Mean Shearing Stroke Frequency of Orthodontic Brackets under Cycling Loading: An In Vitro Study
Abstract
1. Introduction
2. Material and Methods
2.1. Ethical Approval and Preparation of Samples
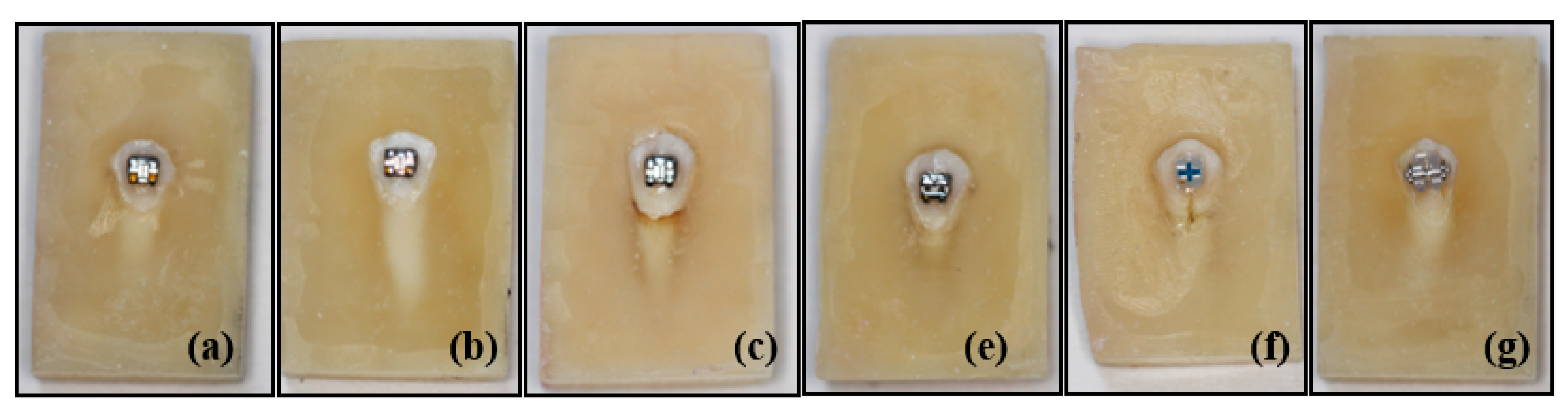
2.2. Storage Conditions of Teeth and Preparation of Acrylic Blocks
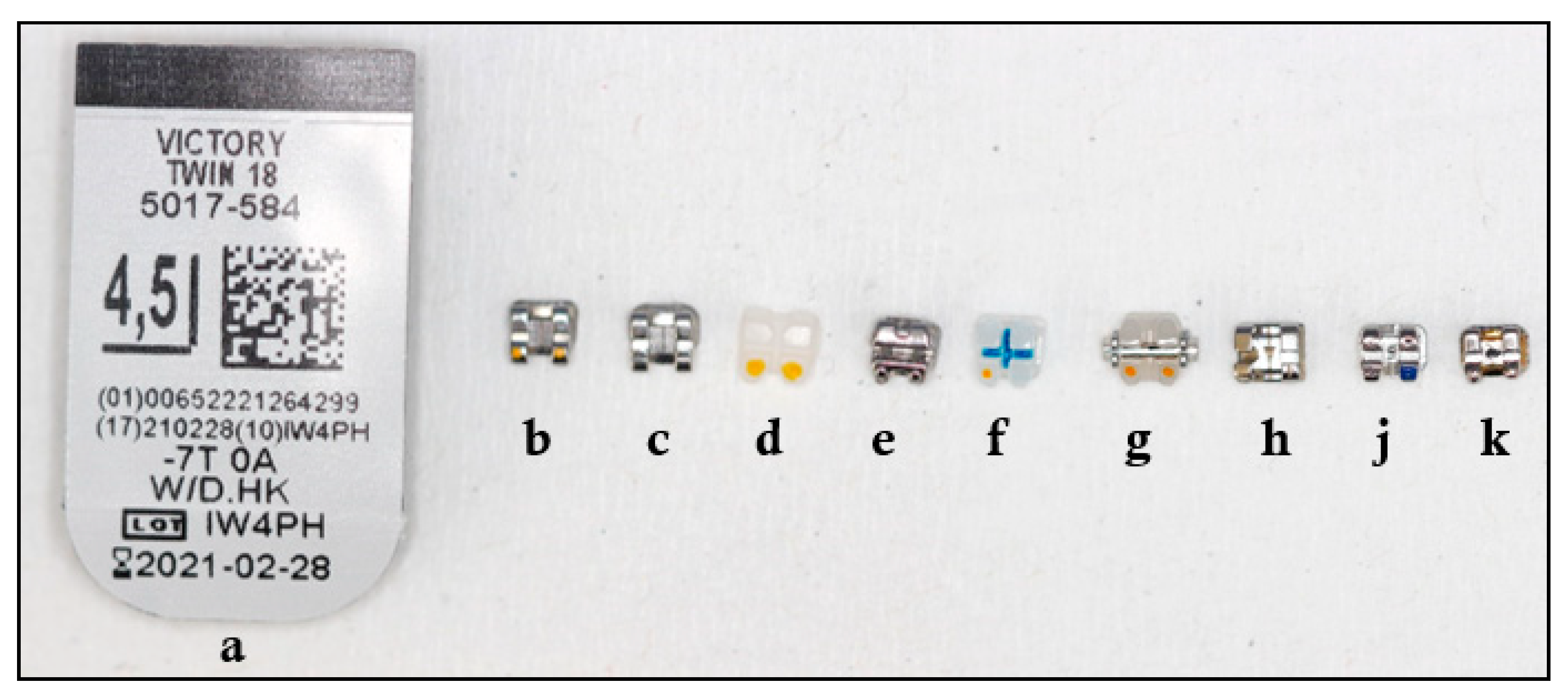
2.3. Brackets Used
2.4. Bonding of Brackets
