Classification and Properties of Dental Zirconia as Implant Fixtures and Superstructures
Abstract
:1. Introduction
2. Evolution and Classification of Dental Zirconia
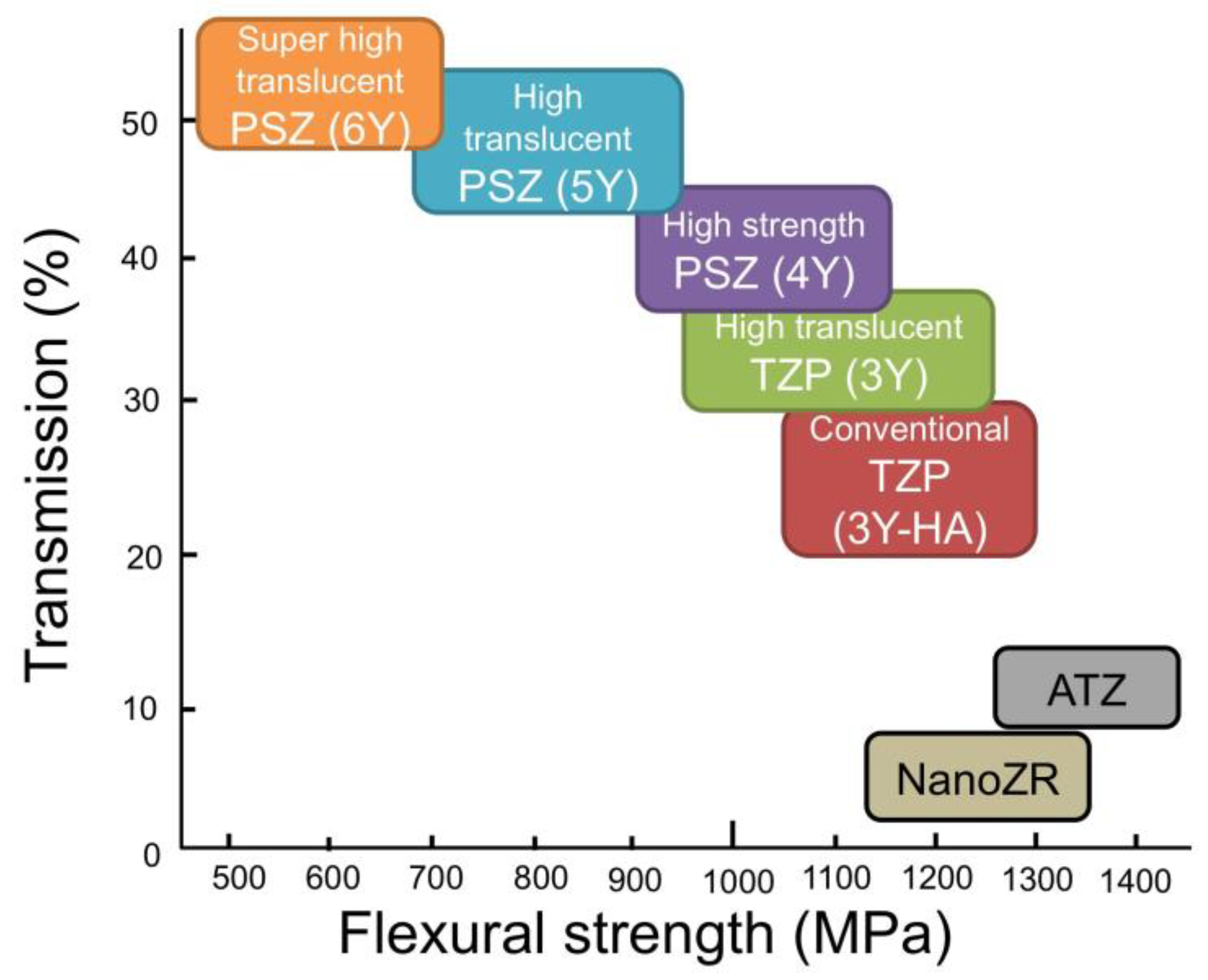
2.1. TZP and PSZ
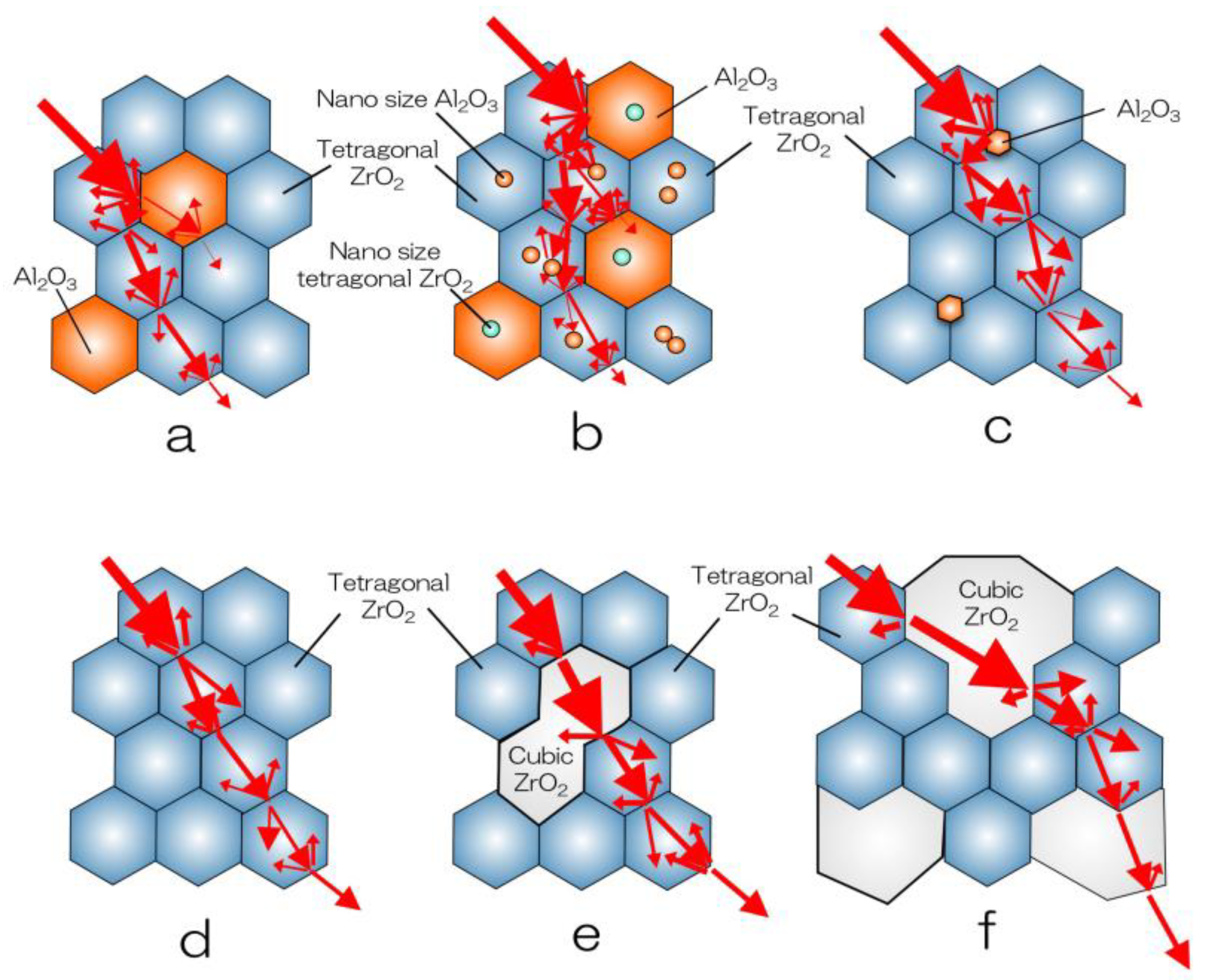
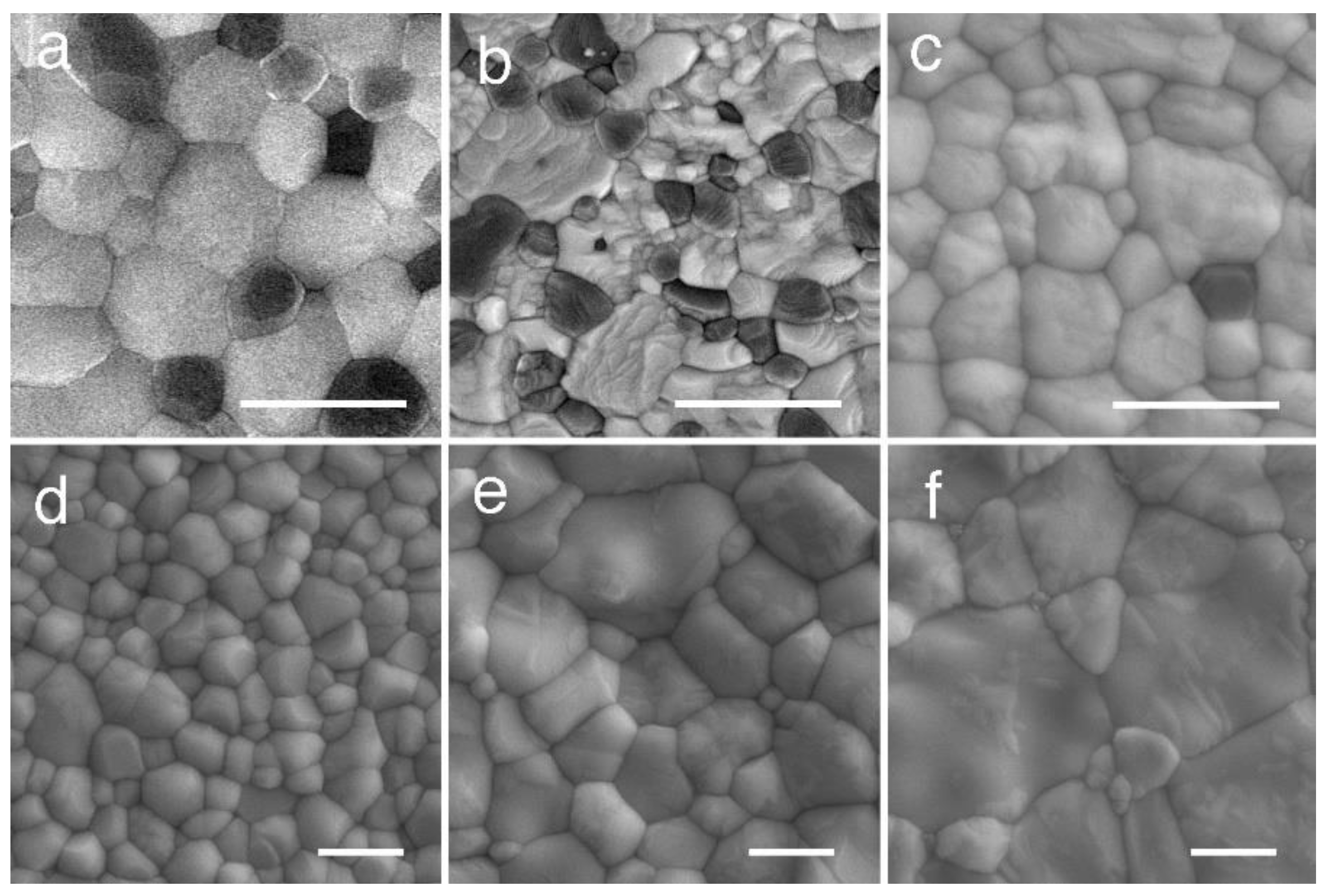
2.2. Zirconia–Alumina Composites
2.3. Evolution of Yttria-Stabilized Dental Zirconia
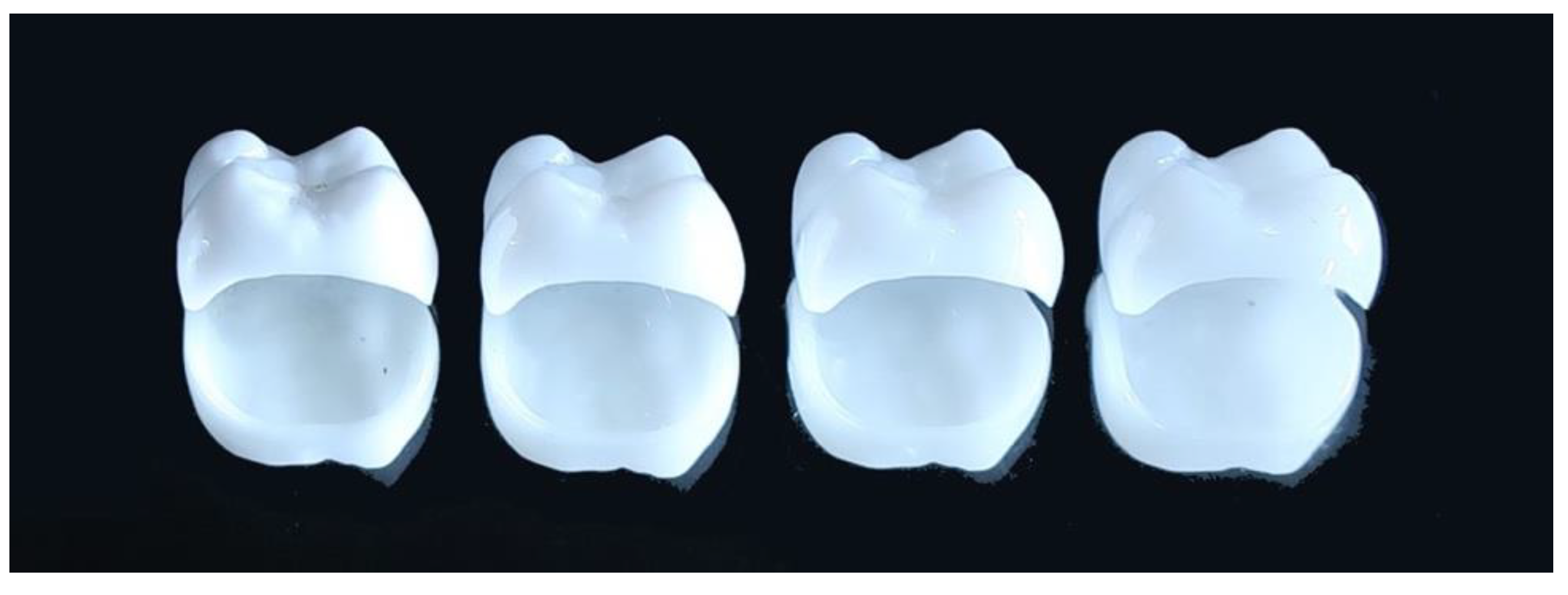
2.4. Classification and Indication of Yttria-Stabilized Dental Zirconia
3. Properties of Dental Zirconia
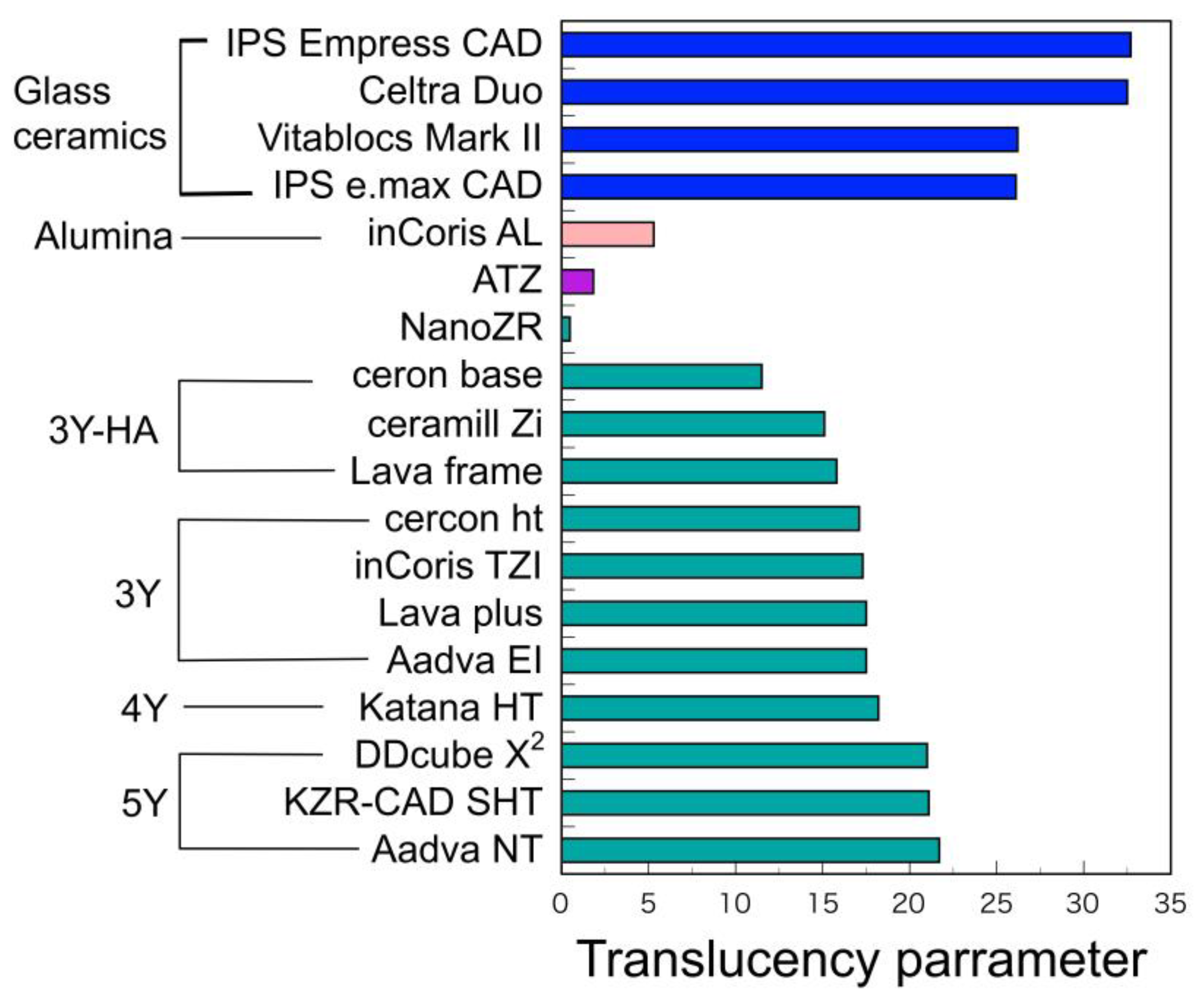
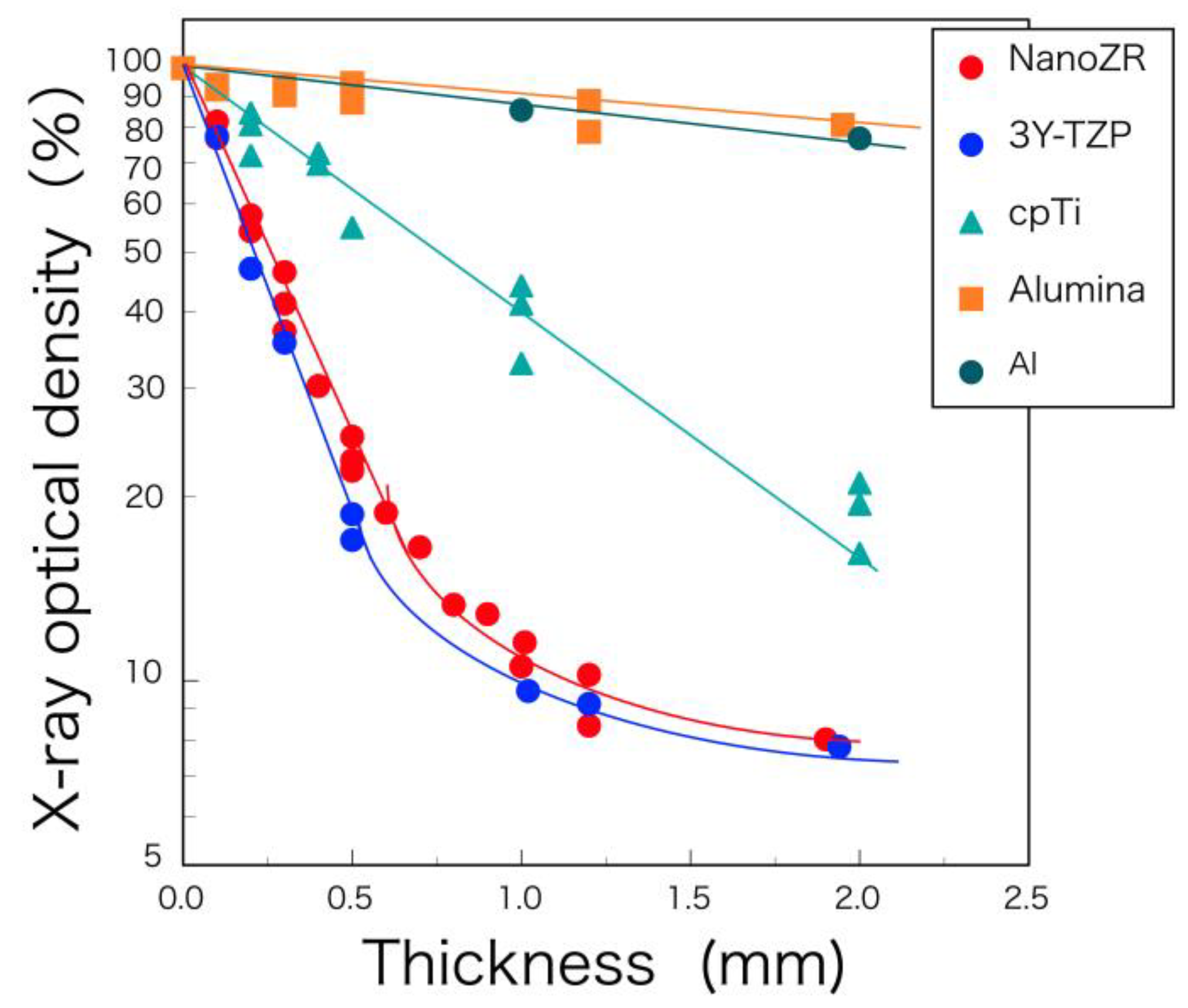
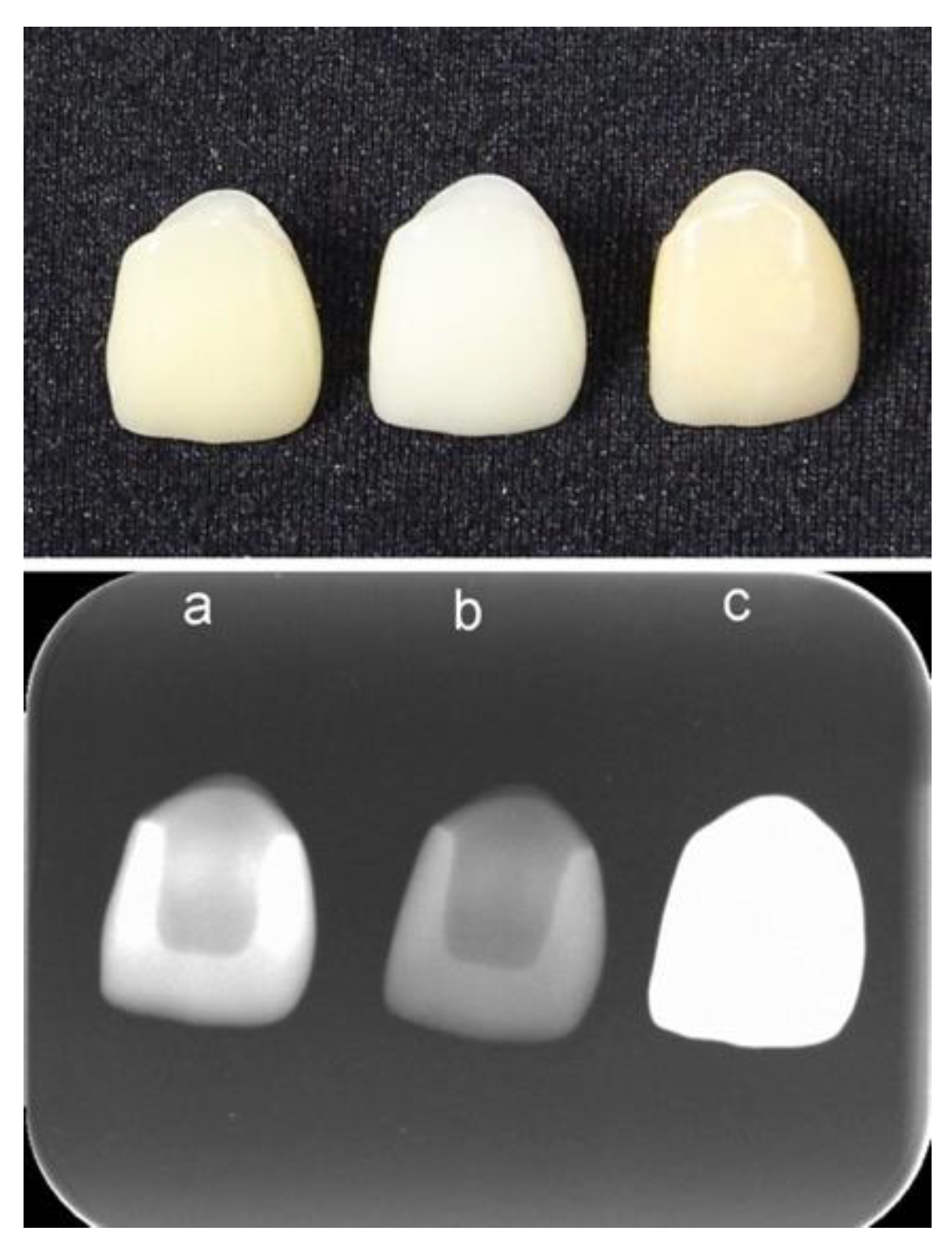
