The Indirect Bonding Technique in Orthodontics—A Narrative Literature Review
Abstract
1. Introduction
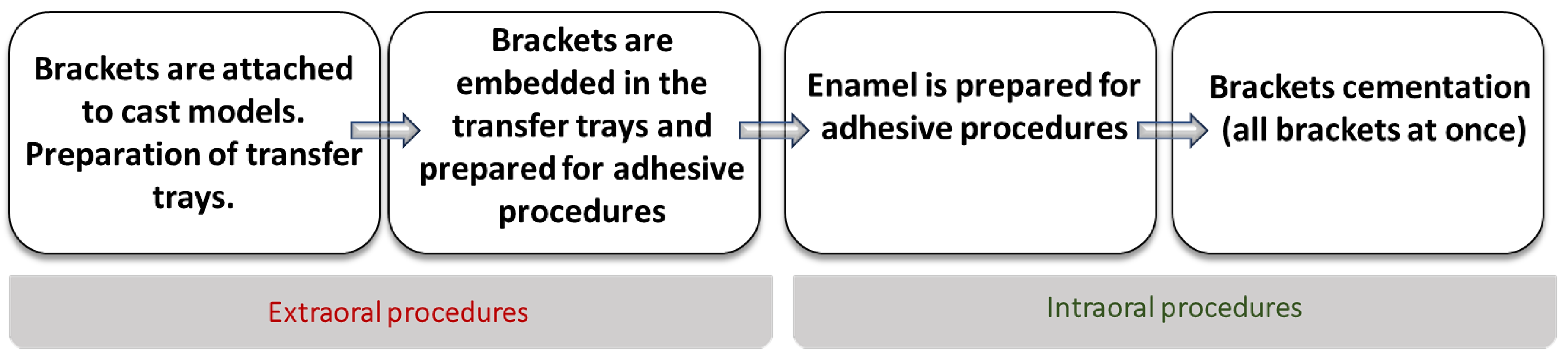
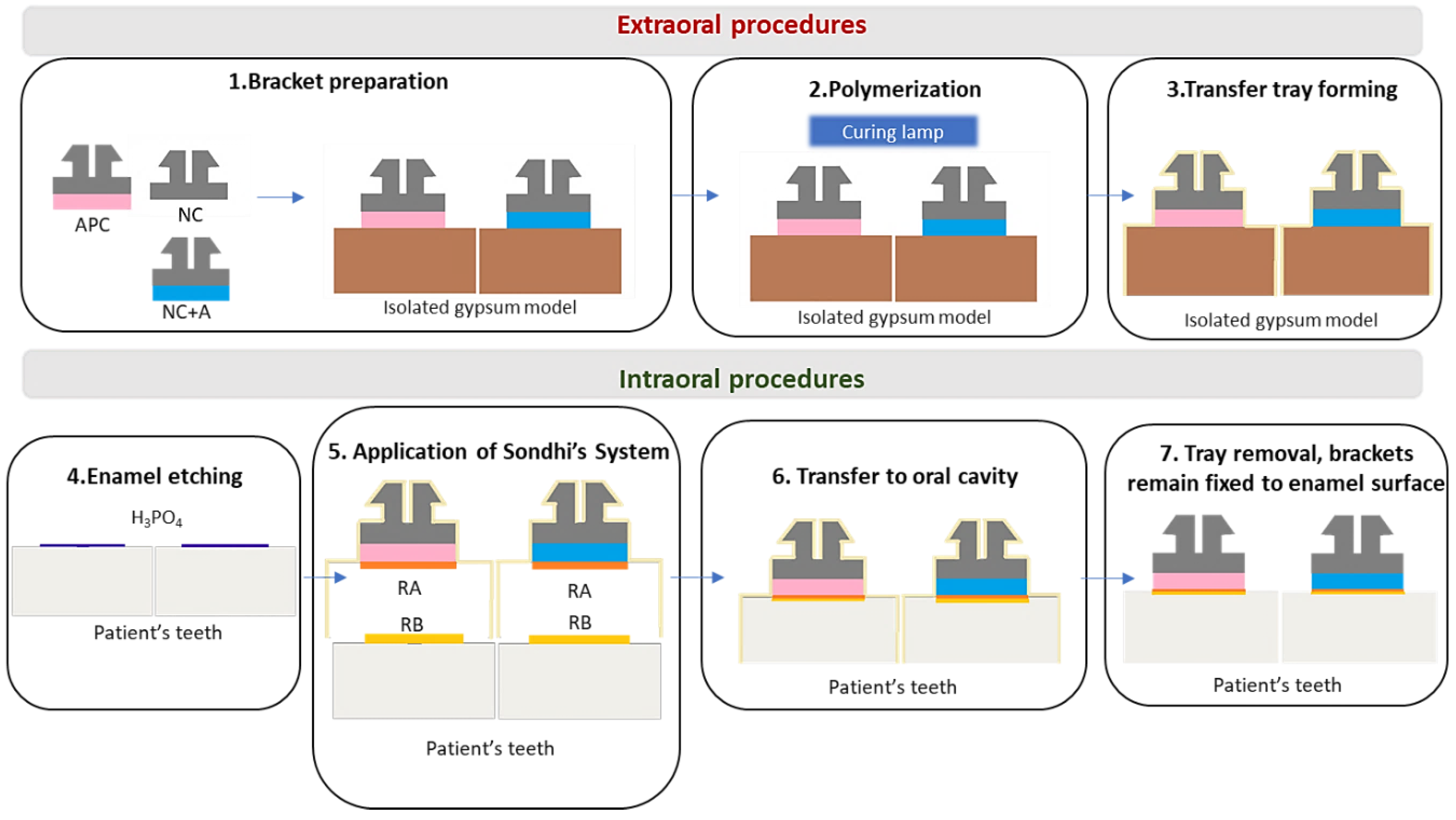
2. The Beginnings of the Indirect Technique (1970–1999)
3. Development of Bonding Systems
4. The 21st Century—Time for Digital Technology
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Silverman, E.; Cohen, M.; Gianelly, A.A.; Dietz, V.S. A universal direct bonding system for both metal and plastic brackets. Am. J. Orthod. 1972, 62, 236–244. [Google Scholar] [CrossRef]
- Newman, G.V. Epoxy adhesives for orthodontic attachments: Progress report. Am. J. Orthod. Dentofac. Orthop. 1965, 51, 901–912. [Google Scholar] [CrossRef]
- Gia, K.Y.; Dunn, W.J.; Taloumis, L.J. Shear bond strength comparison between direct and indirect bonded orthodontic brackets. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 577–581. [Google Scholar]
- Thomas, R.G. Indirect bonding: Simplicity in action. J. Clin. Orthod. JCO 1979, 13, 93–106. [Google Scholar]
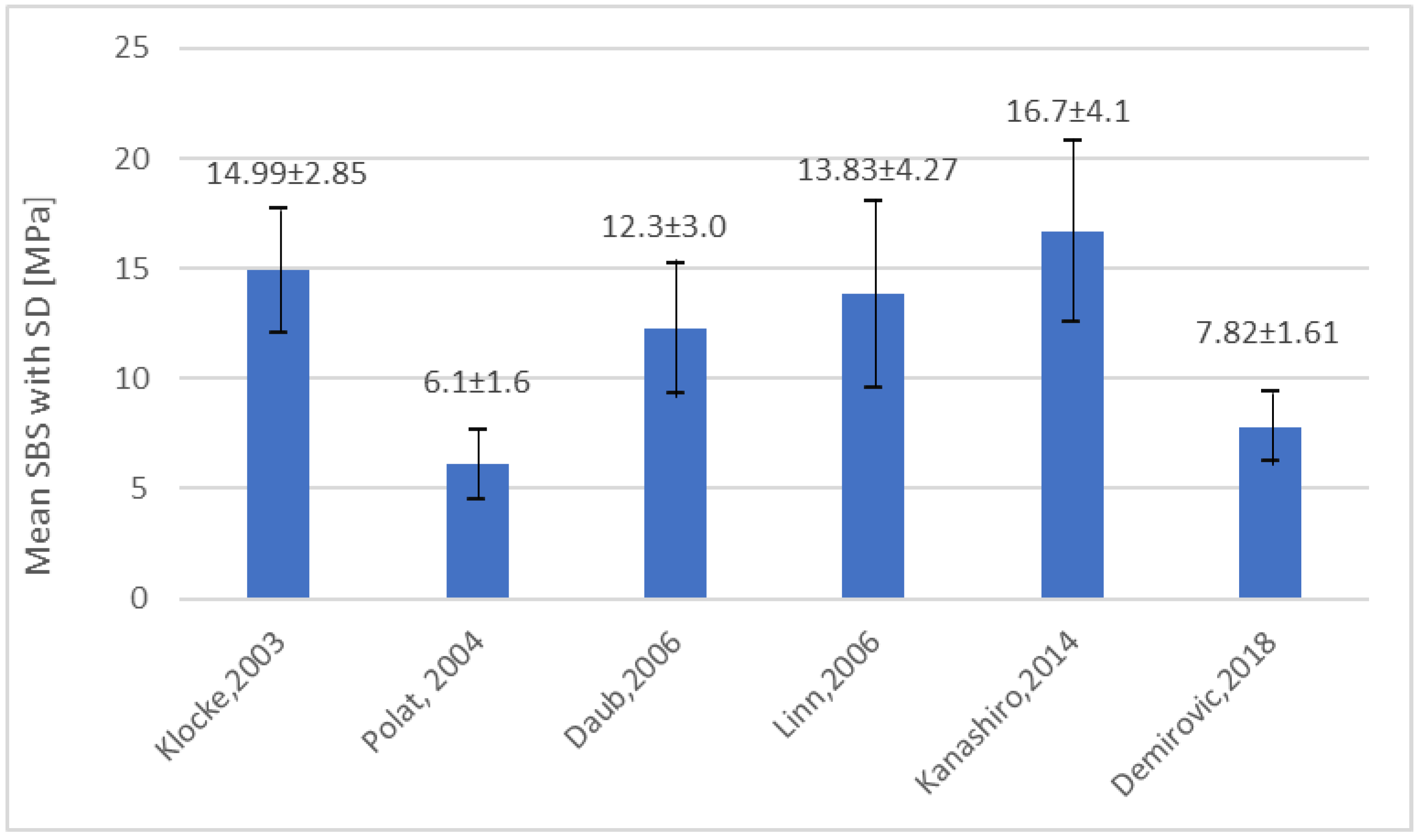
- Klocke, A.; Shi, J.; Kahl-Nieke, B.; Bismayer, U. Bond strength with custom base indirect bonding techniques. Angle Orthod. 2003, 73, 176–180. [Google Scholar] [PubMed]
- Sondhi, A. Efficient and effective indirect bonding. Am. J. Orthod. Dentofac. Orthop. 1999, 115, 352–359. [Google Scholar] [CrossRef]
- Hocevar, R.A.; Vincent, H.F. Indirect versus direct bonding: Bond strength and failure location. Am. J. Orthod. Dentofac. Orthop. 1988, 94, 367–371. [Google Scholar] [CrossRef]
- Linn, B.J.; Berzins, D.W.; Dhuru, V.B.; Bradley, T.G. A comparison of bond strength between direct-and indirect-bonding methods. Angle Orthod. 2006, 76, 289–294. [Google Scholar] [PubMed]
- Milne, J.W.; Andreassen, G.F.; Jakobsen, J.R. Bond strength comparison: A simplified indirect technique versus direct placement of brackets. Am. J. Orthod. Dentofac. Orthop. 1989, 96, 8–15. [Google Scholar] [CrossRef]
