Effect of Restorative Material on Mechanical Response of Provisional Endocrowns: A 3D—FEA Study
Abstract
1. Introduction
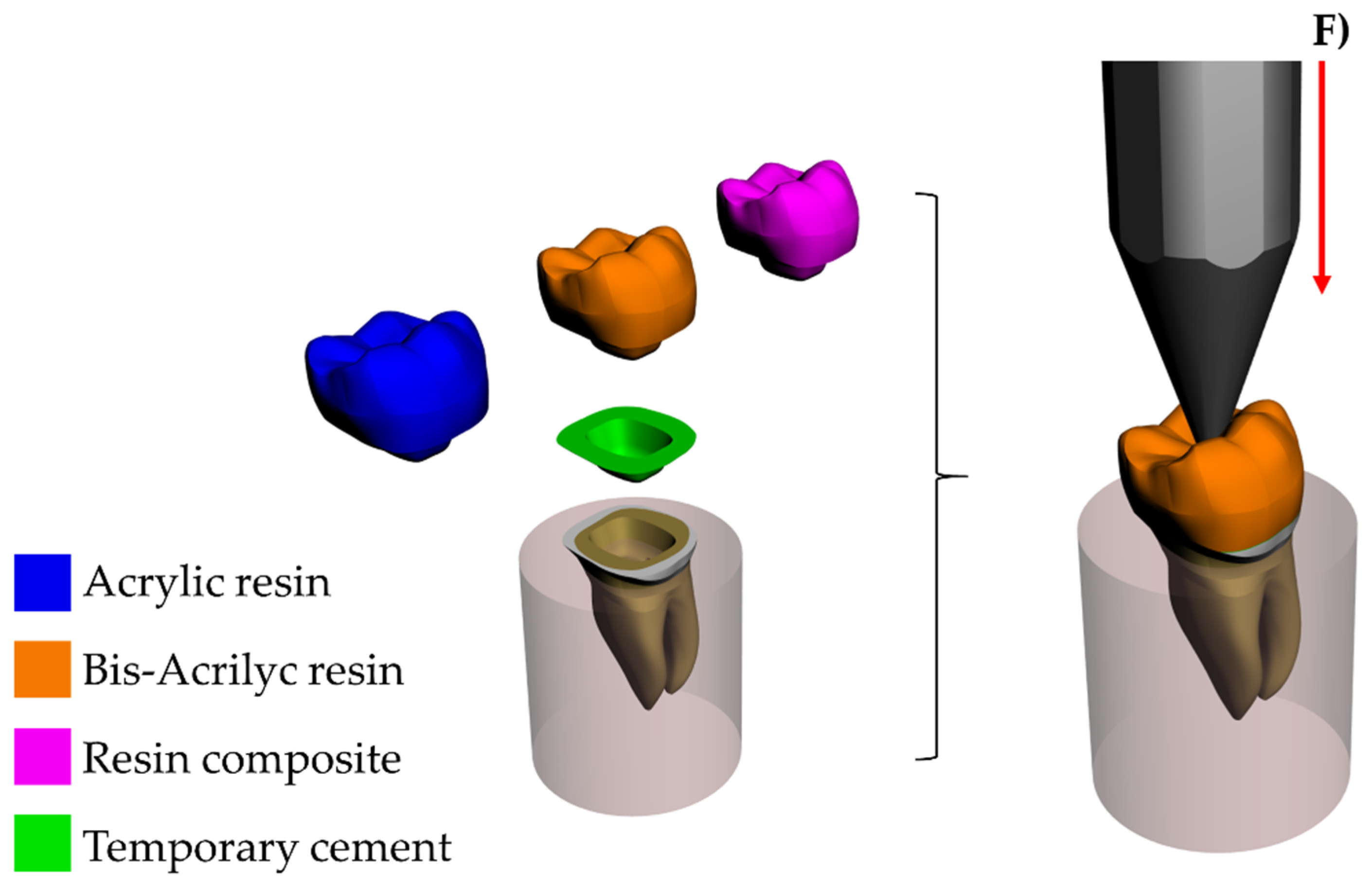
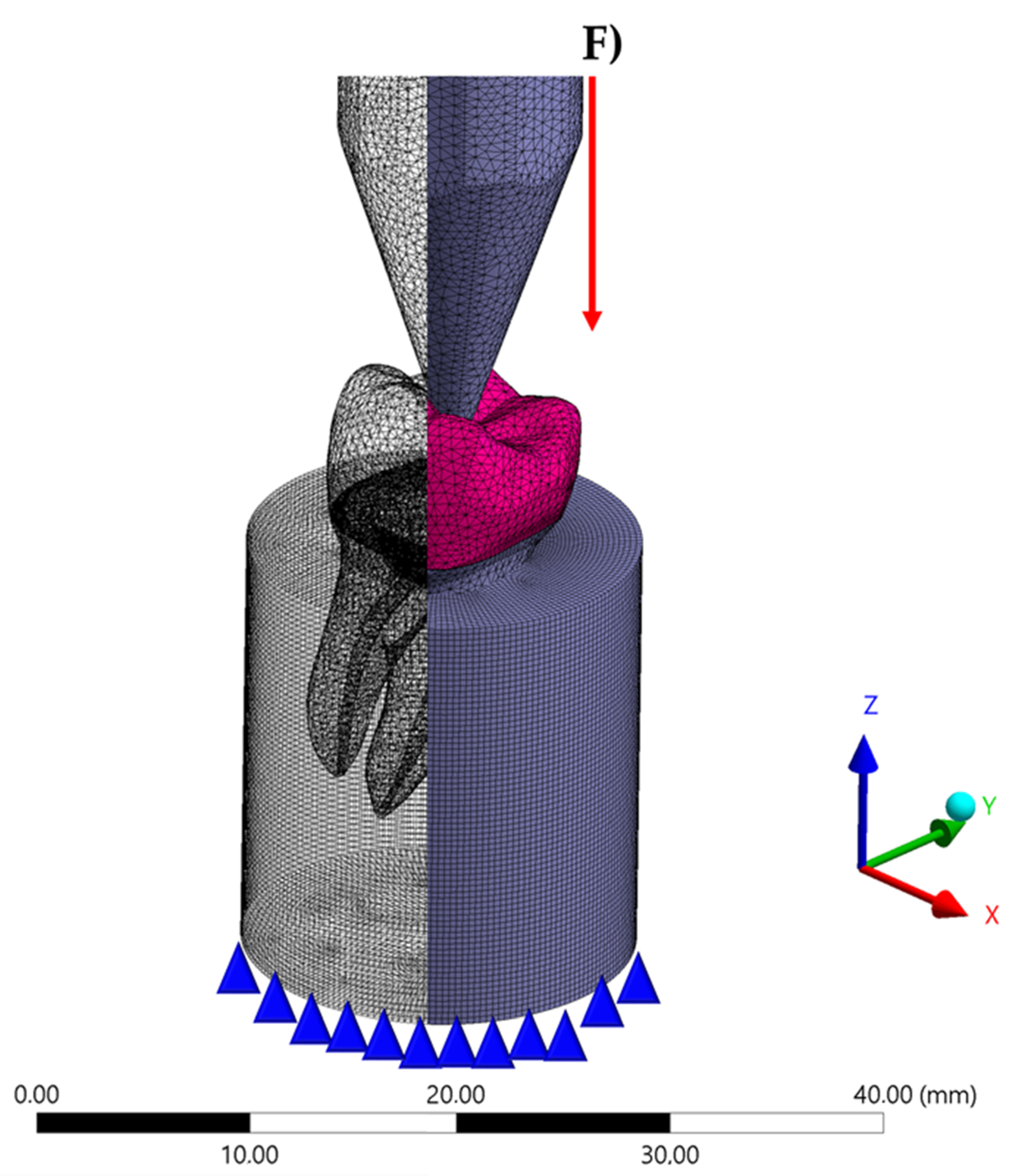
2. Materials and Methods
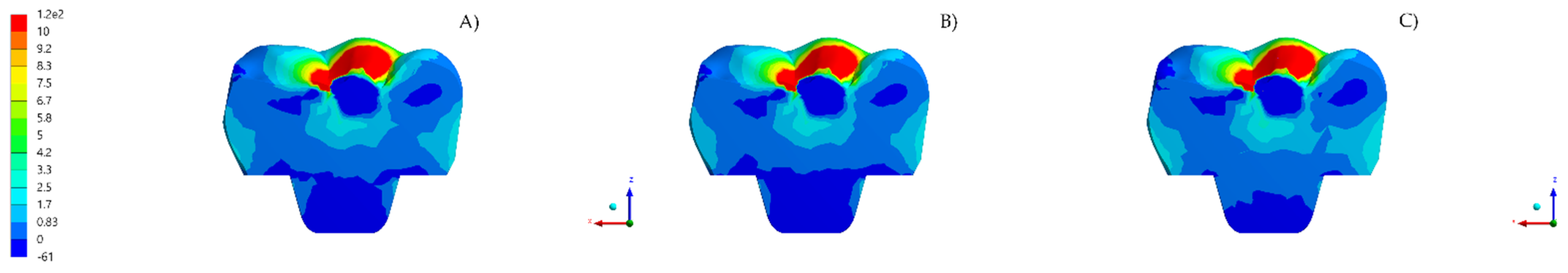
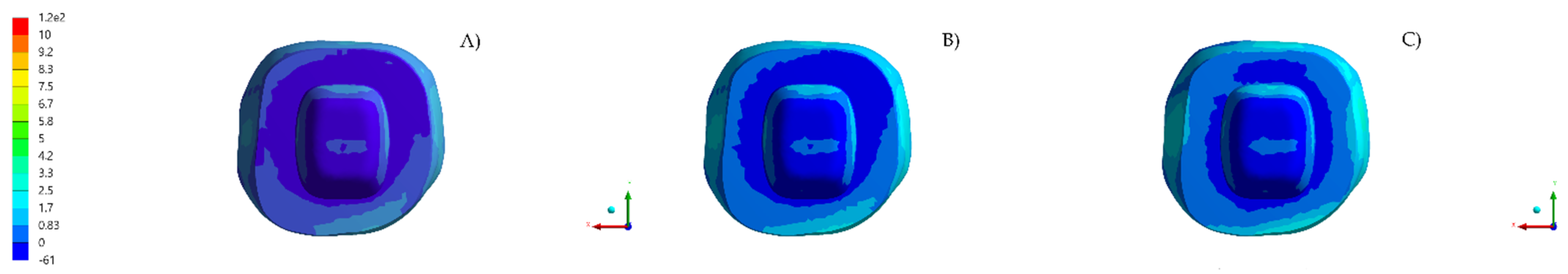
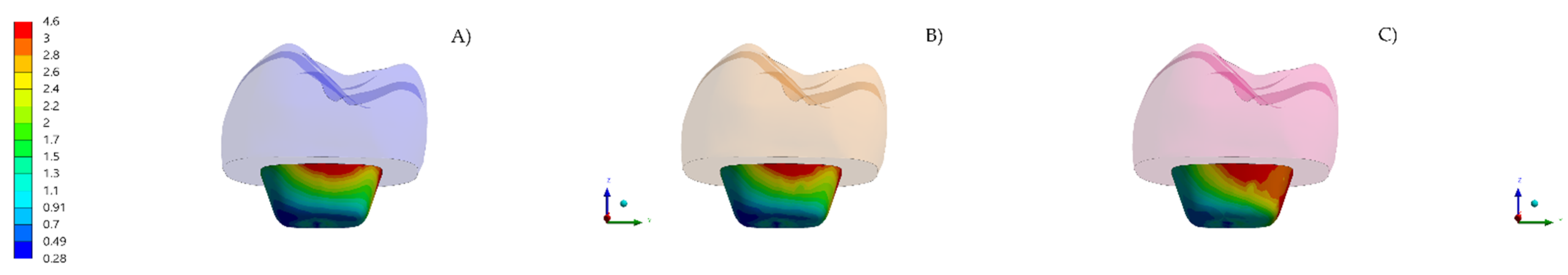
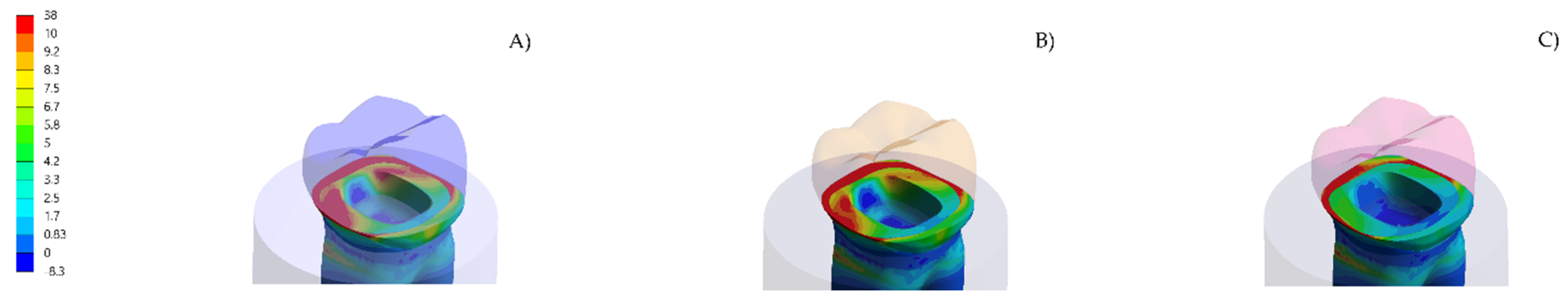
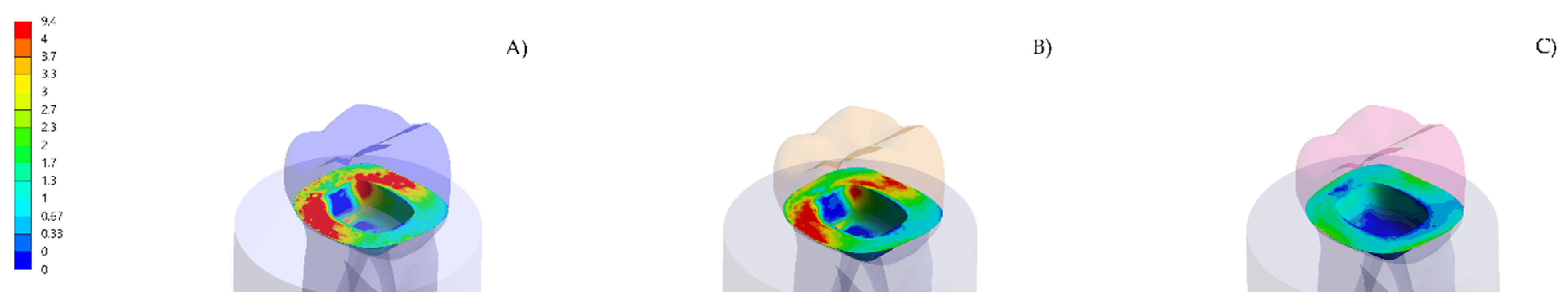
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Balkenhol, M.; Mautner, M.C.; Ferger, P.; Wöstmann, B. Mechanical properties of provisional crown and bridge materials: Chemical-curing versus dual-curing systems. J. Dent. 2008, 36, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Keys, W.F.; Keirby, N.; Ricketts, D.N.J. Provisional Restorations—A Permanent Problem? Dent. Update 2016, 43, 908–912. [Google Scholar] [CrossRef] [PubMed]
- Ha, S.R.; Kim, S.H.; Lee, J.B.; Han, J.S. Improving shear bond strength of temporary crown and fixed dental prosthesis resins by surface treatments. J. Mater. Sci. 2016, 51, 1463–1475. [Google Scholar] [CrossRef]
- Revilla-León, M.; Meyers, M.J.; Zandinejad, A.; Özcan, M. A review on chemical composition, mechanical properties, and manufacturing work flow of additively manufactured current polymers for interim dental restorations. J. Esthet. Restor. Dent. 2019, 31, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Shibasaki, S.; Takamizawa, T.; Suzuki, T.; Nojiri, K.; Tsujimoto, A.; Barkmeier, W.W.; Latta, M.A.; Miyazaki, M. Influence of Different Curing Modes on Polymerization Behavior and Mechanical Properties of Dual-Cured Provisional Resins. Oper. Dent. 2017, 42, 526–536. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; Dal Piva, A.M.O.; de Jager, N.; Bottino, M.A.; de Kok, P.; Kleverlaan, C.J. Full-Crown Versus Endocrown Approach: A 3D-Analysis of Both Restorations and the Effect of Ferrule and Restoration Material. J. Prosthodont. 2020, 28. [Google Scholar] [CrossRef]
