Five Degree Internal Conical Connection and Marginal Bone Stability around Subcrestal Implants: A Retrospective Analysis
Abstract
:1. Introduction
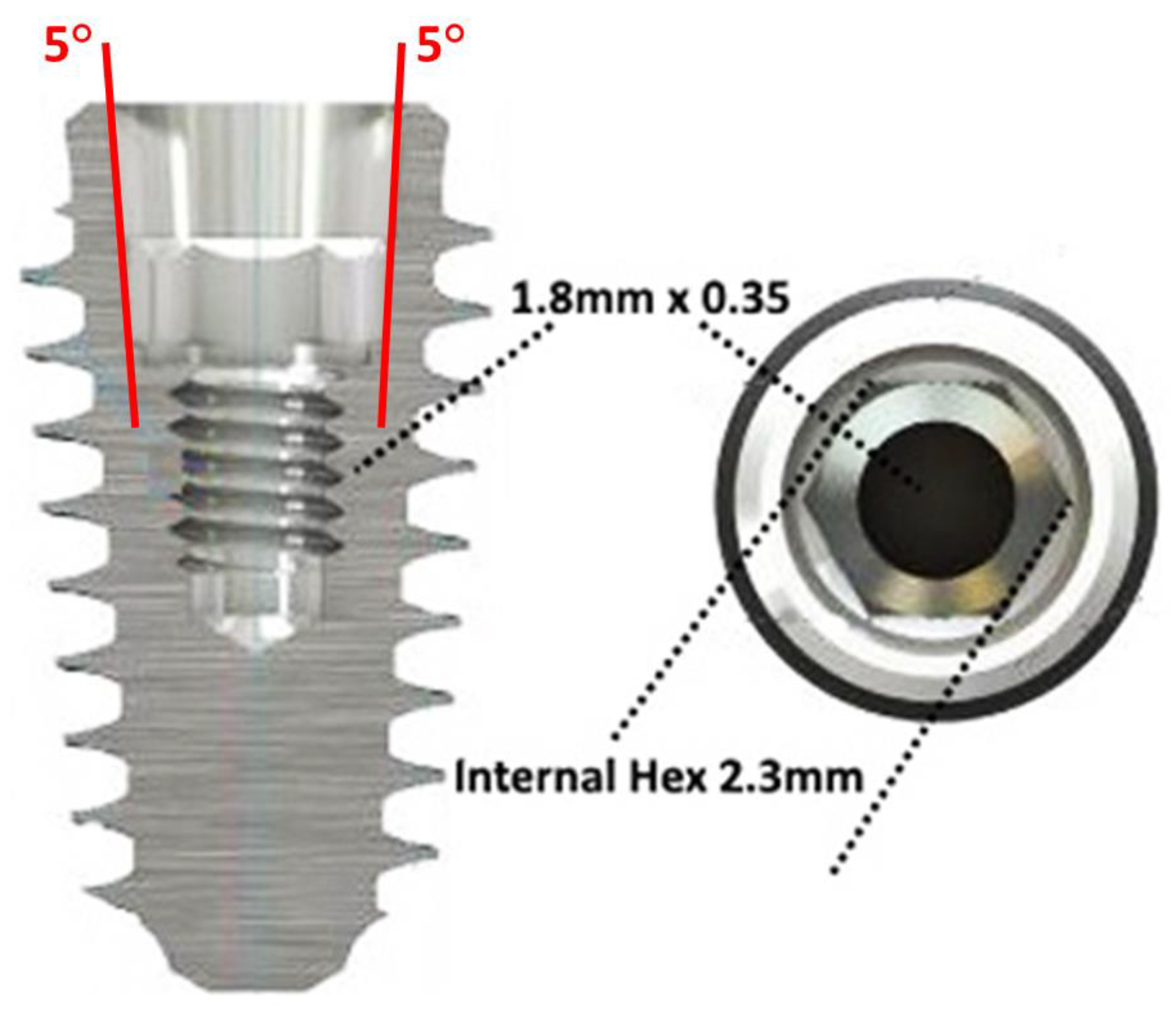
2. Materials and Methods
2.1. Patient Selection
2.2. Surgical and Prosthetic Procedures
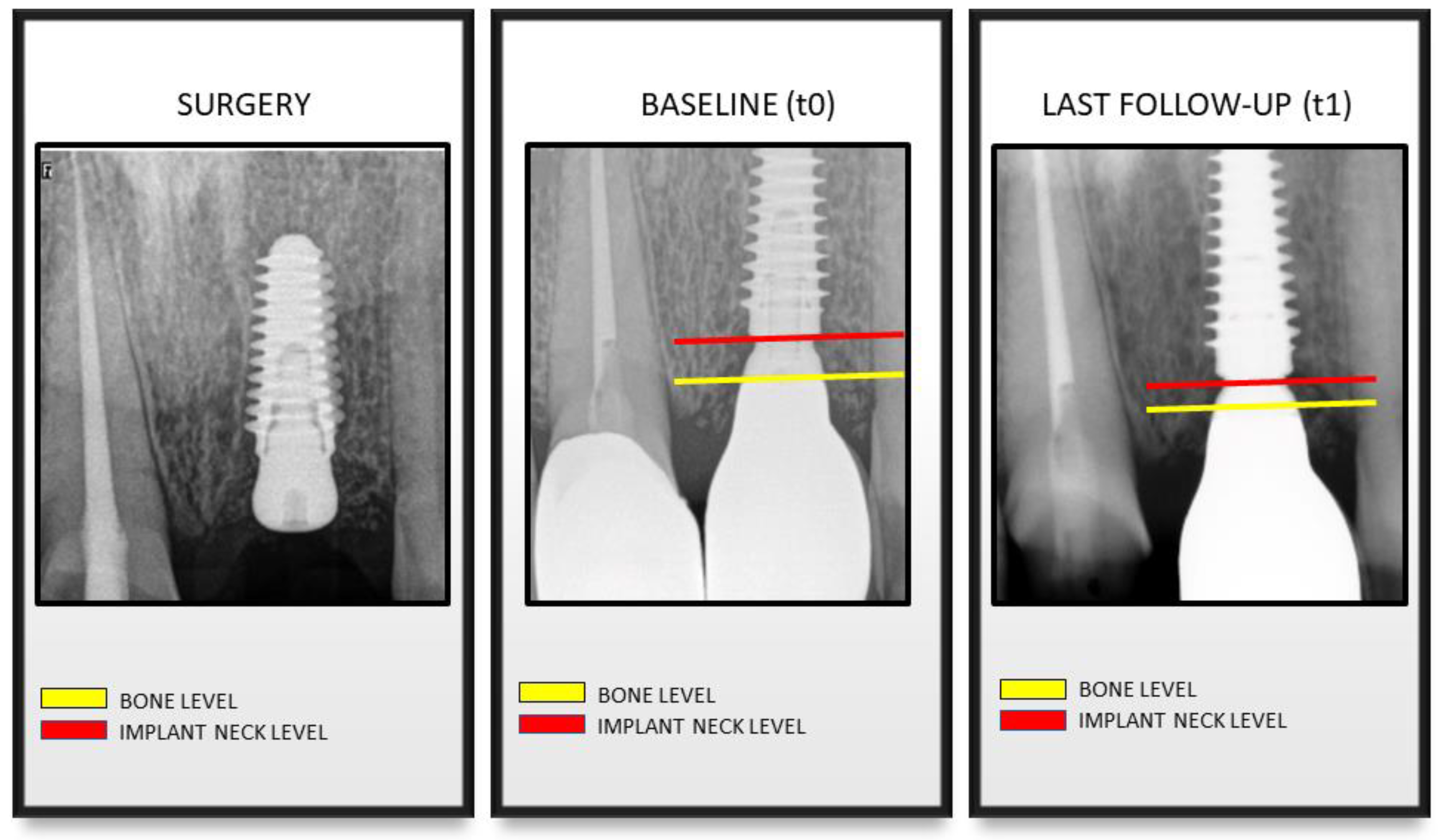
2.3. Clinical and Radiographic Evaluations
2.4. Statistical Analysis
3. Results
3.1. Patient Features
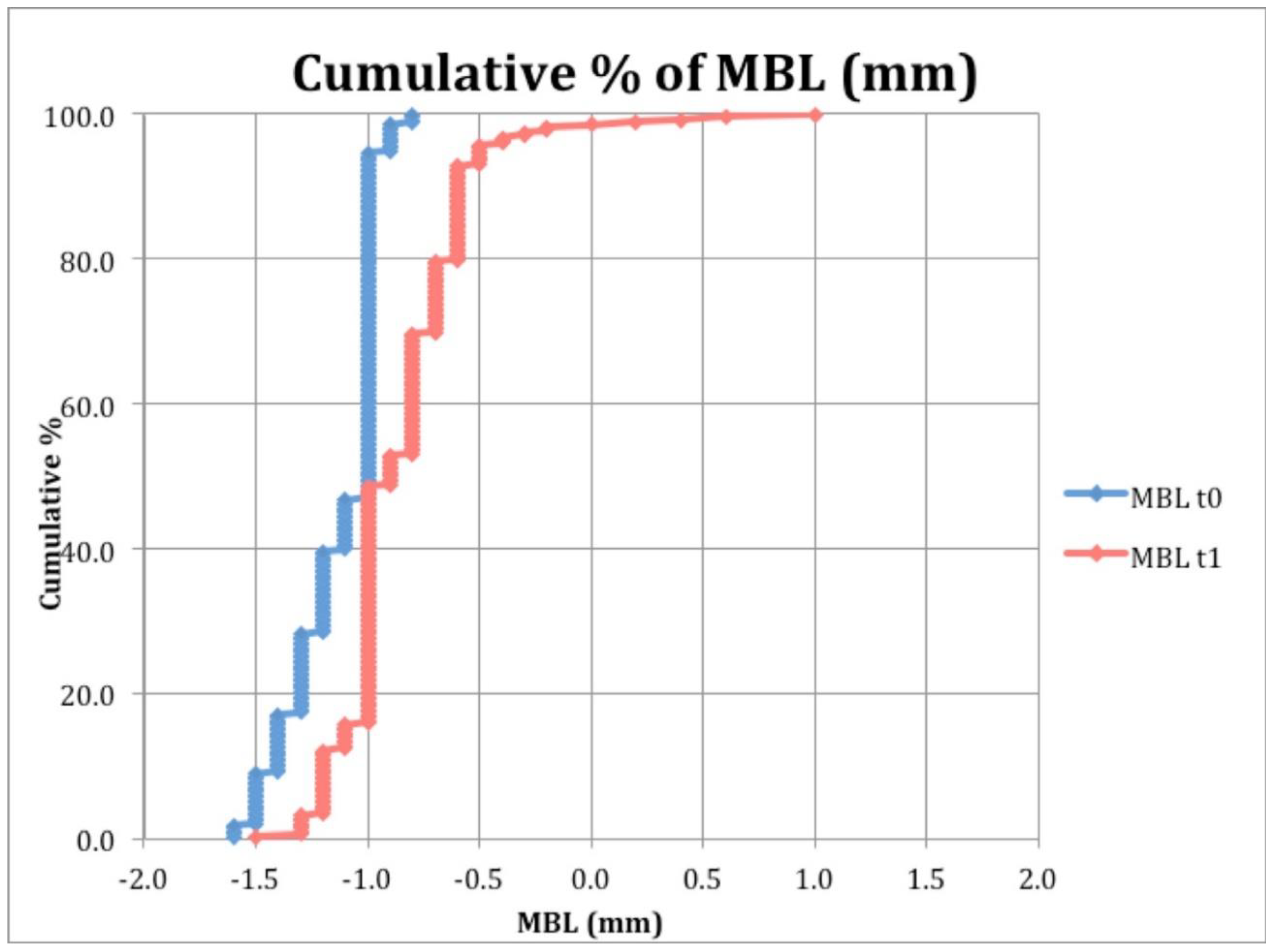
3.2. Clinical and Radiographic Evaluations
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jung, R.E.; Zembic, A.; Pjetursson, B.E.; Zwahlen, M.; Thoma, D.S. Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin. Oral Implants Res. 2012, 23, 2–21. [Google Scholar] [CrossRef] [PubMed]
- Bragger, U.; Karoussis, I.; Persson, R.; Pjetursson, B.; Salvi, G.; Lang, N. Technical and biological complications/failures with single crowns and fixed partial dentures on implants: A 10-year prospective cohort study. Clin. Oral Implants Res. 2005, 16, 326–334. [Google Scholar] [CrossRef] [PubMed]
- Chrcanovic, B.R.; Kisch, J.; Albrektsson, T.; Wennerberg, A. Factors Influencing Early Dental Implant Failures. J. Dent. Res. 2016, 95, 995–1002. [Google Scholar] [CrossRef]
- Albrektsson, T.; Zarb, G.; Worthington, P.; Eriksson, A.R. The long-term efficacy of currently used dental implants: A review and proposed criteria of success. Int. J. Oral Maxillofac. Implants 1986, 1, 11–25. [Google Scholar]
- Adell, R.; Lekholm, U.; Rockler, B.; Branemark, P.I.; Lindhe, J.; Eriksson, B.; Sbordone, L. Marginal tissue reactions at osseointegrated titanium fixtures (I). A 3-year longitudinal prospective study. Int. J. Oral Maxillofac. Surg. 1986, 15, 39–52. [Google Scholar] [CrossRef]
- Albrektsson, T.; Canullo, L.; Cochran, D.; De Bruyn, H. “Peri-Implantitis”: A Complication of a Foreign Body or a Man-Made “Disease”. Facts and Fiction. Clin. Implant Dent. Relat. Res. 2016, 18, 840–849. [Google Scholar] [CrossRef] [PubMed]