- Polat, O.; Karaman, A.I.; Buyukyilmaz, T. In vitro evaluation of shear bond strengths and in vivo analysis of bond survival of indirect-bonding resins. Angle Orthod. 2004, 74, 405–409. [Google Scholar] [PubMed]
- Reynolds, I.R. A review of direct orthodontic bonding. Br. J. Orthod. 1975, 2, 171–178. [Google Scholar] [CrossRef]
- Bishara, S.E.; Olsen, M.; Von Wald, L. Comparisons of shear bond strength of precoated and uncoated brackets. Am. J. Orthod. Dentofac. Orthop. 1997, 112, 617–621. [Google Scholar] [CrossRef]
- Hirani, S. Handling characteristics of precoated and operator-coated brackets. J. Clin. Orthod. JCO 2005, 39, 429. [Google Scholar] [CrossRef] [PubMed]
- Hirani, S.; Sherriff, M. Bonding characteristics of a self-etching primer and precoated brackets: An in vitro study. Eur. J. Orthod. 2006, 28, 400–404. [Google Scholar] [CrossRef]
- Kalange, J.T.; Thomas, R.G. Indirect bonding: A comprehensive review of the literature. In Seminars in Orthodontics; WB Saunders: Paris, France, 2007; Volume 13, pp. 3–10. [Google Scholar]
- Sondhi, A. Effective and efficient indirect bonding: The Sondhi method. In Seminars in Orthodontics; WB Saunders: Paris, France, 2007; Volume 13, pp. 43–57. [Google Scholar]
- Flores, T.; Mayoral, J.R.; Giner, L.; Puigdollers, A. Comparison of enamel-bracket bond strength using direct-and indirect-bonding techniques with a self-etching ion releasing S-PRG filler. Dental Mater. J. 2015, 34, 41–47. [Google Scholar] [CrossRef][Green Version]
- Demirovic, K.; Slaj, M.; Spalj, S.; Slaj, M.; Kobaslija, S. Comparison of Shear Bond Strength of Orthodontic Brackets Using Direct and Indirect Bonding Methods in Vitro and in Vivo. Acta Inform. Med. 2018, 26, 125–129. [Google Scholar] [CrossRef]
- Pamukçu, H.; Özsoy, Ö.P. Indirect Bonding Revisited. Turk. J. Orthod. 2016, 29, 80–86. [Google Scholar] [CrossRef]
