In Vitro Study on the Adhesive Performance of Some Resin-Based Materials Used to Restore Class II Cavities
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics and Study Design
2.2. Resin Composites and Adhesive Systems
2.3. Tooth Restoration and Preparation of Study Groups
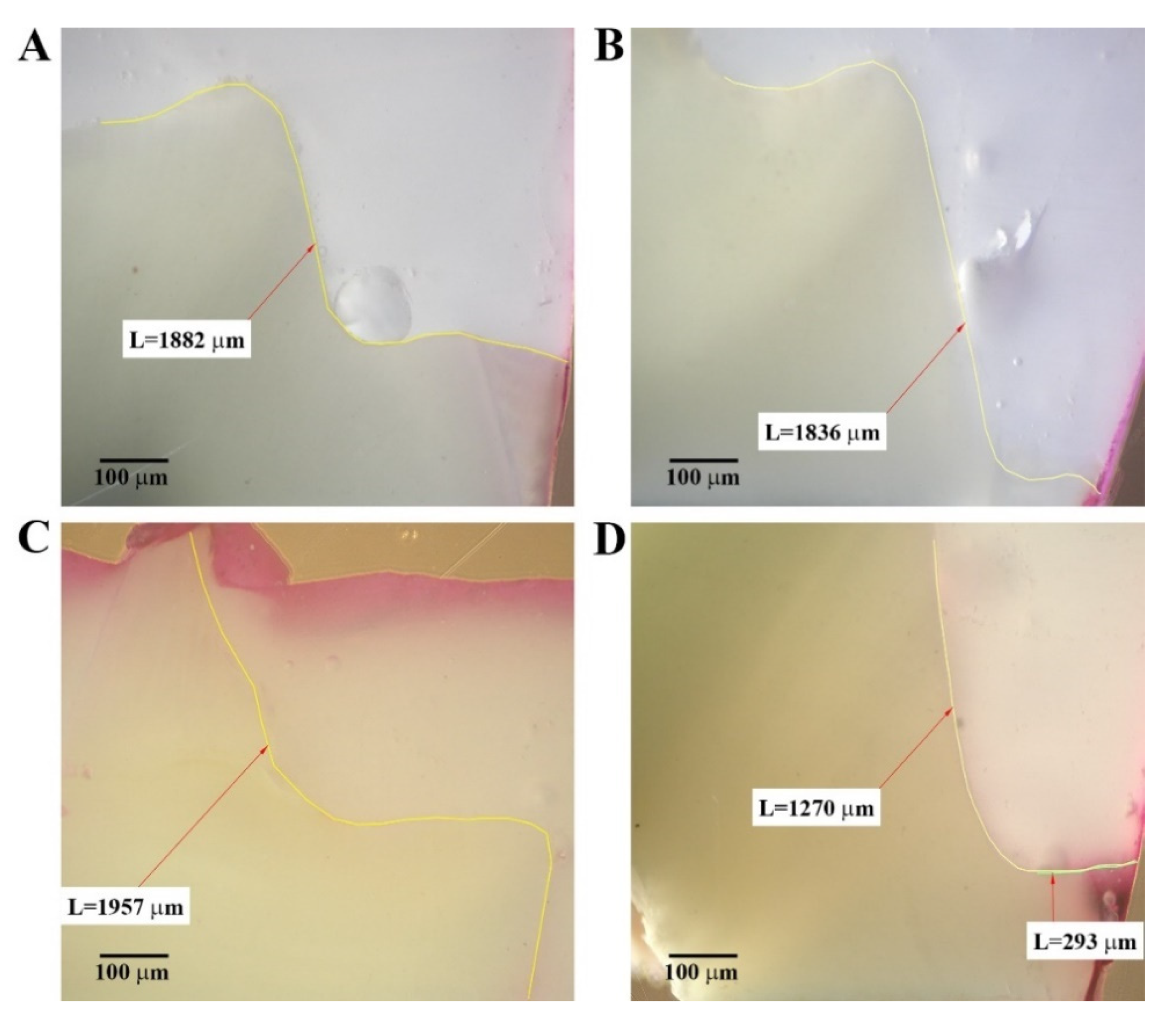
2.4. Microleakage Test
2.5. Data Analysis
3. Results
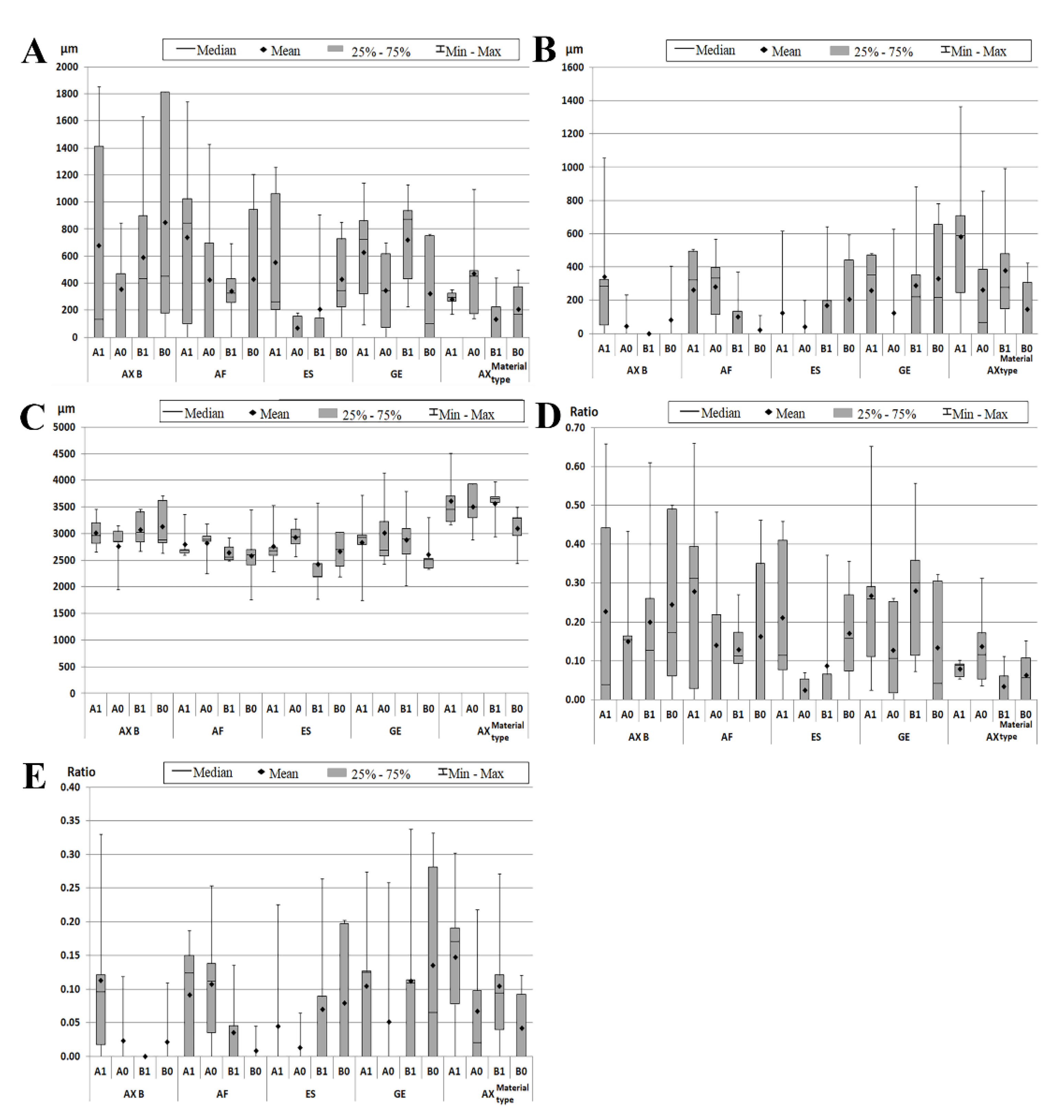
3.1. Microleakage Measurements
3.2. Total Adhesive Interface Measurements
3.3. The Microleakage Ratio
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Amaireh, A.I.; Al-Jundi, S.H.; Alshraideh, H.A. In vitro evaluation of microleakage in primary teeth restored with three adhesive materials: ACTIVA™, composite resin, and resin-modified glass ionomer. Eur. Arch. Paediatr. Dent. 2019, 20, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.D.; Ilie, N.; Hickel, R.; Reis, A.; Loguercio, A.; Rousson, V. Laboratory mechanical parameters of composite resins and their relation to fractures and wear in clinical trials-a systematic review. Dent. Mater. 2017, 33, e101–e114. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.D.; Rousson, V. Clinical effectiveness of direct class II restorations—A meta-analysis. J. Adhes. Dent. 2012, 14, 407–431. [Google Scholar] [PubMed]