- Laurell, L.; Lundgren, D. Marginal bone level changes at dental implants after 5 years in function: A meta-analysis. Clin. Implant Dent. Relat. Res. 2011, 13, 19–28. [Google Scholar] [CrossRef]
- Branemark, P.I.; Hansson, B.O.; Adell, R.; Breine, U.; Lindstrom, J.; Hallen, O.; Ohman, A. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand. J. Plast. Reconstr. Surg. Suppl. 1977, 16, 1–132. [Google Scholar] [PubMed]
- Hermann, F.; Lerner, H.; Palti, A. Factors influencing the preservation of the periimplant marginal bone. Implant Dent. 2007, 16, 165–175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Misch, C.E. Dental Implant Prosthetics-E-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2004. [Google Scholar]
- Misch, C.E. Contemporary Implant Dentistry-E-Book; Elsevier Health Sciences: Amsterdam, The Netherlands, 2007. [Google Scholar]
- Canullo, L.; Pesce, P.; Patini, R.; Antonacci, D.; Tommasato, G. What Are the Effects of Different Abutment Morphologies on Peri-implant Hard and Soft Tissue Behavior? A Systematic Review and Meta-Analysis. Int. J. Prosthodont. 2020, 33, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Canullo, L.; Fedele, G.R.; Iannello, G.; Jepsen, S. Platform switching and marginal bone-level alterations: The results of a randomized-controlled trial. Clin. Oral Implants Res. 2010, 21, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Pieri, F.; Aldini, N.N.; Marchetti, C.; Corinaldesi, G. Influence of implant-abutment interface design on bone and soft tissue levels around immediately placed and restored single-tooth implants: A randomized controlled clinical trial. Int. J. Oral Maxillofac. Implants 2011, 26, 169–178. [Google Scholar] [PubMed]
- Schmitt, C.M.; Nogueira-Filho, G.; Tenenbaum, H.C.; Lai, J.Y.; Brito, C.; Doring, H.; Nonhoff, J. Performance of conical abutment (Morse Taper) connection implants: A systematic review. J. Biomed. Mater. Res. A 2014, 102, 552–574. [Google Scholar] [CrossRef] [PubMed]