- Ghoul, W.E.; Özcan, M.; Tribst, J.P.M.; Salameh, Z. Fracture resistance, failure mode and stress concentration in a modified endocrown design. Biomater. Investig. Dent. 2020, 7, 110–119. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; Dal Piva, A.M.O.; Madruga, C.F.L.; Valera, M.C.; Borges, A.L.S.; Bresciani, E.; de Melo, R.M. Endocrown restorations: Influence of dental remnant and restorative material on stress distribution. Dent. Mater. 2018, 34, 1466–1473. [Google Scholar] [CrossRef]
- Da Fonseca, G.F.; Dal Piva, A.M.; Tribst, J.P.; Borges, A.L. Influence of Restoration Height and Masticatory Load Orientation on Ceramic Endocrowns. J. Contemp. Dent. Pract. 2018, 19, 1052–1057. [Google Scholar] [CrossRef]
- Da Fonseca, G.F.; de Andrade, G.S.; Dal Piva, A.M.O.; Tribst, J.P.M.; Borges, A.L.S. Computer-aided design finite element modeling of different approaches to rehabilitate endodontically treated teeth. J. Indian Prosthodont. Soc. 2018, 18, 329–335. [Google Scholar] [CrossRef]
- El Ghoul, W.A.; Özcan, M.; Ounsi, H.; Tohme, H.; Salameh, Z.J. Effect of different CAD-CAM materials on the marginal and internal adaptation of endocrown restorations: An in vitro study. J. Prosthet. Dent. 2020, 123, 128–134. [Google Scholar] [CrossRef] [PubMed]
- El Ghoul, W.; Özcan, M.; Silwadi, M.; Salameh, Z. Fracture resistance and failure modes of endocrowns manufactured with different CAD/CAM materials under axial and lateral loading. J. Esthet. Restor. Dent. 2019, 31, 378–387. [Google Scholar] [CrossRef] [PubMed]
- Gresnigt, M.M.; Özcan, M.; van den Houten, M.L.; Schipper, L.; Cune, M.S. Fracture strength, failure type and Weibull characteristics of lithium disilicate and multiphase resin composite endocrowns under axial and lateral forces. Dent. Mater. 2016, 32, 607–614. [Google Scholar] [CrossRef]
