.; Kampf, G.; Stender, E.; Willershausen, B.; Ernst, C.-P. Effect of thermocycling with or without 1 year of water storage on retentive strengths of luting cements for zirconia crowns. J. Prosthet. Dent. 2015, 113, 609–615. [Google Scholar] [CrossRef] [PubMed]
- Shahin, R.; Kern, M. Effect of air-abrasion on the retention of zirconia ceramic crowns luted with different cements before and after artificial aging. Dent. Mater. 2010, 26, 922–928. [Google Scholar] [CrossRef] [PubMed]
- Pilo, R.; Folkman, M.; Arieli, A.; Levartovsky, S. Marginal Fit and Retention Strength of Zirconia Crowns Cemented by Self-adhesive Resin Cements. Oper. Dent. 2018, 43, 151–161. [Google Scholar] [CrossRef]
| Code | Group |
|---|---|
| AP | The crowns were air abraded using aluminum oxide particles and cemented by Panavia SA Cement Plus |
| AL | The crowns were air abraded using aluminum oxide particles and cemented by GC LinkForce Cement |
| AHP | The crowns were air abraded using aluminum oxide particles, etched using the hot acid, and cemented by Panavia SA |
| AHP | The crowns were air abraded using aluminum oxide particles, etched with the hot acid, and cemented by Panavia SA |
| Group | Retention Force (N) | Surface Area (mm2) | Retention Strength (Mpa) |
|---|---|---|---|
| AHP | 422.54 ± 88.71 | 109.85 ± 9.24 | 3.83 ± 0.71 |
| AHL | 233.03 ± 54.28 | 114.54 ± 11.48 | 2.00 ± 0.52 |
| AP | 354.95 ± 30.96 | 111.24 ± 9.77 | 3.22 ± 0.35 |
| AL | 163.02 ± 31.57 | 112.36 ± 6.25 | 1.44 ± 0.22 |
| Group | Mean Difference (I-J) | Std. Error Sig. | Sig. | |
|---|---|---|---|---|
| AHP | AHL | 1.829 | 0.218 | 0.000 |
| AP | 0.608 | 0.218 | 0.008 | |