- Ugurel, C.S.; Steiner, M.; Isik-Ozkol, G.; Kutay, O.; Kern, M. Mechanical resistance of screwless morse taper and screw-retained implant-abutment connections. Clin. Oral Implants Res. 2015, 26, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Hansson, S. A conical implant-abutment interface at the level of the marginal bone improves the distribution of stresses in the supporting bone. An axisymmetric finite element analysis. Clin. Oral Implants Res. 2003, 14, 286–293. [Google Scholar] [CrossRef] [PubMed]
- Lazzara, R.J.; Porter, S.S. Platform switching: A new concept in implant dentistry for controlling postrestorative crestal bone levels. Int. J. Periodontics Restor. Dent. 2006, 26, 9–17. [Google Scholar]
- Luongo, R.; Traini, T.; Guidone, P.C.; Bianco, G.; Cocchetto, R.; Celletti, R. Hard and soft tissue responses to the platform-switching technique. Int. J. Periodontics Restor. Dent. 2008, 28, 551–557. [Google Scholar]
- Koutouzis, T.; Neiva, R.; Nonhoff, J.; Lundgren, T. Placement of implants with platform-switched Morse taper connections with the implant-abutment interface at different levels in relation to the alveolar crest: A short-term (1-year) randomized prospective controlled clinical trial. Int. J. Oral Maxillofac. Implants 2013, 28, 1553–1563. [Google Scholar] [CrossRef] [Green Version]
- Degidi, M.; Perrotti, V.; Shibli, J.A.; Novaes, A.B.; Piattelli, A.; Iezzi, G. Equicrestal and subcrestal dental implants: A histologic and histomorphometric evaluation of nine retrieved human implants. J. Periodontol. 2011, 82, 708–715. [Google Scholar] [CrossRef] [PubMed]
- Koutouzis, T.; Neiva, R.; Nair, M.; Nonhoff, J.; Lundgren, T. Cone beam computed tomographic evaluation of implants with platform-switched Morse taper connection with the implant-abutment interface at different levels in relation to the alveolar crest. Int. J. Oral Maxillofac. Implants 2014, 29, 1157–1163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Welander, M.; Abrahamsson, I.; Berglundh, T. Subcrestal placement of two-part implants. Clin. Oral Implants Res. 2009, 20, 226–231. [Google Scholar] [CrossRef] [PubMed]