- Tribst, J.P.; Dal Piva, A.O.; Madruga, C.F.; Valera, M.C.; Bresciani, E.; Bottino, M.A.; de Melo, R.M. The impact of restorative material and ceramic thickness on CAD\CAM endocrowns. J. Clin. Exp. Dent. 2019, 11, 969–977. [Google Scholar] [CrossRef] [PubMed]
- Dogui, H.; Abdelmalek, F.; Amor, A.; Douki, N. Endocrown: An Alternative Approach for Restoring Endodontically Treated Molars with Large Coronal Destruction. Case. Rep. Dent. 2018, 1581952. [Google Scholar] [CrossRef]
- Irmaleny, Z.; Sholeh, A.; Mardiyah, A.; Agustin, D. Endocrown Restoration on Postendodontics Treatment on Lower First Molar. J. Int. Soc. Prev. Community Dent. 2019, 9, 303–310. [Google Scholar]
- Taha, D.; Abu-Elfadl, A.; Morsi, T. Minimally invasive prosthodontic correction of pseudo class III malocclusion by implementing a systematic digital workflow: A clinical report. J. Prosthet. Dent. 2021, 125, 8–14. [Google Scholar] [CrossRef]
- Dejak, B.; Młotkowski, A. A comparison of mvM stress of inlays, onlays and endocrowns made from various materials and their bonding with molars in a computer simulation of mastication—FEA. Dent. Mater. 2020, 36, 854–864. [Google Scholar] [CrossRef]
- Helal, M.A.; Wang, Z. Biomechanical Assessment of Restored Mandibular Molar by Endocrown in Comparison to a Glass Fiber Post-Retained Conventional Crown: 3D Finite Element Analysis. J. Prosthodont. 2019, 28, 988–996. [Google Scholar] [CrossRef] [PubMed]
- Dureja, I.; Yadav, B.; Malhotra, P.; Dabas, N.; Bhargava, A.; Pahwa, R. A comparative evaluation of vertical marginal fit of provisional crowns fabricated by computer-aided design/computer-aided manufacturing technique and direct (intraoral technique) and flexural strength of the materials: An in vitro study. J. Indian Prosthodont. Soc. 2018, 18, 314–320. [Google Scholar] [CrossRef]
