Effect of the Pulsed Electromagnetic Field (PEMF) on Dental Implants Stability: A Randomized Controlled Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Surgical Procedures
2.2. Post-Operative Procedures
2.3. Radiographic Evaluation
2.4. Resonance Frequency Analysis (RFA)
2.5. Inflammatory Mediator Levels
2.6. Analysis of IL1-β and TNF-α
2.7. Statistical Analyses
3. Results
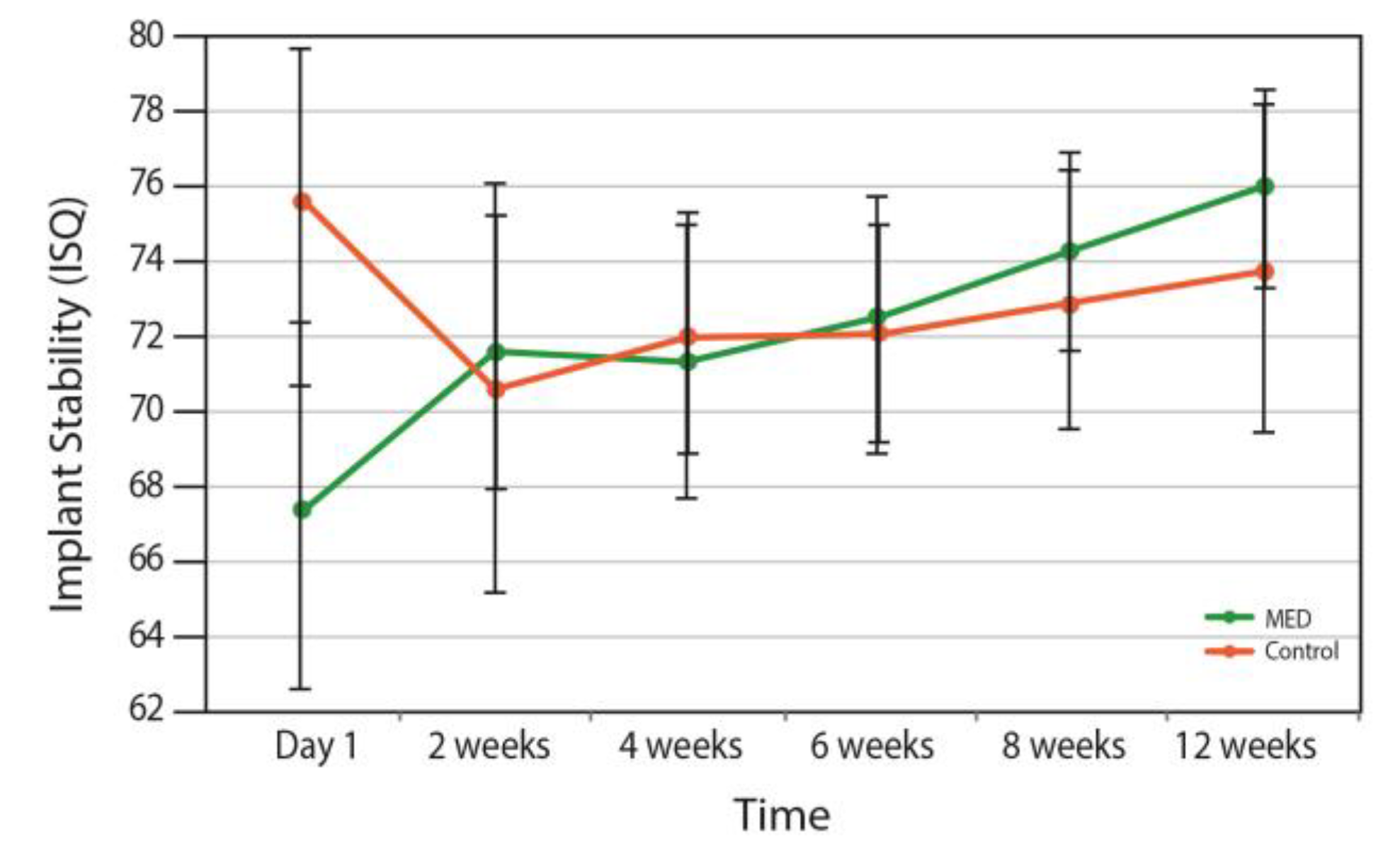
3.1. Implant Stability
3.2. Radiographic Evaluation
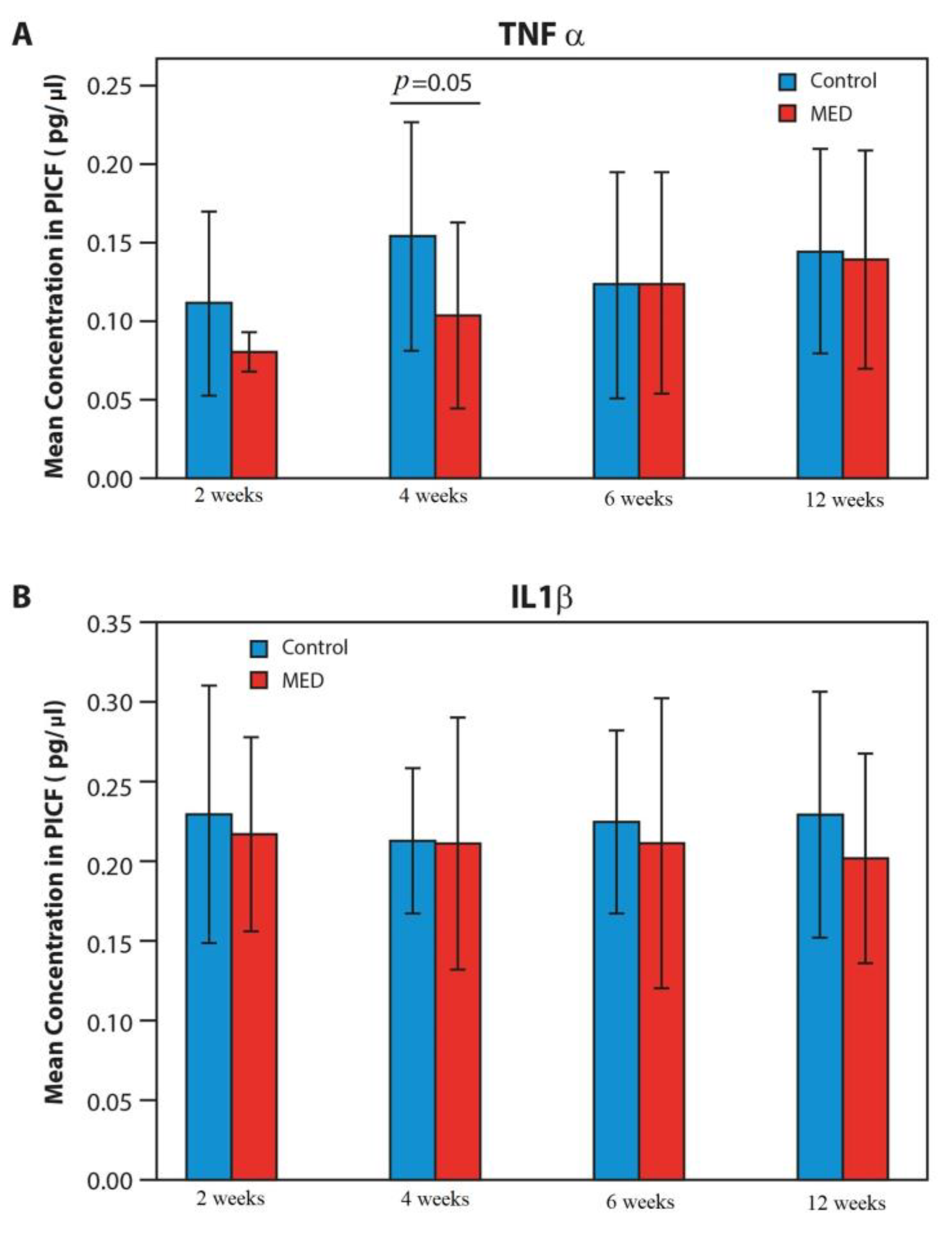
3.3. Proinflammatory Mediators
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Compton, S.M.; Clark, D.; Chan, S.; Kuc, I.; Wubie, B.A.; Levin, L. Dental Implants in the Elderly Population: A Long-Term Follow-up. Int. J. Oral Maxillofac. Implant. 2017, 32, 164. [Google Scholar] [CrossRef] [PubMed]
- Kuchler, U.; Chappuis, V.; Bornstein, M.M.; Siewczyk, M.; Gruber, R.; Maestre, L.; Buser, D. Development of Implant Stability Quotient values of implants placed with simultaneous sinus floor elevation—Results of a prospective study with 109 implants. Clin. Oral Implant. Res. 2017, 28, 109. [Google Scholar] [CrossRef] [PubMed]
- Omura, Y.; Kanazawa, M.; Sato, D.; Kasugai, S.; Minakuchi, S. Comparison of patient-reported outcomes between immediately and conventionally loaded mandibular two-implant overdentures: A preliminary study. J. Prosthodont. Res. 2016, 60, 185. [Google Scholar] [CrossRef] [PubMed]