- Deahl, S.T.; Salome, N.; Hatch, J.P.; Rugh, J.D. Practice-based comparison of direct and indirect bonding. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 738–742. [Google Scholar] [CrossRef]
- Kanashiro, L.K.; Robles-Ruíz, J.J.; Ciamponi, A.L.; Medeiros, I.S.; Dominguez, G.C.; de Fantini, S.M. Effect of adhesion boosters on indirect bracket bonding. Angle Orthod. 2013, 84, 171–176. [Google Scholar] [CrossRef]
- Ciuffolo, F.; Epifania, E.; Duranti, G.; De Luca, V.; Raviglia, D.; Rezza, S.; Festa, F. Rapid prototyping: A new method of preparing trays for indirect bonding. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 75–77. [Google Scholar] [CrossRef]
- Son, K.H.; Park, J.W.; Lee, D.K.; Kim, K.D.; Baek, S.H. New virtual orthodontic treatment system for indirect bonding using the stereolithographic technique. Korean J. Orthod. 2011, 41, 138–146. [Google Scholar] [CrossRef]
- Kim, J.; Chun, Y.S.; Kim, M. Accuracy of bracket positions with a CAD/CAM indirect bonding system in posterior teeth with different cusp heights. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 298–307. [Google Scholar] [CrossRef] [PubMed]
- Nichols, D.A.; Gardner, G.; Carballeyra, A.D. Reproducibility of bracket positioning in the indirect bonding technique. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 770–776. [Google Scholar] [CrossRef] [PubMed]
- Padmaprabha, B.P.; Ayinipully, H.; Paul, R.T.; Ponnambathayil, S.A.; Rasheed, A.T. A Unique Bonding Technique for Immediate Orthognathic Surgery. J. Clin. Diagn. Res. JCDR 2015, 9, ZC26. [Google Scholar] [CrossRef]
- Bovali, E.; Kiliaridis, S.; Cornelis, M.A. Indirect vs. direct bonding of mandibular fixed retainers in orthodontic patients: A single-center randomized controlled trial comparing placement time and failure over a 6-month period. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 701–708. [Google Scholar] [CrossRef]