- Li, X.; Kang, T.; Zhan, D.; Xie, J.; Guo, L. Biomechanical behavior of endocrowns vs fiber post-core-crown vs cast post-core-crown for the restoration of maxillary central incisors with 1 mm and 2 mm ferrule height: A 3D static linear finite element analysis. Medicine (Baltimore). 2020, 99, e22648. [Google Scholar] [CrossRef] [PubMed]
- Ausiello, P.; Ciaramella, S.; De Benedictis, A.; Lanzotti, A.; Tribst, J.P.M.; Watts, D.C. The use of different adhesive filling material and mass combinations to restore class II cavities under loading and shrinkage effects: A 3D-FEA. Comput. Methods Biomech. Biomed. Eng. 2020, 22, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, B.; Devi, N.N.; Gupta, N.; Singh, R. Comparative Evaluation of Various Temperature Changes on Stress Distribution in Class II Mesial-occlusal-distal Preparation restored with Different Restorative Materials: A Finite Element Analysis. Int. J. Clin. Pediatr. Dent. 2018, 11, 167–170. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.M.; Kelly, A.; Tagiyeva, N.; Kanagasingam, S. Comparing endocrown restorations on permanent molars and premolars: A systematic review and meta-analysis. Br. Dent. J. 2020, 12. [Google Scholar] [CrossRef] [PubMed]
- Belleflamme, M.M.; Geerts, S.O.; Louwette, M.M.; Grenade, C.F.; Vanheusden, A.J.; Mainjot, A.K. No post-no core approach to restore severely damaged posterior teeth: An up to 10-year retrospective study of documented endocrown cases. J. Dent. 2017, 63, 1–7. [Google Scholar] [CrossRef]
- Hollanders, A.C.C.; Kuper, N.K.; Huysmans, M.C.D.N.J.M.; Versluis, A. The effect of occlusal loading on cervical gap deformation: A 3D finite element analysis. Dent. Mater. 2020, 36, 681–686. [Google Scholar] [CrossRef]