3.1. Physical Properties
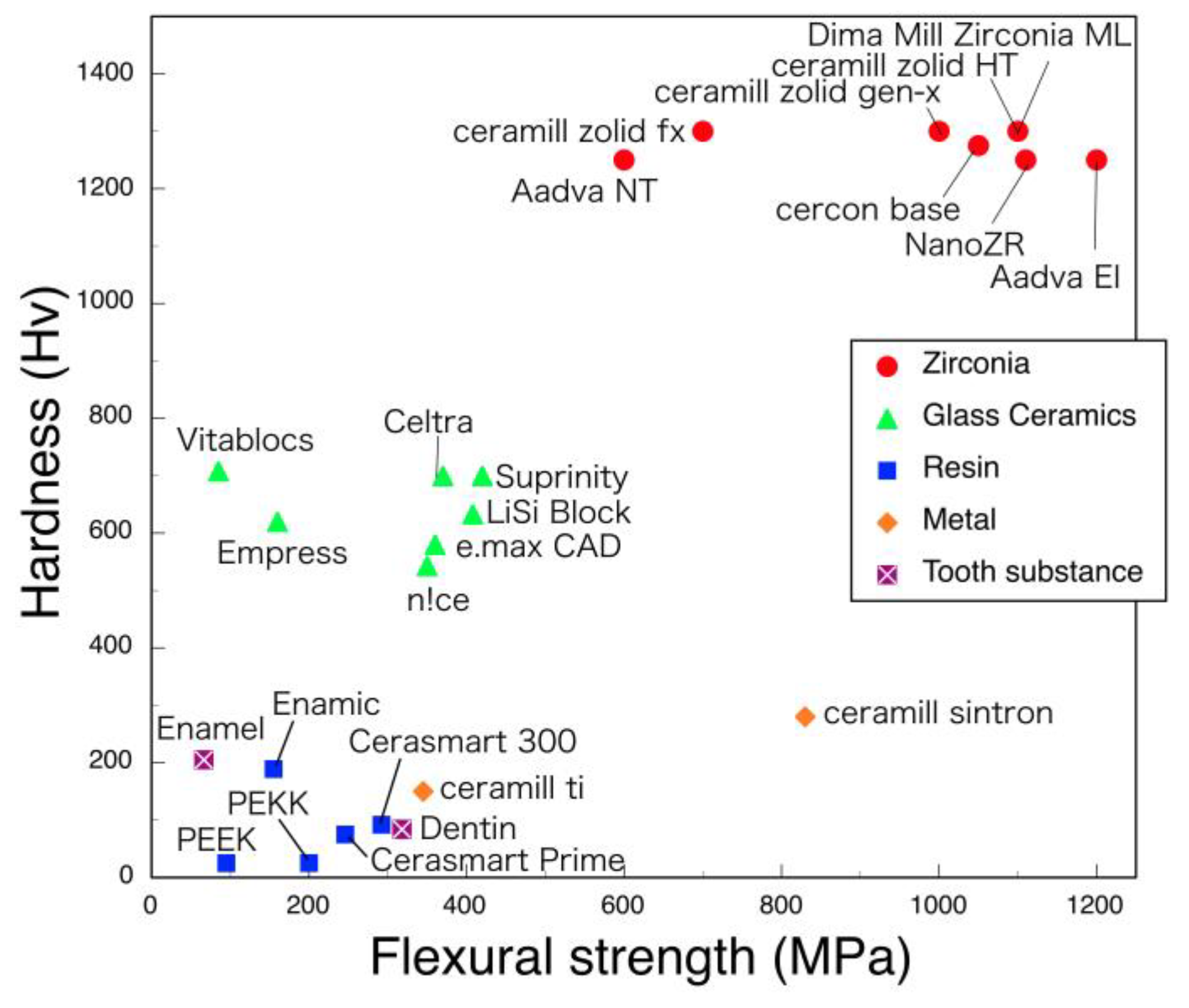
3.2. Mechanical Properties
3.2.1. Hardness, Flexural Strength, and Fracture Toughness
3.2.2. Fracture Strength of Zirconia Implant
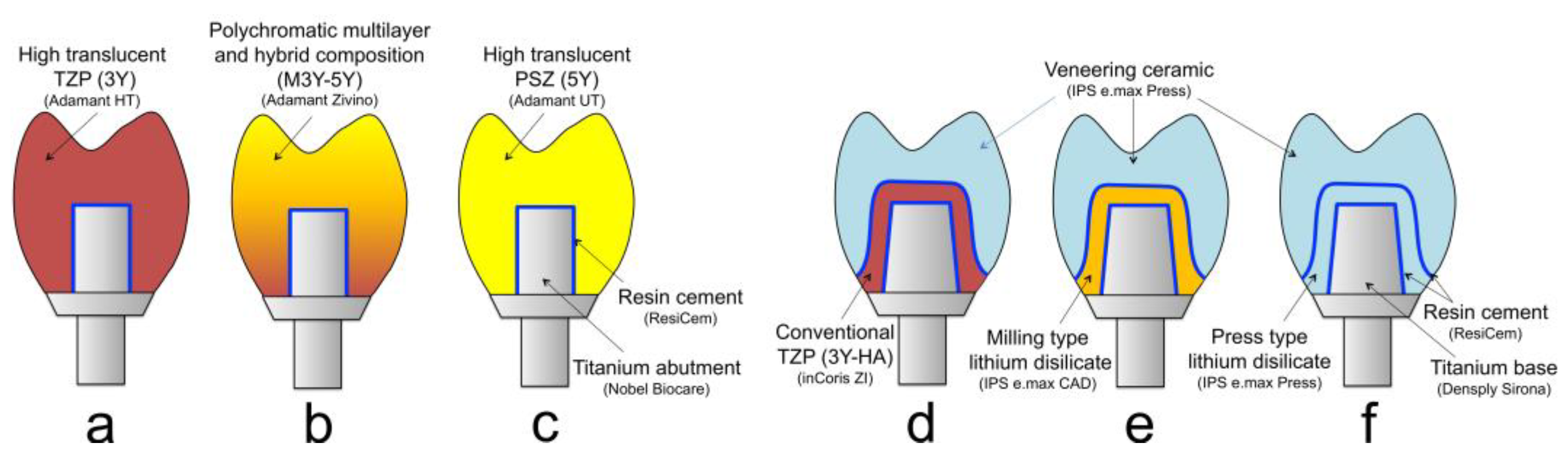
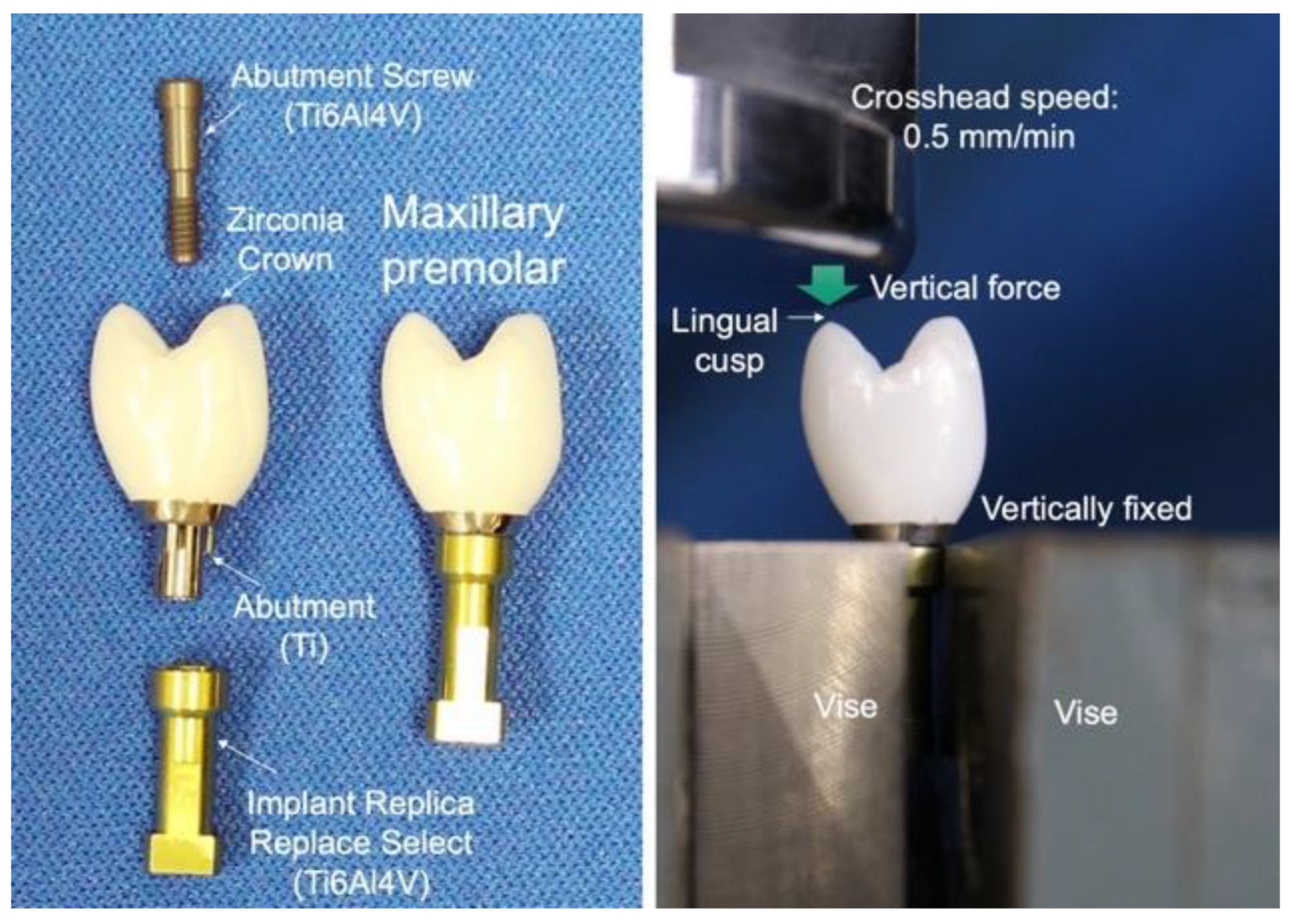
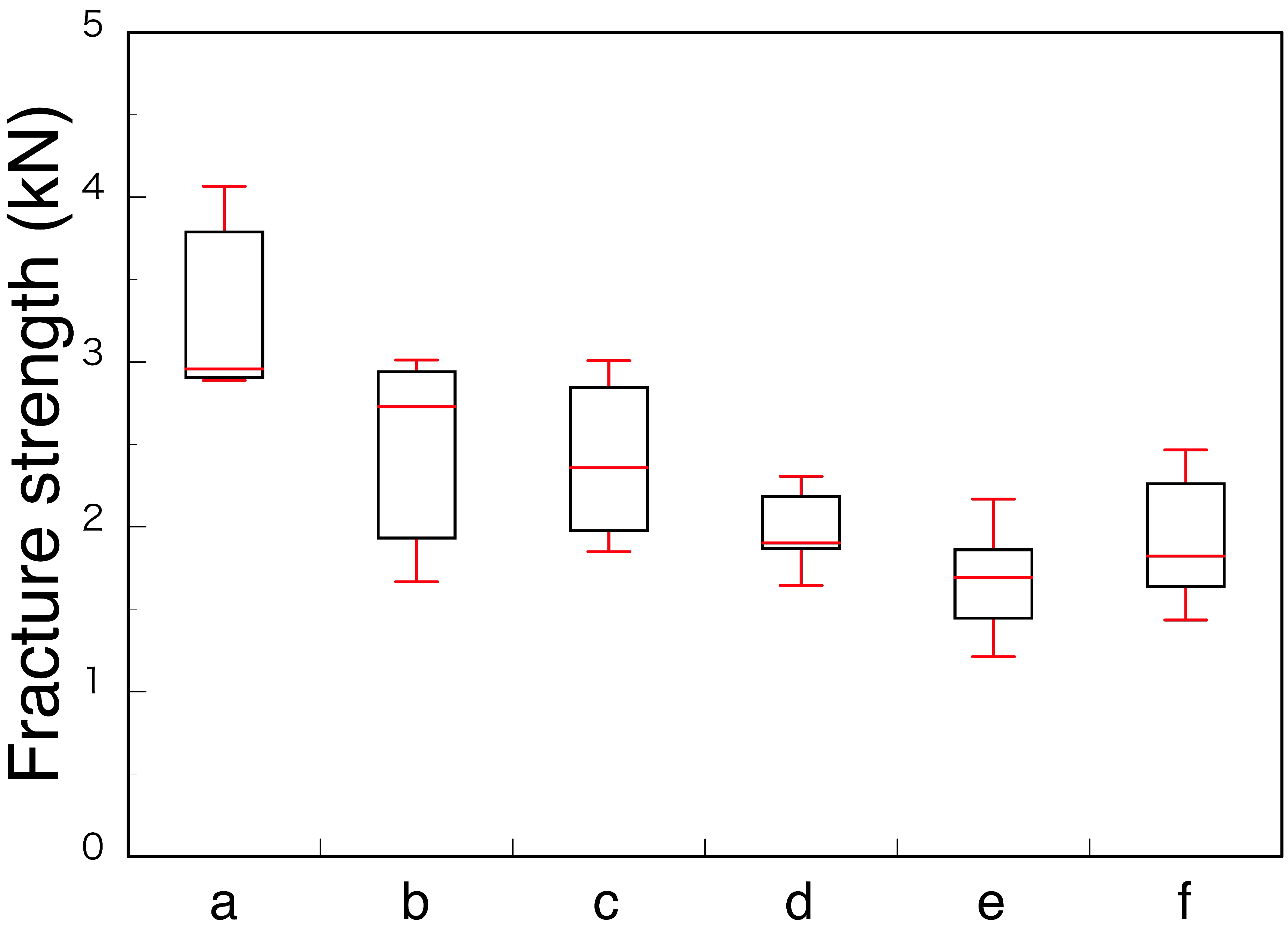
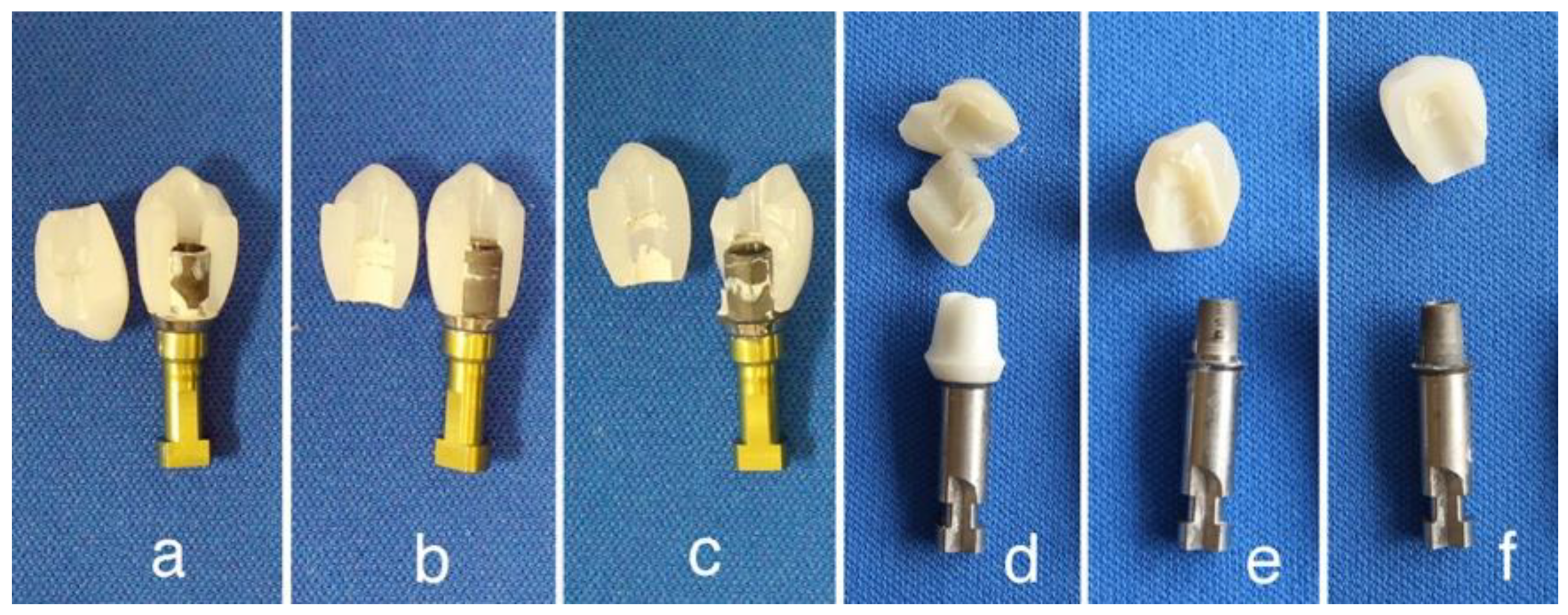
3.2.3. Fracture Strength of Zirconia Superstructure
3.3. Chemical Properties
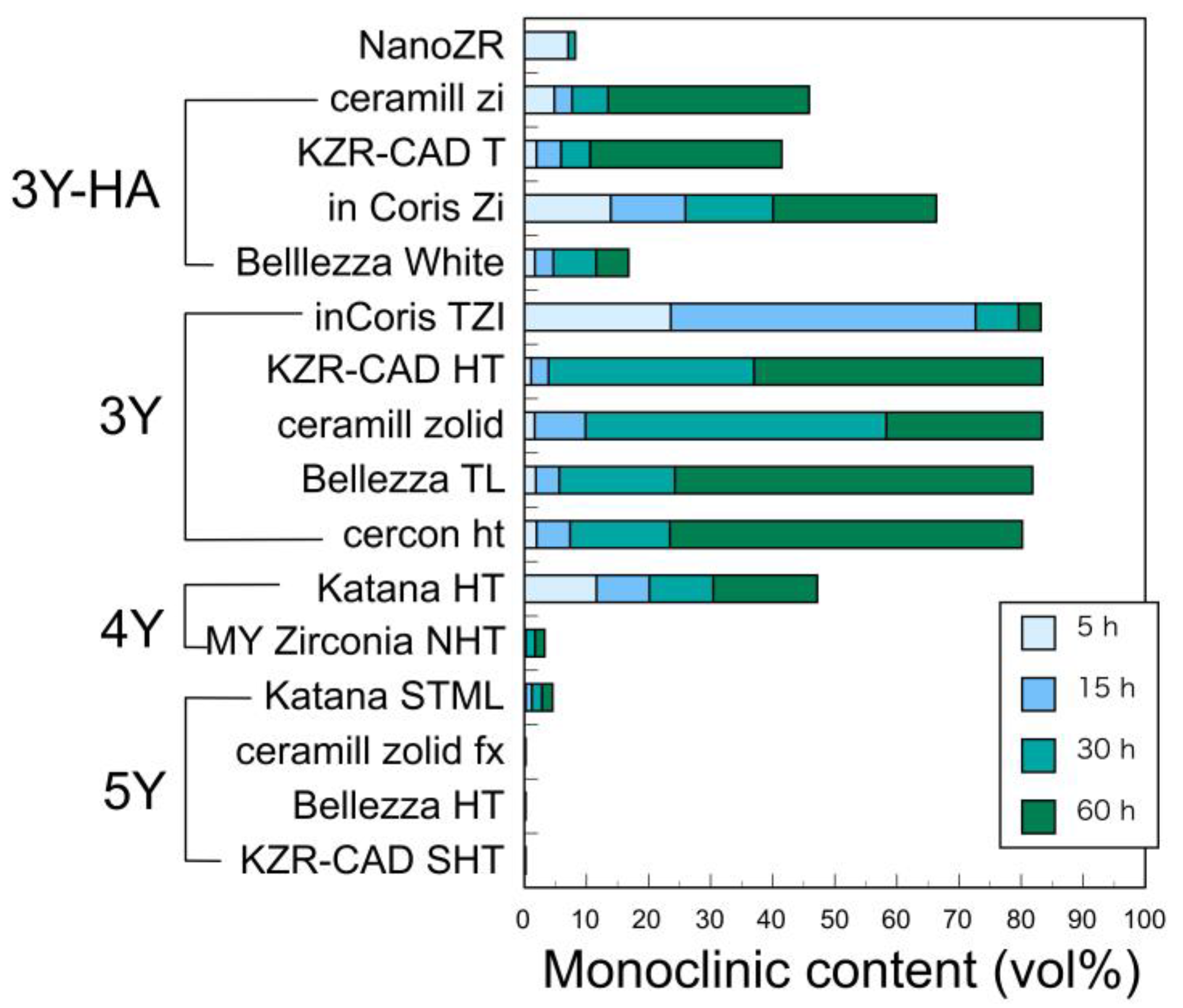
3.3.1. Low Temperature Degradation (LTD)
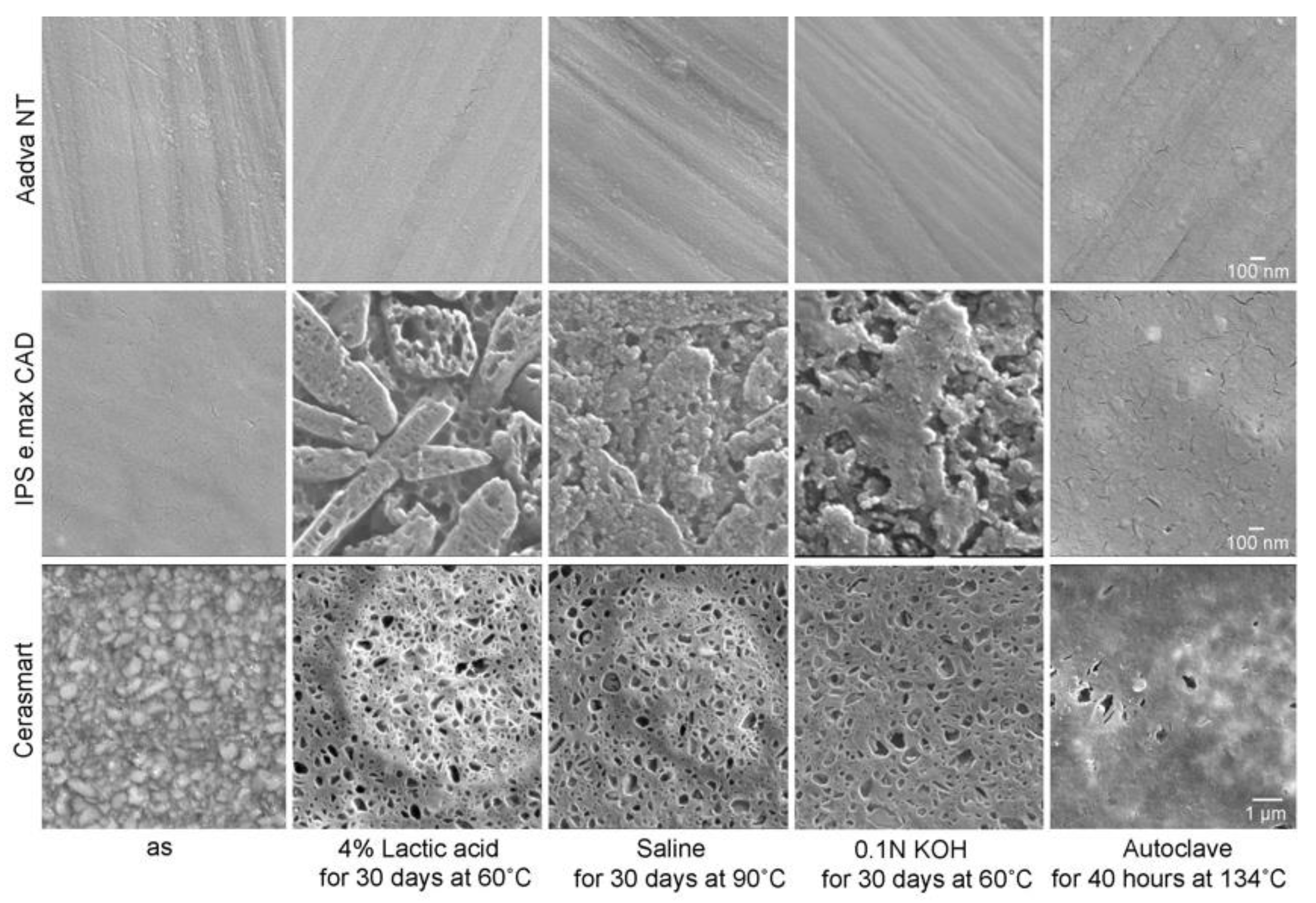
3.3.2. Erosion in Water-Based Solution
3.4. Abrasion Properties