- Behery, H.; El-Mowafy, O.; El-Badrawy, W.; Nabih, S.; Saleh, B. Gingival microleakage of class II bulk-fill composite resin restorations. Dent. Med. Probl. 2018, 55, 383–388. [Google Scholar] [CrossRef]
- Alani, A.H.; Toh, C.G. Detection of microleakage around dental restorations: A review. Oper. Dent. 1997, 22, 173–185. [Google Scholar]
- Hilton, T.J.; Schwartz, R.S.; Ferracane, J.L. Microleakage of four class II resin composite insertion techniques at intraoral temperature. Quintessence Int. 1997, 28, 135–144. [Google Scholar]
- Sudhapalli, S.K.; Sudhapalli, S.; Razdan, R.A.; Singh, V.; Bhasin, A. A comparative evaluation of microleakage among newer composite materials: An in vitro study. Contemp. Clin. Dent. 2018, 9, 587–591. [Google Scholar] [CrossRef]
- Mitra, S.B.; Wu, D.; Holmes, B.N. An application of nanotechnology in advanced dental materials. J. Am. Dent. Assoc. 2003, 134, 1382–1390. [Google Scholar] [CrossRef]
- Tomaszewska, I.M.; Kearns, J.O.; Ilie, N.; Fleming, G.J.P. Bulk fillrestoratives: To cap or not to cap—That is the question? J. Dent. 2015, 43, 309–316. [Google Scholar] [CrossRef]
- Politi, I.; McHugh, L.E.J.; Al-Fodeh, R.S.; Fleming, G.J.P. Modification of the restoration protocol for resin-based composite (RBC) restoratives (conventional and bulk fill) on cuspal movement and microleakage score in molar teeth. Dent. Mater. 2018, 34, 1271–1277. [Google Scholar] [CrossRef]