2.5. Preparation of Groups
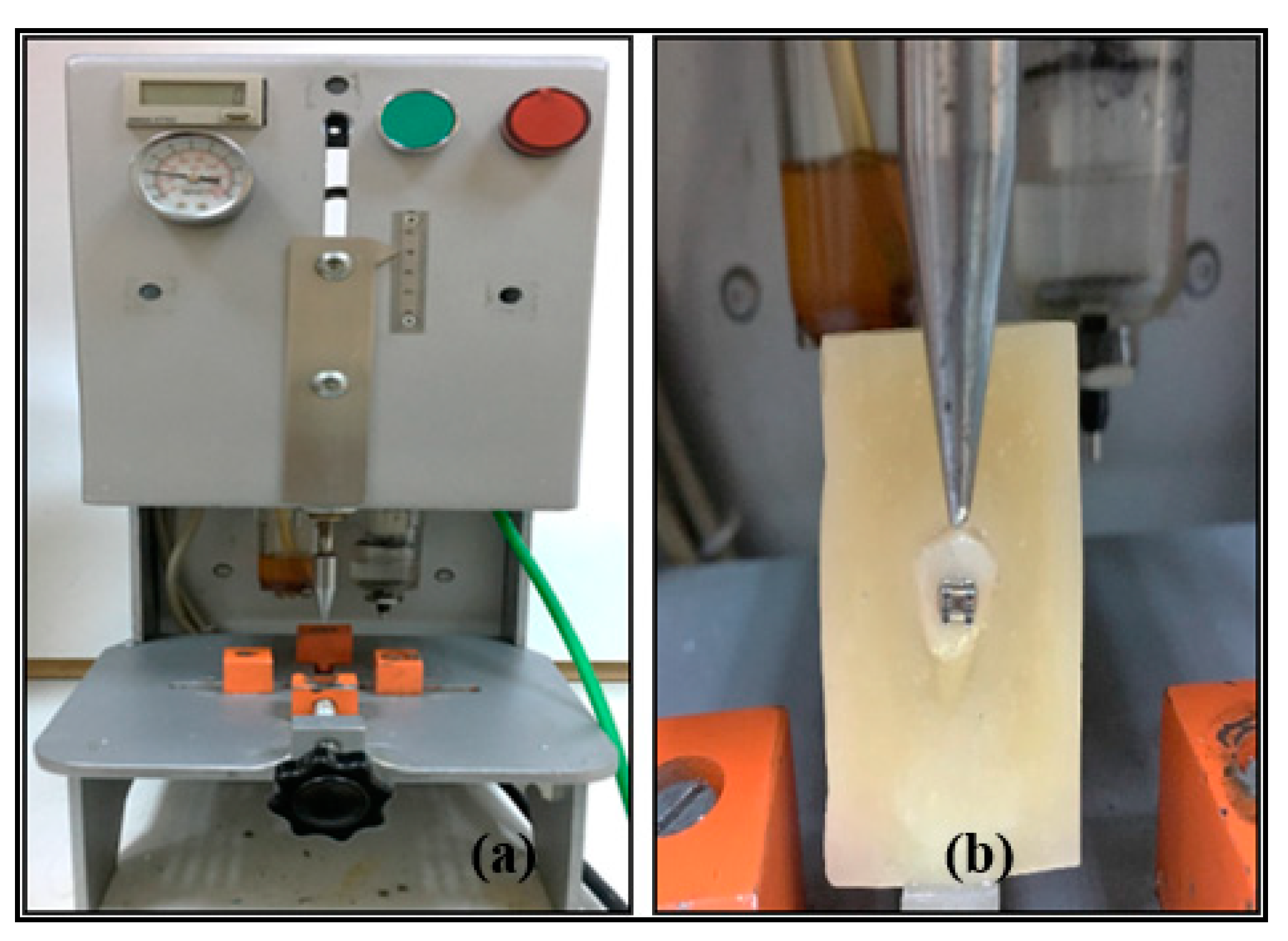
2.6. Fatigue Testing
2.7. Statistical Analysis
3. Results
3.1. Results of APC Brackets
3.2. Results According to Bracket Raw Materials
3.3. Results According to Ligation Types
3.4. Results According to Brackets Brand
3.5. Results According to Type of Adhesive Agents
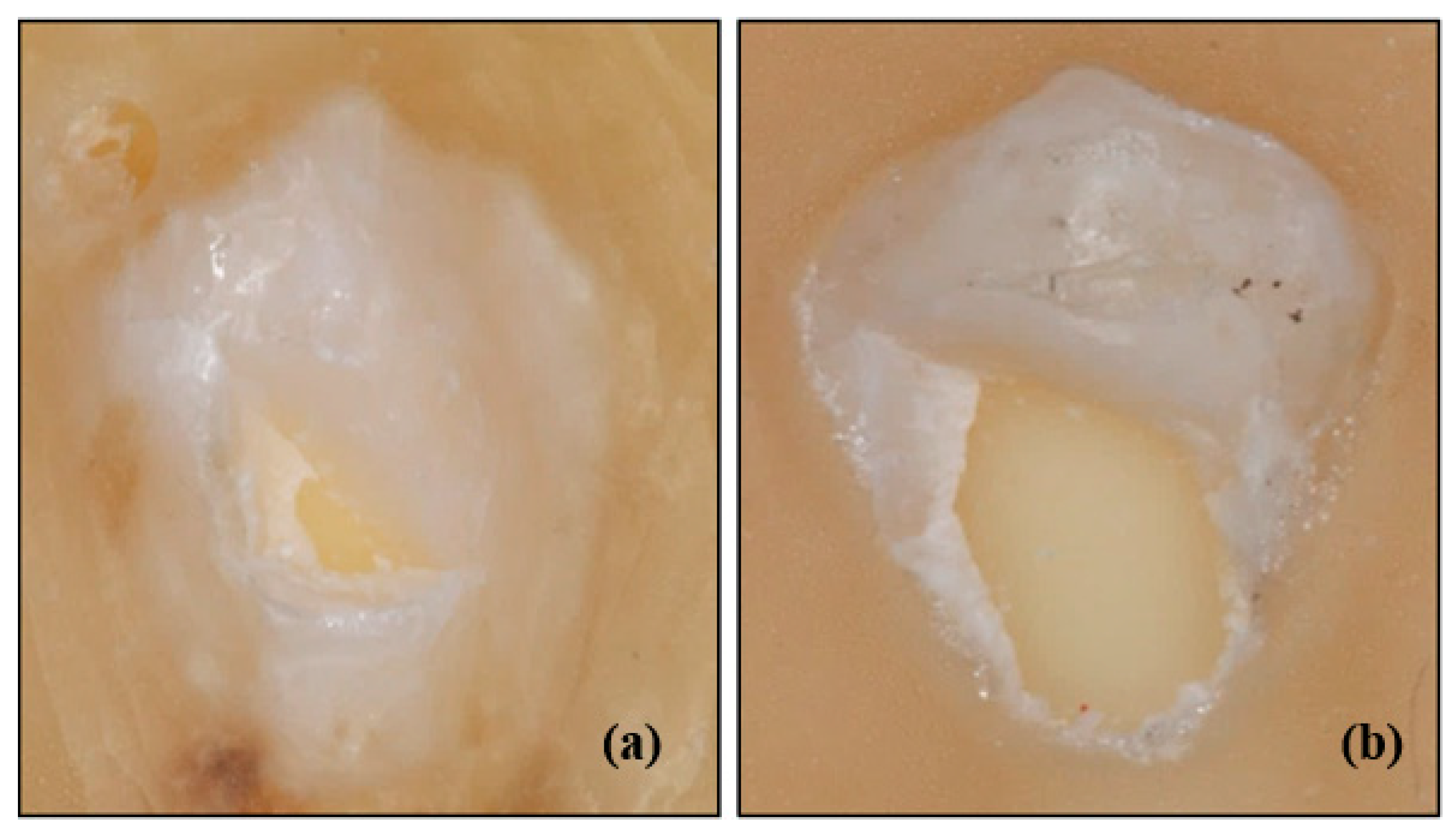
3.6. Bracket Wing Breakings and Dental Hard Tissue Damages
4. Discussion
- (i)
- statistically significantly higher shearing strokes frequency was found in Victory series metal brackets when compared with Mini Sprint® metal and Mini Master metal brackets,
- (ii)
- equilibrium 2 metal brackets showed statistically significantly higher shearing stroke frequency than that of Gemini SL self-ligating metal brackets.