3.5. Biological Properties
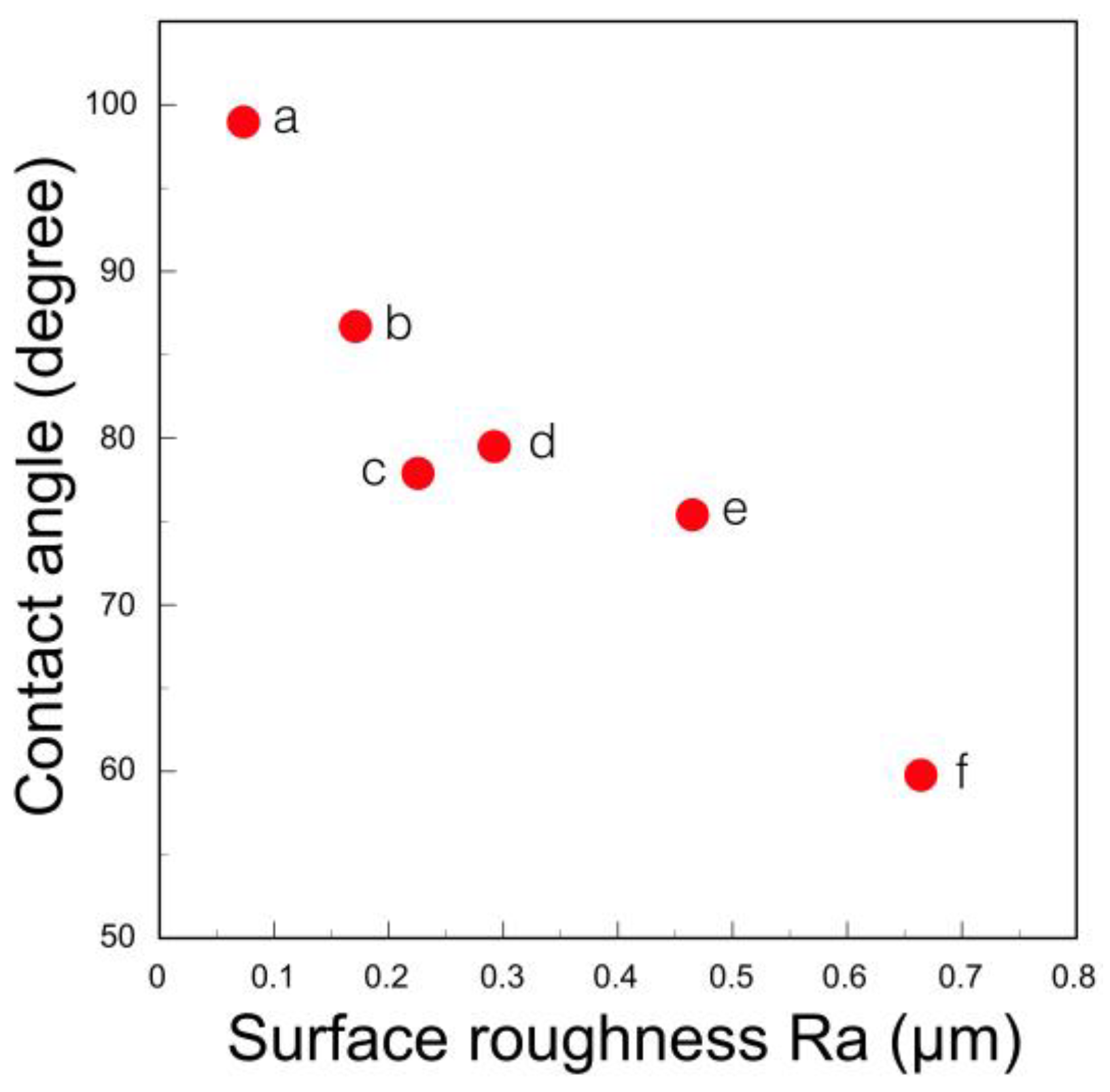
3.5.1. Bacterial Adhesion
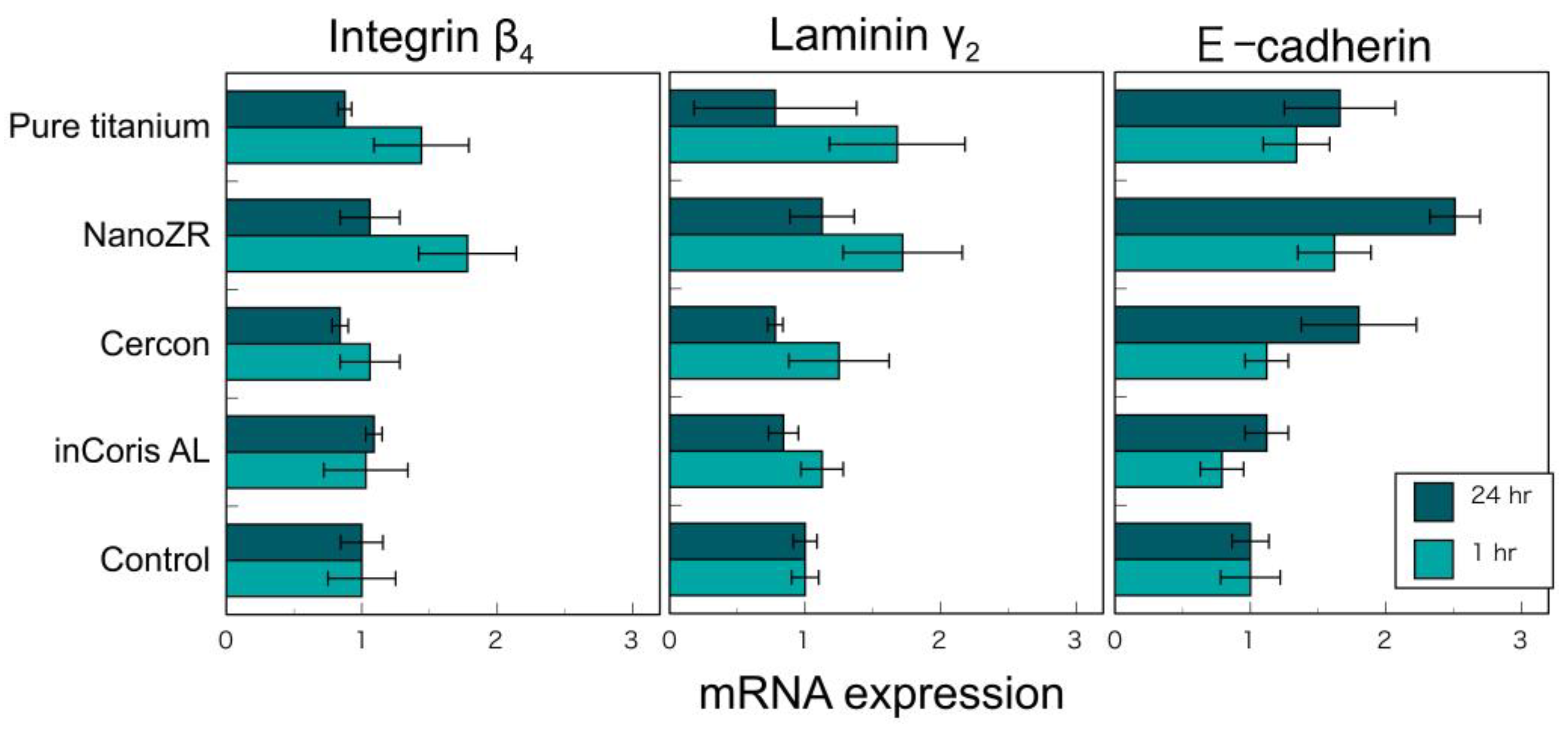
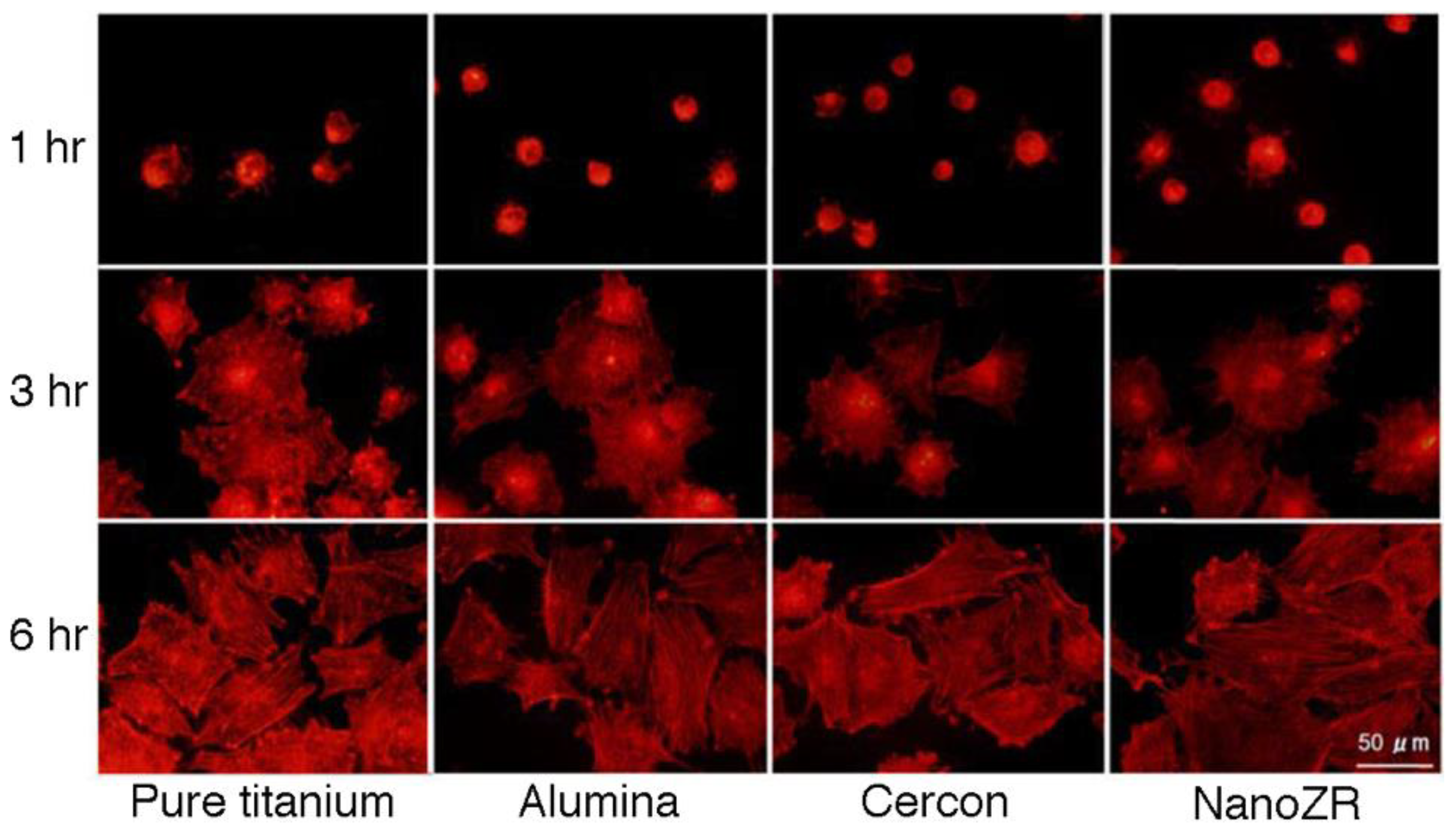
3.5.2. Adhesion of Soft Tissue
4. Surface Modification for Better Adhesion of Hard Tissue
4.1. Roughening
4.1.1. Sandblasting
4.1.2. Etching
4.1.3. Laser Irradiation
4.1.4. Sintering
4.2. Surface Activation
4.2.1. Ultraviolet Irradiation
4.2.2. Plasma Irradiation
4.3. Coating
4.3.1. Glass Coating
4.3.2. Apatite-Containing Glass Coating
4.3.3. Apatite Coating
5. Conclusions
- Dental zirconia continues to increase and is classified into 12 species in the yttria system alone. They are classified with yttria content, monochromatic/polychromatic, uniform/hybrid composition, and monolayer/multilayer.
- Higher yttria content zirconia has higher translucency and lower mechanical strength. Fracture strength of superstructures strongly depends on the strength on the occlusal contact region. Therefore, adequate zirconia should be selected as the superstructure crown, depending on whether strength or esthetics is prioritized.
- Low temperature degradation of dental zirconia decreased with yttria content, but even 3Y zirconia has a sufficient durability in oral condition.
- Although zirconia is the hardest dental materials, zirconia restoratives rarely wear the antagonist teeth when it is mirror polished.
- Zirconia has less bacterial adhesion and better soft tissue adhesion when it is mirror polished. Therefore, zirconia has advantageous for implant superstructures.
- Zirconia–alumina composites, such as ATZ and NanoZR, are adequate for implant fixtures because they have excellent mechanical strength in spite of insufficient esthetic properties.
- Zirconia is required for surface modification to obtain osseointegration to bone. Various surface treatments, such as roughening, surface activation, and coating, have been developed and improved.
