Comparison between Hydrofluoric Acid and Single-Component Primer as Conditioners on Resin Cement Adhesion to Lithium Silicate and Lithium Disilicate Glass Ceramics
Abstract
:1. Introduction
2. Materials and Methods
2.1. Microshear Bond Strength Test (µSBS)
2.2. Statistical Analysis
2.3. Scanning Electron Microscope Evaluation (SEM)
3. Results
3.1. Microshear Bond Strength Test (µSBS)
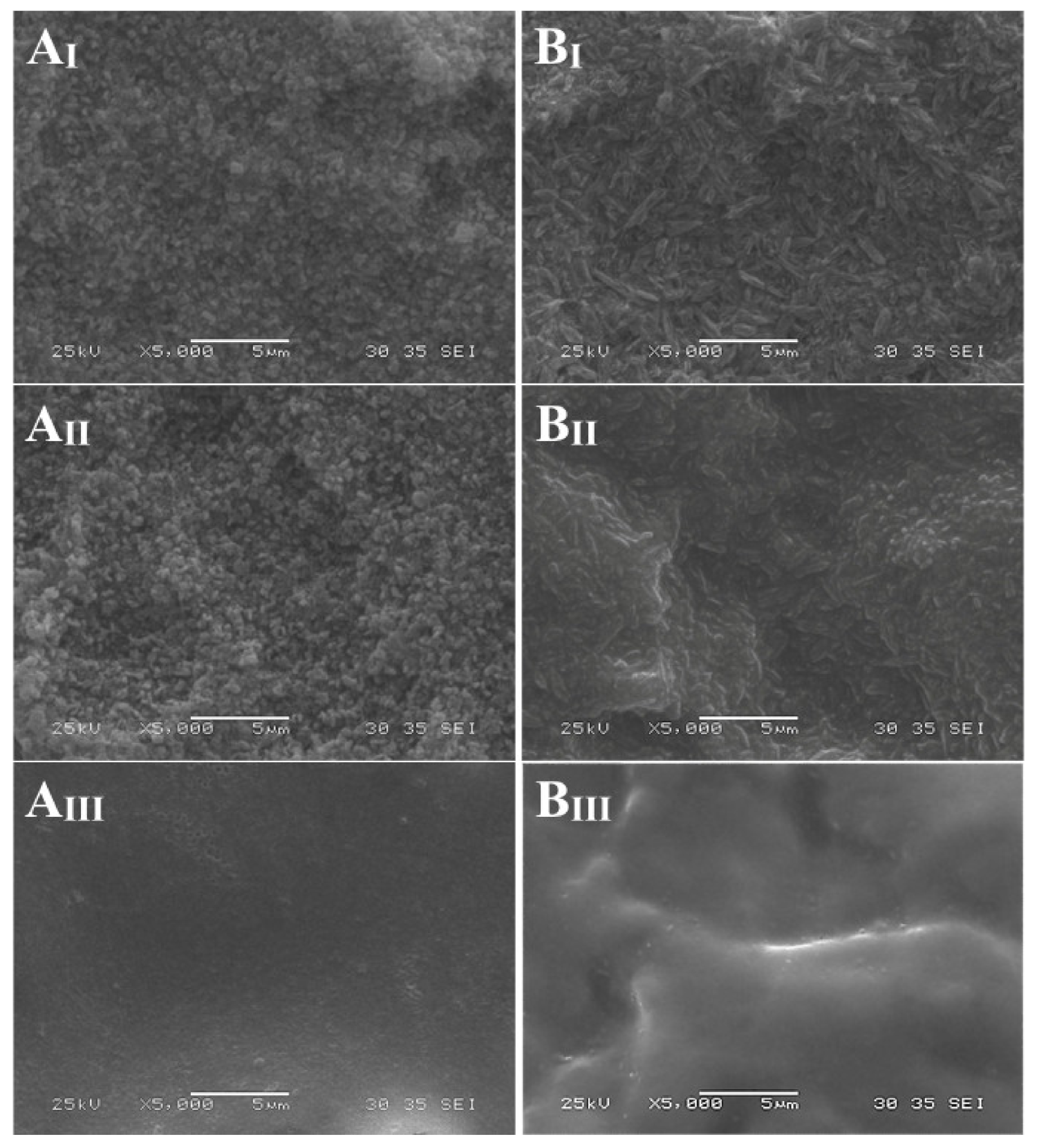
3.2. Scanning Electron Microscope Evaluation (SEM)
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fabian Fonzar, R.; Carrabba, M.; Sedda, M.; Ferrari, M.; Goracci, C.; Vichi, A. Flexural resistance of heat-pressed and CAD-CAM lithium disilicate with different translucencies. Dent. Mater. 2017, 33, 63–70. [Google Scholar] [CrossRef]
- Vichi, A.; Sedda, M.; Del Siena, F.; Louca, C.; Ferrari, M. Flexural resistance of Cerec CAD/CAM system ceramic blocks. Part 1: Chairside materials. Am. J. Dent. 2013, 26, 255–259. [Google Scholar]
- Vichi, A.; Fabian Fonzar, R.; Goracci, C.; Carrabba, M.; Ferrari, M. Effect of finishing and polishing on roughness and gloss of lithium disilicate and lithium silicate zirconia reinforced glass ceramic for CAD/CAM systems. Oper. Dent. 2018, 43, 90–100. [Google Scholar] [CrossRef]
- Aboushelib, M.N.; Sleem, D. Microtensile bond strength of lithium disilicate ceramics to resin adhesives. J. Adhes. Dent. 2014, 16, 547–552. [Google Scholar]
- Della Bona, A.; Shen, C.; Anusavice, K.J. Work of adhesion of resin on treated lithia disilicate-based ceramic. Dent. Mater. 2004, 20, 338–344. [Google Scholar] [CrossRef]
- ISO-Standards ISO 6872. Dentistry: Ceramic Materials International Organization for Standardization, 4th ed.; ISO: Geneve, Switzerland, 2015. [Google Scholar]
- Heintze, S.D.; Cavalleri, A.; Zellweger, G.; Büchler, A.; Zappini, G. Fracture frequency of all-ceramic crowns during dynamic loading in a chewing simulator using different loading and luting protocols. Dent. Mater. 2008, 24, 1352–1361. [Google Scholar] [CrossRef] [PubMed]
- Özcan, M.; Vallittu, P.K. Effect of surface conditioning methods on the bond strength of luting cement to ceramics. Dent. Mater. 2003, 19, 725–731. [Google Scholar] [CrossRef] [Green Version]
- Gerth, H.U.; Dammaschke, T.; Züchner, H.; Schäfer, E. Chemical analysis and bonding reaction of RelyX Unicem and Bifix composites—A comparative study. Dent. Mater. 2006, 22, 934–941. [Google Scholar] [CrossRef]
- Hu, M.; Weiger, R.; Fischer, J. Comparison of two test designs for evaluating the shear bond strength of resin composite cements. Dent. Mater. 2016, 32, 223–232. [Google Scholar] [CrossRef]
- Magne, P.; Carvalho, A.O.; Bruzi, G.; Giannini, M. Fatigue resistance of ultrathin CAD/CAM complete crowns with a simplified cementation process. J. Prosthet. Dent. 2015, 114, 574–579. [Google Scholar] [CrossRef]