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Barbosa, I.V.; Miranda Ladewig, V.; Almeida Pedrin, R.R.; Cardoso, M.A.; Junior, J.F.S.; Conti, A.C.C.F. The association between patient’s compliance and age with the bonding failure of orthodontic brackets: A cross-sectional study. Prog. Orthod. 2018, 19, 1–5. [Google Scholar] [CrossRef]
- Ishida, K.; Endo, T.; Shinkai, K.; Katoh, Y. Shear bond strength of rebonded brackets after removal of adhesives with Er, Cr: YSGG laser. Odontology 2011, 99, 129–134. [Google Scholar]
- Sukhia, H.; Sukhia, R.; Mahar, A. Bracket De-Bonding & Breakage Prevalence in Orthodontic Patients. Pak. Oral Dent. J. 2011, 31, 71–76. [Google Scholar]
- Pandis, N.; Eliades, T. A comparative in vivo assessment of the long-term failure rate of 2 self-etching primers. Am. J. Orthod. Dentofac. Orthop. 2005, 128, 96–98. [Google Scholar] [CrossRef]
- Daniels, A.S.; Seacat, J.D.; Inglehart, M.R. Orthodontic treatment motivation and cooperation: A cross-sectional analysis of adolescent patients’ and parents’ responses. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 780–787. [Google Scholar] [CrossRef] [PubMed]
- Feldens, C.A.; Nakamura, E.K.; Tessarollo, F.R.; Closs, L.Q. Desire for orthodontic treatment and associated factors among adolescents in Southern Brazil. Angle Orthod. 2015, 85, 224–232. [Google Scholar] [CrossRef] [PubMed]
- Graber, L.W.; Vanarsdall, R.L.; Vig, K.W.; Huang, G.J. Orthodontics: Current Principles and Techniques, 6th ed.; Elsevier Health Science: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Usumez, S.; Erverdi, N. Adhesives and Bonding in Orthodontics. In Current Therapy in Orthodontics, 1st ed.; Nanda, R., Kapila, S., Eds.; Mosby: St Louis, MA, USA, 2010; pp. 45–67. [Google Scholar]
- Knox, J.; Hubsch, P.; Jones, M.L.; Middleton, J. The influence of bracket base design on the strength of the bracket–cement interface. J. Orthod. 2000, 27, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Reimann, S.; Mezey, J.; Daratsianos, N.; Jäger, A.; Bourauel, C. The influence of adhesives and the base structure of metal brackets on shear bond strength. J. Orofac. Orthop. Fortschr. Kieferorthopädie 2012, 73, 184–193. [Google Scholar] [CrossRef]
- Smith, N.R.; Reynolds, I.R. A Comparison of Three Bracket Bases: An In Vitro Study. Br. J. Orthod. 1991, 18, 29–35. [Google Scholar] [CrossRef]
- Ødegaard, J.; Segner, D. Shear bond strength of metal brackets compared with a new ceramic bracket. Am. J. Orthod. Dentofac. Orthop. 1988, 94, 201–206. [Google Scholar] [CrossRef]
- Fan, P.; Stanford, C.M.; Stanford, W.B.; Leung, R.; Stanford, J.W. Effects of backing reflectance and mold size on polymerization of photo-activated composite resin. J. Dent. Res. 1984, 63, 1245–1247. [Google Scholar] [CrossRef]
- Staderini, E.; Guglielmi, F.; Cornelis, M.A.; Cattaneo, P.M. Three-dimensional prediction of roots position through cone-beam computed tomography scans-digital model superimposition: A novel method. Orthod. Craniofacial Res. 2019, 22, 16–23. [Google Scholar] [CrossRef]
- Fields, H.W.; Proffit, W.R.; Case, J.C.; Vig, K.W.L. Variables Affecting Measurements of Vertical Occlusal Force. J. Dent. Res. 1986, 65, 135–138. [Google Scholar] [CrossRef]