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CSZ | Cubic-stabilized zirconia (almost 100% cubic phase) |
| PSZ | partially stabilized zirconia (mixture of cubic and tetragonal phase) |
| TZP | tetragonal zirconia polycrystal (almost 100% tetragonal phase) |
| 3Y-TZP | TZP stabilized with 3-mol% yttria |
| Ce-TZP | TZP stabilized with ceria |
| ATZ | alumina-toughened zirconia |
| ZTA | zirconia-toughened alumina |
| NanoZR | Ce-TZP/Al2O3 nanocomposite |
| 3Y-HA | conventional TZP stabilized with 3-mol% yttria and added with a relatively high content of alumina (0.25–0.5 wt%) |
| 3Y | high translucent TZP stabilized with 3-mol% yttria and added with a relatively low content of alumina (less than 0.05 wt%) |
| 4Y | high strength PSZ stabilized with 4-mol% yttria and added with a relatively low content of alumina (less than 0.05 wt%) |
| 5Y | high translucent PSZ stabilized with 5-mol% yttria and added with a relatively low content of alumina (less than 0.05 wt%) |
| 6Y | super high translucent PSZ stabilized with 6-mol% yttria and added with a relatively low content of alumina (less than 0.05 wt%) |
| M3Y | polychromatic multilayered 3Y |
| M4Y | polychromatic multilayered 4Y |
| M5Y | polychromatic multilayered 5Y |
| M6Y | polychromatic multilayered 6Y |
| M3Y-5Y | polychromatic multilayer with hybrid composition from 3Y to 5Y |
| M3Y-4Y | polychromatic multilayer with hybrid composition from 3Y to 4Y |
| M4Y-5Y | polychromatic multilayer with hybrid composition from 4Y to 5Y |
| LTD | low temperature degradation |
| HIP | hot isostatic press |
| CIM | ceramic injection molding |
References
- Piconi, C.; Maccauro, G. Zirconia as a ceramic biomaterial. Biomaterials 1999, 20, 1–25. [Google Scholar] [CrossRef]
- Chevalier, J. What future for zirconia as a biomaterial? Biomaterials 2006, 27, 535–543. [Google Scholar] [CrossRef]
- Ban, S. Properties of zirconia for realization of all-ceramic restoration. Shika Gakuho 2007, 107, 670–684. [Google Scholar]
- Miyazaki, T.; Nakamura, T.; Matsumura, H.; Ban, S.; Kobayashi, T. Current status of zirconia restoration. J. Prosthodont. Res. 2013, 57, 236–261. [Google Scholar] [CrossRef] [Green Version]
- Ban, S. Esthetic dental restorations taking advantage of zirconia characteristics. J. Jpn. Dent. Assoc. 2014, 67, 607–618. [Google Scholar]
- Ban, S. (Ed.) Types of Zirconia. In CAD/CAM Material Complete Guidebook; Ishiyaku Publishers: Tokyo, Japan, 2017; pp. 14–20. ISBN 978-4-263-46420-5. [Google Scholar]
- Nishihara, H.; Adanez, M.H.; Att, W. Current status of zirconia implants in dentistry: Preclinical tests. J. Prosthodont. Res. 2019, 63, 1–14. [Google Scholar] [CrossRef]
- Gross, C.; Bergfeldt, T.; Fretwurst, T.; Rothweiler, R.; Nelson, K.; Stricker, A. Elemental analysis of commercial zirconia dental implants—Is “metal free” devoid of metals? J. Mech. Behav. Biomed. Mater. 2020, 107, 103759. [Google Scholar] [CrossRef]
- Osman, R.B.; Swain, M.V. A critical review of dental implant materials with an emphasis on titanium versus zirconia. Materials 2015, 8, 932–958. [Google Scholar] [CrossRef] [Green Version]
- Cionca, N.; Hashim, D.; Mombelli, A. Two-piece zirconia implants supporting all-ceramic crowns: Six-year results of a prospective cohort study. Clin. Oral Implants Res. 2021, 32, 695–701. [Google Scholar] [CrossRef]
- Comisso, I.; Arias-Herrera, S.; Gupta, S. Zirconium dioxide implants as an alternative to titanium: A systematic review. J. Clin. Exp. Dent. 2021, 13, e511–e519. [Google Scholar] [CrossRef]
- Depprich, R.; Zipprich, H.; Ommerborn, M.; Naujoks, C.; Wiesmann, H.-P.; KiattaVorncharoen, S.; Lauer, H.-C.; Meyer, U.; Kübler, N.R.; Handschel, J. Osseointegration of zirconia implants compared with titanium: An in vivo study. Head Face Med. 2008, 4, 30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brånemark, P.-I.; Zarb, G.A.; Albrektsson, T. Tisue Integrated Prostheses. Osseointegration in Clinical Dentistry; Quintessence Publishing: Chicago, IL, USA, 1985. [Google Scholar]
- Listgarten, M.A. Soft and hard tissue response to endosseous dental implants. Anat. Rec. 1996, 245, 410–425. [Google Scholar] [CrossRef]
- Bosshardt, D.D.; Chappuis, V.; Buser, D. Osseointegration of titanium, titanium alloy and zirconia dental implants: Current knowledge and open questions. Periodontology 2000, 73, 22–40. [Google Scholar] [CrossRef]
- Ban, S. Material selection of implant superstructure in digital dentistry. J. Kyushu Dent. Soc. 2019, 72, 36–41. [Google Scholar]
- Straumann CARES Tooth Prosthetic Procedures: Basic Information. March 2017. Available online: https://www.straumann.com/content/dam/media-center/straumann/en/documents/brochure/technical-information/152.821-en_low.pdf (accessed on 23 July 2021).
- Affatato, S.; Torrecllas, R.; Taddel, P.; Rocchi, M.; Fagnano, C.; Ciapetti, G.; Toni, A. Advanced nanocomposite materials for orthopaedic applications. I. A long-term in vitro wear study of zirconia-toughened alumina. J. Biomed. Mater. Res. Part B 2006, 78, 76–82. [Google Scholar] [CrossRef]
- Kohal, R.-J.; Wolkewitz, M.; Mueller, C. Alumina-renforced zirconia implants: Survival rate and fracture strength in a masticatory simulation trial. Clin. Oral Implants Res. 2010, 21, 1345–1352. [Google Scholar] [CrossRef]
- Schierano, G.; Mussano, F.; Faga, M.G.; Menicucci, G.; Manzella, C.; Sabione, C.; Genova, T.; von Degerfeld, M.M.; Peirone, B.; Cassenti, A.; et al. An alumina toughened zirconia composite for dental implant application: In vivo animal results. BioMed Res. Int. 2015, 2015, 157360. [Google Scholar] [CrossRef] [Green Version]
- Busch, A.; Wassenaar, D.; Zinser, W.; Jäger, M. A bicentric approach evaluating the combination of a hemispheric cup with a novel ceramic head in total hip arthroplasty. Orthop. Rev. 2021, 13, 8794. [Google Scholar] [CrossRef]
- Zeramex® Family Image. Available online: https://www.zeramex.com/docs/de/medien_downloads/logos_bilder/zeramex_product_family.png (accessed on 23 July 2021).
- Nawa, M.; Nakamoto, S.; Sekino, T.; Niihara, K. Tough and strong Ce-TZP/alumina nanocomposites doped with titania. Ceram. Int. 1998, 24, 497–506. [Google Scholar] [CrossRef]
- Sato, H.; Yamada, K.; Pizzotti, G.; Nawa, M.; Ban, S. Mechanical properties of dental zirconia ceramics changed with sandblasting and heat treatment. Dent. Mater. J. 2008, 27, 408–414. [Google Scholar] [CrossRef] [Green Version]
- Ban, S.; Sato, H.; Suehiro, Y.; Nakanishi, H.; Nawa, M. Biaxial flexure strength and low temperature degradation of Ce-TZP/Al2O3 nanocomposite and Y-TZP as dental restoratives. J. Biomed. Mater. Res. B Appl. Biomater. 2008, 87B, 492–498. [Google Scholar] [CrossRef] [PubMed]
- Komasa, S.; Nishizaki, M.; Zhang, H.; Takao, S.; Yin, D.; Terada, C.; Kobayashi, Y.; Kusumoto, T.; Yoshimine, S.; Nishizaki, H.; et al. Osseointegration of alkali-modified NANOZR implants: An in vivo study. Int. J. Mol. Sci. 2019, 20, 842. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ban, S. Reliability and properties of core materials for all-ceramic dental restorations. Jpn. Dent. Sci. Rev. 2008, 44, 3–21. [Google Scholar] [CrossRef] [Green Version]
- Fujisaki, H.; Kawamura, K.; Imai, K. Translucent zirconia powder “Zpex” suitable to dental materials. Tosoh Res. Tech. Rev. 2012, 56, 57–61. [Google Scholar]
- Fujisaki, H.; Kawamura, K. Dental zirconia “Zpex” coloring grade and “Zpex Smile” with enhanced translucency. Tosoh Res. Tech. Rev. 2014, 58, 43–47. [Google Scholar]
- Ban, S. Evolution of dental zirconia and features of new high translucent multi-layer type. Dent. Diam. 2016, 41, 140–151. [Google Scholar]
- Amano, S.; Fujisaki, H.; Nagayama, H.; Azechi, S. Dental zirconia powder “Zpex4”. Tosoh Res. Tech. Rev. 2019, 63, 61–65. [Google Scholar]
- Okuda, Y.; Noda, M.; Kono, H.; Miyamoto, M.; Sato, H.; Ban, S. Radio-opacity of core materials for all-ceramic restorations. Dent. Mater. J. 2010, 29, 35–40. [Google Scholar]
- Belli, R.; Hurle, K.; Schürrlen, J.; Petschelt, A.; Werbach, K.; Peterlik, H.; Rabe, T.; Mieller, B.; Lohbauer, U. A revised relationship between fracture toughness and Y2O3 content in modern dental zirconias. ChemRxiv 2021, 1–23. [Google Scholar] [CrossRef]
- Bethke, A.; Pieralli, S.; Kohal, R.-J.; Burkhardt, F.; von Stein-Lausnitz, M.; Vach, K.; Spies, B.C. Fracture resistance of zirconia oral implants in vitro: A systematic review and meta-analysis. Materials 2020, 13, 562. [Google Scholar] [CrossRef] [Green Version]
- Kohal, R.-J.; Klaus, G.; Strub, J.R. Zirconia-implant-supported all-ceramic crowns withstand long-term load: A pilot investigation. Clin. Oral Implants Res. 2006, 17, 565–571. [Google Scholar] [CrossRef]
- Kohal, R.-J.; Christian, H.; Klaus, G. Stability of prototype two-piece zirconia and titanium implants after artificial aging: An in vitro pilot study. Clin. Implant Dent. Relat. Res. 2009, 11, 323–329. [Google Scholar] [CrossRef]
- Chang, C.-L.; Chen, C.-S.; Yeung, T.C.; Hsu, M.-L. Biomechanical effect of a zirconia dental implant-crown system: A three-dimensional finite element analysis. Int. J. Oral Maxillofac. Implants 2012, 27, e49–e57. [Google Scholar]
- Ban, S. CAD/CAM material as an implant superstructure. In Proceedings of the 6th Information Exchange Meeting of Academy of Dental Digital Design, Tokyo, Japan, 21 October 2018. [Google Scholar]
- Okamura, M.; Shimidzu, H.; Masumi, S.; Ban, S. Fracture strength of ceramic abutments made of two lithium disilicates and a zirconia. In Proceedings of the 38th Asia Pacific Dental Congress, Hong Kong, China, 17–19 June 2016. [Google Scholar]
- Okamura, M.; Kawano, T.; Shimidzu, H.; Masumi, S. Evaluation of fracture strength reliability in three types of ceramic implant abutments. In Proceedings of the Japan Prosthodontic Society Kyushu Branch and Chugoku-Shikoku Branch Joint Academic Meeting, Kumamoto, Japan, 9 September 2016. [Google Scholar]
- Rohr, N.; Märtin, S.; Fischer, J. Correlations between fracture load of zirconia implant supported single crowns and mechanical properties of restorative material and cement. Dent. Mater. J. 2018, 37, 222–228. [Google Scholar] [CrossRef] [Green Version]
- El-S’adany, A.F.; Masoud, G.E.; Kamel, M.S.; Korsel, A.M. Fracture resistance of all ceramic crowns supported by zirconia and alumina versus titanium implant abutments. Tanta Dent. J. 2013, 10, 103–111. [Google Scholar] [CrossRef] [Green Version]
- Lawson, S. Environmental degradation of zirconia ceramics. J. Euro-Ceram. Soc. 1995, 15, 485–502. [Google Scholar] [CrossRef]