- Yousaf, A.; Aman, N.; Manzoor, M.A.; Shah, J.A. Postoperative sensitivity of self-etch versus total etch adhesive. J. Coll. Physicians Surg. Pak. 2014, 24, 383–386. [Google Scholar] [PubMed]
- Tian, T.; Tsoi, J.K.; Matinlinna, J.P.; Burrow, M.F. Aspects of bonding between resin luting cements and glass ceramic materials. Dent. Mater. 2014, 30, 147–162. [Google Scholar] [CrossRef]
- Filho, A.M.; Vieira, L.C.; Araújo, E.; Monteiro Júnior, S. Effect of different ceramic surface treatments on resin microtensile bond strength. J. Prosthodont. 2004, 13, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Gökçe, B.; Ozpinar, B.; Dündar, M.; Cömlekoglu, E.; Sen, B.H.; Güngör, M.A. Bond strengths of all-ceramics: Acid vs laser etching. Oper. Dent. 2007, 32, 173–178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matinlinna, J.P.; Lassila, L.V.; Özcan, M.; Yli-Urpo, A.; Vallittu, P.K. An introduction to silanes and their clinical applications in dentistry. Int. J. Prosthodont. 2004, 17, 155–164. [Google Scholar]
- Spohr, A.M.; Sobrinho, L.C.; Consani, S.; Sinhoreti, M.A.; Knowles, J.C. Influence of surface conditions and silane agent on the bond of resin to IPS Empress 2 ceramic. Int. J. Prosthodont. 2003, 16, 277–282. [Google Scholar]
- Güler, A.U.; Yilmaz, F.; Yenisey, M.; Güler, E.; Ural, C. Effect of acid etching time and a self-etching adhesive on the shear bond strength of composite resin to porcelain. J. Adhes. Dent. 2006, 8, 21–25. [Google Scholar]
- Della Bona, A.; Anusavice, K.J. Microstructure, composition, and etching topography of dental ceramics. Int. J. Prosthodont. 2002, 15, 159–167. [Google Scholar]
- Söderholm, K.J.; Shang, S.W. Molecular orientation of silane at the surface of colloidal silica. J. Dent. Res. 1993, 72, 1050–1054. [Google Scholar] [CrossRef] [PubMed]
- Kern, M. Bonding to oxide ceramics—Laboratory testing versus clinical outcome. Dent. Mater. 2015, 31, 8–14. [Google Scholar] [CrossRef]
- Jardel, V.; Degrange, M.; Picard, B.; Derrien, G. Correlation of topography to bond strength of etched ceramic. Int. J. Prosthodont. 1999, 12, 59–64. [Google Scholar]
- Amaral, R.; Özcan, M.; Bottino, M.A.; Valandro, L.F. Microtensile bond strength of a resin cement to glass infiltrated zirconia-reinforced ceramic: The effect of surface conditioning. Dent. Mater. 2006, 22, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Özcan, M.; Allahbeickaraghi, A.; Dündar, M. Possible hazardous effects of hydrofluoric acid and recommendations for treatment approach: A review. Clin. Oral Investig. 2012, 16, 15–23. [Google Scholar] [CrossRef]
- Siqueira, F.S.; Alessi, R.S.; Cardenas, A.F.; Kose, C.; Souza Pinto, S.C.; Bandeca, M.C. New single-bottle ceramic primer: 6-month case report and laboratory performance. J. Contemp. Dent. Pract. 2016, 17, 1033–1039. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fabian Fonzar, R.; Goracci, C.; Carrabba, M.; Louca, C.; Ferrari, M.; Vichi, A. Influence of acid concentration and etching time on composite cement adhesion to lithium-silicate glass ceramics. J. Adhes. Dent. 2020, 22, 175–182. [Google Scholar]