- Imani, M.M.; Azizi, F.; Bahrami, K.; Golshah, A.; Safari-Faramani, R. In vitro bleaching effect of hydrogen peroxide with different time of exposition and concentration on shear bond strength of orthodontic brackets to human enamel: A meta-analysis of in vitro studies. Int. Orthod. 2020, 18, 22–31. [Google Scholar] [CrossRef]
- Elekdag-Turk, S.; Cakmak, F.; Isci, D.; Turk, T. 12-month self-ligating bracket failure rate with a self-etching primer. Angle Orthod. 2008, 78, 1095–1100. [Google Scholar] [CrossRef]
- Sunna, S.; Rock, W.P. Clinical performance of orthodontic brackets and adhesive systems: A randomized clinical trial. Br. J. Orthod. 1998, 25, 283–287. [Google Scholar] [CrossRef]
- Murray, S.D.; Hobson, R.S. Comparison of in vivo and in vitro shear bond strength. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 2–9. [Google Scholar] [CrossRef]
- Scribante, A.; Contreras-Bulnes, R.; Montasser, M.A.; Vallittu, P.K. Orthodontics: Bracket Materials, Adhesives Systems, and Their Bond Strength. BioMed Res. Int. 2016, 2016, 1329814. [Google Scholar] [CrossRef]
- Gaffey, P.G.; Major, P.W.; Glover, K.; Grace, M.; Koehler, J.R. Shear/peel bond strength of repositioned ceramic brackets. Angle Orthod. 1995, 65, 351–358. [Google Scholar]
- Littlewood, S.; Redhead, A. Use of jigs to standardise orthodontic bond testing. J. Dent. 1998, 26, 539–545. [Google Scholar] [CrossRef]
- Klocke, A.; Kahl-Nieke, B. Effect of debonding force direction on orthodontic shear bond strength. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 261–265. [Google Scholar] [CrossRef] [PubMed]
- Dall’Igna, C.M.; Marchioro, E.M.; Spohr, A.M.; Mota, E.G. Effect of curing time on the bond strength of a bracket-bonding system cured with a light-emitting diode or plasma arc light. Eur. J. Orthod. 2011, 33, 55–59. [Google Scholar] [CrossRef]
- Staderini, E.; Luca, M.; Candida, E.; Rizzo, M.I.; Rajabtork Zadeh, O.; Bucci, D.; Zama, M.; Lajolo, C.; Cordaro, M.; Gallenzi, P. Lay People Esthetic Evaluation of Primary Surgical Repair on Three-Dimensional Images of Cleft Lip and Palate Patients. Medicina 2019, 55, 576. [Google Scholar] [CrossRef] [PubMed]
- Scribante, A.; Sfondrini, M.F.; Gatti, S.; Gandini, P. Disinclusion of unerupted teeth by mean of self-ligating brackets: Effect of blood contamination on shear bond strength. Med. Oral Patol. Oral Cir. Bucal 2013, 18, e162–e167. [Google Scholar] [CrossRef]
- Romano, F.L.; Tavares, S.W.; Nouer, D.F.; Consani, S.; Magnani, M.B.B.A. Shear bond strength of metallic orthodontic brackets bonded to enamel prepared with self-etching primer. Angle Orthod. 2005, 75, 849–853. [Google Scholar]
- Sayinsu, K.; Isik, F.; Sezen, S.; Aydemir, B. New protective polish effects on shear bond strength of brackets. Angle Orthod. 2006, 76, 306–309. [Google Scholar]
- Signorelli, M.D.; Kao, E.; Ngan, P.W.; Gladwin, M.A. Comparison of bond strength between orthodontic brackets bonded with halogen and plasma arc curing lights: An in-vitro and in-vivo study. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 277–282. [Google Scholar] [CrossRef]