- Kalra, S.; Singh, A.; Gupta, M.; Chadha, V. Ormocer: An aesthetic direct restorative material; An in vitro study comparing the marginal sealing ability of organically modified ceramics and a hybrid composite using an ormocer-based bonding agent and a conventional fifth-generation bonding agent. Contemp. Clin. Dent. 2012, 3, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Monsarrat, P.; Garnier, S.; Vergnes, J.N.; Nasr, K.; Grosgogeat, B.; Joniot, S. Survival of directly placed ormocer-based restorative materials: A systematic review and meta-analysis of clinical trials. Dent. Mater. 2017, 33, e212–e220. [Google Scholar] [CrossRef] [PubMed]
- AlHabdan, A.A. Review of microleakage evaluation tools. J. Int. Oral Health 2017, 9, 141–145. [Google Scholar]
- Roman, A.; Stratul, S.I.; Rusu, D.; Boariu, M.; Soanca, A.; Balazsi, R.; Suciu, M.; Moldovan, M.; Bulboacă, A.E. Investigations on the adhesion of new composites for restoring cervical lesions using energy dispersive X-ray analysis and scanning electron microscopy. Sci. Rep. 2019, 9, 9853. [Google Scholar] [CrossRef] [PubMed]
- Brochure—Voco. Available online: https://www.voco.dental/en/products.aspx (accessed on 14 May 2021).
- Brochure—GC. Available online: https://europe.gc.dental/en (accessed on 14 May 2021).