- Cardoso, P.E.; Braga, R.R.; Carrilho, M.R. Evaluation of micro-tensile, shear and tensile tests determining the bond strength of three adhesive systems. Dent. Mater. 1998, 14, 394–398. [Google Scholar] [CrossRef]
- Chen, J.H.; Matsumura, H.; Atsuta, M. Effect of different etching periods on the bond strength of a composite resin to a machinable porcelain. J. Dent. 1998, 26, 53–58. [Google Scholar] [CrossRef]
- Della Bona, A.; Anusavice, K.J.; Hood, J.A. Effect of ceramic surface treatment on tensile bond strength to a resin cement. Int. J. Prosthodont. 2002, 15, 248–253. [Google Scholar] [PubMed]
- Sundfeld Neto, D.; Naves, L.Z.; Costa, A.R.; Correr, A.B.; Consani, S.; Borges, G.A. The effect of hydrofluoric acid concentration on the bond strength and morphology of the surface and interface of glass ceramics to a resin cement. Oper. Dent. 2015, 40, 470–479. [Google Scholar] [CrossRef] [Green Version]
- Da Silveira, B.L.; Paglia, A.; Burnett, L.H.; Shinkai, R.S.; Eduardo Cde, P.; Spohr, A.M. Micro-tensile bond strength between a resin cement and an aluminous ceramic treated with Nd:YAG laser, Rocatec System, or aluminum oxide sandblasting. Photomed. Laser Surg. 2005, 23, 543–548. [Google Scholar] [CrossRef]
- Kukiattrakoon, B.; Thammasitboon, K. The effect of different etching times of acidulated phosphate fluoride gel on the shear bond strength of high-leucite ceramics bonded to composite resin. J. Prosthet. Dent. 2007, 98, 17–23. [Google Scholar] [CrossRef]
- Panah, F.G.; Rezai, S.M.; Ahmadian, L. The influence of ceramic surface treatments on the micro-shear bond strength of composite resin to IPS Empress. J. Prosthodont. 2008, 17, 409–414. [Google Scholar] [CrossRef] [PubMed]
- Pisani-Proenca, J.; Erhardt, M.C.; Valandro, L.F.; Gutierrez-Aceves, G.; Bolanos-Carmona, M.V.; Del Castillo-Salmeron, R. Influence of ceramic surface conditioning and resin cements on microtensile bond strength to a glass ceramic. J. Prosthet. Dent. 2006, 96, 412–417. [Google Scholar] [CrossRef]
- Heintze, S.D.; Zimmerli, B. Relevance of in vitro tests of adhesive and composite dental materials. A review in 3 parts. Part 3: In vitro tests of adhesive systems. Schweiz. Monatsschr. Zahnmed. 2011, 121, 1024–1040. [Google Scholar]
- Ho, G.W.; Matinlinna, J.P. Insights on ceramics as dental materials. Part II: Chemical surface treatments. Silicon 2011, 3, 117–123. [Google Scholar] [CrossRef]
- El-Damanhoury, H.M.; Gaintantzopoulou, M.D. Self-etching ceramic primer versus hydrofluoric acid etching: Etching efficacy and bonding performance. J. Prosthodont. Res. 2018, 62, 75–83. [Google Scholar] [CrossRef]
- Román-Rodríguez, J.L.; Perez-Barquero, J.A.; Gonzalez-Angulo, E.; Fons-Font, A.; Bustos-Salvador, J.L. Bonding to silicate ceramics: Conventional technique compared with a simplified technique. J. Clin. Exp. Dent. 2017, 9, 384–386. [Google Scholar] [CrossRef] [Green Version]