- Egli, F.; Bovali, E.; Kiliaridis, S.; Cornelis, M.A. Indirect vs. direct bonding of mandibular fixed retainers in orthodontic patients: Comparison of retainer failures and posttreatment stability. A 2-year follow-up of a single-center randomized controlled trial. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 15–27. [Google Scholar] [CrossRef]

| Author (Year) | Data from Research | ||||
|---|---|---|---|---|---|
| Method | Material | Number of Teeth | Mean SBS (SD) | Conclusions | |
| Hocevar et al., 1988 [7] | Direct | Concise (3M, St Paul, Minn, USA) | 18 | 6.69 (0.92) | NSD |
| Indirect | Concise (3M, St Paul, Minn, USA) | 18 | 6.40 (0.87) | ||
| Milne et al., 1989 [9] | Direct | Concise (3M, St Paul, Minn, USA) | 12 | 19.06 (1.67) | NSD |
| Indirect | Concise (3M, St Paul, Minn, USA) | 12 | 16.77 (3.04) | ||
| Yi et al., 2003 [3] | Direct | Transbond XT (3M Unitek, Monrovia, CA, USA) | 27 | 10.9 (2.9) | NSD |
| Indirect | APC, Sondhi Rapid Set (3M Unitek, Monrovia, CA, USA) | 27 | 11.2 (2.6) | ||
| Klocke et al., 2003 [5] | Direct | Transbond XT (3M Unitek, Monrovia, CA, USA) | 20 | 13.88 (4.33) | TC: lower SBS LC, CC: NSD |
| Indirect | Thermacure+MaximumCure (Reliance Orthodontic Products, Itasca, Ill, USA) | 20 | 7.28 (4.88) | ||
| Thermacure+Custom IQ (Reliance Orthodontic Products, Itasca, Ill, USA) | 20 | 7.07 (4.11) | |||
| PhaseII+MaximumCure (Reliance Orthodontic Products, Itasca, Ill, USA) | 20 | 15.41 (3.21) | |||
| APC, Sondhi Rapid Set (3M Unitek, Monrovia, CA, USA) | 20 | 14.99 (2.85) | |||
| Polat et al., 2004 [10] | Direct | Transbond XT (3M Unitek, Monrovia, CA, USA) | 20 | 12,8 (5.4) | Transbond XT + SondhiRapidSet: lower SBS |
| Indirect | Thermacure+CustomIQ+adhesion booster (Reliance Orthodontic Products, Itasca, Ill, USA) | 20 | 10.3 (4.1) | ||
| Transbond XT, Sondhi Rapid Set (3M Unitek, Monrovia, CA, USA) | 20 | 6.1 (1.6) | |||
| Linn et al., 2006 [8] | Direct | Transbond XT (3M Unitek, Monrovia, CA, USA) | 20 | 16,27 (4.74) | NSD |
| Indirect | Transbond XT, Sondhi Rapid Set (3M Unitek, Monrovia, CA, USA) | 20 | 14.76 (4.06) | ||