- Penarrocha-Oltra, D.; Penarrocha-Diago, M.; Aloy-Prosper, A.; Covani, U.; Penarrocha, M. Immediate Versus Conventional Loading of Complete-Arch Implant-Supported Prostheses in Mandibles with Failing Dentition: A Patient-Centered Controlled Prospective Study. Int. J. Prosthodont. 2015, 28, 499. [Google Scholar] [CrossRef] [PubMed]
- Degidi, M.; Iezzi, G.; Perrotti, V.; Piattelli, A. Comparative analysis of immediate functional loading and immediate nonfunctional loading to traditional healing periods: A 5-year follow-up of 550 dental implants. Clin. Implant. Dent. Relat. Res. 2009, 11, 257. [Google Scholar] [CrossRef] [PubMed]
- Javed, F.; Ahmed, H.B.; Crespi, R.; Romanos, G.E. Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interv. Med. Appl. Sci. 2013, 5, 162. [Google Scholar] [CrossRef] [PubMed]
- Natali, A.N.; Carniel, E.L.; Pavan, P.G. Investigation of viscoelastoplastic response of bone tissue in oral implants press fit process. J. Biomed. Mater. Res. B Appl. Biomater. 2009, 91, 868. [Google Scholar] [CrossRef] [PubMed]
- Ferroni, L.; Gardin, C.; Dolkart, O.; Salai, M.; Barak, S.; Piattelli, A.; Amir-Barak, H.; Zavan, B. Pulsed electromagnetic fields increase osteogenetic commitment of MSCs via the mTOR pathway in TNF-alpha mediated inflammatory conditions: An in-vitro study. Sci. Rep. 2018, 8. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, H.; Ochi, M.; Abiko, Y.; Hirose, Y.; Kaku, T.; Sakaguchi, K. Pulsed electromagnetic fields promote bone formation around dental implants inserted into the femur of rabbits. Clin. Oral Implant. Res. 2000, 11, 354–360. [Google Scholar] [CrossRef] [PubMed]
- Barak, S.; Neuman, M.; Iezzi, G.; Piattelli, A.; Perrotti, V.; Gabet, Y. A new device for improving dental implants anchorage: A histological and micro-computed tomography study in the rabbit. Clin. Oral Implant. Res. 2016, 27, 935. [Google Scholar] [CrossRef] [PubMed]
- Barak, S.; Matalon, S.; Dolkart, O.; Zavan, B.; Mortellaro, C.; Piattelli, A. Miniaturized Electromagnetic Device Abutment Improves Stability of the Dental Implants. J. Craniofacial Surg. 2019. [Google Scholar] [CrossRef] [PubMed]
- Shibli, J.A.; Melo, L.; Ferrari, D.S.; Figueiredo, L.C.; Faveri, M.; Feres, M. Composition of supra- and subgingival biofilm of subjects with healthy and diseased implants. Clin. Oral Implant. Res. 2018, 19, 975. [Google Scholar] [CrossRef] [PubMed]
- Albrektsson, T.; Zarb, G.A. Current interpretations of the osseointegrated response: Clinical significance. Int. J. Prosthodont. 1993, 6, 95–105. [Google Scholar] [PubMed]
- Bosshardt, D.D.; Chappuis, V.; Buser, D. Osseointegration of titanium, titanium alloy and zirconia dental implants: Current knowledge and open questions. Periodontology 2000, 73, 22–40. [Google Scholar] [CrossRef] [PubMed]