- Froum, S.J.; Cho, S.C.; Suzuki, T.; Yu, P.; Corby, P.; Khouly, I. Epicrestal and subcrestal placement of platform-switched implants: 18 month-result of a randomized, controlled, split-mouth, prospective clinical trial. Clin. Oral Implants Res. 2018, 29, 353–366. [Google Scholar] [CrossRef] [PubMed]
- Gualini, F.; Salina, S.; Rigotti, F.; Mazzarini, C.; Longhin, D.; Grigoletto, M.; Trullenque-Eriksson, A.; Sbricoli, L.; Esposito, M. Subcrestal placement of dental implants with an internal conical connection of 0.5 mm versus 1.5 mm: Outcome of a multicentre randomised controlled trial 1 year after loading. Eur. J. Oral Implantol. 2017, 10, 73–82. [Google Scholar]
- Cosyn, J.; Eghbali, A.; De Bruyn, H.; Collys, K.; Cleymaet, R.; De Rouck, T. Immediate single-tooth implants in the anterior maxilla: 3-year results of a case series on hard and soft tissue response and aesthetics. J. Clin. Periodontol. 2011, 38, 746–753. [Google Scholar] [CrossRef] [PubMed]
- Lops, D.; Chiapasco, M.; Rossi, A.; Bressan, E.; Romeo, E. Incidence of inter-proximal papilla between a tooth and an adjacent immediate implant placed into a fresh extraction socket: 1-year prospective study. Clin. Oral Implants Res. 2008, 19, 1135–1140. [Google Scholar] [CrossRef]
- Galindo-Moreno, P.; Fernandez-Jimenez, A.; O’Valle, F.; Monje, A.; Silvestre, F.J.; Juodzbalys, G.; Sanchez-Fernandez, E.; Catena, A. Influence of the crown-implant connection on the preservation of peri-implant bone: A retrospective multifactorial analysis. Int. J. Oral Maxillofac. Implants 2015, 30, 384–390. [Google Scholar] [CrossRef] [Green Version]
- Lops, D.; Parpaiola, A.; Paniz, G.; Sbricoli, L.; Magaz, V.R.; Venezze, A.C.; Bressan, E.; Stellini, E. Interproximal Papilla Stability Around CAD/CAM and Stock Abutments in Anterior Regions: A 2-Year Prospective Multicenter Cohort Study. Int. J. Periodontics Restor. Dent. 2017, 37, 657–665. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lops, D.; Romeo, E.; Chiapasco, M.; Procopio, R.M.; Oteri, G. Behaviour of soft tissues healing around single bone-level-implants placed immediately after tooth extraction A 1 year prospective cohort study. Clin. Oral Implants Res. 2013, 24, 1206–1213. [Google Scholar] [CrossRef]