- Ban, S. Chemical durability of high translucent dental zirconia. Dent. Mater. J. 2020, 39, 12–23. [Google Scholar] [CrossRef] [Green Version]
- Noda, M.; Okuda, Y.; Arikawa, H.; Kanie, T.; Fujii, K.; Ban, S. Acid resistance of zirconia. J. Dent. Mater. 2009, 28, 114. [Google Scholar]
- Iwata, J.; Uematsu, Y.; Tomino, M.; Tsuruta, S.; Hayashi, T.; Kawai, T.; Ban, S. Chemical durability of CAD/CAM dental materials. J. Dent. Mater. 2015, 34, 315. [Google Scholar]
- Ban, S.; Iwata, J.; Okada, R.; Asakura, M.; Kawai, T. Chemical durability of dental glass ceramics. J. Dent. Mater. 2016, 35, 122. [Google Scholar]
- Wiederhorn, S.M.; Bolz, L.H. Stress corrosion and static fatigue of glass. J. Am. Ceram. Soc. 1970, 53, 543–548. [Google Scholar] [CrossRef]
- Michalske, T.A.; Freiman, S.W. A molecular mechanism for stress corrosion in vitreous silica. J. Am. Ceram. Soc. 1983, 66, 284–288. [Google Scholar] [CrossRef]
- Harada, A.; Ban, S.; Matsuura, M.; Kato, N.; Watanabe, K.; Koyama, K.; Takada, A.; Iwase, H.; Hasegawa, J. Factors affecting on the flexure strength of dental porcelains. Surface finish and measurement environment. J. Dent. Mater. 1994, 13, 170–171. [Google Scholar]
- Ban, S.; Harada, A.; Hasegawa, J. Effect of glazing on the bi-axial flexure strength of dental porcelains. In Microstructures and Mechanical Properties of New Engineering Materials; Xu, B., Tokuda, M., Song, J., Eds.; International Academic Publishers: Beijing, China, 1995; pp. 3–8. [Google Scholar]
- Hattori, M.; Ban, S.; Hasegawa, J. Biaxial flexure strength—Effect of test environment. J. Dent. Mater. 1997, 16, 109. [Google Scholar]
- Ban, S.; Iwata, J.; Asakura, M.; Kawai, T. Biaxial flexural strengths of pressed glass ceramics. J. Dent. Mater. 2017, 36, 68. [Google Scholar]
- Mair LH: Wear in dentistry-current terminology. J. Dent. 1992, 20, 140–144. [CrossRef]
- Ban, S. Polishing of zirconia full-contour restoratives and wear of opposing teeth. QDT 2012, 37, 26–40. [Google Scholar]
- Jung, Y.-S.; Lee, J.-W.; Choi, Y.-J.; Ahn, J.-S.; Shin, S.-W.; Huh, J.-B. A study on the in-vitro wear of the natural tooth structure by opposing zirconia or dental porcelain. J. Adv. Prosthodont. 2010, 2, 1111–1115. [Google Scholar] [CrossRef] [Green Version]
- Albashaireh, Z.S.M.; Ghazal, M.; Kern, M. Two-body wear of different ceramic materials opposed to zirconia ceramic. J. Prosthet. Dent. 2010, 104, 105–113. [Google Scholar] [CrossRef]
- Janyavula, S.; Lawson, N.; Cakir, D.; Beck, P.; Ramp, L.; Burgess, J. The wear of polished and glazed zirconia against enamel. J. Prosthet. Dent. 2013, 109, 22–29. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Özcan, M.; Scmutz, F.; Trottmann, A.; Roos, M.; Hämmerle, F. Two-body wear of monolithic, veneered and glazed zirconia and their corresponding enamel antagonists. Acta Odontol. Scand. 2013, 71, 2013. [Google Scholar] [CrossRef] [Green Version]
- Sakakibara, T.; Jimbo, R.; Ban, S.; Kawai, T.; Murakami, H. Abrasion of enamel against mirror polished zirconia. In Proceedings of the 29th Annual Meeting Academy of Osseointegration, Seattle, DC, USA, 7 March 2014. [Google Scholar]
- Ban, S.; Iwata, J.; Okada, R.; Sakakibara, T.; Mieki, A.; Kataoka, H.; Kurita, S.; Kawai, T. Wear performance of dental zirconia in comparison to lithium disilicate. In Proceedings of the 38th Asia Pacific Dental Congress, Hong Kong, China, 17–19 June 2016. [Google Scholar]
- Ban, S. Think of common sense of zirconia restoration vol.2. Pract. Prosthodont. 2019, 52, 140–152. [Google Scholar]
- Scarano, A.; Piattelli, M.; Caputi, S.; Favero, G.A.; Piattelli, A. Bacterial adhesion on commercially pure titanium and zirconium oxide disks: An in vivo human study. J. Periodontol. 2004, 75, 292–296. [Google Scholar] [CrossRef]
- Degidi, M.; Artese, L.; Scarano, A.; Perrotti, V.; Gehrke, P.; Piattelli, A. Inflammatory infiltrate, micro vessel density, nitric oxide synthase expression, vascular endothelial growth factor expression, and proliferative activity in peri-implant soft tissues around titanium and zirconium oxide healing caps. J. Periodontol. 2006, 77, 73–80. [Google Scholar] [CrossRef]
- Nakamura, K. Zirconia as a dental implant abutment material: A systematic review. Int. J. Prosthodont. 2010, 23, 299–309. [Google Scholar]
- Roehling, S.; Astasov-Frauenhoffer, M.; Hauser-Gerspach, I.; Braissant, O.; Woelfer, H.; Waltimo, T.; Kniha, H.; Gahlert, M. In vitro biofilm formation on titanium and zirconia implant surface. J. Periodontol. 2017, 88, 298–307. [Google Scholar] [CrossRef]
- Nakazato, G.; Tuchiya, H.; Sato, M.; Yamaguchi, M. In vitro plaque formation on implant materials. Int. J. Oral Maxillofac. Implants 1989, 4, 321–326. [Google Scholar]
- Ban, S. Think of common sense of zirconia restoration Vol.9. Pract. Prosthodont. 2020, 53, 275–285. [Google Scholar]
- Okabe, E.; Ishihara, Y.; Kikuchi, T.; Izawa, A.; Kobayashi, S.; Goto, H.; Komiya, Y.; Sasaki, K.; Ban, S.; Noguchi, T.; et al. Adhesion properties of human oral epithelial-derived cells to zirconia. Clin. Implants Dent. Relat. Res. 2016, 18, 906–916. [Google Scholar] [CrossRef]
- van Brakel, R.; Meijer, G.J.; Verhoeven, J.W.; Jansen, J.; de Putter, C.; Cune, M.S. Soft tissue response to zirconia and titanium implant abutments: An in vivo within-subject comparison. J. Clin. Periodont. 2012, 39, 995–1001. [Google Scholar] [CrossRef]
- Yamano, S.; Ma, K.-Y.A.; Ahanti, R.M.; Kim, S.-W.; Wada, K.; Sukotjo, C. The influence of different implant materials on human gingival fibroblast morphology, proliferation, and gene expression. Int. J. Oral Maxillofac. Implants 2011, 26, 1247–1255. [Google Scholar]
- Ban, S. Surface modification of zirconia as hard tissue alternative material. J. Jpn. Soc. Biomater. 2016, 34, 62–65. [Google Scholar]
- Karthigeyan, S.; Ravindran, A.J.; Bhat, R.T.B.; Nageshwarao, M.N.; Murugesan, S.V.; Angamuthu, V. Surface Modification Techniques for Zirconia-Based Bioceramics: A Review. J. Pharm. Bioallied Sci. 2019, 11 (Suppl. 2), S131–S134. [Google Scholar]
- Liu, Y.; Rath, B.; Tingart, M.; Eschweiler, J. Role of implants surface modification in osseointegration: A systematic review. J. Biomed. Mater. Res. 2020, 108A, 470–484. [Google Scholar] [CrossRef] [Green Version]
- Cerroni, L. Ceramics for Dentistry: Coomercial devices and their clinical analysis. In Advances in Ceramic Biomaterials, 1st ed.; Palmero, P., De Barra, E., Cambier, F., Eds.; Woodhead Publishing: Cambridge, UK, 2017; pp. 181–248. ISBN 13978-0081008812. [Google Scholar]
- Straumann PURE Ceramic Implant System Basic Information on the Surgical and Prosthetic Procedures: Technical Information. December 2019. Available online: https://www.straumann.com/content/dam/media-center/straumann/en-us/documents/brochure/product-information/USLIT.1194.PURE.Ceramic.Implant.System.pdf (accessed on 15 August 2021).
- Yamashita, D.; Machigashira, M.; Miyamoto, M.; Takeuchi, H.; Noguchi, K.; Izumi, Y.; Ban, S. Effect of surface roughness on initial responses of osteoblast-like cells on two types of zirconia. Dent. Mater. J. 2009, 28, 461–470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Warashina, H.; Sakano, S.; Kitamura, S.; Yamauchi, K.; Yamaguchi, J.; Ishiguro, N.; Hasegawa, Y. Biological reaction to alumina, zirconia, titanium and polyethylene particles implanted onto murine calvaria. Biomaterials 2003, 24, 3655–3661. [Google Scholar] [CrossRef]
- Kohal, R.J.; Weng, D.; Bächle, M.; Strub, J.R. Load custom-made zirconia and titanium implants show similar osseointegration: An animal experiment. J. Periodontol. 2004, 75, 1262–1268. [Google Scholar] [CrossRef]
- Ko, H.C.; Han, J.S.; Bächle, M.; Jang, J.H.; Shin, S.W.; Kim, D.J. Initial osteoblast-like cell response to pure titanium and zirconia/alumina ceramics. Dent. Mater. 2007, 23, 1349–1355. [Google Scholar] [CrossRef]
- Oliva, J.; Oliva, X.; Oliva, J.D. Five-year success rate of 831 consecutively placed Zirconia dental implants in humans: A comparison of three different rough surfaces. Intern. J. Oral Maxillofac. Implants 2010, 25, 336–344. [Google Scholar]
- Fischer, J.; Schott, A.; Märtin, S. Surface micro-structuring of zirconia dental implants. Clin. Oral Implants Res. 2016, 27, 162–166. [Google Scholar] [CrossRef]
- Bachle, M.; Butz, F.; Hubner, U.; Bakalinis, E.; Kohal, R.J. Behavior of CAL72 osteoblast-like cells cultured on zirconia ceramics with different surface topographies. Clin. Oral Implants Res. 2007, 18, 53–59. [Google Scholar] [CrossRef]
- Gahlert, M.; Rohling, S.; Wieland, M.; Sprecher, C.M.; Kniha, H.; Milz, S. Osseointegration of zirconia and titanium dental implants: A histological and histomorphometrical study in the maxilla of pigs. Cin. Oral Implants Res. 2009, 20, 1247–1253. [Google Scholar] [CrossRef]
- Noda, M.; Okuda, Y.; Tsuruki, J.; Minesaki, Y.; Takenouchi, Y.; Ban, S. Surface damages of zirconia by Nd: YAG dental laser irradiation. Dent. Mater. J. 2010, 29, 536–541. [Google Scholar] [CrossRef] [Green Version]
- Hao, L.; Lawrence, J.; Chian, K.S. Osteoblast cell adhesion on a laser modified zirconia based bioceramic. J. Mater. Sci. Mater. Med. 2005, 16, 719–726. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Ruiz, R.A.; Calvo-Guirado, J.L.; Morena, P.; Guardia, J.; Gomez-Moreno, G.; Mate-Sánchez, J.E.; Ramirez-Fernández, P.; Chiva, F. Femtosecond laser microstructuring of zirconia dental implants. J. Biomed. Mater. Res. Part B Appl. Biomater. 2011, 96B, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Daskalova, A.; Angelova, L.; Carvalho, A.; Trifonov, A.; Nathala, C.; Monteiro, F.; Buchvarov, I. Effect of surface modification by femtosecond laser on zirconia based ceramics for screening of cell-surface interaction. Appl. Surf. Sci. 2020, 513, 145914. [Google Scholar] [CrossRef]
- Sennerby, L.; Dasmah, A.; Larsson, B.; Iverhed, M. Bone tissue responses to surface-modified zirconia implants: A histomorphometric and removal torque study in the rabbit. Clin. Implants Dent. Relat. Res. 2005, 7, S13–S20. [Google Scholar] [CrossRef]
- Kohal, R.J.; Wolkewitz, M.; Hinze, M.; Han, J.-S.; Bächle, M.; Butz, F. Biochemical and histological behavior of zirconia implants: An experiment in the rat. Clin. Oral. Implants Res. 2009, 20, 333–339. [Google Scholar] [CrossRef]
- Setzer, B.; Bächle, M.; Metzger, M.C.; Kohal, R.J. The gene-expression and phenotypic response of hFOB 1.19 osteoblasts to surface-modified titanium and zirconia. Biomaterials 2009, 30, 979–990. [Google Scholar] [CrossRef]