- Bielemann, A.M.; Marcello-Machado, R.M.; Leite, F.R.M.; Martinho, F.C.; Chagas-Junior, O.L.; Antoninha Del Bel Cury, A.; Faot, F. Comparison between inflammation-related markers in peri-implant crevicular fluid and clinical parameters during osseointegration in edentulous jaws. Clin. Oral Investig. 2018, 22, 531. [Google Scholar] [CrossRef] [PubMed]
- Barak, S.D.; Dolkart, M.; Faveri, M.; Bueno-Silva, B.; Soares, G.M.; Feres, M.; Shibli, J.A. Antimicrobial effects of pulsed electromagnetic field: In vitro polymicrobial periodontal subgingival model. J. Clin. Periodontol. 2018. [Google Scholar] [CrossRef]

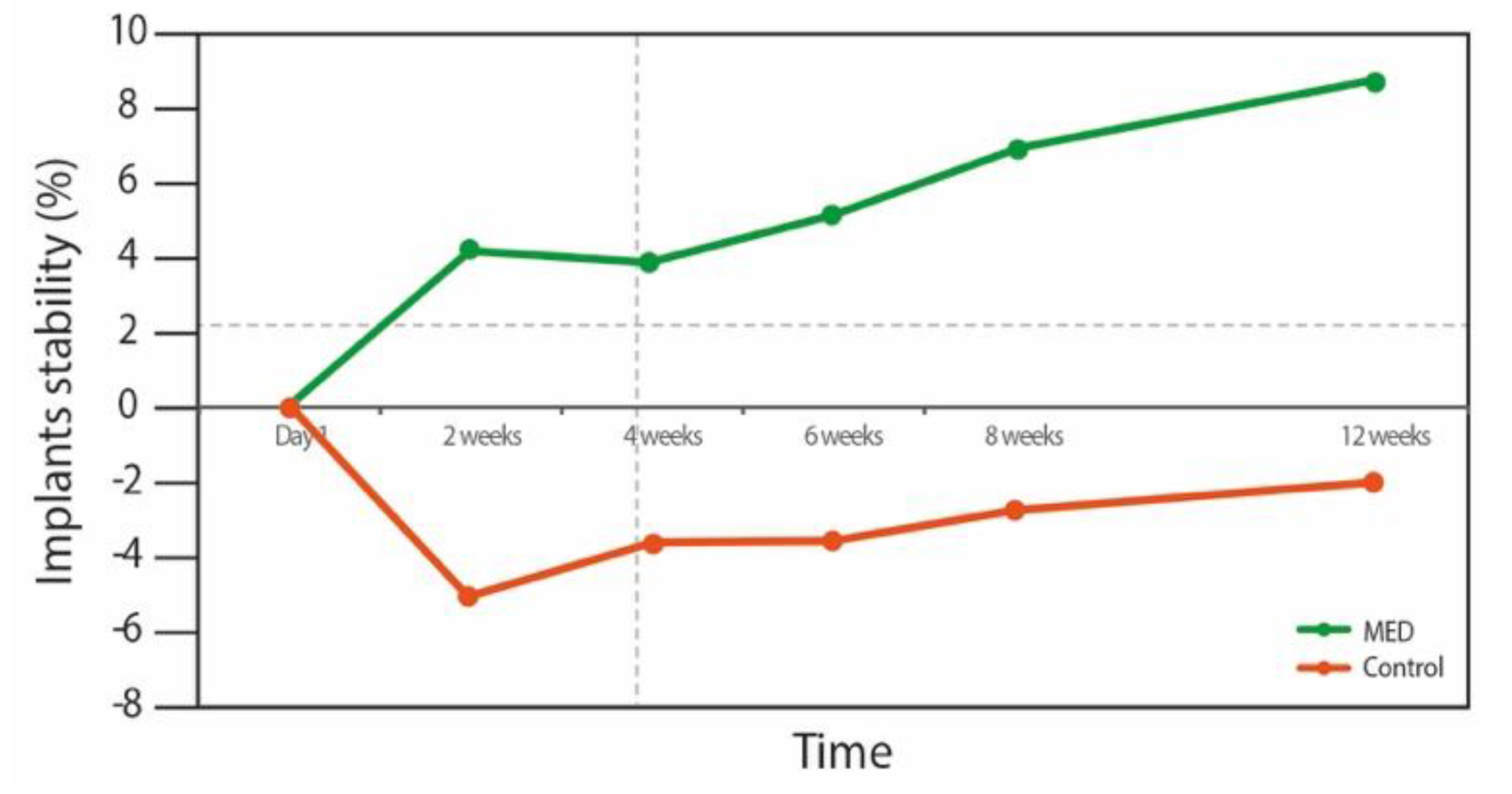

| Time Points | Group | Mean Differences | Standard Error | * p Value | Change % |
|---|---|---|---|---|---|
| Day 1 vs. 2 weeks | MED | −4.1 | 2.6 | 0.12 | +6.1 |
| Control | 5 | 2.4 | 0.05 | −6.7 | |
| Day 1 vs. 4 weeks | MED | −3.8 | 3 | 0.21 | +6.2 |
| Control | 3.5 | 1 | 0.003 | −6.6 | |
| Day 1 vs. 6 weeks | MED | −5.1 | 3.1 | 0.12 | +7.6 |
| Control | 3.4 | 0.8 | 0.001 | −4.6 | |
| Day 1 vs. 8 weeks | MED | −6.9 | 3.2 | 0.04 | +10.2 |
| Control | 2.7 | 0.6 | 0.00 | −3.6 | |
| Day 1 vs. 12 weeks | MED | −8.5 | 3.3 | 0.02 | +12 |