- Van Landuyt, K.L.; Snauwaert, J.; De Munck, J.; Peumans, M.; Yoshida, Y.; Poitevin, A.; Coutinho, E.; Suzuki, K.; Lambrechts, P.; Van Meerbeek, B. Systematic review of the chemical composition of contemporary dental adhesives. Biomaterials 2007, 28, 3757–3785. [Google Scholar] [CrossRef]
- Liebenberg, W.H. Posterior composite resin restorations: Operative innovations. Pract. Periodontics Aesthet. Dent. 1996, 8, 769–778, quiz 780. [Google Scholar]
- Popovici, A.; Nicola, C.; Moldovan, M.; Bondor, C.I.; Badet, C.; Roman, A.; Băciuţ, G.; Băciuţ, M.; Bran, S. A microleakage comparative study for indirect composite restorations on posterior teeth. J. Optoelectron. Adv. Mater. 2009, 11, 490–493. [Google Scholar]
- Soancă, A.; Rominu, M.; Moldovan, M.; Bondor, C.I.; Nicola, C.; Roman, A. Microscopic evaluation of the interface between composite biomaterials and dentin biostructure. Dig. J. Nanomater. Biostruct. 2011, 6, 383–392. [Google Scholar]
- Mixson, J.M.; Richards, N.D.; Mitchell, R.J. Effects of dentin age and bonding on microgap formation. Am. J. Dent. 1993, 6, 72–76. [Google Scholar]
- Weinmann, W.; Thalacker, C.; Guggenberger, R. Siloranes in dental composites. Dent. Mater. 2005, 21, 68–74. [Google Scholar] [CrossRef]
- El-Mowafy, O.; El-Badrawy, W.; Eltanty, A.; Abbasi, K.; Habib, N. Gingival microleakage of Class II resin composite restorations with fiber inserts. Oper. Dent. 2007, 32, 298–305. [Google Scholar] [CrossRef]
- Luque-Martinez, I.V.; Mena-Serrano, A.; Muñoz, M.A.; Hass, V.; Reis, A.; Loguercio, A.D. Effect of bur roughness on bond to sclerotic dentin with self-etch adhesive systems. Oper. Dent. 2013, 38, 39–47. [Google Scholar] [CrossRef] [PubMed]
- Peumans, M.; De Munck, J.; Mine, A.; Van Meerbeek, B. Clinical effectiveness of contemporary adhesives for the restoration of non-carious cervical lesions. A systematic review. Dent. Mater. 2014, 30, 1089–1103. [Google Scholar] [CrossRef] [PubMed]
- Peumans, M.; Politano, G.; Van Meerbeek, V. Treatment of noncarious cervical lesions: When, why, and how. IEJD 2020, 15, 16–42. [Google Scholar]
- Correia, A.; Bresciani, E.; Borges, A.B.; Pereira, D.M.; Maia, L.C.; Caneppele, T. Do Tooth- and Cavity-related Aspects of Noncarious Cervical Lesions Affect the Retention of Resin Composite Restorations in Adults? A Systematic Review and Meta-analysis. Oper. Dent. 2020, 45, E124–E140. [Google Scholar] [CrossRef] [PubMed]
- Santos, V.R.; Lucchesi, J.A.; Cortelli, S.C.; Amaral, C.M.; Feres, M.; Duarte, P.M. Effects of glass ionomer and microfilled composite subgingival restorations on periodontal tissue and subgingival biofilm: A 6-month evaluation. J. Periodontol. 2007, 78, 1522–1528. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.; Forjanic, M.; Cavalleri, A. Microleakage of Class II restorations with different tracers--comparison with SEM quantitative analysis. J. Adhes. Dent. 2008, 10, 259–267. [Google Scholar]
- Celik, C.; Cehreli, S.B.; Arhun, N. Resin composite repair: Quantitative microleakage evaluation of resin-resin and resin-tooth interfaces with different surface treatments. Eur. J. Dent. 2015, 9, 92–99. [Google Scholar] [CrossRef]