- Zorzin, J.; Belli, R.; Wagner, A.; Petschelt, A.; Lohbauer, U. Self-adhesive resin cements: Adhesive performance to indirect restorative ceramics. J. Adhes. Dent. 2014, 16, 541–546. [Google Scholar]
- Sato, T.P.; Anami, L.C.; Melo, R.M.; Valandro, L.F.; Bottino, M.A. Effects of surface treatments on the bond strength between resin cement and a new zirconia-reinforced lithium silicate ceramic. Oper. Dent. 2016, 41, 284–292. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salvio, L.A.; Correr-Sobrinho, L.; Consani, S.; Sinhoreti, M.A.; de Goes, M.F.; Knowles, J.C. Effect of water storage and surface treatments on the tensile bond strength of IPS Empress 2 ceramic. J. Prosthodont. 2007, 16, 192–199. [Google Scholar] [CrossRef]
- Pollington, S.; Fabianelli, A.; van Noort, R. Microtensile bond strength of a resin cement to a novel fluorcanasite glass-ceramic following different surface treatments. Dent. Mater. 2010, 26, 864–872. [Google Scholar] [CrossRef]
- Canay, S.; Hersek, N.; Ertan, A. Effect of different acid treatments on a porcelain surface. J. Oral Rehabil. 2001, 28, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Barghi, N.; Fischer, D.E.; Vatani, L. Effects of porcelain leucite content, types of etchants, and etching time on porcelain-composite bond. J. Esthet. Restor. Dent. 2006, 18, 47–53. [Google Scholar] [CrossRef]
- Caparroso, C.B.; Latorre, F.; Arroyave, L.J.; Grajales, C.A. In vitro evaluation of the effect of hydrofluoric acid concentration and application time on adhesion to lithium disilicate. Rev. Fac. Odontol. Univ. Antioq. 2014, 26, 62–75. [Google Scholar]
- Shimada, Y.; Yamaguchi, S.; Tagami, J. Micro-shear bond strength of dual-cured resin cement to glass ceramics. Dent. Mater. 2002, 18, 380–388. [Google Scholar] [CrossRef]
- Scrabeck, J.G.; Eames, W.B.; Noonan, J.E. A method for uniform seating pressure on castings during cementation. J. Prosthet. Dent. 1987, 57, 537–539. [Google Scholar] [CrossRef]
- Sato, K.; Matsumura, H.; Atsuta, M. Effect of three-liquid bonding agents on bond strength to a machine-milled ceramic material. J. Oral Rehabil. 1999, 26, 570–574. [Google Scholar] [CrossRef]
- Prado, M.; Prochnow, C.; Marchionatti, A.M.E.; Baldissara, P.; Valandro, L.F.; Wandscher, V.F. Ceramic surface treatment with a single-component primer: Resin adhesion to glass ceramics. J. Adhes. Dent. 2018, 20, 99–105. [Google Scholar]
- Maier, E.; Bordihn, V.; Belli, R.; Taschner, M.; Petschelt, A.; Lohbauer, U. New approaches in bonding to glass-ceramic: Self-etch glass-ceramic primer and universal adhesives. J. Adhes. Dent. 2019, 21, 209–217. [Google Scholar]
- Lyann, S.K.; Takagaki, T.; Nikaido, T.; Uo, M.; Ikeda, M.; Sadr, A. Effect of different surface treatments on the tensile bond strength to lithium disilicate glass ceramics. J. Adhes. Dent. 2018, 20, 261–268. [Google Scholar]