- Naqash, T.A.; Alfarsi, M.; Hussain, M.W. Marginal accuracy of provisional crowns using three material systems and two techniques: A scanning electron microscope study. Pak. J. Med. Sci. 2019, 35, 55–60. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhao, Y.P. Adhesive Contact of Nanowire in Three-Point Bending Test. J. Adhes. Sci. Technol. 2011, 10, 1107–1129. [Google Scholar] [CrossRef][Green Version]
- Haralur, S.B.; Alamrey, A.A.; Alshehri, S.A.; Alzahrani, D.S.; Alfarsi, M. Effect of different preparation designs and all ceramic materials on fracture strength of molar endocrowns. J. Appl. Biomater. Funct. Mater. 2020, 18. [Google Scholar] [CrossRef]
- Lin, J.; Lin, Z.; Zheng, Z. Effect of different restorative crown design and materials on stress distribution in endodontically treated molars: A finite element analysis study. BMC. Oral. Health 2020, 18, 226. [Google Scholar] [CrossRef]
- Govare, N.; Contrepois, M. Endocrowns: A systematic review. J. Prosthet. Dent. 2020, 123, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Wang, D.; Rong, Q.; Qian, J.; Wang, X. Effect of central retainer shape and abduction angle during preparation of teeth on dentin and cement layer stress distributions in endocrown-restored mandibular molars. Dent. Mater. J. 2020, 5, 464–470. [Google Scholar] [CrossRef] [PubMed]
- Eskitaşçioğlu, M.; Küçük, O.; Eskitaşçioğlu, G.; Eraslan, O.; Belli, S. The Effect of Different Materials and Techniques on Stress Distribution in CAD/CAM Endocrowns. Strength Mater. 2020, 52, 812–819. [Google Scholar] [CrossRef]
- Yamaguchi, S.; Kani, R.; Kawakami, K.; Tsuji, M.; Inoue, S.; Lee, C.; Kiba, W.; Imazato, S. Fatigue behavior and crack initiation of CAD/CAM resin composite molar crowns. Dent. Mater. 2018, 34, 1578–1584. [Google Scholar] [CrossRef] [PubMed]