- Altmann, B.; Kohal, R.J.; Steinberg, T.; Tomakidi, P.; Bächle-Haas, M.; Wennerberg, A.; Att, W. Distinct cell functions of osteoblasts on UV-functionalized titanium- and zirconia-based implant materials are modulated by surface topography. Tissue Eng. Part C 2013, 19, 850–863. [Google Scholar] [CrossRef] [Green Version]
- Al Qahtani, M.S.A.; Wu, Y.; Spintzyk, S.; Krieg, P.; Killinger, A.; Schwizer, E.; Stephan, I.; Scheideler, L.; Geis-Gerstorfer, J.; Rupp, F. UV-A and UV-C light induced hydrophillization of dental implants. Dent. Mater. 2015, 31, e157–e167. [Google Scholar] [CrossRef]
- Chu, P.K.; Chen, J.Y.; Wang, L.P.; Huang, N. Plasma-surface modification of biomaterials. Mater. Sci. Eng. 2002, R36, 143–206. [Google Scholar] [CrossRef] [Green Version]
- Yoshinari, M. Future prospects of zirconia for oral implants—A review. Dent. Mater. J. 2020, 39, 37–45. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.-W.; Kong, Y.-M.; Bae, C.-J.; Noh, Y.-J.; Kim, H.-E. Sol-gel derived fluor-hydroxyapatite biocoatings on zirconia substrate. Biomaterials 2004, 25, 2919–2926. [Google Scholar] [CrossRef]
- Kim, H.-W.; Georgiou, G.; Knowles, J.C.; Koh, Y.-H.; Kim, H.-E. Calcium phosphates and glass composite coating on zirconia for enhanced biocompatibility. Biomaterials 2004, 25, 4203–4213. [Google Scholar] [CrossRef]
- Ferraris, M.; Verné, E.; Appendino, P.; Moisescu, C.; Krajewski, A.; Ravaglioli, A. Coatings on zirconia for medical applications. Biomaterials 2000, 21, 765–773. [Google Scholar] [CrossRef]
- Noda, M.; Okuda, Y.; Tsuruki, J.; Miyamoto, M.; Ban, S. Apatite forming ability in vitro of HA-containing glass powder for coating on zirconia. In Proceeding of the International Dental Materials Congress 2011, Seoul, Korea, 27–29 May 2011; p. 273. [Google Scholar]
- Yamashita, D.; Noda, M.; Machigashira, M.; Miyamoto, M.; Takeuchi, H.; Takeuchi, N.; Kono, H.; Noguchi, K.; Ban, S. In Vitro evaluation of hydroxyapatite-containing glass coating on zirconia. Key Eng. Mater. 2012, 493, 7–10. [Google Scholar] [CrossRef]
- Yoshihara, K.; Ban, S.; Kawai, T.; Tanaka, T. Reaction of dental zirconia with phosphate-bonded investments for heat pressing technique. Key Eng. Mater. 2013, 529, 537–542. [Google Scholar] [CrossRef]
- Ban, S.; Okuda, Y.; Noda, M.; Tsuruki, J.; Kawai, T.; Kono, H. Contamination of dental zirconia before final firing: Effects on mechanical strength. Dent. Mater. J. 2013, 32, 1011–1019. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uchida, M.; Kim, H.-M.; Kokubo, T.; Nawa, M.; Asano, T.; Tanaka, K.; Nakamura, T. Apatite-forming ability of a zirconia/alumina nano-composite induced by chemical treatment. J. Biomed. Mater. Res. 2002, 60, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, K.; Hayashi, T.; Asakura, M.; Ando, M.; Kawai, T.; Ban, S. Improving biocompatibility of zirconia surface by incorporating Ca ions. Dent. Mater. J. 2015, 34, 336–344. [Google Scholar] [CrossRef] [PubMed] [Green Version]






| Basic Grades | S Grades | High Translucent Grades | ||||
|---|---|---|---|---|---|---|
| TZ-3YB-E® | TZ-3YSB-E® | Zpex® | Zpex 4® | Zpex Smile® | ||
| Powder characteristics | ||||||
| Y2O3 | mol% | 3 | 3 | 3 | 3.9 | 5.3 |
| wt% | 5.2 ± 0.5 | 5.2 ± 0.5 | 5.35 ± 0.2 | 6.9 | 9.35 | |
| Al2O3 (wt%) | 0.25 | 0.25 | 0.05 | 0.05 | 0.05 | |
| Actual particle size (nm) | 40 | 90 | 40 | 90 | 90 | |
| Crystallite size(nm) | 27 | 36 | 36 | 36 | 36 | |
| density (g/cm3) | 1.1 | 1.2 | 1.2 | 1.25 | 1.2 | |
| Specific surface area (m2/g) | 16 | 7 ± 2 | 13 ± 2 | 10 | 10 | |
| Typical properties of sintered body | ||||||
| Green density (g/cm3) | 3.04 | 3.14 | 3.22 | 3.28 | 3.27 | |
| Sintered temperature (°C) | 1350 | 1450 | 1400 | 1500 | 1450 | |
| Sintered density (g/cm3) | 6.06 | 6.05 | 6.08 | 6.07 | 6.04 | |
| 3-P Bending strength (MPa) | 1200 | 1200 | 1100 | 1100 | 600 | |
| Fracture toughness (MPa·m0.5) | 5 | 5 | 5 | - | 2.4 | |
| Hardness (Hv10) | 1250 | 1250 | 1250 | 1250 | 1250 | |
| Transmittance (%) | 17 | 35 | 41 | 45 | 49 | |
| (1) Monochromic and uniform composition | ||
| Group | Name | Manufacturer |
| ATZ | ATZ Bio-HIP | Metoxit AG (Switzerland) |
| NanoZR | Nanozirconia | Yamakin Co. Ltd. (Japan) |
| HIP 3Y-HA | TZP-A Bio-HIP | Metoxit AG (Switzerland) |
| 3Y-HA | Cercon base | Dentsply Sirona (USA) |
| inCoris Zi | Dentsply Sirona (USA) | |
| Vita YZ T | Vita Zahnfabrik H. Rauter GmbH & Co. KG (Germany) | |
| Aadva ST | GC Corp. (Japan) | |
| ceramill zi | Amann Girrbach AG (Austria) | |
| DD Bio Z | Dental Direkt GmbH (Germany) | |
| Z-CAD HD | Metoxit AG (Switzerland) | |
| Copran Zri | Whitepeaks Dental Solutions GmbH & Co. KG (Germany) | |
| dima Mill Zirconia ST | Kulzer GmbH (Germany) | |
| 3Y | Cercon ht | Dentsply Sirona (USA) |
| Vita YZ HT | Vita Zahnfabrik H. Rauter GmbH & Co. KG (Germany) | |
| Aadva EI | GC Corp. (Japan) | |
| ceramill zolid | Amann Girrbach AG (Austria) | |
| inCoris TZI | Dentsply Sirona (USA) | |
| DD Bio ZX2 | Dental Direkt GmbH (Germany) | |
| Z-CAD HTL | Metoxit AG (Switzerland) | |
| IPS e.max ZirCAD MO/LT | Ivoclar Vivadent AG (Lichtenstein) | |
| 4Y | Katana Zirconia HT | Kuraray Noritake Dental Inc. (Japan) |
| ceramill zolid HT+ | Amann Girrbach AG (Austria) | |
| DDcube ONE | Dental Direkt GmbH (Germany) | |
| Z-CAD One4All | Metoxit AG (Switzerland) | |
| CopraSupreme | Whitepeaks Dental Solutions GmbH & Co. KG (Germany) | |
| IPS e.max ZirCAD MT | Ivoclar Vivadent AG (Lichtenstein) | |
| Vita YZ ST | Vita Zahnfabrik H. Rauter GmbH & Co. KG (Germany) | |
| 5Y | Aadva NT | GC Corp. (Japan) |
| Prettau Anterior | Zirkonzahn GmbH (Italy) | |
| DD cube X2 | Dental Direkt GmbH (Germany) | |
| Vita YZ XT | Vita Zahnfabrik H. Rauter GmbH & Co. KG (Germany) | |
| Z-CAD Smile | Metoxit AG (Switzerland) | |
| CopraSmile | Whitepeaks Dental Solutions GmbH & Co. KG (Germany) | |
| Ceramill zolid fx | Amann Girrbach AG (Austria) | |
| Cercon xt | Dentsply Sirona (USA) | |
| 6Y | Katana Zirconia UT | Kuraray Noritake Dental Inc. (Japan) |
| (2) Polychromic multilayer and uniform composition | ||
| Group | Name | Manufacturer |
| M3Y | Dima Mill Zirconia ML | Kulzer GmbH (Germany) |
| Nacera Pearl Multi-Shade | Doceram Medical Ceramics GmbH (Germany) | |
| Prettau 2 Dispersive | Zirkonzahn GmbH (Italy) | |
| M4Y | Katana Zirconia ML | Kuraray Noritake Dental Inc. (Japan) |
| Z-CAD One4All Multi | Metoxit AG (Switzerland) | |
| DDcube ONE ML | Dental Direkt GmbH (Germany) | |
| Vita YZ ST Multicolor | Vita Zahnfabrik H. Rauter GmbH & Co. KG (Germany) | |
| Ceramill zolid gen-x | Amann Girrbach AG (Austria) | |
| CopraSupreme Symphony | Whitepeaks Dental Solutions GmbH & Co. KG (Germany) | |
| Shofu Block Zr Lucent CEREC | Shofu Inc./Adamant Namiki (Japan) | |
| M5Y | Katana Zirconia Block STML | Kuraray Noritake Dental Inc. (Japan) |
| Z-CAD Smile Multi | Metoxit AG (Switzerland) | |
| DD cube X2 ML | Dental Direkt GmbH (Germany) | |
| Ceramill zolid fx multilayer | Amann Girrbach AG (Austria) | |
| Cercon xt ML | Dentsply Sirona (USA) | |
| CopraSmile Symphony | Whitepeaks Dental Solutions GmbH & Co. KG (Germany) | |
| Vita YZ XT Multicolor | Vita Zahnfabrik H. Rauter GmbH & Co. KG (Germany) | |
| Prettau 4 Anterior Dispersive | Zirkonzahn GmbH (Italy) | |
| Lucent FA | Shofu Inc./Adamant Namiki (Japan) | |
| M6Y | Katana Zirconia UTML | Kuraray Noritake Dental Inc. (Japan) |
| Nacera Pearl Q3 Multi-Shade | Doceram Medical Ceramics GmbH (Germany) | |
| (3) Polychromic multilayer and hybrid composition | ||
| Group | Name | Manufacturer |
| M3Y-5Y | IPS e.max ZirCAD Prime | Ivoclar Vivadent AG (Lichtenstein) |
| Prettau 3 Dispersive | Zirkonzahn GmbH (Italy) | |
| Tanaka Enamel ZR Multi 5 | ATD Japan Co., Ltd. (Japan) | |
| Zivino | Yoshida Dental Co., Ltd./Adamant Namiki (Japan) | |
| Lucent Supra | Shofu Inc./Adamant Namiki (Japan) | |
| M3Y-4Y | Sakura Zirconia | Straumann Japan/Adamant Namiki (Japan) |
| M4Y-5Y | CopraSupreme Hyperion | Whitepeaks Dental Solutions GmbH & Co. KG (Germany) |
| IPS e.max ZirCAD MT Multi | Ivoclar Vivadent AG (Lichtenstein) | |
| Manufacturer | Brand Name | Material | Design | Surface Treatment |
|---|---|---|---|---|
| CeraRoot SL (Barcelona, Spain) | CeraRoot | 3Y-HA (Toso TZ-3YB-E) | One-piece | Acid etching (ICE surface) |
| Z-systems AG (Stuttgart, Germany) | Zirkolith Z5m | TZP-A Bio-HIP (HIP TZP) | One-piece | Sandblasting + Laser irradiation |
| Zirkolith Z5c | Two-piece (cementation) | |||
| Zirkolith Z5BL | Two-piece (ceramic screw) | |||
| METOXIT dental (Thayngen, Switzerland) | TZP-A Bio-HIP | Ziraldent HIP TZP | Two-piece | Sandblasting + Zirconia-slurry coating and firing (ZircaPore) |
| ATZ Bio-HIP | Ziraldent HIP ATZ | |||
| bredent medical (Senden, Germany) | whiteSKY Tissue Line | Y-TZP | One-piece | Sandblasting |
| Ziterion (Uffenheim, Germany) | Zit-vario | Y-TZP | Two-piece | Sandblasting |
| Dentalpoint AG (Zurich, Switzerland) | ZERAMEX T | HIP TZP | Two-piece (carbon fiber-reinforced polymer screw) | Sandblasting + Acid etching (Zerafil) |
| ZERAMEX P | ATZ | |||
| ZERAMEX XT | ||||
| Incermed (Lausanne, Switzerland) | Sigma | HIP TZP | Two-piece | Sandblasting |
| AXIS biodent/Camlog (Les Bois, Switzerland) | Hexalobe | Y-TZP + PEEK | Two-piece | CIM (Ceramic Injection Molding) |
| Monobloc | Y-TZP | One-piece | ||
| Straumann (Basel, Switzerland) | PURE Ceramic Implant | HIP TZP | One-piece | Sandblasting + Acid etching (ZLA) |
| SNOW Ceramic Implant (Z-systems AG) | Two-piece (Ti or ceramic screw) | Sandblasting + Laser irradiation | ||
| Nobel Biocare | Nobel Pearl (Dentalpoint AG) | ATZ | Two-piece (carbon fiber-reinforced polymer screw) | Sandblasting + Acid etching (Zerafil) |
| VITA Zahnfabrik | Ceramic Implant | Y-TZP | One-piece | Sandblasting + Acid etching + Heat treatment |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ban, S. Classification and Properties of Dental Zirconia as Implant Fixtures and Superstructures. Materials 2021, 14, 4879. https://doi.org/10.3390/ma14174879
Ban S. Classification and Properties of Dental Zirconia as Implant Fixtures and Superstructures. Materials. 2021; 14(17):4879. https://doi.org/10.3390/ma14174879
Chicago/Turabian StyleBan, Seiji. 2021. "Classification and Properties of Dental Zirconia as Implant Fixtures and Superstructures" Materials 14, no. 17: 4879. https://doi.org/10.3390/ma14174879
APA StyleBan, S. (2021). Classification and Properties of Dental Zirconia as Implant Fixtures and Superstructures. Materials, 14(17), 4879. https://doi.org/10.3390/ma14174879