- Lopes, G.C.; Perdigão, J.; Baptista, D.; Ballarin, A. Does a self-etching ceramic primer improve bonding to lithium disilicate ceramics? Bond strengths and FESEM analyses. Oper. Dent. 2019, 44, 210–218. [Google Scholar] [CrossRef] [PubMed]
- Dönmez, M.B.; Yucel, M.T.; Kilic, I.; Okutan, Y. Novel ceramic primer vs. conventional treatment methods: Effects on roughness and bond strength of all-ceramic restorations. Am. J. Dent. 2018, 31, 249–252. [Google Scholar] [PubMed]
- Wille, S.; Lehmann, F.; Kern, M. Durability of resin bonding to lithium disilicate and zirconia ceramic using a self-etching primer. J. Adhes. Dent. 2017, 19, 491–496. [Google Scholar] [PubMed]
| Material | Conditioning Protocol | Mean | SD | N |
|---|---|---|---|---|
| ZLS 25.51 (8.94) | HF | 24.66 | 11.02 | 15 |
| HF + S | 23.13 | 8.97 | 15 | |
| EP | 28.42 | 5.68 | 15 | |
| LD 26.23 (10.53) | HF | 19.73 | 8.38 | 15 |
| HF + S | 27.24 | 12.96 | 15 | |
| EP | 31.06 | 6.41 | 15 | |
| Conditioning Protocol | ||||
| HF b 22.19 (9.94) HF + S ab 25.12 (11.11) EP a 29.81 (6.13) | ||||
| Groups | |||||||
|---|---|---|---|---|---|---|---|
| ZLS HF a | ZLS HF + S a | ZLS EP b | LD HF a | LD HF + S a | LD EP a | ||
| Failure modes | M | 4 | 4 | 14 | 3 | 0 | 0 |
| A | 11 | 11 | 1 | 12 | 13 | 13 | |
| CR | 0 | 0 | 0 | 0 | 2 | 2 | |
| CC | 0 | 0 | 0 | 0 | 0 | 0 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vichi, A.; Fabian Fonzar, R.; Carrabba, M.; Louca, C.; Scotti, N.; Mazzitelli, C.; Breschi, L.; Goracci, C. Comparison between Hydrofluoric Acid and Single-Component Primer as Conditioners on Resin Cement Adhesion to Lithium Silicate and Lithium Disilicate Glass Ceramics. Materials 2021, 14, 6776. https://doi.org/10.3390/ma14226776
Vichi A, Fabian Fonzar R, Carrabba M, Louca C, Scotti N, Mazzitelli C, Breschi L, Goracci C. Comparison between Hydrofluoric Acid and Single-Component Primer as Conditioners on Resin Cement Adhesion to Lithium Silicate and Lithium Disilicate Glass Ceramics. Materials. 2021; 14(22):6776. https://doi.org/10.3390/ma14226776
Chicago/Turabian StyleVichi, Alessandro, Riccardo Fabian Fonzar, Michele Carrabba, Chris Louca, Nicola Scotti, Claudia Mazzitelli, Lorenzo Breschi, and Cecilia Goracci. 2021. "Comparison between Hydrofluoric Acid and Single-Component Primer as Conditioners on Resin Cement Adhesion to Lithium Silicate and Lithium Disilicate Glass Ceramics" Materials 14, no. 22: 6776. https://doi.org/10.3390/ma14226776
APA StyleVichi, A., Fabian Fonzar, R., Carrabba, M., Louca, C., Scotti, N., Mazzitelli, C., Breschi, L., & Goracci, C. (2021). Comparison between Hydrofluoric Acid and Single-Component Primer as Conditioners on Resin Cement Adhesion to Lithium Silicate and Lithium Disilicate Glass Ceramics. Materials, 14(22), 6776. https://doi.org/10.3390/ma14226776