- Penteado, M.M.; Tribst, J.P.M.; Dal Piva, A.M.; Ausiello, P.; Zarone, F.; Garcia-Godoy, F.; Borges, A.L. Mechanical behavior of conceptual posterior dental crowns with functional elasticity gradient. Am. J. Dent. 2019, 32, 165–168. [Google Scholar]
- Zimmermann, M.; Valcanaia, A.; Neiva, G.; Mehl, A.; Fasbinder, D. Three-Dimensional Digital Evaluation of the Fit of Endocrowns Fabricated from Different CAD/CAM Materials. J. Prosthodont. 2019, 28, 504–509. [Google Scholar] [CrossRef]
- Zheng, Z.; He, Y.; Ruan, W.; Ling, Z.; Zheng, C.; Gai, Y.; Yan, W. Biomechanical behavior of endocrown restorations with different CAD-CAM materials: A 3D finite element and in vitro analysis. J. Prosthet. Dent. 2020, 26. [Google Scholar] [CrossRef]
- Al-Dabbagh, R.A. Survival and success of endocrowns: A systematic review and meta-analysis. J. Prosthet. Dent. 2020, 17. [Google Scholar] [CrossRef]
- Biacchi, G.R.; Mello, B.; Basting, R.T. The endocrown: An alternative approach for restoring extensively damaged molars. J. Esthet. Restor. Dent. 2013, 25, 383–390. [Google Scholar] [CrossRef]
- Madhavan, S.; Jude, S.M.; Achammada, S.; Ullattuthodi, S.; Kuriachan, T.; Jacob, J. Comparison of Marginal Accuracy of Interim Restoration Fabricated from Self-cure Composite and Autopolymerizing Acrylic Resin: An In Vitro Study. J. Pharm. Bioallied Sci. 2020, 12, S361–S366. [Google Scholar] [CrossRef]
- Miura, S.; Fujisawa, M.; Komine, F.; Maseki, T.; Ogawa, T.; Takebe, J.; Nara, Y. Importance of interim restorations in the molar region. J. Oral Sci. 2019, 18, 195–199. [Google Scholar] [CrossRef] [PubMed]


| Material/Structure | Composition | Elastic Modulus (GPa) * | Poisson Ratio | Reference |
|---|---|---|---|---|
| Enamel | - | 80 | 0.30 | [22] |
| Dentin | - | 18 | 0.23 | [22] |
| Fixation cylinder | Polyurethane resin | 3.6 | 0.30 | [5] |
| Temporary cement | Zinc oxide-based cement | 1.35 | 0.30 | [23] |