- Finnema, K.J.; Özcan, M.; Post, W.J.; Ren, Y.; Dijkstra, P.U. In-vitro orthodontic bond strength testing: A systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 615–622. [Google Scholar] [CrossRef]
- Bakhadher, W.; Halawany, H.; Talic, N.; Abraham, N.; Jacob, V. Factors Affecting the Shear Bond Strength of Orthodontic Brackets-A Review of In Vitro Studies. Acta Med. 2015, 58, 43–48. [Google Scholar] [CrossRef]
- Hung, C.Y.; Yu, J.H.; Su, L.W.; Uan, J.Y.; Chen, Y.C.; Lin, D.J. Shear Bonding Strength and Thermal Cycling Effect of Fluoride Releasable/Rechargeable Orthodontic Adhesive Resins Containing LiAl-F Layered Double Hydroxide (LDH) Filler. Materials 2019, 12, 3204. [Google Scholar] [CrossRef]
- Klocke, A.; Kahl-Nieke, B. Influence of force location in orthodontic shear bond strength testing. Dent. Mater. 2005, 21, 391–396. [Google Scholar] [CrossRef] [PubMed]
- Thomasa, R.L.; Rijk, W.G.; Evans, C.A. Tensile and shear stresses in the orthodontic attachment adhesive layer with 3D finite element analysis. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 530–532. [Google Scholar] [CrossRef]
- Bonetti, G.A.; Zanarini, M.; Parenti, S.I.; Lattuca, M.; Marchionni, S.; Gatto, M.R. Evaluation of enamel surfaces after bracket debonding: An in-vivo study with scanning electron microscopy. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 696–702. [Google Scholar]
- Abd, S.D.; Al-Khatieeb, M.M. Shear Bond Strength and Excess Adhesive Surface Topography of Different Bonding Systems after Thermocycling: A Comparative In-vitro Study. Int. J. Med. Res. Health Sci. 2018, 7, 46–54. [Google Scholar]
- Mirzakouchaki, B.; Kimyai, S.; Hydari, M.; Shahrbaf, S.; Mirzakouchaki-Boroujeni, P. Effect of self-etching primer/adhesive and conventional bonding on the shear bond strength in metallic and ceramic brackets. Med. Oral Patol. Oral Cir. Bucal 2012, 17, 164–170. [Google Scholar] [CrossRef][Green Version]
- Liu, J.K.; Chung, C.H.; Chang, C.Y.; Shieh, D.B. Bond strength and debonding characteristics of a new ceramic bracket. Am. J. Orthod. Dentofac. Orthop. 2005, 128, 761–765. [Google Scholar] [CrossRef]
- Bishara, S.E.; Oonsombat, C.; Soliman, M.M.; Warren, J.J.; Laffoon, J.F.; Ajlouni, R. Comparison of bonding time and shear bond strength between a conventional and a new integrated bonding system. Angle Orthod. 2005, 75, 237–242. [Google Scholar]
- Sfondrini, M.F.; Gatti, S.; Scribante, A. Shear bond strength of self-ligating brackets. Eur. J. Orthod. 2011, 33, 71–74. [Google Scholar] [CrossRef]
- Northrup, R.G.; Berzins, D.W.; Bradley, T.G.; Schuckit, W. Shear bond strength comparison between two orthodontic adhesives and self-ligating and conventional brackets. Angle Orthod. 2007, 77, 701–706. [Google Scholar] [CrossRef]
- Theodorakopoulou, L.P.; Sadowsky, P.L.; Jacobson, A.; Lacefield, W., Jr. Evaluation of the debonding characteristics of 2 ceramic brackets: An in vitro study. Am. J. Orthod. Dentofac. Orthop. 2004, 125, 329–336. [Google Scholar] [CrossRef]
- Zielinski, V.; Reimann, S.; Jäger, A.; Bourauel, C. Comparison of shear bond strength of plastic and ceramic brackets. J. Orofac. Orthop. Fortschr. Kieferorthopädie 2014, 75, 345–357. [Google Scholar]