- Lang, N.P.; Berglundh, T. Periimplant diseases: Where are we now?--Consensus of the Seventh European Workshop on Periodontology. J. Clin. Periodontol. 2011, 38, 178–181. [Google Scholar] [CrossRef] [Green Version]
- Galindo-Moreno, P.; León-Cano, A.; Ortega-Oller, I.; Monje, A.; O’Valle, F.; Catena, A. Marginal bone loss as success criterion in implant dentistry: Beyond 2 mm. Clin. Oral Implants Res. 2015, 26, 28–34. [Google Scholar] [CrossRef]
- Spinato, S.; Stacchi, C.; Lombardi, T.; Bernardello, F.; Messina, M.; Zaffe, D. Biological width establishment around dental implants is influenced by abutment height irrespective of vertical mucosal thickness: A cluster randomized controlled trial. Clin. Oral Implants Res. 2019, 30, 649–659. [Google Scholar] [CrossRef] [PubMed]
- Lombardi, T.; Berton, F.; Salgarello, S.; Barbalonga, E.; Rapani, A.; Piovesana, F.; Gregorio, C.; Barbati, G.; Di Lenarda, R.; Stacchi, C. Factors Influencing Early Marginal Bone Loss around Dental Implants Positioned Subcrestally: A Multicenter Prospective Clinical Study. J. Clin. Med. 2019, 8, 1168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomasi, C.; Tessarolo, F.; Caola, I.; Piccoli, F.; Wennstrom, J.L.; Nollo, G.; Berglundh, T. Early healing of peri-implant mucosa in man. J. Clin. Periodontol. 2016, 43, 816–824. [Google Scholar] [CrossRef]
- Palacios-Garzón, N.; Velasco-Ortega, E.; López-López, J. Bone Loss in Implants Placed at Subcrestal and Crestal Level: A Systematic Review and Meta-Analysis. Materials 2019, 12, 154. [Google Scholar] [CrossRef] [Green Version]
- Salina, S.; Gualini, F.; Rigotti, F.; Mazzarini, C.; Longhin, D.; Grigoletto, M.; Buti, J.; Sbricoli, L.; Esposito, M. Subcrestal placement of dental implants with an internal conical connection of 0.5 mm versus 1.5 mm: Three-year after loading results of a multicentre within-person randomised controlled trial. Int. J. Oral Implantol. 2019, 12, 155–167. [Google Scholar]