| Acrylic resin | Polymethyl methacrylate, diethyl phthalate, benzoyl peroxide, titanium dioxide. | 2.2 | 0.30 | [5] |
| Bis-acrylic resin | UDMA, bis-GMA, benzoyl peroxide, Amine and fillers. | 2.9 | 0.30 | [5] |
| Resin composite | UDMA, bis-GMA, bis-EMA, TEGDMA, Silica and fillers. | 8.0 | 0.25 | [22] |
| Acrylic Resin | Bis-Acrylic Resin | Resin Composite | |
|---|---|---|---|
| Tensile stress in the endocrown | 9.6 | 9.7 | 10.1 |
| Shear stress in the endocrown | 4.2 | 4.3 | 4.7 |
| Tensile stress in the cement layer | 8.9 | 8.8 | 3.4 |
| Shear stress in the cement layer | 9.2 | 9.0 | 7.5 |
| Tensile stress in the enamel tissue | 16.5 | 16.1 | 13.4 |
| Tensile stress in the dentin tissue | 15.9 | 15.2 | 9.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tribst, J.P.M.; Borges, A.L.S.; Silva-Concílio, L.R.; Bottino, M.A.; Özcan, M. Effect of Restorative Material on Mechanical Response of Provisional Endocrowns: A 3D—FEA Study. Materials 2021, 14, 649. https://doi.org/10.3390/ma14030649
Tribst JPM, Borges ALS, Silva-Concílio LR, Bottino MA, Özcan M. Effect of Restorative Material on Mechanical Response of Provisional Endocrowns: A 3D—FEA Study. Materials. 2021; 14(3):649. https://doi.org/10.3390/ma14030649
Chicago/Turabian StyleTribst, João Paulo Mendes, Alexandre Luiz Souto Borges, Laís Regiane Silva-Concílio, Marco Antonio Bottino, and Mutlu Özcan. 2021. "Effect of Restorative Material on Mechanical Response of Provisional Endocrowns: A 3D—FEA Study" Materials 14, no. 3: 649. https://doi.org/10.3390/ma14030649
APA StyleTribst, J. P. M., Borges, A. L. S., Silva-Concílio, L. R., Bottino, M. A., & Özcan, M. (2021). Effect of Restorative Material on Mechanical Response of Provisional Endocrowns: A 3D—FEA Study. Materials, 14(3), 649. https://doi.org/10.3390/ma14030649