- Stein, S.; Kleye, A.; Schauseil, M.; Hellak, A.; Korbmacher-Steiner, H.; Braun, A. 445-nm diode laser-assisted debonding of self-ligating ceramic brackets. Biomed. Eng. Biomed. Tech. 2017, 62, 513–520. [Google Scholar]
- Jeiroudi, M.T. Enamel fracture caused by ceramic brackets. Am. J. Orthod. Dentofac. Orthop. 1991, 99, 97–99. [Google Scholar]
- Viazis, A.D.; Cavanaugh, G.; Bevis, R.R. Bond strength of ceramic brackets under shear stress: An in vitro report. Am. J. Orthod. Dentofac. Orthop. 1990, 98, 214–221. [Google Scholar]
- Sheibaninia, A.; Sepasi, S.; Saghiri, M.A.; Sepasi, S. The Effect of an Acidic Food-Simulating Environment on the Shear Bond Strength of Self-Ligating Brackets with Different Base Designs. Int. J. Dent. 2014, 2014, 689536. [Google Scholar]
- Cozza, P.; Martucci, L.; Toffol, L.; Penco, S.I. Shear bond strength of metal brackets on enamel. Angle Orthod. 2006, 76, 851–856. [Google Scholar]
- Bishara, S.E.; VonWald, L.; Laffoon, J.F.; Warren, J.J. Effect of a self-etch primer/adhesive on the shear bond strength of orthodontic brackets. Am. J. Orthod. Dentofac. Orthop. 2001, 119, 621–624. [Google Scholar]
- Turk, T.; Elekdag-Turk, S.; Isci, D. Effects of self-etching primer on shear bond strength of orthodontic brackets at different debond times. Angle Orthod. 2007, 77, 108–112. [Google Scholar]
- Yamada, R.; Hayakawa, T.; Kasai, K. Effect of using self-etching primer for bonding orthodontic brackets. Angle Orthod. 2002, 72, 558–564. [Google Scholar]
- Farahani, M.; Kabiri, S.; Motamedian, S.R.; Hajighadimi, M. Effect of Bracket Base Sandblasting on Bonding of Orthodontic Brackets on Enamel Surface. Dent. Hypotheses 2016, 7, 133–136. [Google Scholar]
- Dalaie, K.; Mirfasihi, A.; Eskandarion, S.; Kabiri, S. Effect of bracket base design on shear bond strength to feldspathic porcelain. Eur. J. Dent. 2016, 10, 351–355. [Google Scholar] [CrossRef] [PubMed]
- Patini, R.; Staderini, E.; Camodeca, A.; Guglielmi, F.; Gallenzi, P. Case Reports in Pediatric Dentistry Journals: A Systematic Review about Their Effect on Impact Factor and Future Investigations. Dent. J. 2019, 7, 103. [Google Scholar] [CrossRef] [PubMed]

| Manufacturer | Adhesive Materials | Group/Groups Used | Composition of Adhesive Agent | % by Wt |
|---|---|---|---|---|
| Bisphenol A diglycidyl ether dimethacrylate (BISGMA) | 45–55 | |||
| 3M Unitek, Monrovia, CA, USA | Transbond™ XT Light Cure Adhesive Primer | Group 1 (etch-and-rinse) | Triethylene glycol dimethacrylate (TEGDMA) | 45–55 |
| 4-(Dimethylamino)-benzeneethanol | <0.5 | |||
| Methacrylated pyrophosphates | 10–25 | |||
| Ethylene dimethacrylate | 0–2 | |||
| Phosphoric acid | 0–2 | |||
| 3M Unitek, Monrovia, CA, USA | Transbond™ Plus Self Etching Primer | Group 2 (self-etching-primer) | 2-Hydroxyethyl methacrylate (HEMA) | <1 |
| 2-Propenoic acid, 2-methyl-, phosphinicobis (oxy-2,1-ethandiyl) ester | 25–40 | |||
| Water | 15–25 | |||
| DL-Camphorquinone | <3 | |||
| Silane-treated quartz | 70–80 | |||
| Bisphenol A diglycidyl ether dimethacrylate (BISGMA) | 10–20 | |||
| Bisphenol A dimethacrylate | 5–10 | |||
| 3M Unitek, Monrovia, CA, USA | Transbond™ XT Light Cure Adhesive Paste | Group 1 and Group 2 | Silane-treated silica | <2 |
| Diphenyliodonium hexafluorophosphate | <1 | |||
| Triphenylantimony | <1 |