- Pedram, P.; Hooshmand, T.; Heidari, S. Effect of Different Cavity Lining Techniques on Marginal Sealing of Class II Resin Composite Restorations In Vitro. Int. J. Periodontics Restor. Dent. 2018, 38, 895–901. [Google Scholar] [CrossRef]
- Gladys, S.; Van Meerbeek, B.; Lambrechts, P.; Vanherle, G. Microleakage of adhesive restorative materials. Am. J. Dent. 2001, 14, 170–176. [Google Scholar]
- Cândea Ciurea, A.; Şurlin, P.; Stratul, Ş.I.; Soancă, A.; Roman, A.; Moldovan, M.; Tudoran, B.L.; Pall, E. Evaluation of the biocompatibility of resin composite-based dental materials with gingival mesenchymal stromal cells. Microsc. Res. Tech. 2019, 82, 1768–1778. [Google Scholar] [CrossRef] [PubMed]
- Al-Hiyasat, A.S.; Darmani., H.; Milhem, M.M. Cytotoxicity evaluation of dental resin composites and their flowable derivatives. Clin. Oral Investig. 2005, 9, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Ajlouni, R.; Bishara, S.; Soliman, M.M.; Oonsombat, C.; Laffoon, J.F.; Warren, J. The use of Ormocer as an alternative material for bonding orthodontic brackets. Angle Orthod. 2005, 75, 106–108. [Google Scholar]
- Gamarra, V.S.S.; Borges, G.A.; Júnior, L.H.B.; Spohr, A.M. Marginal adaptation and microleakage of a bulk-fill composite resin photopolymerized with different techniques. Odontology 2018, 106, 56–63. [Google Scholar] [CrossRef]
- Gerdolle, D.A.; Mortier, E.; Loos-Ayav, C.; Jacquot, B.; Panighi, M.M. In vitro evaluation of microleakage of indirect composite inlays cemented with four luting agents. J. Prosthet. Dent. 2005, 93, 563–570. [Google Scholar] [CrossRef]
- Ferrari, M.; Cagidiaco, M.C.; Davidson, C.L. Resistance of cementum in Class II and V cavities to penetration by an adhesive system. Dent. Mater. 1997, 13, 157–162. [Google Scholar] [CrossRef]
- Kaushik, M.; Yadav, M. Marginal microleakage properties of activa bioactive restorative and nanohybrid composite resin using two different adhesives in non carious cervical lesions—An in vitro study. J. West Afr. Coll. Surg. 2017, 7, 1–14. [Google Scholar]
- Crim, G.A.; Mattingly, S.L. Evaluation of two methods for assessing marginal leakage. J. Prosthet. Dent. 1981, 45, 160–163. [Google Scholar] [CrossRef]
- van Dijken, J.W.V.; Pallesen, U. Posterior bulk-filled resin composite restorations: A 5-year randomized controlled clinical study. J. Dent. 2016, 51, 29–35. [Google Scholar] [CrossRef]
- Van Dijken, J.W.; Pallesen, U. A randomized controlled three year evaluation of ‘‘bulk-filled’’ posterior resin restorations based on stress decreasing resin technology. Dent. Mater. 2014, 30, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Bayraktar, Y.; Ercan, E.; Hamidi, M.M.; Colak, H. One-year clinical evaluation of different types of bulk-fill composites. J. Investig. Clin. Dent. 2016, 22, 1–9. [Google Scholar] [CrossRef]
- Van Ende, A.; De Munck, J.; Lise, D.P.; Van Meerbeek, B. Bulk-Fill Composites: A Review of the Current Literature. J. Adhes. Dent. 2017, 19, 95–109. [Google Scholar] [PubMed]
- Hansen, E.K. Effect of cavity depth and application technique on marginal adaptation of resins in dental cavities. J. Dent. Res. 1986, 65, 1319–1321. [Google Scholar] [CrossRef] [PubMed]
- Lutz, F.; Krijci, I.; Barbakow, F. Quality and durability of marginal adaptation in bonded composite restorations. Dent. Mater. 1991, 7, 107–113. [Google Scholar] [CrossRef]