- Gatti, C.; Gatti, F.; Silvestri, M.; Mintrone, F.; Rossi, R.; Tridondani, G.; Piacentini, G.; Borrelli, P. A Prospective Multicenter Study on Radiographic Crestal Bone Changes Around Dental Implants Placed at Crestal or Subcrestal Level: One-Year Findings. Int. J. Oral Maxillofac. Implants 2018, 33, 913–918. [Google Scholar] [CrossRef]
- Linkevicius, T.; Puisys, A.; Linkevicius, R.; Alkimavicius, J.; Gineviciute, E.; Linkeviciene, L. The influence of submerged healing abutment or subcrestal implant placement on soft tissue thickness and crestal bone stability. A 2-year, randomized clinical trial. Clin. Implant Dent. Relat. Res. 2020, 6. [Google Scholar] [CrossRef]
- Vervaeke, S.; Matthys, C.; Nassar, R.; Christiaens, V.; Cosyn, J.; De Bruyn, H. Adapting the vertical position of implants with a conical connection in relation to soft tissue thickness prevents early implant surface exposure: A 2-year prospective intra-subject comparison. J. Clin. Periodontol. 2018, 45, 605–612. [Google Scholar] [CrossRef]
- Pico, A.; Martín-Lancharro, P.; Caneiro, L.; Nóvoa, L.; Batalla, P.; Blanco, J. Influence of abutment height and implant depth position on interproximal peri-implant bone in sites with thin mucosa: A 1-year randomized clinical trial. Clin. Oral Implants Res. 2019, 30, 595–602. [Google Scholar] [CrossRef]
- Wennerberg, A.; Sennerby, L.; Kultje, C.; Lekholm, U. Some soft tissue characteristics at implant abutments with different surface topography. A study in humans. J. Clin. Periodontol. 2003, 30, 88–94. [Google Scholar] [CrossRef]
- Caricasulo, R.; Malchiodi, L.; Ghensi, P.; Fantozzi, G.; Cucchi, A. The influence of implant-abutment connection to peri-implant bone loss: A systematic review and meta-analysis. Clin. Implant Dent. Relat. Res. 2018, 20, 653–664. [Google Scholar] [CrossRef] [PubMed]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Diabetes and oral implant failure: A systematic review. J. Dent. Res. 2014, 93, 859–867. [Google Scholar] [CrossRef] [PubMed]