| Control | 1.8 | 0.5 | 0.003 | −2.5 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nayak, B.P.; Dolkart, O.; Satwalekar, P.; Kumar, Y.P.; Chandrasekar, A.; Fromovich, O.; Yakobson, E.; Barak, S.; Dayube, U.; Shibli, J.A. Effect of the Pulsed Electromagnetic Field (PEMF) on Dental Implants Stability: A Randomized Controlled Clinical Trial. Materials 2020, 13, 1667. https://doi.org/10.3390/ma13071667
Nayak BP, Dolkart O, Satwalekar P, Kumar YP, Chandrasekar A, Fromovich O, Yakobson E, Barak S, Dayube U, Shibli JA. Effect of the Pulsed Electromagnetic Field (PEMF) on Dental Implants Stability: A Randomized Controlled Clinical Trial. Materials. 2020; 13(7):1667. https://doi.org/10.3390/ma13071667
Chicago/Turabian StyleNayak, Bhukya P., Oleg Dolkart, Parth Satwalekar, Yeramala P. Kumar, Anam Chandrasekar, Ophir Fromovich, Elad Yakobson, Shlomo Barak, Ulisses Dayube, and Jamil A. Shibli. 2020. "Effect of the Pulsed Electromagnetic Field (PEMF) on Dental Implants Stability: A Randomized Controlled Clinical Trial" Materials 13, no. 7: 1667. https://doi.org/10.3390/ma13071667
APA StyleNayak, B. P., Dolkart, O., Satwalekar, P., Kumar, Y. P., Chandrasekar, A., Fromovich, O., Yakobson, E., Barak, S., Dayube, U., & Shibli, J. A. (2020). Effect of the Pulsed Electromagnetic Field (PEMF) on Dental Implants Stability: A Randomized Controlled Clinical Trial. Materials, 13(7), 1667. https://doi.org/10.3390/ma13071667