- Sadek, F.T.; Moura, S.K.; Ballester, R.Y.; Muench, A.; Cardoso, P.E.C. The effect of long-term storage on the microleakage of composite resin restorations: Qualitative and quantitative evaluation. Pesqui Odontol Bras. 2003, 17, 261–266. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Calenic, B.; Greabu, M.; Caruntu, C.; Nicolescu, M.I.; Moraru, L.; Surdu-Bob, C.C.; Badulescu, M.; Anghel, A.; Logofatu, C.; Boda, D. Oralkeratinocyte stem cells behavior on diamond like carbon films. Rom. Biotechnol. Lett. 2016, 21, 11914–11922. [Google Scholar] [CrossRef]

| Type of Resin Composite | Restorative Material | Manufacturer | Matrix Monomers | Filler Content | Adhesive System |
|---|---|---|---|---|---|
| Ormocer Nano-hybrid | Admira Fusion X-tra®—AX | Voco, Cuxhaven Germany | -aliphatic and aromatic dimethacrylates, -methacrylate functionalized polysiloxane | 84% weight; barium–aluminium–glass, pyrogenic silica dioxide | Futurabond M+® (Voco) (1-step self-etching) -UDMA -HEMA -acid adhesive monomer -phosphorylate monomer -catalyzer -ethanol -water |
| Ormocer Nano-hybrid | Admira Fusion®—AF | Voco, Cuxhaven Germany | -aliphatic and aromatic dimethacrylates, -methacrylate functionalized polysiloxane | 84% weight; barium–aluminium–glass, pyrogenic silica dioxide | |
| Microfilled-hybrid | Essentia®—ES | GC EUROPE N.V. Leuven | -UDMA, -Bis-MEPP, -Bis-EMA, -Bis-GMA, -TEGDMA | 81% weight; pre-polymerized filler, barium glass, fumed silica | G-Bond® (GC Corporation) (1-step self-etching) −4-META -UDMA -TEGDMA -distilled water -acetone |
| Microfilled-hybrid | G-aenial posterior®—GE | GC EUROPE N.V. Leuven | -UDMA -dimethacrylate co-monomers; | 76% weight; pre-polymerized fillers 16–17 μm: silica-containing, strontium and lanthanoid fluoride containing inorganic filler >100 nm: silica, Inorganic filler <100 nm: fumed silica; |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ciurea, A.; Delean, A.G.; Didilescu, A.; Monea, M.; Roman, A.; Boariu, M.; Stratul, Ș.I.; Mîrza, C.-M.; Micu, I.C.; Șurlin, P.; et al. In Vitro Study on the Adhesive Performance of Some Resin-Based Materials Used to Restore Class II Cavities. Materials 2021, 14, 4299. https://doi.org/10.3390/ma14154299
Ciurea A, Delean AG, Didilescu A, Monea M, Roman A, Boariu M, Stratul ȘI, Mîrza C-M, Micu IC, Șurlin P, et al. In Vitro Study on the Adhesive Performance of Some Resin-Based Materials Used to Restore Class II Cavities. Materials. 2021; 14(15):4299. https://doi.org/10.3390/ma14154299
Chicago/Turabian StyleCiurea, Andreea, Ada Gabriela Delean, Andreea Didilescu, Monica Monea, Alexandra Roman, Marius Boariu, Ștefan Ioan Stratul, Camelia-Manuela Mîrza, Iulia Cristina Micu, Petra Șurlin, and et al. 2021. "In Vitro Study on the Adhesive Performance of Some Resin-Based Materials Used to Restore Class II Cavities" Materials 14, no. 15: 4299. https://doi.org/10.3390/ma14154299
APA StyleCiurea, A., Delean, A. G., Didilescu, A., Monea, M., Roman, A., Boariu, M., Stratul, Ș. I., Mîrza, C.-M., Micu, I. C., Șurlin, P., & Soancă, A. (2021). In Vitro Study on the Adhesive Performance of Some Resin-Based Materials Used to Restore Class II Cavities. Materials, 14(15), 4299. https://doi.org/10.3390/ma14154299