| Groups | Levene Statistics | df1 | df2 | Significance Value (p) |
|---|---|---|---|---|
| Group 1 | 1.56 | 9 | 140 | 0.13 |
| Group 2 | 3.32 | 9 | 140 | 0.001 * |
| Group | Sum of Squares | df | Mean of Squares | F | Significance Value (p) | |
|---|---|---|---|---|---|---|
| Group 1 | Between groups | 4651.57 | 9 | 516.84 | 28.62 | <0.001 |
| In-group | 2528.26 | 140 | 18.05 | |||
| Total | 7179.84 | 149 |
| Group | Sum of Squares | df | Mean of Squares | F | Significance Value (p) | |
|---|---|---|---|---|---|---|
| Group 2 | Between groups | 2853.62 | 9 | 317.07 | 35.54 | <0.001 |
| In-group | 1249.06 | 140 | 8.92 | |||
| Total | 4102.69 | 149 |
| Group | Bracket Type | Sample | Strokes | Smin | Smax |
|---|---|---|---|---|---|
| Group 1 | APC Victory series metal bracket | 15 | 18.00 ± 4.79 | 9 | 28 |
| Victory series metal bracket | 15 | 19.06 ± 3.89 | 12 | 25 | |
| Gemini metal bracket | 15 | 15.26 ± 4.49 | 5 | 22 | |
| Gemini Clear ceramic bracket | 15 | 24.46 ± 4.24 | 19 | 32 | |
| Gemini SL self-ligating metal bracket | 15 | 14.66 ± 2.76 | 10 | 19 | |
| Clarity Advanced ceramic bracket | 15 | 20.86 ± 3.48 | 12 | 26 | |
| Clarity SL self-ligating ceramic bracket | 15 | 22.26 ± 7.28 | 14 | 45 | |
| Equilibrium® 2 metal bracket | 15 | 19.66 ± 4.65 | 13 | 33 | |
| Mini Sprint® metal bracket | 15 | 6.40 ± 2.22 | 4 | 12 | |
| Mini Master series metal bracket | 15 | 8.13 ± 2.16 | 4 | 11 | |
| Mean | 150 | 16.88 ± 6.94 | 4 | 45 | |
| Group 2 | APC Victory series metal bracket | 15 | 12.40 ± 2.64 | 10 | 18 |
| Victory series metal bracket | 15 | 13.73 ± 3.97 | 8 | 22 | |
| Gemini metal bracket | 15 | 12.33 ± 2.19 | 8 | 16 | |
| Gemini Clear ceramic bracket | 15 | 20.86 ± 4.18 | 15 | 29 | |
| Gemini SL self-ligating metal bracket | 15 | 12.26 ± 2.54 | 9 | 18 | |
| Clarity Advanced ceramic bracket | 15 | 16.13 ± 3.48 | 10 | 23 | |
| Clarity SL self-ligating ceramic bracket | 15 | 15.06 ± 3.69 | 10 | 22 | |
| Equilibrium® 2 metal bracket | 15 | 19.20 ± 2.78 | 14 | 25 | |
| Mini Sprint® metal bracket | 15 | 5.86 ± 1.68 | 4 | 9 | |
| Mini Master series metal bracket | 15 | 7.86 ± 1.12 | 6 | 9 | |
| Mean | 150 | 13.57 ± 5.24 | 4 | 29 |
| Adhesive Agent | Sample Size | Strokes |
|---|---|---|
| Group 1 (Transbond XT) | 150 | 16.88 ± 6.94 |
| Group 2 (Transbond Plus) | 150 | 13.57 ± 5.24 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cicek, O.; Ozkalayci, N.; Yetmez, M. Mean Shearing Stroke Frequency of Orthodontic Brackets under Cycling Loading: An In Vitro Study. Materials 2020, 13, 4280. https://doi.org/10.3390/ma13194280
Cicek O, Ozkalayci N, Yetmez M. Mean Shearing Stroke Frequency of Orthodontic Brackets under Cycling Loading: An In Vitro Study. Materials. 2020; 13(19):4280. https://doi.org/10.3390/ma13194280
Chicago/Turabian StyleCicek, Orhan, Nurhat Ozkalayci, and Mehmet Yetmez. 2020. "Mean Shearing Stroke Frequency of Orthodontic Brackets under Cycling Loading: An In Vitro Study" Materials 13, no. 19: 4280. https://doi.org/10.3390/ma13194280
APA StyleCicek, O., Ozkalayci, N., & Yetmez, M. (2020). Mean Shearing Stroke Frequency of Orthodontic Brackets under Cycling Loading: An In Vitro Study. Materials, 13(19), 4280. https://doi.org/10.3390/ma13194280