- Moraschini, V.; Barboza, E.S.; Peixoto, G.A. The impact of diabetes on dental implant failure: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2016, 45, 1237–1245. [Google Scholar] [CrossRef] [PubMed]
- Montero, J.; Fernandezruiz, A.; Pardalpelaez, B.; Jimenezguerra, A.; Velascoortega, E.; Nicolassilvente, A.I.; Monsalveguil, L. Effect of Rough Surface Platforms on the Mucosal Attachment and the Marginal Bone Loss of Implants: A Dog Study. Materials 2020, 13, 802. [Google Scholar] [CrossRef] [Green Version]
| Diameter (mm) | Total | ||||||
|---|---|---|---|---|---|---|---|
| 3.5 | 4 | 4.5 | 5 | 6.5 | |||
| Length (mm) | 7 | 2 | 2 | 7 | 8 | 11 | 30 |
| 8.5 | 4 | 13 | 1 | 2 | 12 | 32 | |
| 10 | 10 | 45 | 39 | 11 | 1 | 106 | |
| 11.5 | 11 | 8 | 3 | 1 | 0 | 23 | |
| 13 | 34 | 83 | 69 | 4 | 0 | 190 | |
| 15 | 22 | 3 | 4 | 0 | 0 | 29 | |
| Total | 83 | 154 | 123 | 26 | 24 | 410 | |
| Anterior | Posterior | Total | |
|---|---|---|---|
| Maxilla | 75 | 156 | 231 |
| Mandible | 45 | 134 | 179 |
| Total | 120 | 290 | 410 |
| Type of Prosthesis | Follow-Up | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 2 Years | 3 Years | 4 Years | 5 Years | 6 Years | 7 Years | 9 Years | |||
| SC | 24 | 5 | 4 | 1 | 1 | 0 | 0 | 35 | |
| FPD | 55 | 11 | 14 | 11 | 1 | 3 | 1 | 96 | |
| FFD | 10 | 0 | 2 | 0 | 0 | 0 | 0 | 12 | |
| TO | 17 | 2 | 0 | 1 | 0 | 1 | 0 | 21 | |
| Total | 106 | 18 | 20 | 13 | 2 | 4 | 1 | 164 | |
| Follow-up | Frequency | MBL t0 | MBL t1 | MBL Change | |||
|---|---|---|---|---|---|---|---|
| Mean | sd | Mean | sd | Mean | sd | ||
| 2 years | 280 | −1.09 | 0.37 | −0.85 | 0.29 | −0.24 | 0.41 |
| 3 years | 38 | −1.08 | 0.66 | −1.02 | 0.39 | −0.06 | 0.58 |
| 4 years | 50 | −0.77 | 1.32 | −1.36 | 0.19 | 0.59 | 1.28 |
| 5 years | 25 | −1.62 | 0.20 | −1.48 | 0.18 | −0.14 | 0.29 |
| 6 years | 3 | −1.47 | 0.29 | −1.30 | 0.17 | −0.17 | 0.12 |
| 7 years | 12 | −1.12 | 1.31 | −1.61 | 0.17 | 0.49 | 1.23 |
| 9 years | 2 | −2.10 | 0.14 | −1.95 | 0.07 | −0.15 | 0.21 |
| Total | 410 | −1.09 | 0.65 | −1.00 | 0.37 | −0.09 | 0.68 |
| Clinical Conditions | ||||||
|---|---|---|---|---|---|---|