| AL | 2.39 | 0.218 | 0.000 | |
| AHL | AP | −1.221 | 0.218 | 0.000 |
| AL | 0.562 | 0.218 | 0.014 | |
| AP | AL | 1.783 | 0.218 | 0.000 |
| Variable | Sum of Squares | df | Mean | F | p |
|---|---|---|---|---|---|
| Etching | 3.416 | 1 | 3.416 | 14.439 | 0.001 |
| Cement | 32.5981 | 1 | 1 | 137.769 | 0.000 |
| Etching × Cement | 0.005 | 1 | 32.598 | 0.022 | 0.882 |
| Error | 8.518 | 36 | 0.005 | - | - |
| Total | 319.911 | 40 | 0.237 | - | - |
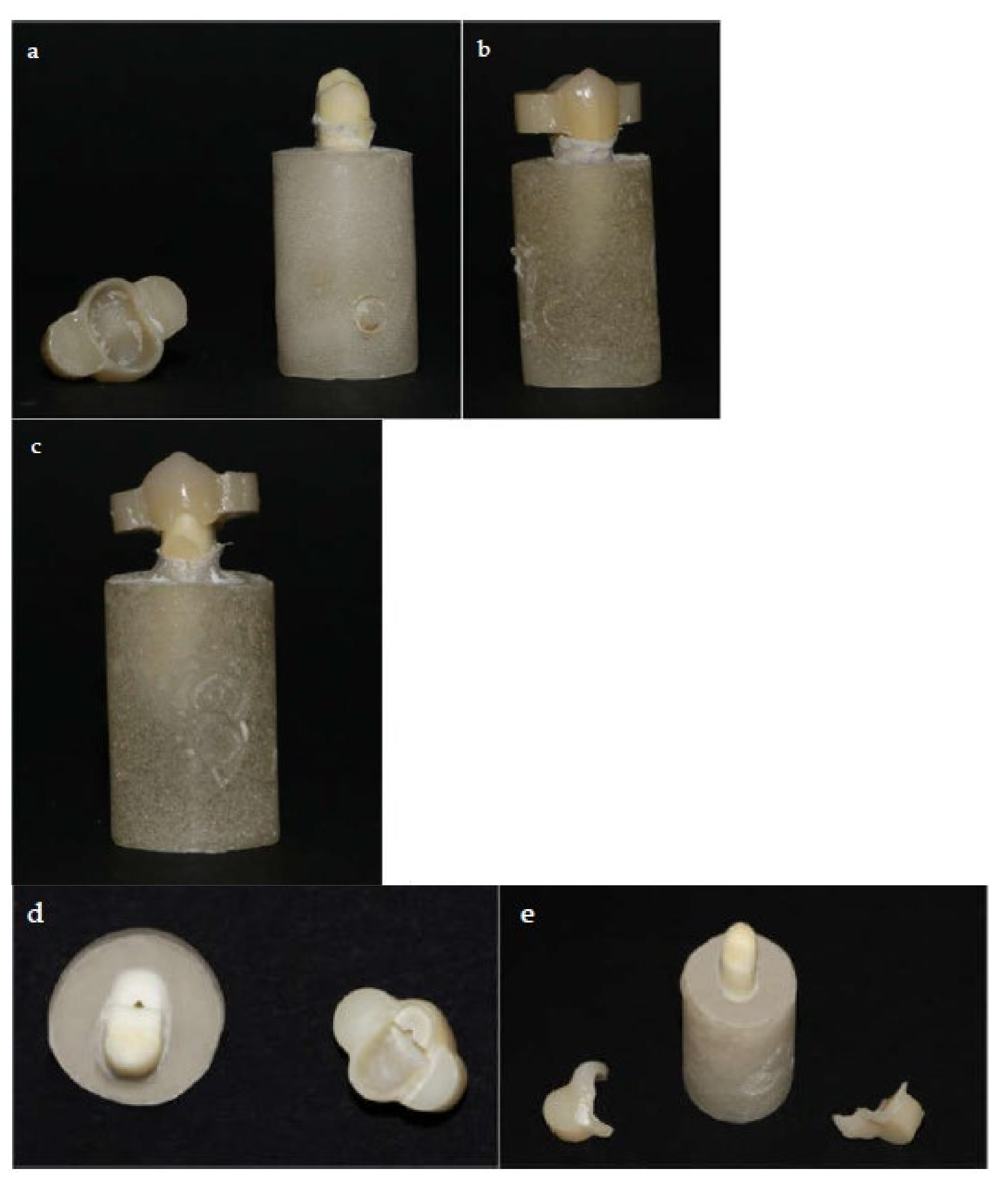
| Group | Adhesive | Cohesive | Mixed |
|---|---|---|---|
| AHP | 2 | 2 | 6 |
| AHL | 5 | 2 | 3 |
| AP | 3 | 1 | 6 |
| AL | 10 | 0 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harb, O.; Al-Zordk, W.; Özcan, M.; Sakrana, A.A. Influence of Hydrofluoric and Nitric Acid Pre-Treatment and Type of Adhesive Cement on Retention of Zirconia Crowns. Materials 2021, 14, 960. https://doi.org/10.3390/ma14040960
Harb O, Al-Zordk W, Özcan M, Sakrana AA. Influence of Hydrofluoric and Nitric Acid Pre-Treatment and Type of Adhesive Cement on Retention of Zirconia Crowns. Materials. 2021; 14(4):960. https://doi.org/10.3390/ma14040960
Chicago/Turabian StyleHarb, Osama, Walid Al-Zordk, Mutlu Özcan, and Amal Abdelsamad Sakrana. 2021. "Influence of Hydrofluoric and Nitric Acid Pre-Treatment and Type of Adhesive Cement on Retention of Zirconia Crowns" Materials 14, no. 4: 960. https://doi.org/10.3390/ma14040960
APA StyleHarb, O., Al-Zordk, W., Özcan, M., & Sakrana, A. A. (2021). Influence of Hydrofluoric and Nitric Acid Pre-Treatment and Type of Adhesive Cement on Retention of Zirconia Crowns. Materials, 14(4), 960. https://doi.org/10.3390/ma14040960