| Enlight LV, OrthoSolo (Orm- co Corporation, Glendora, Calif, USA) | 20 | 13,83 (4.27) | |||
| Enamel Preparation | Adhesive on Bracket Base | Sealant | Advantages | Disadvantages |
|---|---|---|---|---|
| AET | CC | CC(2 components, (catalyst on bracket base and universal unfilled resin on enamel) | -Less failures than in Silvermann’s technique [5] -Better control of the material amount [4] | -Limited time for bracket placement [8,15] -Incomplete curing of sealant [5,8] |
| AET | TC | CC(2 components, mixed before application) | -Unlimited time for bracket placement [8] -Reduced risk of material excess [8] | -Lower SBS in comparison to LC and CC bracket bases [5,16] -Not recommended for ceramic brackets [16] |
| AET | LC | CC (2 components, mixed before application) | -Unlimited time for bracket placement [8] -Fast polymerization [8,15] -Reduced risk of material excess [5,8] - Bond strengths similar to the DB [15] | The risk of bonding failure between sealant and composite [5] |
| SET | LC | SET, LC (2 components, mixed before an application) | Reduced amount of adhesive after debonding (lower ARI) in comparison to AET [17] | Lower SBS than AET [17] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nawrocka, A.; Lukomska-Szymanska, M. The Indirect Bonding Technique in Orthodontics—A Narrative Literature Review. Materials 2020, 13, 986. https://doi.org/10.3390/ma13040986
Nawrocka A, Lukomska-Szymanska M. The Indirect Bonding Technique in Orthodontics—A Narrative Literature Review. Materials. 2020; 13(4):986. https://doi.org/10.3390/ma13040986
Chicago/Turabian StyleNawrocka, Agnieszka, and Monika Lukomska-Szymanska. 2020. "The Indirect Bonding Technique in Orthodontics—A Narrative Literature Review" Materials 13, no. 4: 986. https://doi.org/10.3390/ma13040986
APA StyleNawrocka, A., & Lukomska-Szymanska, M. (2020). The Indirect Bonding Technique in Orthodontics—A Narrative Literature Review. Materials, 13(4), 986. https://doi.org/10.3390/ma13040986