| No (n = 72) | Smoke (n = 15) | Diabetes (n = 4) | Bisphosphonates (n = 2) | p Value | ||
| MBL change | Mean | −0.13 | −0.14 | −0.42 | 1.30 | 0.031 |
| sd | 0.49 | 0.14 | 0.25 | 1.98 | ||
| Vs. Followup | n | Mean | sd | p Value | |
|---|---|---|---|---|---|
| MBL change | 2 years | 280 | −0.24 | 0.41 | p < 0.001 |
| >2years | 130 | 0.22 | 0.99 |
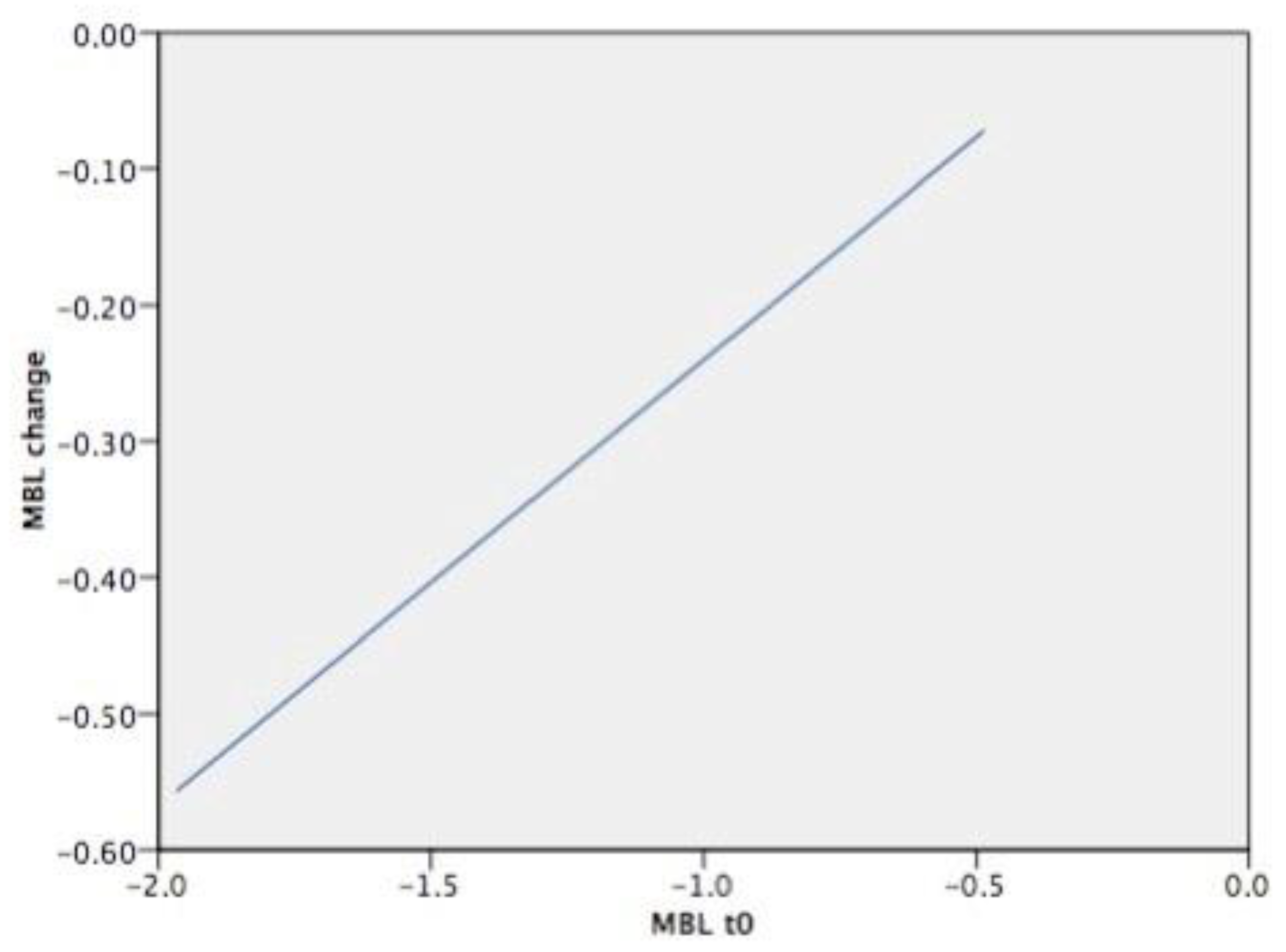
| Predictors | Unstandardized Coefficients (B) | Standard Error | t-Statistics | p-Value |
|---|---|---|---|---|
| Constant | 0.062 | 0.052 | 1.195 | 0.233 |
| Follow-up | 0.086 | 0.011 | 8.165 | <0.001 |
| MBL(t0) | 0.346 | 0.049 | 7.126 | <0.001 |
| Diabetes | −0.292 | 0.048 | −6.033 | <0.001 |
| Predictor | MBL Change | |
|---|---|---|
| Follow-up | 2 years, 3 years | −0.43 |
| 4 years, 5 years, 6 years, 7 years, 9 years | −0.21 | |
| Presence of diabetes | yes | −0.46 |
| no | −0.18 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lops, D.; Stocchero, M.; Motta Jones, J.; Freni, A.; Palazzolo, A.; Romeo, E. Five Degree Internal Conical Connection and Marginal Bone Stability around Subcrestal Implants: A Retrospective Analysis. Materials 2020, 13, 3123. https://doi.org/10.3390/ma13143123
Lops D, Stocchero M, Motta Jones J, Freni A, Palazzolo A, Romeo E. Five Degree Internal Conical Connection and Marginal Bone Stability around Subcrestal Implants: A Retrospective Analysis. Materials. 2020; 13(14):3123. https://doi.org/10.3390/ma13143123
Chicago/Turabian StyleLops, Diego, Michele Stocchero, Jason Motta Jones, Alessandro Freni, Antonino Palazzolo, and Eugenio Romeo. 2020. "Five Degree Internal Conical Connection and Marginal Bone Stability around Subcrestal Implants: A Retrospective Analysis" Materials 13, no. 14: 3123. https://doi.org/10.3390/ma13143123
APA StyleLops, D., Stocchero, M., Motta Jones, J., Freni, A., Palazzolo, A., & Romeo, E. (2020). Five Degree Internal Conical Connection and Marginal Bone Stability around Subcrestal Implants: A Retrospective Analysis. Materials, 13(14), 3123. https://doi.org/10.3390/ma13143123







